Effectiveness of a Dual-Task Intervention Involving Exercise and Vocalized Cognitive Tasks
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
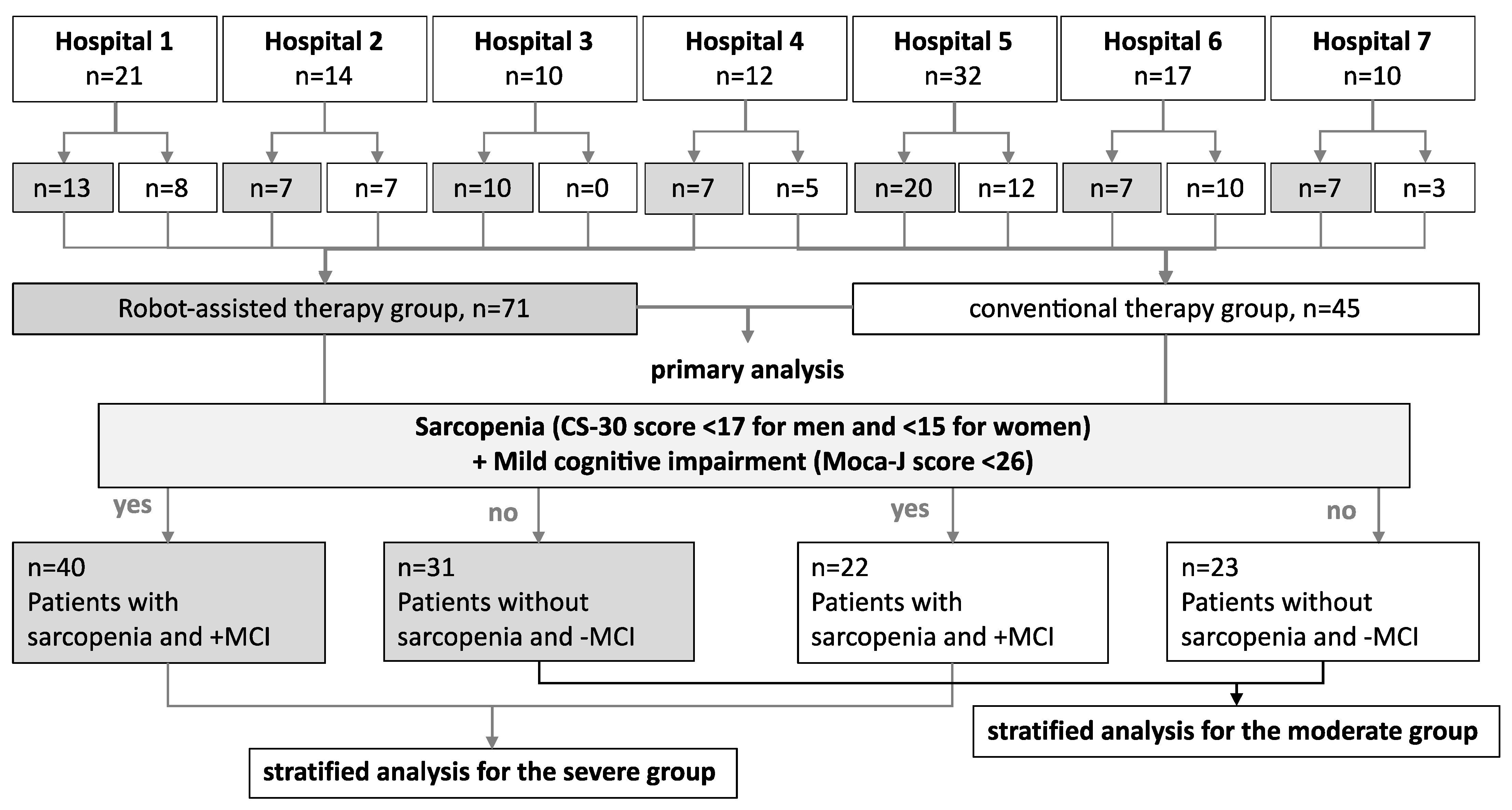
2.2. Participants
2.3. “Robot-Assisted” and Conventional Therapy Programs
2.4. Variables and Timing
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
3.1. Participants
3.2. Descriptive Data
3.3. Outcome Data
3.4. Effects of the Interventions on the Lower-Limb Function
3.5. Effects of the Interventions on the Cognitive Function
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Director-General for Statistics, Information System Management and Industrial Relations Ministry of Health, Labour and Welfare Government of Japan. Abridged Life Tables for Japan 2022; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2022; pp. 1–9.
