Wearable EMG Measurement Device Using Polyurethane Foam for Motion Artifact Suppression
Abstract
:1. Introduction
2. Materials and Methods
2.1. Proposed Structure of Wearable EMG Measurement Device Using Polyurethane Form
2.2. Theoretical Calculation of Contact Pressure with or without Using Polyurethane Form
2.3. Simulation Method
2.4. Experimental Method
3. Results
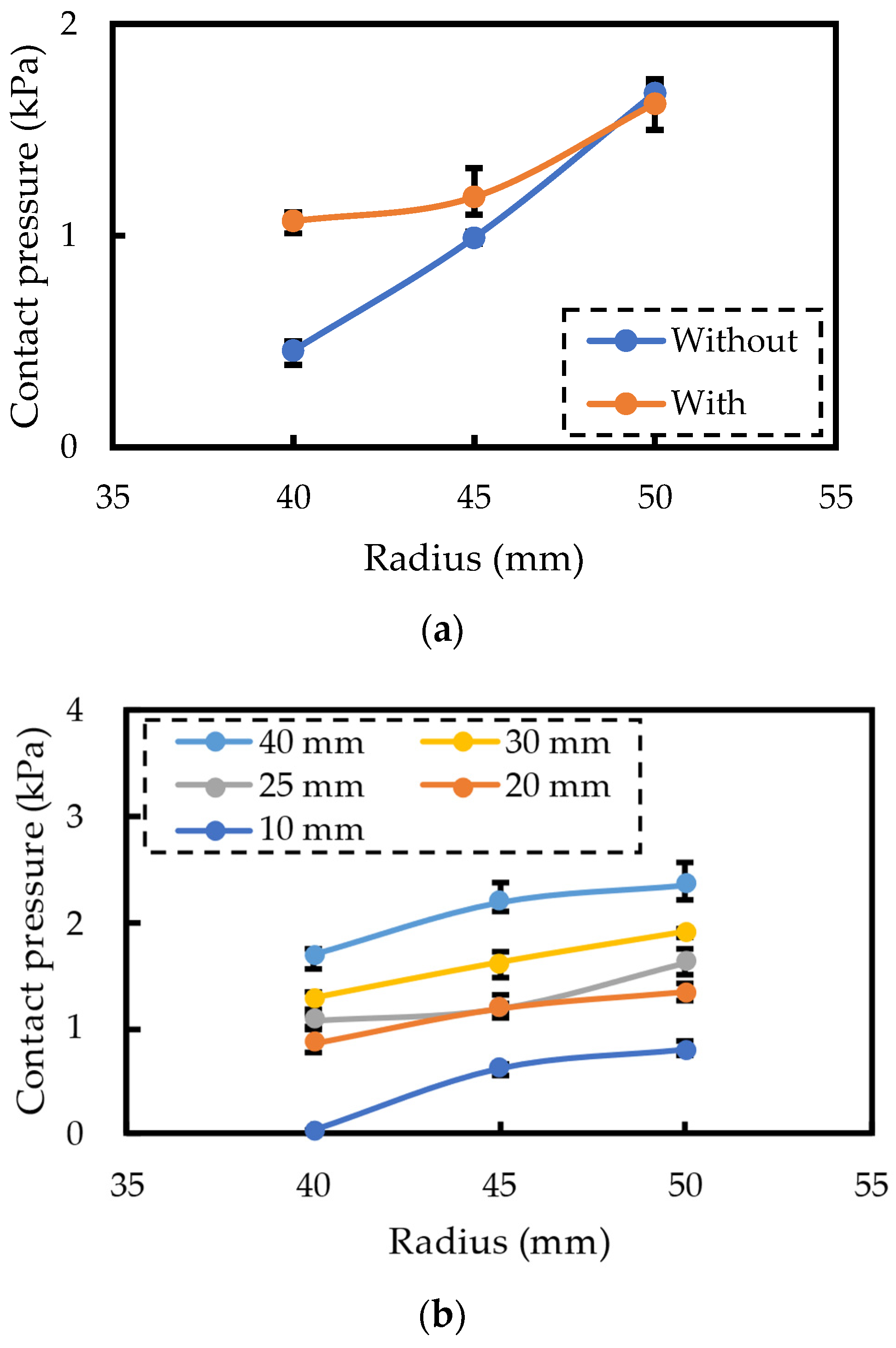
3.1. Simulation Results
3.2. Contact Pressure Measurement Experiment Results
3.3. EMG Measurement Experiment Results
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Takei, K.; Honda, W.; Harada, S.; Arie, T.; Akita, S. Toward flexible and wearable human-interactive health-monitoring devices. Adv. Healthc. Mater. 2015, 4, 487–500. [Google Scholar] [CrossRef] [PubMed]
- Mukhopadhyay, S.C. Wearable sensors for human activity monitoring: A review. IEEE Sens. J. 2014, 15, 1321–1330. [Google Scholar] [CrossRef]
- Takamatsu, S.; Itoh, T. Investigation of Mechanical and Electrical Properties of E-textile Bioelectrode Consisting of Conductive Polymer and Ionic Liquid Gel on Knit Fabric. IEEJ Trans. Sens. Micromachines 2023, 143, 2–5. [Google Scholar] [CrossRef]
- Kwak, Y.H.; Kim, W.; Park, K.B.; Kim, K.; Seo, S. Flexible heartbeat sensor for wearable device. Biosens. Bioelectron. 2017, 94, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Hinde, K.; White, G.; Armstrong, N. Wearable devices suitable for monitoring twenty four hour heart rate variability in military populations. Sensors 2021, 21, 1061. [Google Scholar] [CrossRef] [PubMed]
- Shao, M.; Zhou, Z.; Bin, G.; Bai, Y.; Wu, S. A wearable electrocardiogram telemonitoring system for atrial fibrillation detection. Sensors 2020, 20, 606. [Google Scholar] [CrossRef]
- Takamatsu, S.; Lonjaret, T.; Crisp, D.; Badier, J.-M.; Malliaras, G.G.; Ismailova, E. Direct patterning of organic conductors on knitted textiles for long-term electrocardiography. Sci. Rep. 2015, 5, 15003. [Google Scholar] [CrossRef] [PubMed]
- Sato, W.; Murata, K.; Uraoka, Y.; Shibata, K.; Yoshikawa, S.; Furuta, M. Emotional valence sensing using a wearable facial EMG device. Sci. Rep. 2021, 11, 5757. [Google Scholar] [CrossRef] [PubMed]
- Milosevic, B.; Benatti, S.; Farella, E. Design Challenges for Wearable EMG Applications. In Design, Automation & Test in Europe Conference & Exhibition (DATE); IEEE: Piscataway, NJ, USA, 2017; pp. 1432–1437. [Google Scholar]
