Traditional, Complementary and Alternative Medicines in the Treatment of Ejaculatory Disorders: A Systematic Review
Abstract
:1. Introduction
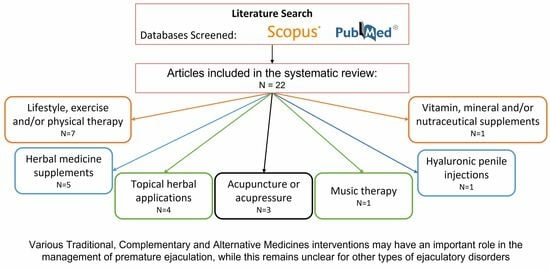
2. Materials and Methods
3. Results
4. Discussion
4.1. Lifestyle, Exercise and/or Physical Therapy
4.2. Herbal Medicine Supplements
4.3. Topical Herbal Applications
4.4. Acupuncture and Electroacupuncture
4.5. Vitamin, Mineral and Nutraceutical Supplements
4.6. Hyaluronic Acid
4.7. Music Therapy
4.8. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Otani, T. Clinical review of ejaculatory dysfunction. Reprod. Med. Biol. 2019, 18, 331–343. [Google Scholar] [CrossRef] [PubMed]
- Jannini, E.A.; Lenzi, A. Ejaculatory disorders: Epidemiology and current approaches to definition, classification and subtyping. World J. Urol. 2005, 23, 68–75. [Google Scholar] [CrossRef] [PubMed]
- McMahon, C.; Jannini, E.; Waldinger, M.; Rowland, D. Standard operating procedures in the disorders of orgasm and ejaculation. J. Sex. Med. 2013, 10, 204–229. [Google Scholar] [CrossRef] [PubMed]
- Parnham, A.; Serefoglu, E.C. Retrograde ejaculation, painful ejaculation and hematospermia. Transl. Androl. Urol. 2016, 5, 592. [Google Scholar] [CrossRef]
- Di Sante, S.; Mollaioli, D.; Gravina, G.L.; Ciocca, G.; Limoncin, E.; Carosa, E.; Lenzi, A.; Jannini, E.A. Epidemiology of delayed ejaculation. Transl. Androl. Urol. 2016, 5, 541. [Google Scholar] [CrossRef]
- Mazzilli, R.; Defeudis, G.; Olana, S.; Zamponi, V.; Macera, M.; Mazzilli, F. The role of ejaculatory dysfunction on male infertility. Clin. Ter. 2020, 171, E523–E527. [Google Scholar]
- Serefoglu, E.C.; Mcmahon, C.G.; Waldinger, M.D.; Althof, S.E.; Shindel, A.; Adaikan, G.; Becher, E.F.; Dean, J.; Giuliano, F.; Hellstrom, W.J.G.; et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: Report of the Second International Society for Sexual Medicine ad hoc committee for the definition of premature ejaculation. Sex. Med. 2014, 2, 41–59. [Google Scholar] [CrossRef]
- Waldinger, M.D.; Quinn, P.; Dilleen, M.; Mundayat, R.; Schweitzer, D.H.; Boolell, M. A multinational population survey of intravaginal ejaculation latency time. J. Sex. Med. 2005, 2, 492–497. [Google Scholar] [CrossRef]
- Patrick, D.L.; Giuliano, F.; Ho, K.F.; Gagnon, D.D.; McNulty, P.; Rothman, M. The premature ejaculation profile: Validation of self-reported outcome measures for research and practice. BJU Int. 2009, 103, 358–364. [Google Scholar] [CrossRef]
- Symonds, T.; Perelman, M.; Althof, S.; Giuliano, F.; Martin, M.; Abraham, L.; Crossland, A.; Morris, M.; May, K. Further evidence of the reliability and validity of the premature ejaculation diagnostic tool. Int. J. Impot. Res. 2007, 19, 521–525. [Google Scholar] [CrossRef]
- Arafa, M.; Shamloul, R. Development and evaluation of the Arabic index of premature ejaculation (AIPE). J. Sex. Med. 2007, 4, 1750–1756. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Y.M.; Xin, Z.C.; Jiang, H.; Guo, Y.J.; Liu, W.J.; Tian, L.; Zhu, J.C. Sexual function of premature ejaculation patients assayed with Chinese Index of Premature Ejaculation. Asian J. Androl. 2004, 6, 121–126. [Google Scholar] [PubMed]
- Rosen, R.C.; Catania, J.A.; Althof, S.E.; Pollack, L.M.; O’Leary, M.; Seftel, A.D.; Coon, D.W. Development and validation of four-item version of Male Sexual Health Questionnaire to assess ejaculatory dysfunction. Urology 2007, 69, 805–809. [Google Scholar] [CrossRef] [PubMed]
- Jern, P.; Piha, J.; Santtila, P. Validation of three early ejaculation diagnostic tools: A composite measure is accurate and more adequate for diagnosis by updated diagnostic criteria. PLoS ONE 2013, 8, e77676. [Google Scholar] [CrossRef]
- Althof, S.E. Patient reported outcomes in the assessment of premature ejaculation. Transl. Androl. Urol. 2016, 5, 470–474. [Google Scholar] [CrossRef]
- Jefferys, A.; Siassakos, D.; Wardle, P. The management of retrograde ejaculation: A systematic review and update. Fertil. Steril. 2012, 97, 306–312.e6. [Google Scholar] [CrossRef]
- Kendirci, M.; Hellstrom, W.J.G. Retrograde ejaculation: Etiology, diagnosis, and management. Curr. Sex. Health Rep. 2006, 3, 133–138. [Google Scholar] [CrossRef]
- Jenkins, L.C.; Mulhall, J.P. Delayed orgasm and anorgasmia. Fertil. Steril. 2015, 104, 1082–1088. [Google Scholar] [CrossRef]
- Nguyen, V.; Dolendo, I.; Uloko, M.; Hsieh, T.C.; Patel, D. Male delayed orgasm and anorgasmia: A practical guide for sexual medicine providers. Int. J. Impot. Res. 2023; online ahead of print. [Google Scholar] [CrossRef]
- Gray, M.; Zillioux, J.; Khourdaji, I.; Smith, R.P. Contemporary management of ejaculatory dysfunction. Transl. Androl. Urol. 2018, 7, 686–702. [Google Scholar] [CrossRef]
- Mohee, A.; Eardley, I. Medical therapy for premature ejaculation. Ther. Adv. Urol. 2011, 3, 211–222. [Google Scholar] [CrossRef]