- Ministry of Health, Labour and Welfare. Vital Statistics; e-Stat: Tokyo, Japan, 2021.
- Myers, J.; Prakash, M.; Froelicher, V.; Do, D.; Partington, S.; Atwood, J.E. Exercise capacity and mortality among men referred for exercise testing. N. Engl. J. Med. 2002, 346, 793–801. [Google Scholar] [CrossRef] [PubMed]
- Gates, N.; Fiatarone Singh, M.A.; Sachdev, P.S.; Valenzuela, M. The effect of exercise training on cognitive function in older adults with mild cognitive impairment: A meta-analysis of randomized controlled trials. Am. J. Geriatr. Psychiatry 2013, 21, 1086–1097. [Google Scholar] [CrossRef] [PubMed]
- Venturelli, M.; Scarsini, R.; Schena, F. Six-month walking program changes cognitive and ADL performance in patients with Alzheimer. Am. J. Alzheimers Dis. Other Demen. 2011, 26, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Yuan, F.; Klavon, E.; Liu, Z.; Lopez, R.P.; Zhao, X. A Systematic Review of Robotic Rehabilitation for Cognitive Training. Front. Robot AI 2021, 8, 605715. [Google Scholar] [CrossRef] [PubMed]
- Barnes, D.E.; Mehling, W.; Wu, E.; Beristianos, M.; Yaffe, K.; Skultety, K.; Chesney, M.A. Preventing loss of independence through exercise (PLIE): A pilot clinical trial in older adults with dementia. PLoS ONE 2015, 10, e0113367. [Google Scholar] [CrossRef] [PubMed]
- Jardim, N.Y.V.; Bento-Torres, N.V.O.; Costa, V.O.; Carvalho, J.P.R.; Pontes, H.T.S.; Tomas, A.M.; Sosthenes, M.C.K.; Erickson, K.I.; Bento-Torres, J.; Diniz, C.W.P. Dual-Task Exercise to Improve Cognition and Functional Capacity of Healthy Older Adults. Front. Aging Neurosci. 2021, 13, 589299. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988; p. 567. [Google Scholar]
- Sawada, S.; Ozaki, H.; Natsume, T.; Deng, P.; Yoshihara, T.; Nakagata, T.; Osawa, T.; Ishihara, Y.; Kitada, T.; Kimura, K.; et al. The 30-s chair stand test can be a useful tool for screening sarcopenia in elderly Japanese participants. BMC Musculoskelet. Disord. 2021, 22, 639. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 601. [Google Scholar] [CrossRef]
- Fujiwara, Y.; Suzuki, H.; Yasunaga, M.; Sugiyama, M.; Ijuin, M.; Sakuma, N.; Inagaki, H.; Iwasa, H.; Ura, C.; Yatomi, N.; et al. Brief screening tool for mild cognitive impairment in older Japanese: Validation of the Japanese version of the Montreal Cognitive Assessment. Geriatr. Gerontol. Int. 2010, 10, 225–232. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bedirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Zanini, A.; Crisafulli, E.; D’Andria, M.; Gregorini, C.; Cherubino, F.; Zampogna, E.; Azzola, A.; Spanevello, A.; Schiavone, N.; Chetta, A. Minimum Clinically Important Difference in 30-s Sit-to-Stand Test After Pulmonary Rehabilitation in Subjects with COPD. Respir. Care 2019, 64, 1261–1269. [Google Scholar] [CrossRef]
- Wright, A.A.; Cook, C.E.; Baxter, G.D.; Dockerty, J.D.; Abbott, J.H. A comparison of 3 methodological approaches to defining major clinically important improvement of 4 performance measures in patients with hip osteoarthritis. J. Orthop Sports Phys. Ther. 2011, 41, 319–327. [Google Scholar] [CrossRef]