- Takei, Y.; Takeshita, T.; Yoshida, M.; Kobayashi, T. Evaluation method for muscles, measuring mechanomyogram induced by electrical muscle stimulation using lead zirconate titanate-based acoustic sensor. Jpn. J. Appl. Phys. 2019, 58, SLLD11. [Google Scholar] [CrossRef]
- De Luca, C.J. The use of surface electromyography in biomechanics. J. Appl. Biomech. 1997, 13, 135–163. [Google Scholar] [CrossRef]
- Macaluso, A.; Nimmo, M.A.; Foster, J.E.; Cockburn, M.; McMillan, N.C.; De Vito, G. Contractile muscle volume and agonist-antagonist coactivation account for differences in torque between young and older women. Muscle Nerve 2002, 25, 858–863. [Google Scholar] [CrossRef] [PubMed]
- Aagaard, P.; Suetta, C.; Caserotti, P.; Magnusson, S.P.; Kjær, M. Role of the nervous system in sarcopenia and muscle atrophy with aging: Strength training as a countermeasure. Scand. J. Med. Sci. Sports 2010, 20, 49–64. [Google Scholar] [CrossRef] [PubMed]
- Simao, M.; Mendes, N.; Gibaru, O.; Neto, P. A review on electromyography decoding and pattern recognition for human-machine interaction. IEEE Access 2019, 7, 39564–39582. [Google Scholar] [CrossRef]
- Tigrini, A.; Verdini, F.; Fioretti, S.; Mengarelli, A. On the decoding of shoulder joint intent of motion from transient EMG: Feature evaluation and classification. IEEE Trans. Med. Robot. Bionics 2023, 5, 1037–1044. [Google Scholar] [CrossRef]
- Mobarak, R.; Tigrini, A.; Verdini, F.; Al-Timemy, A.H.; Fioretti, S.; Burattini, L.; Mengarelli, A. A minimal and multi-source recording setup for ankle joint kinematics estimation during walking using only proximal information from lower limb. IEEE Trans. Neural Syst. Rehabil. Eng. 2024, 32, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Leleux, P.; Johnson, C.; Strakosas, X.; Rivnay, J.; Hervé, T.; Owens, R.M.; Malliaras, G.G. Ionic liquid gel-assisted electrodes for long-term cutaneous recordings. Adv. Healthc. Mater. 2014, 3, 1377–1380. [Google Scholar] [CrossRef] [PubMed]
- Yapici, M.K.; Alkhidir, T.; Samad, Y.A.; Liao, K. Graphene-clad textile electrodes for electrocardiogram monitoring. Sens. Actuators B 2015, 221, 1469–1474. [Google Scholar] [CrossRef]
- Paul, G.; Torah, R.; Beeby, S.; Tudor, J. Novel active electrodes for ECG monitoring on woven textiles fabricated by screen and stencil printing. Sens. Actuators A 2015, 221, 60–66. [Google Scholar] [CrossRef]