- Mcmahon, C.G. Management of ejaculatory dysfunction. Intern. Med. J. 2014, 44, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Sin, V.J.-E.; Anand, G.S.; Koh, H.-L. Botanical medicine and natural products used for erectile dysfunction. Sex. Med. Rev. 2021, 9, 568–592. [Google Scholar] [CrossRef] [PubMed]
- Malviya, N.; Jain, S.; Gupta, V.B.; Vyas, S. Recent studies on aphrodisiac herbs for the management of male sexual dysfunction—A review. Acta Pol. Pharm.-Drug Res. 2011, 68, 3–8. [Google Scholar]
- Bella, A.J.; Shamloul, R. Traditional Plant Aphrodisiacs and Male Sexual Dysfunction. Phyther. Res. 2014, 28, 831–835. [Google Scholar] [CrossRef] [PubMed]
- Leisegang, K.; Finelli, R. Alternative medicine and herbal remedies in the treatment of erectile dysfunction: A systematic review. Arab. J. Urol. 2021, 19, 323–339. [Google Scholar] [CrossRef]
- Sen, G.; Akbulut, S.; Karaköse, M. Ethnopharmacological study of medicinal plants in Kastamonu province (Türkiye). Open Chem. 2022, 20, 873–911. [Google Scholar] [CrossRef]
- Karaköse, M. An ethnobotanical study of medicinal plants in Güce district, north-eastern Turkey. Plant Divers. 2022, 44, 577–597. [Google Scholar] [CrossRef]
- Akbulut, S.; Karaköse, M.; Şen, G. Medicinal plants used in folk medicine of Akçaabat district (Turkey). Fresenius Environ. Bull. 2022, 31, 7160–7176. [Google Scholar]
- WHO Traditional Medicine Strategy: 2014–2023. Available online: https://www.who.int/publications/i/item/9789241506096 (accessed on 3 July 2023).
- Susan Wieland, L.; Manheimer, E.; Berman, B.M. Development and classification of an operational definition of complementary and alternative medicine for the Cochrane Collaboration. Altern. Ther. Health Med. 2011, 17, 50–59. [Google Scholar]
- Ng, J.Y.; Dhawan, T.; Dogadova, E.; Taghi-Zada, Z.; Vacca, A.; Wieland, L.S.; Moher, D. Operational definition of complementary, alternative, and integrative medicine derived from a systematic search. BMC Complement. Med. Ther. 2022, 22, 104. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- McMahon, C.G.; McMahon, C.N.; Leow, L.J. New agents in the treatment of premature ejaculation. Neuropsychiatr. Dis. Treat. 2006, 2, 489. [Google Scholar] [CrossRef] [PubMed]
- Attia, A.A.; Amer, M.A.E.; Elmezayen, M.M. The role of vitamin D supplementation in lifelong premature ejaculation. Int. J. Health Sci. 2022, 6, 2223–2233. [Google Scholar] [CrossRef]
- Mirone, V.; Arcaniolo, D.; Rivas, D.; Bull, S.; Aquilina, J.W.; Verze, P. Results from a prospective observational study of men with premature ejaculation treated with dapoxetine or alternative care: The PAUSE study. Eur. Urol. 2014, 65, 733–739. [Google Scholar] [CrossRef]
- Pettitt, G.A. Retarded ejaculation: Adjunctive treatment by hypnotically induced dreams in the context of sex therapy. Aust. J. Clin. Exp. Hypn. 1982, 10, 89–98. [Google Scholar]
- Yin, T.L.; Yang, J.; Zhang, B.; Yan, W.J.; Xu, W.M.; Li, W.; Yu, L.; Li, S.J.; Wu, G.X. Folic acid supplementation as adjunctive treatment premature ejaculation. Med. Hypotheses 2011, 76, 414–416. [Google Scholar] [CrossRef]
- Zhang, Q.; Wu, W.C.; Wu, J.Z.; Zhou, R.L.; Yan, C.H.; Yin, F.X.; Guo, Z.H.; Zhu, L.X. Ejaculatio deficiens treated with acupuncture. Report of 110 cases. J. Tradit. Chin. Med. 1984, 4, 181–182. [Google Scholar]
- Xiao, Y. Treatment of functional retrograde ejaculation with acupuncture and TCM herbal drugs. J. Tradit. Chin. Med. 2002, 22, 286–287. [Google Scholar]
- Shinghal, R.; Barnes, A.; Mahar, K.M.; Stier, B.; Giancaterino, L.; Condreay, L.D.; Black, L.; Mccallum, S.W. Safety and efficacy of epelsiban in the treatment of men with premature ejaculation: A randomized, double-blind, placebo-controlled, fixed-dose study. J. Sex. Med. 2013, 10, 2506–2517. [Google Scholar] [CrossRef]
- El Najjar, M.R.; El Hariri, M.; Ramadan, A.; Hefny Hashem, A.A. A double blind, placebo controlled, randomized trial to evaluate the efficacy and tolerability of on-demand oral Pregablin (150 mg and 75 mg) in treatment of premature ejaculation. J. Sex. Med. 2020, 17, 442–446. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Tafuri, A.; Bettica, P.; Ziviani, L.; Lund, J.; Poggesi, I.; Marcer, A.; Cacciamani, G.E.; Lorenzo-Gomez, M.F.; Porcaro, A.B.; et al. A double-blind, placebo-controlled parallel group study to evaluate the effect of a single oral dose of 5-HT1A antagonist GSK958108 on ejaculation latency time in male patients suffering from premature ejaculation. J. Sex. Med. 2021, 18, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.C.; Lin, M.C.; Cheng, C.J. A new sperm collection method for treatment of retrograde ejaculation. J. Formos. Med. Assoc. 1990, 89, 484–486. [Google Scholar] [PubMed]