- Wu, C.Y.; Hung, S.J.; Lin, K.C.; Chen, K.H.; Chen, P.; Tsay, P.K. Responsiveness, Minimal Clinically Important Difference, and Validity of the MoCA in Stroke Rehabilitation. Occup. Ther. Int. 2019, 2019, 2517658. [Google Scholar] [CrossRef]
- Forte, R.; Trentin, C.; Tocci, N.; Lucia, S.; Aydin, M.; Di Russo, F. Motor-cognitive exercise with variability of practice and feedback improves functional ability and cognition in older individuals. Aging Clin. Exp. Res. 2023, 35, 2797–2806. [Google Scholar] [CrossRef]
- Chen, I.C.; Chuang, I.C.; Chang, K.C.; Chang, C.H.; Wu, C.Y. Dual task measures in older adults with and without cognitive impairment: Response to simultaneous cognitive-exercise training and minimal clinically important difference estimates. BMC Geriatr. 2023, 23, 663. [Google Scholar] [CrossRef]
- van het Reve, E.; de Bruin, E.D. Strength-balance supplemented with computerized cognitive training to improve dual task gait and divided attention in older adults: A multicenter randomized-controlled trial. BMC Geriatr. 2014, 14, 134. [Google Scholar] [CrossRef]
- Adcock, M.; Sonder, F.; Schattin, A.; Gennaro, F.; de Bruin, E.D. A usability study of a multicomponent video game-based training for older adults. Eur. Rev. Aging Phys. Act. 2020, 17, 3. [Google Scholar] [CrossRef]
- Azadian, E.; Torbati, H.R.; Kakhki, A.R.; Farahpour, N. The effect of dual task and executive training on pattern of gait in older adults with balance impairment: A Randomized controlled trial. Arch. Gerontol. Geriatr. 2016, 62, 83–89. [Google Scholar] [CrossRef]
- Bayouk, J.F.; Boucher, J.P.; Leroux, A. Balance training following stroke: Effects of task-oriented exercises with and without altered sensory input. Int. J. Rehabil. Res. 2006, 29, 51–59. [Google Scholar] [CrossRef]
- Begde, A.; Alqurafi, A.; Pain, M.T.G.; Blenkinsop, G.; Wilcockson, T.D.W.; Hogervorst, E. The Effectiveness of Home-Based Exergames Training on Cognition and Balance in Older Adults: A Comparative Quasi-Randomized Study of Two Exergame Interventions. Innov. Aging 2023, 7, igad102. [Google Scholar] [CrossRef]
- Hong, X.L.; Cheng, L.J.; Feng, R.C.; Goh, J.; Gyanwali, B.; Itoh, S.; Tam, W.S.W.; Wu, X.V. Effect of physio-cognitive dual-task training on cognition in pre-ageing and older adults with neurocognitive disorders: A meta-analysis and meta-regression of randomized controlled trial. Arch. Gerontol. Geriatr. 2024, 116, 105161. [Google Scholar] [CrossRef]
- Li, F.; Harmer, P.; Eckstrom, E.; Fitzgerald, K.; Winters-Stone, K. Clinical Effectiveness of Cognitively Enhanced Tai Ji Quan Training on Global Cognition and Dual-Task Performance During Walking in Older Adults With Mild Cognitive Impairment or Self-Reported Memory Concerns: A Randomized Controlled Trial. Ann. Intern. Med. 2023, 176, 1498–1507. [Google Scholar] [CrossRef]
- Kramer, A.F.; Larish, J.F.; Strayer, D.L. Training for attentional control in dual task settings: A comparison of young and old adults. J. Exp. Psychol. Appl. 1995, 1, 50–76. [Google Scholar] [CrossRef]