- Myers, A.C.; Huang, H.; Zhu, Y. Wearable silver nanowire dry electrodes for electrophysiological sensing. RSC Adv. 2015, 5, 11627–11632. [Google Scholar] [CrossRef]
- Jung, H.-C.; Moon, J.-H.; Baek, D.-H.; Lee, J.-H.; Choi, Y.-Y.; Hong, J.-S.; Lee, S.-H. CNT/PDMS composite flexible dry electrodesfor long-term ECG monitoring. IEEE Trans. Biomed. Eng. 2012, 59, 1472–1479. [Google Scholar] [CrossRef]
- Yamamoto, Y.; Yamamoto, D.; Takada, M.; Naito, H.; Arie, T.; Akita, S.; Takei, K. Efficient skin temperature sensor and stable gel-less sticky ECG sensor for a wearable flexible healthcare patch. Adv. Healthc. Mater. 2017, 6, 1700495. [Google Scholar] [CrossRef] [PubMed]
- Stauffer, F.; Thielen, M.; Sauter, C.; Chardonnens, S.; Bachmann, S.; Tybrandt, K.; Peters, C.; Hierold, C.; Vörös, J. Skin conformal polymer electrodes for clinical ECG and EEG recordings. Adv. Healthc. Mater. 2018, 7, 1700994. [Google Scholar] [CrossRef] [PubMed]
- Muhlsteff, J.; Such, O.; Schmidt, R.; Perkuhn, M.; Reiter, H.; Lauter, J.; Thijs, J.; Musch, G.; Harris, M. Wearable approach for continuous ECG-and activity patient-monitoring. In Proceedings of the 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, 1–5 September 2004; pp. 2184–2187. [Google Scholar]
- Arief, Z.; Sulistijono, I.A.; Ardiansyah, R.A. Comparison of five time series EMG features extractions using Myo Armband. In International Electronics Symposium (IES); IEEE: Piscataway, NJ, USA, 2015; pp. 11–14. [Google Scholar]
- Tsukada, Y.T.; Tokita, M.; Murata, H.; Hirasawa, Y.; Yodogawa, K.; Iwasaki, Y.-k.; Asai, K.; Shimizu, W.; Kasai, N.; Nakashima, H.; et al. Validation of wearable textile electrodes for ECG monitoring. Heart Vessel. 2019, 34, 1203–1211. [Google Scholar] [CrossRef]
- Takeshita, T.; Yoshida, M.; Takei, Y.; Ouchi, A.; Hinoki, A.; Uchida, H.; Kobayashi, T. Relationship between contact pressure and motion artifacts in ECG measurement with electrostatic flocked electrodes fabricated on textile. Sci. Rep. 2019, 9, 5897. [Google Scholar] [CrossRef] [PubMed]
- Tada, Y.; Amano, Y.; Sato, T.; Saito, S.; Inoue, M. A smart shirt made with conductive ink and conductive foam for the measurement of electrocardiogram signals with unipolar precordial leads. Fibers 2015, 3, 463–477. [Google Scholar] [CrossRef]
- Paiva, A.; Catarino, A.; Carvalho, H.; Postolache, O.; Postolache, G.; Ferreira, F. Design of a long sleeve T-shirt with ECG and EMG for athletes and rehabilitation patients. In International Conference on Innovation, Engineering and Entrepreneurship; Springer International Publishing: Cham, Switzerland, 2018; pp. 244–250. [Google Scholar]