- Salonia, A.; Maga, T.; Colombo, R.; Scattoni, V.; Briganti, A.; Cestari, A.; Guazzoni, G.; Rigatti, P.; Montorsi, F. A prospective study comparing paroxetine alone versus paroxetine plus sildenafil in patients with premature ejaculation. J. Urol. 2002, 168, 2486–2489. [Google Scholar] [CrossRef]
- Littara, A.; Palmieri, B.; Rottigni, V.; Iannitti, T. A clinical study to assess the effectiveness of a hyaluronic acid-based procedure for treatment of premature ejaculation. Int. J. Impot. Res. 2013, 25, 117–120. [Google Scholar] [CrossRef]
- Xin, Z.C.; Choi, Y.D.; Seong, D.H.; Choi, H.K. Sensory evoked potential and effect of SS-cream in premature ejaculation. Yonsei Med. J. 1995, 36, 397–401. [Google Scholar] [CrossRef]
- Xin, Z.C.; Choi, Y.D.; Lee, W.H.; Choi, Y.J.; Yang, W.J.; Choi, H.K.; Kim, D.K. Penile vibratory threshold changes with various doses of SS-cream in patients with primary premature ejaculation. Yonsei Med. J. 2000, 41, 29–33. [Google Scholar] [CrossRef]
- Ma, G.C.; Zou, Z.J.; Lai, Y.F.; Zhang, X.; Zhang, Y. Regular penis-root masturbation, a novel behavioral therapy in the treatment of primary premature ejaculation. Asian J. Androl. 2019, 21, 631. [Google Scholar]
- Pryor, J.L.; LeRoy, S.C.; Nagel, T.C.; Hensleigh, H.C. Vibratory stimulation for treatment of anejaculation in quadriplegic men. Arch. Phys. Med. Rehabil. 1995, 76, 59–64. [Google Scholar] [CrossRef]
- Cai, T.; Verze, P.; Massenio, P.; Tiscione, D.; Malossini, G.; Cormio, L.; Carrieri, G.; Mirone, V. Rhodiola rosea, folic acid, zinc and biotin (EndEP ®) is able to improve ejaculatory control in patients affected by lifelong premature ejaculation: Results from a phase I-II study. Exp. Ther. Med. 2016, 12, 2083–2087. [Google Scholar] [CrossRef]
- Kulkarni, M.P.; Shinde, B.S.; Chaudhari, M.K.V.; Avhad, G.M.; Pensalwar, S.V.; Prasad, B.S.V.; Deshpande, M.K.M.; Rosenbloom, R.A. Efficacy and safety of two polyherbal combinations: E-MA-H and E-MA-HP in male sexual dysfunction. Am. J. Ther. 2011, 18, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Sansalone, S.; Leonardi, R.; Antonini, G.; Vitarelli, A.; Vespasiani, G.; Basic, D.; Morgia, G.; Cimino, S.; Russo, G.I. Alga Ecklonia bicyclis, Tribulus terrestris, and glucosamine oligosaccharide improve erectile function, sexual quality of life, and ejaculation function in patients with moderate mild-moderate erectile dysfunction: A prospective, randomized, placebo-contr. BioMed Res. Int. 2014, 2014, 12139. [Google Scholar] [CrossRef] [PubMed]
- McVary, K.T.; Gange, S.N.; Gittelman, M.C.; Goldberg, K.A.; Patel, K.; Shore, N.D.; Levin, R.M.; Rousseau, M.; Beahrs, J.R.; Kaminetsky, J.; et al. Erectile and ejaculatory function preserved with convective water vapor energy treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia: Randomized controlled study. J. Sex. Med. 2016, 13, 924–933. [Google Scholar] [CrossRef]
- Abdel-Hamid, I.A.; El Naggar, E.A.; El Gilany, A.H. Assessment of as needed use of pharmacotherapy and the pause-squeeze technique in premature ejaculation. Int. J. Impot. Res. 2001, 13, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Wang, F.; Zhou, Q.; Geng, Q.; Gao, Q.; Zhang, R.; Zhang, C.; Xuan, Z.; Cai, J.; Bin, B.; et al. Safety and efficacy of traditional Chinese medicine, Qiaoshao formula, combined with dapoxetine in the treatment of premature ejaculation: An open-label, real-life, retrospective multicentre study in Chinese men. Andrologia 2021, 53, e13915. [Google Scholar] [CrossRef]
- Dhikav, V.; Karmarkar, G.; Gupta, M.; Anand, K.S. Yoga in premature ejaculation: A comparative trial with fluoxetine. J. Sex. Med. 2007, 4, 1726–1732. [Google Scholar] [CrossRef]
- Kilinc, M.F.; Aydogmus, Y.; Yildiz, Y.; Doluoglu, O.G. Impact of physical activity on patient self-reported outcomes of lifelong premature ejaculation patients: Results of a prospective, randomised, sham-controlled trial. Andrologia 2018, 50, e12799. [Google Scholar] [CrossRef]
- Pastore, A.L.; Palleschi, G.; Leto, A.; Pacini, L.; Iori, F.; Leonardo, C.; Carbone, A. A prospective randomized study to compare pelvic floor rehabilitation and dapoxetine for treatment of lifelong premature ejaculation. Int. J. Androl. 2012, 35, 528–533. [Google Scholar] [CrossRef]
- Optale, G.; Burigat, S.; Chittaro, L.; Riva, G. Smartphone-based therapeutic exercises for men affected by premature ejaculation: A pilot study. Sex. Med. 2020, 8, 461–471. [Google Scholar] [CrossRef]
- Jiang, M.; Yan, G.; Deng, H.; Liang, H.; Lin, Y.; Zhang, X. The efficacy of regular penis-root masturbation, versus Kegel exercise in the treatment of primary premature ejaculation: A quasi-randomised controlled trial. Andrologia 2020, 52, e13473. [Google Scholar] [CrossRef]