- Patelaki, E.; Foxe, J.J.; Mantel, E.P.; Kassis, G.; Freedman, E.G. Paradoxical improvement of cognitive control in older adults under dual-task walking conditions is associated with more flexible reallocation of neural resources: A Mobile Brain-Body Imaging (MoBI) study. Neuroimage 2023, 273, 120098. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Spagna, A.; Mackie, M.A.; Fan, J. Resource sharing in cognitive control: Behavioral evidence and neural substrates. Neuroimage 2023, 273, 120084. [Google Scholar] [CrossRef]
- Lundin-Olsson, L.; Nyberg, L.; Gustafson, Y. “Stops walking when talking” as a predictor of falls in elderly people. Lancet. 1997, 349, 617. [Google Scholar] [CrossRef]
- Beauchet, O.; Annweiler, C.; Allali, G.; Berrut, G.; Dubost, V. Dual task-related changes in gait performance in older adults: A new way of predicting recurrent falls? J. Am. Geriatr. Soc. 2008, 56, 181–182. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, A.F.; Olsson, E.; Wahlund, L.O. Effect of divided attention on gait in subjects with and without cognitive impairment. J. Geriatr. Psychiatry Neurol. 2007, 20, 58–62. [Google Scholar] [CrossRef]
- Manckoundia, P.; Pfitzenmeyer, P.; d’Athis, P.; Dubost, V.; Mourey, F. Impact of cognitive task on the posture of elderly subjects with Alzheimer’s disease compared to healthy elderly subjects. Mov. Disord. 2006, 21, 236–241. [Google Scholar] [CrossRef]
- Beauchet, O.; Dubost, V.; Herrmann, F.; Rabilloud, M.; Gonthier, R.; Kressig, R.W. Relationship between dual-task related gait changes and intrinsic risk factors for falls among transitional frail older adults. Aging Clin. Exp. Res. 2005, 17, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Hausdorff, J.M.; Yogev, G.; Springer, S.; Simon, E.S.; Giladi, N. Walking is more like catching than tapping: Gait in the elderly as a complex cognitive task. Exp. Brain Res. 2005, 164, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Plummer-D’Amato, P.; Altmann, L.J.; Saracino, D.; Fox, E.; Behrman, A.L.; Marsiske, M. Interactions between cognitive tasks and gait after stroke: A dual task study. Gait Posture 2008, 27, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Marusic, U.; Taube, W.; Morrison, S.A.; Biasutti, L.; Grassi, B.; De Pauw, K.; Meeusen, R.; Pisot, R.; Ruffieux, J. Aging effects on prefrontal cortex oxygenation in a posture-cognition dual-task: An fNIRS pilot study. Eur. Rev. Aging Phys. Act. 2019, 16, 2. [Google Scholar] [CrossRef]
- Ohara, K.; Kuriyama, C.; Hada, T.; Suzuki, S.; Nakayama, Y.; Abo, M. A pilot study verifying the effectiveness of high-frequency repetitive transcranial magnetic stimulation in combination with intensive speech-language-hearing therapy in patients with chronic aphasia. NeuroRehabilitation 2021, 49, 459–467. [Google Scholar] [CrossRef]



| Characteristics | All Patients (n = 116) | Dual-Task Group (n = 71) | Control (n = 45) | Statistics for Severe vs. Moderate | |||
|---|---|---|---|---|---|---|---|
| Dual-Task Group | Control | Severe | Moderate | Severe | Moderate | ||
| Number of patients | 70 | 45 | 40 | 31 | 22 | 23 | χ2 = 116, p = 0.456 |
| Age (years) | 76 (70–80) | 79 (73–86) | 78 (72–81) | 72 (67–80) | 80 (73–87) | 78 (74–83) | F = 5.03, p = 0.03, η2 = 0.04 |