- Takeshita, T.; Yoshida, M.; Takei, Y.; Ouchi, A.; Hinoki, A.; Uchida, H.; Kobayashi, T. Development of wearable multi-lead ECG measurement device using cubic flocked electrode. Sci. Rep. 2022, 12, 19308. [Google Scholar] [CrossRef]
- Catrysse, M.; Puers, R.; Hertleer, C.; Van Langenhove, L.; Van Egmond, H.; Matthys, D. Towards the integration of textile sensors in a wireless monitoring suit. Sens. Actuators A 2004, 114, 302–311. [Google Scholar] [CrossRef]
- Tomita, N.; Takamatsu, S.; Itoh, T. Fabrication of an E-textile bioelectrode array with screen-printed wiring and an ionic liquid gel toward cutaneous whole-body electromyography. IEEE Access 2023, 11, 68421–68427. [Google Scholar] [CrossRef]
- Ishimaru, S.; Nakamura, M.; Nonomura, C.; Yokoyama, A. Effect of the human body pressure on a pressure sensation and comfort sensation. J. Jpn. Res. Assoc. Text. End-Uses 2011, 52, 197–207. (In Japanese) [Google Scholar]
- Kirk, W., Jr.; Ibrahim, S. Fundamental relationship of fabric extensibility to anthropometric requirements and garment performance. Text. Res. J. 1966, 36, 37–47. [Google Scholar] [CrossRef]
- McColl, I.; Ding, J.; Leen, S. Finite element simulation and experimental validation of fretting wear. Wear 2004, 256, 1114–1127. [Google Scholar] [CrossRef]









| Model | Length of Clothing | Width of Polyurethane Foam | Thickness of Polyurethane Foam |
|---|---|---|---|
| Without polyurethane foam | 45 | - | - |
| With polyurethane foam | 80 | 30 | 25 mm or 15–30 mm |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takagi, T.; Tomita, N.; Sato, S.; Yamamoto, M.; Takamatsu, S.; Itoh, T. Wearable EMG Measurement Device Using Polyurethane Foam for Motion Artifact Suppression. Sensors 2024, 24, 2985. https://doi.org/10.3390/s24102985
Takagi T, Tomita N, Sato S, Yamamoto M, Takamatsu S, Itoh T. Wearable EMG Measurement Device Using Polyurethane Foam for Motion Artifact Suppression. Sensors. 2024; 24(10):2985. https://doi.org/10.3390/s24102985
Chicago/Turabian StyleTakagi, Takuma, Naoto Tomita, Suguru Sato, Michitaka Yamamoto, Seiichi Takamatsu, and Toshihiro Itoh. 2024. "Wearable EMG Measurement Device Using Polyurethane Foam for Motion Artifact Suppression" Sensors 24, no. 10: 2985. https://doi.org/10.3390/s24102985