- Rodríguez, J.E.; Marzo, J.C.; Piqueras, J.A. Efficacy of Sphincter Control Training (SCT) in the treatment of premature ejaculation, a new cognitive behavioral approach: A parallel-group randomized, controlled trial. PLoS ONE 2019, 14, e0212274. [Google Scholar] [CrossRef] [PubMed]
- Ventus, D.; Gunst, A.; Arver, S.; Dhejne, C.; Öberg, K.G.; Zamore-Söderström, E.; Kärnä, A.; Jern, P. Vibrator-assisted start–stop exercises improve premature ejaculation symptoms: A randomized controlled trial. Arch. Sex. Behav. 2020, 49, 1559–1573. [Google Scholar] [CrossRef] [PubMed]
- Asgari, S.A.; Falahatkar, S.; Sharifi, S.H.H.; Enshaei, A.; Jalili, M.F.; Allahkhah, A. Safety and efficacy of the herbal drug hypericum perforatum for the treatment of premature ejaculation. UroToday Int. J. 2010, 3. [Google Scholar] [CrossRef]
- Sansalone, S.; Russo, G.I.; Mondaini, N.; Cantiello, F.; Antonini, G.; Cai, T. A combination of tryptophan, Satureja montana, Tribulus terrestris, Phyllanthus emblica extracts is able to improve sexual quality of life in patient with premature ejaculation. Arch. Ital. Urol. Androl. 2016, 88, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Panda, S.K.; Nirvanashetty, S.; Parachur, V.A.; Mohanty, N. A randomized double-blind placebo-control study to assess the efficacy and safety of OLNP-05 versus placebo for the treatment of subjects with premature ejaculation. J. Med. Food 2020, 23, 1006–1013. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Gao, Q.-H.; Wang, F.; Yu, G.-J.; Zhang, J.-W.; Zeng, Y.; Geng, Q.; Guo, B.-D.; Han, Q. Efficacy and safety of Qiaoshao Formula on patients with lifelong premature ejaculation of Gan (Liver) depression and Shen (Kidney) deficiency syndrome: A randomized controlled trial. Chin. J. Integr. Med. 2016, 22, 889–893. [Google Scholar] [CrossRef]
- Song, G.H.; Halmurat, C.; Feng, L.C.; Yilihamujiang, S.; Ma, C.; Liu, J. Clinical study on the treatment of premature ejaculation by Uighur medicine gu-jing-mai-si-ha tablet. Chin. J. Integr. Med. 2007, 13, 185–189. [Google Scholar] [CrossRef]
- Cui, Y.D.; Hu, S.-B.; Wu, B.; Li, S.J.; Xiang, K.; Liao, Z.L.; Zhang, H.P.; Zhu, C.H.; Rao, M. Efficacy of combined traditional Chinese medicine spray with premature ejaculation desensitization therapy for the treatment of primary premature ejaculation. Afr. Health Sci. 2017, 17, 603–613. [Google Scholar] [CrossRef]
- Choi, H.K.; Xin, Z.C.; Choi, Y.D.; Lee, W.H.; Mah, S.Y.; Kim, D.K. Safety and efficacy study with various doses of SS-cream in patients with premature ejaculation in a double-blind, randomized, placebo controlled clinical study. Int. J. Impot. Res. 1999, 11, 261–264. [Google Scholar] [CrossRef]
- Choi, H.K.; Jung, G.W.; Moon, K.H.; Xin, Z.C.; Choi, Y.D.; Lee, W.H.; Rha, K.H.; Choi, Y.J.; Kim, D.K. Clinical study of SS-cream in patients with lifelong premature ejaculation. Urology 2000, 55, 257–261. [Google Scholar] [CrossRef]
- Moosavi-Asil, S.H.; Ahmadian-Attari, M.M.; Shirzad, M.; Yekaninejad, M.S.; Nikoobakht, M.R.; Karimi, M. Effect of a topical polyherbal formulation for premature ejaculation: A randomized triple-blind placebo-controlled trial. Adv. Integr. Med. 2021, 8, 210–215. [Google Scholar] [CrossRef]
- Sunay, D.; Sunay, M.; Aydoǧmuş, Y.; Baǧbanci, S.; Arslan, H.; Karabulut, A.; Emir, L. Acupuncture versus paroxetine for the treatment of premature ejaculation: A randomized, placebo-controlled clinical trial. Eur. Urol. 2011, 59, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Han, H.; Zhang, Z.; Chen, H.; Huang, X.; Zhang, R. Study on the efficacy of electric acupuncture in the treatment of premature ejaculation based on testosterone level. J. Healthc. Eng. 2022, 2022, 8331688. [Google Scholar] [CrossRef] [PubMed]
- Sahin, S.; Bicer, M.; Yenice, M.G.; Seker, K.G.; Yavuzsan, A.H.; Tugcu, V. A prospective randomized controlled study to compare acupuncture and dapoxetine for the treatment of premature ejaculation. Urol. Int. 2016, 97, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Nagao, K.; Tai, T.; Kobayashi, H.; Nakajima, K. Randomized crossover trial of amoxapine versus vitamin B12 for retrograde ejaculation. Int. Braz. J. Urol. 2017, 43, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Alahwany, A.; Ragab, M.W.; Zaghloul, A.; Abdallah, H.; Mostafa, T. Hyaluronic acid injection in glans penis for treatment of premature ejaculation: A randomized controlled cross-over study. Int. J. Impot. Res. 2019, 31, 348–355. [Google Scholar] [CrossRef]
- Micoogullari, U.; Kisa, E.; Celik, O.; Furkan Erbay, O.; Koc, E.; Gok, B. Nueva terapia conductual en el tratamiento de la eyaculación precoz adquirida: Un estudio comparativo de escuchar música. Arch. Esp. Urol. 2021, 74, 519–525. [Google Scholar]
- Cooper, K.; Martyn-St James, M.; Kaltenthaler, E.; Dickinson, K.; Cantrell, A.; Ren, S.; Wylie, K.; Frodsham, L.; Hood, C. Complementary and alternative medicine for management of premature ejaculation: A systematic review. Sex. Med. 2017, 5, e1–e18. [Google Scholar] [CrossRef]