| Sex (females:males) | 40:31 | 24:21 | 22:18 | 18:13 | 10:12 | 14:9 | χ2 = 0.10, p = 0.751 |
| Grip power | |||||||
| Right side, kg | 23.7 (19.4–28.0) | 22.3 (15.5–28.5) | 22.3 (18.4–24.1) | 25.5 (20.1–31.1) | 21.8 (14.8–29.6) | 22.7 (17.8–27.1) | F = 2.09, p = 0.15, η2 = 0.04 |
| Left side, kg | 19.8 (15.3–24.5) | 20.0 (14.5–25.5) | 19.1 (14.5–21.0) | 20.7(17.1–25.1) * | 17.6 (13.3–18.9) | 22.3 (16.8–27.9) * | F = 6.12, p = 0.02, η2 = 0.05 |
| 30 s chair stand test | 14 (10–17) | 14 (11–17) | 11 (9–13) | 17 (13–21) * | 11 (9–13) | 18 (14–19) * | F = 78.52, p < 0.001, η2 = 0.40 |
| Montreal Cognitive Assessment | 22 (20–24) | 23 (21–26) | 21 (19–23) | 24 (21–27) | 22 (21–23) | 24 (21–27) | F = 15.23, p < 0.001, η2 = 0.12 |
| Barthel Index | 99 (100–100) | 99 (100–100) | 100 (100–100) | 99 (100–100) | 99 (96–100) | 99 (100–100) | F = 0.03, p = 0.864, η2 = 0.00 |
| Time Course | Robot (n = 71) | Control (n = 45) | Repeated-Measures ANOVA (Time Course × Group) |
|---|---|---|---|
| CS-30 | |||
| Pre | 13.8 ± 5.0 | 14.3 ± 5.1 | †F = 0.58, p = 0.46, η2 = 0.01 |
| During | 14.9 ± 5.5 | 15.2 ± 6.3 | Assumption checks |
| Post | 15.6 ± 5.8 * | 15.0 ± 6.2 | Mauchly’s W = 0.91, p = 0.01 |
| MoCA-J | |||
| Pre | 22.2 ± 3.4 | 23.2 ± 3.3 | F = 0.71, p = 0.49, η2 = 0.00 |
| During | 23.0 ± 3.7 | 23.8 ± 4.1 | Assumption checks |
| Post | 24.2 ± 3.6 *† | 24.5 ± 3.7 | Mauchly’s W = 0.96, p = 0.09 |
| Time Course | Severe | Repeated-Measures ANOVA Time Course × Group | Moderate | Repeated-Measures ANOVA Time Course × Group | ||
|---|---|---|---|---|---|---|
| Robot (n = 40) | Control (n = 22) | Robot (n = 31) | Control (n = 23) | |||
| CS-30 | ||||||
| Pre | 10.9 ± 2.6 | 10.9 ± 2.5 | †F = 0.58, p = 0.54, η2 = 0.00. Assumption checks; Mauchly’s W = 0.84, p = 0.01 | 17.5 ± 5.1 | 17.5 ± 4.9 | F = 0.26, p = 0.77, η2 = 0.00. Assumption checks; Mauchly’s W = 0.95, p = 0.29 |
| During | 12.1 ± 3.8 | 12.0 ± 3.8 | 18.6 ± 5.4 | 18.2 ± 6.7 | ||
| Post | 12.9 ± 4.5 * | 12.0 ± 3.9 | 19.1 ± 5.4 | 17.9 ± 6.6 | ||
| MoCA-J | ||||||
| Pre | 21.0 ± 2.4 | 22.1 ± 2.4 | F = 0.02, p = 0.98, η2 = 0.00. Assumption checks; Mauchly’s W = 0.93, p = 0.13 | 23.6 ± 3.9 | 24.2 ± 3.7 | F = 2.3, p = 0.11, η2 = 0.01. Assumption checks; Mauchly’s W = 0.95, p = 0.84 |
| During | 21.9 ± 3.0 | 22.4 ± 3.7 | 24.4 ± 4.1 | 25.0 ± 4.1 | ||
| Post | 22.8 ± 3.4 * | 23.2 ± 3.7 | 26.0 ± 3.0 *† | 25.8 ± 3.4 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abo, M.; Hamaguchi, T. Effectiveness of a Dual-Task Intervention Involving Exercise and Vocalized Cognitive Tasks. J. Clin. Med. 2024, 13, 2962. https://doi.org/10.3390/jcm13102962
Abo M, Hamaguchi T. Effectiveness of a Dual-Task Intervention Involving Exercise and Vocalized Cognitive Tasks. Journal of Clinical Medicine. 2024; 13(10):2962. https://doi.org/10.3390/jcm13102962
Chicago/Turabian StyleAbo, Masahiro, and Toyohiro Hamaguchi. 2024. "Effectiveness of a Dual-Task Intervention Involving Exercise and Vocalized Cognitive Tasks" Journal of Clinical Medicine 13, no. 10: 2962. https://doi.org/10.3390/jcm13102962