- Xu, J.X.; Gao, G.; Xu, N.; Yang, Y.Y. Yimusake alone or combined with trazodone hydrochloride for primary premature ejaculation. Zhonghua Nan Ke Xue 2012, 18, 376–378. [Google Scholar]
- Chen, Z.X. Control study on acupuncture and medication for treatment of primary simple premature ejaculation. Zhongguo Zhen Jiu 2009, 29, 13–15. [Google Scholar]
- Xu, G.; Jiang, H.W.; Fang, J.; Wen, H.; Gu, B.; Liu, J.; Zhang, L.M.; Ding, Q.; Zhang, Y.F. An improved dosage regimen of sertraline hydrochloride in the treatment for premature ejaculation: An 8-week, single-blind, randomized controlled study followed by a 4-week, open-label extension study. J. Clin. Pharm. Ther. 2014, 39, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Li, J.-X.; Lu, Q.-G. Efficacy of Qilin Pills combined with sertraline in the treatment of secondary non-consolidated kidney qi premature ejaculation. Zhonghua Nan Ke Xue 2015, 21, 443–446. [Google Scholar] [PubMed]
- Sun, Z.; Wang, Y.; Chen, L.; Jin, F. Clinical study on treatment of premature ejaculation with fluoxetine hydrochloride and tamsulosin. Chin. J. Androl. 2010, 24, 43–45. [Google Scholar]
- Kulkarni, P.; Chandola, H. Evaluation of Stambhanakaraka Yoga and counseling in the management of Shukragata Vata (premature ejaculation). AYU Int. Q. J. Res. Ayurveda 2013, 34, 42. [Google Scholar] [CrossRef]
- Cohen, D.; Gonzalez, J.; Goldstein, I. The role of pelvic floor muscles in male sexual dysfunction and pelvic pain. Sex. Med. Rev. 2016, 4, 53–62. [Google Scholar] [CrossRef]
- Rodas, M.C.; García-Perdomo, H.A. From Kegel exercises to pelvic floor rehabilitation: A physiotherapeutic perspective. Rev. Mex. Urol. 2018, 78, 402–411. [Google Scholar]
- Clarke, T.C.; Black, L.I.; Stussman, B.J.; Barnes, P.M.; Nahin, R.L. Trends in the use of complementary health approaches among adults: United States, 2002–2012. Natl. Health Stat. Report 2015, 79, 1–16. [Google Scholar]
- Park, C.L.; Braun, T.; Siegel, T. Who practices yoga? A systematic review of demographic, health-related, and psychosocial factors associated with yoga practice. J. Behav. Med. 2015, 38, 460–471. [Google Scholar] [CrossRef]
- Dhikav, V.; Karmarkar, G.; Verma, M.; Gupta, R.; Gupta, S.; Mittal, D.; Anand, K. Yoga in male sexual functioning: A noncompararive pilot study. J. Sex. Med. 2010, 7, 3460–3466. [Google Scholar] [CrossRef]
- Joshi, A.M.; Veettil, R.A.; Deshpande, S. Role of yoga in the management of premature ejaculation. World J. Mens. Health 2019, 37, 495. [Google Scholar] [CrossRef]
- Hofmann, S.G.; Andreoli, G.; Carpenter, J.K.; Curtiss, J. Effect of Hatha yoga on anxiety: A meta-analysis. J. Evid. Based. Med. 2016, 9, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Saeed, S.A.; Cunningham, K.; Bloch, R.M. Depression and anxiety disorders: Benefits of exercise, yoga, and meditation. Am. Fam. Physician 2019, 99, 620–627. [Google Scholar] [PubMed]
- Heinrich, M.; Anagnostou, S. From pharmacognosia to DNA-based medicinal plant authentication—Pharmacognosy through the centuries. Planta Med. 2017, 83, 1110–1116. [Google Scholar] [CrossRef]
- Kennedy, D.O.; Wightman, E.L. Herbal extracts and phytochemicals: Plant secondary metabolites and the enhancement of human brain function. Adv. Nutr. 2011, 2, 32–50. [Google Scholar] [CrossRef] [PubMed]
- Nobakht, S.Z.; Akaberi, M.; Mohammadpour, A.H.; Moghadam, A.T.; Emami, S.A. Hypericum perforatum: Traditional uses, clinical trials, and drug interactions. Iran. J. Basic Med. Sci. 2022, 26, 1045–1058. [Google Scholar]
- Ng, Q.X.; Venkatanarayanan, N.; Ho, C.Y.X. Clinical use of Hypericum perforatum (St John’s wort) in depression: A meta-analysis. J. Affect. Disord. 2017, 210, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, R.; Nikfar, S.; Abdollahi, M. Efficacy and tolerability of Hypericum perforatum in major depressive disorder in comparison with selective serotonin reuptake inhibitors: A meta-analysis. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2009, 33, 118–127. [Google Scholar] [CrossRef]
- Otunctemur, A.; Ozbek, E.; Kirecci, S.L.; Ozcan, L.; Dursun, M.; Cekmen, M.; Ozdogan, H.K. Relevance of serum nitric oxide levels and the efficacy of selective serotonin reuptake inhibitors treatment on premature ejaculation: Decreased nitric oxide is associated with premature ejaculation. Andrologia 2014, 46, 951–955. [Google Scholar] [CrossRef]
- Estienne, M.J.; Harper, A.F. Semen characteristics and libido in boars treated repeatedly with PGF 2α. J. Anim. Sci. 2004, 82, 1494–1498. [Google Scholar] [CrossRef]
- Alizadeh, F.; Rangzan, N.; Mohseni, M.; Hosseini, S. Serum testosterone and gonadotropins levels in patients with premature ejaculation: A comparison with normal men. Adv. Biomed. Res. 2014, 3, 6. [Google Scholar] [CrossRef]
- Zavatti, M.; Zanoli, P.; Benelli, A.; Rivasi, M.; Baraldi, C.; Baraldi, M. Experimental study on Satureja montana as a treatment for premature ejaculation. J. Ethnopharmacol. 2011, 133, 629–633. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Nair, V.; Gupta, Y.K. Evaluation of the aphrodisiac activity of Tribulus terrestris Linn. in sexually sluggish male albino rats. J. Pharmacol. Pharmacother. 2012, 3, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Wang, Q.; Du, Y.; Zhang, X. Network pharmacology-based strategy to investigate pharmacological mechanisms of Qiaoshao formula for treatment of premature ejaculation. Evid. Based Complement. Altern. Med. 2020, 2020, 1418634. [Google Scholar] [CrossRef] [PubMed]
- Xin, Z.C.; Choi, Y.D.; Lee, S.H.; Choi, H.K. Efficacy of a topical agent SS-cream in the treatment of premature ejaculation: Preliminary clinical studies. Yonsei Med. J. 1997, 38, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Xin, Z.C.; Choi, Y.D.; Choi, H.K. The effects of SS-cream and its individual components on rabbit corpus cavernosal muscles. Yonsei Med. J. 1996, 37, 312–318. [Google Scholar] [CrossRef]
- Patil, S.; Sen, S.; Bral, M.; Reddy, S.; Bradley, K.K.; Cornett, E.M.; Fox, C.J.; Kaye, A.D. The role of acupuncture in pain management. Curr. Pain Headache Rep. 2016, 20, 22. [Google Scholar] [CrossRef] [PubMed]
- Linde, K.; Vickers, A.; Hondras, M.; ter Riet, G.; Thormählen, J.; Berman, B.; Melchart, D. Systematic reviews of complementary therapies—An annotated bibliography. Part 1: Acupuncture. BMC Complement. Altern. Med. 2001, 1, 3. [Google Scholar] [CrossRef]
- Ma, S.X.; Lee, P.C.; Jiang, I.; Ma, E.; Hu, J.S.; Li, X.Y. Influence of age, gender, and race on nitric oxide release over acupuncture points-meridians. Sci. Rep. 2015, 5, 17547. [Google Scholar] [CrossRef]
- Lin, J.-G.; Kotha, P.; Chen, Y.-H. Understandings of acupuncture application and mechanisms. Am. J. Transl. Res. 2022, 14, 1469–1481. [Google Scholar]
- Zhao, Z.Q. Neural mechanism underlying acupuncture analgesia. Prog. Neurobiol. 2008, 85, 355–375. [Google Scholar] [CrossRef]
- Lee, E.J.; Warden, S. The effects of acupuncture on serotonin metabolism. Eur. J. Integr. Med. 2016, 8, 355–367. [Google Scholar] [CrossRef]
- Ma, S.-x. Nitric oxide signaling molecules in acupoints: Toward mechanisms of acupuncture. Chin. J. Integr. Med. 2017, 23, 812–815. [Google Scholar] [CrossRef] [PubMed]
- Calderón-Ospina, C.A.; Nava-Mesa, M.O. B Vitamins in the nervous system: Current knowledge of the biochemical modes of action and synergies of thiamine, pyridoxine, and cobalamin. CNS Neurosci. Ther. 2020, 26, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Abatangelo, G.; Vindigni, V.; Avruscio, G.; Pandis, L.; Brun, P. Hyaluronic acid: Redefining its role. Cells 2020, 9, 1743. [Google Scholar] [CrossRef] [PubMed]
- Sze, J.H.; Brownlie, J.C.; Love, C.A. Biotechnological production of hyaluronic acid: A mini review. 3 Biotech 2016, 6, 67. [Google Scholar] [CrossRef]
- Zucchi, A.; Scroppo, F.I.; Capogrosso, P.; Salonia, A.; Duante, J.; Bini, V.; Liguori, G.; Bartoletti, R. Clinical use of hyaluronic acid in andrology: A review. Andrology 2022, 10, 42–50. [Google Scholar] [CrossRef]
- Kosseifi, F.; Chebbi, A.; Raad, N.; Ndayra, A.; El Samad, R.; Achkar, K.; Durand, X.; Noujeim, A. Glans penis augmentation using hyaluronic acid for the treatment of premature ejaculation: A narrative review. Transl. Androl. Urol. 2021, 9, 2814–2820. [Google Scholar] [CrossRef]
- Kwak, T.I.; Jin, M.H.; Kim, J.J.; Moon, D.G. Long-term effects of glans penis augmentation using injectable hyaluronic acid gel for premature ejaculation. Int. J. Impot. Res. 2008, 20, 425–428. [Google Scholar] [CrossRef]
- Kim, J.J.; Kwak, T.I.; Jeon, B.G.; Cheon, J.; Moon, D.G. Effects of glans penis augmentation using hyaluronic acid gel for premature ejaculation. Int. J. Impot. Res. 2004, 16, 547–551. [Google Scholar] [CrossRef]
- Abdallah, H.; Abdelnasser, T.; Hosny, H.; Selim, O.; Al-Ahwany, A.; Shamloul, R. Treatment of premature ejaculation by glans penis augmentation using hyaluronic acid gel: A pilot study. Andrologia 2012, 44, 650–653. [Google Scholar] [CrossRef]
- Shebl, S.E.; Ali, S.; Shokr, M. Hyaluronic acid injection in the glans penis for the treatment of refractory premature ejaculation: A prospective, controlled study. Andrologia 2021, 53, e14084. [Google Scholar] [CrossRef] [PubMed]
- de Witte, M.; Pinho, A.D.S.; Stams, G.J.; Moonen, X.; Bos, A.E.R.; van Hooren, S. Music therapy for stress reduction: A systematic review and meta-analysis. Health Psychol. Rev. 2022, 16, 134–159. [Google Scholar] [CrossRef] [PubMed]
- Shirani Bidabadi, S.; Mehryar, A. Music therapy as an adjunct to standard treatment for obsessive compulsive disorder and co-morbid anxiety and depression: A randomized clinical trial. J. Affect. Disord. 2015, 184, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Mu, X. Effects of the music therapy on the serotonin and tubulin in brain tissue of chronic unpredictable mild stress rats. Chin. J. Behav. Med. Brain Sci. 2014, 12, 531–533. [Google Scholar]


| Ref. | Study Design | Patient Cohort | Intervention (n) | Comparison (n) | Outcomes of Interest | Other Outcomes | Adverse Effects |
|---|---|---|---|---|---|---|---|
| Lifestyle, Exercise and/or Physical Therapy | |||||||
| Dhikav et al., 2007 [58] | Open-label control trial | PE patients | Yoga (2 pranayanams and 12 asnas) for 1 h daily for 12 weeks (n = 38) | Fluoxetine (20–60 mg) daily for 12 weeks (n = 30) |
| Fluoxetine induced nausea, vomiting, anxiety and insomnia in some patients | |
| Kilinc et al., 2018 [59] | RCT | LPE patients with IELT < 1 min and PEDT > 11 | Moderate physical activity (running > 30 min 5 days weekly) for 30 days. (n = 35) | Sedentary lifestyle with dapoxetine (30 mg) on demand for 30 days (n = 35) and minimal physical activity (walking < 30 min 5 days per week) for 30 days (n = 35) |
| Yawning, nausea, dizziness and headache were reported for 5 dapoxetine patients. | |
| Pastore et al., 2012 [60] | RCT | LPE with IELT < 1 min | PFM rehabilitation 60 min trice per week for 12 weeks (n = 19) | Dapoxetine 30 mg (n = 8) or 60 mg (n = 7) on demand for 12 weeks |
| Nausea and diarrhea reported in 4 dapoxetine patients | |
| Optale et al., 2020 [61] | RCT | LPE with IELT < 1 min | Mobile coaching application of physical and mental distancing exercises (10 min) 3 times a day for 3 months (n =17) | Verbal and printed instructions for physical and mental distancing exercises (10 min) 3 times a day for 3 months (n = 15) |
|
| Not reported |
| Jiang et al., 2020 [62] | RCT | Primary PE patients with IELT < 1 min for >1 year | PRM for 3 months (n = 18) | Kegel exercise for 3 months (n = 19) |
| None | |
| Rodríguez et al., 2019 [63] | Parallel RCT | PE patients with IELT of ≤2 min and PEDT of ≥11 | GWD for 7 weeks (n = 18) | GWtD for 7 weeks (n = 17) |
| None | |
| Ventus et al., 2020 [64] | RCT | Self-reported IELT < 3 min | VSS+ trice a week for 6 weeks. (n = 13) | VSS trice a week for 6 weeks (n = 12) and waiting list group control group (n = 5) |
|
| None |
| Herbal Medicine Supplements | |||||||
| Asgari et al., 2010 [65] | Double-blind RCT | PE patients with IELT < 2 min occurring >50% of coital attempts | Hypericum perforatum extract (150 mg containing 160 μg of hypericin) 3 times daily for 30 days (n = 22) | Placebo tablets 3 times daily for 30 days (n = 20) |
|
| Headache, constipation, photosensitivity and nausea were reported for Hypericum perforatum in 6 patients |
| Sansalone et al., 2016 [66] | Multi-center RCT | PE patients for ≥6 months and IELT of ≤2 min in >75% of coital attempts | EiacuMev® (300 mg) daily for 3 months (n = 63) | Counselling and sexual behavioral treatment for 3 months (n = 65) |
|
| Not reported |
| Panda et al., 2020 [67] | Single-center double-blind RCT | PE patients with IELT < 2 min and PEP ≥ 11 | OLNP-05 (450 mg) twice daily for 8 weeks (n = 29) | Placebo capsule twice daily for 8 weeks (n = 28) |
|
| Constipation, fatigue and fever in 3 patients treated with OLNP-05 and in 5 controls |
| Guo et al., 2016 [68] | RCT | LPE > year with IELT ≤ 0.5 and ≤2 min and IIEF-5 > 21 | QSF granules twice a day for 4 weeks (n = 29) | One bag of dapoxetine twice daily for 4 weeks (n = 30) |
|
| Slight discomfort in the stomach in 1 QSF patient; Dizziness and nausea in 5 controls |
| Song et al., 2007 [69] | RCT | PE patients with IELT < 2 min and partner satisfaction < 50% | Gu-jing-mai-si-ha (GJMSHT, Kanghabo Co., Ltd.) 4 tablets twice a day for 15 days (n = 35) | No drug (n = 33) |
|
| Not reported |
| Topical Herbal Applications | |||||||
| Cui et al., 2017 [70] | RCT | PE patients with IELT < 2 min and CIPE-5 < 18 | TCMS applied daily and 30 min before sexual intercourse and washed off before coitus for 6 weeks. (n = 29) | Desensitization Therapy (DT) 3 times per week for 6 weeks (n = 28) and combination of DT and TCMS for 6 weeks (n = 29) |
| Local burning sensation reported by some patients | |
| Choi et al., 1999 [71] | Double-blind RCT | Primary PE patients only with IELT < 3 min and Sexual Satisfaction Rate < 50% | Application of SS-Cream (0.05, 0.1, 0.15 and 0.2 g) on glans penis 1 h before intercourse, washing off before sexual intercourse | Placebo cream on the glans penis 1 h before intercourse, washing off before sexual intercourse |
|
| Local mild burning sensation (14%) |
| n = 50 patients in total taking each dose once for 250 test trials | |||||||
| Choi et al., 2000 [72] | Double-blind RCT | LPE patients with ejaculatory latency < 3 min and/or Sexual Satisfaction Rate < 30%. | Application of SS-Cream (0.2 g) on glans penis 1 h before intercourse, washing off before sexual intercourse | Placebo (not specified) on glans penis 1 h before intercourse, washing off before sexual intercourse |
|
| Mild local irritant symptoms including a sense of mild burning (n = 78), mild pain (n = 20), sporadic erectile dysfunction (n = 3), delayed ejaculation of more than 45 min (n = 4) and abrupt end of erectile response with failure to culminate with ejaculation (n = 5) |
| n = 106 patients taking each dose 5 times for 530 test trials + 106 test trials with a placebo | |||||||
| Moosavi-Asil et al., 2021 [73] | Triple-blind RCT | PE patients ≥ 6 months duration with IELT < 1 min, PEDT score > 11 and IIEF > 22 | Application of Polyherb Formula (0.25 cc) on the penis glans and shaft each night and 1 h before intercourse for 3 weeks (n = 30) | Application of placebo base oil (0.25 cc) on the penis glans and shaft each night and 1 h before intercourse for 3 weeks (n = 33) |
| Testicular pain (n = 1) and acute drug allergy (n = 1) that dropped out of the study | |
| Acupuncture or Acupressure | |||||||
| Sunay et al., 2011 [74] | RCT | PE patients with IELT of <2 min in >70% of coital attempts | Acupuncture twice per week for 4 weeks (n = 30) | Sham acupuncture twice per week for 4 weeks (n = 30) and 20 mg of paroxetine daily for 4 weeks (n = 30) |
| None | |
| Sahin et al., 2016 [76] | RCT | Self-reported LPE patients | Acupuncture twice for 4 weeks (n = 29) | Sham acupuncture twice for 4 weeks (n = 28) and dapoxetine 30 mg (n = 28) or 60 mg (n = 27) for 4 weeks |
| In the dapoxetine groups, nausea, dizziness, diarrhea, insomnia and headaches were reported No side-effects were reported in the acupuncture groups. | |
| Lu et al., 2022 [75] | RCT | Chinese medicine diagnosis for premature ejaculation | Electroacupuncture for 30 min once daily for 6 days, with 1 rest day, for 4 weeks (n = 25) | 300 mL of Longdan Xiegan daily for 4 weeks (n = 25) |
|
| Dizziness (n = 2) and subcutaneous hematoma (n = 3) in the electroacupuncture group Malady (n = 6), stomach discomfort (n = 4), mild diarrhea (n = 1) and dizziness (n = 1) in the controls |
| Vitamin, Mineral and/or Nutraceutical Supplements | |||||||
| Hu et al., 2017 [77] | Open-label, randomized, crossover study | RE patients | Amoxapine (Pfizer, Japan) group, 50 mg daily for 4 weeks; After 1-week washout period, patients took 1500 µg of vit B12 for 4 weeks (n = 13) | Vit B12, 1500 µg for 4 weeks; After a 1-week washout period, controls took 50 mg of amoxapine daily for 4 weeks. (n = 12) |
| Amoxapine-treated patients reported sleepiness (n = 1) and constipation (n = 2); No adverse events Reported for vit B12 | |
| Hyaluronic Penile Injections | |||||||
| Alahwany et al., 2019 [78] | Crossover RCT | PE patients with IELT < 1 min for LPE and <3 min | 2 mL HA (25 mg/mL) into glans penis (6 injections at coronal level and 4 injections at urethral meatus) with evaluation at 1 week and 1 month; 18 months wash out, followed by crossover with saline injection (n = 15) | 2 mL saline injection into glans penis (6 injections at coronal level and 4 injections at urethral meatus) with evaluation at 1 week and 1 month; 1 month wash out period, followed by crossover with HA injection (n = 15) |
| HA injection reported gradually decreasing local discomfort at the injection site (n = 3), glans penis ecchymosis (n = 2) and irregular blanched papule (n = 1). Saline injection reported injection site ecchymosis (n = 1). No adverse effects 1 month following injection. | |
| Music Therapy | |||||||
| Micoogullari et al., 2021 [79] | RCT | PE patients | Music therapy (the patient decided the type) for 45 min before the sexual intercourse for 60 days (n = 60) | Dapoxetine (30 mg) daily for 60 days (n = 60) |
|
| Not reported |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leisegang, K.; Opuwari, C.S.; Moichela, F.; Finelli, R. Traditional, Complementary and Alternative Medicines in the Treatment of Ejaculatory Disorders: A Systematic Review. Medicina 2023, 59, 1607. https://doi.org/10.3390/medicina59091607
Leisegang K, Opuwari CS, Moichela F, Finelli R. Traditional, Complementary and Alternative Medicines in the Treatment of Ejaculatory Disorders: A Systematic Review. Medicina. 2023; 59(9):1607. https://doi.org/10.3390/medicina59091607
Chicago/Turabian StyleLeisegang, Kristian, Chinyerum Sylvia Opuwari, Faith Moichela, and Renata Finelli. 2023. "Traditional, Complementary and Alternative Medicines in the Treatment of Ejaculatory Disorders: A Systematic Review" Medicina 59, no. 9: 1607. https://doi.org/10.3390/medicina59091607