The Role of Phytonutrient Kaempferol in the Prevention of Gastrointestinal Cancers: Recent Trends and Future Perspectives
Abstract
:Simple Summary
Abstract
1. Introduction
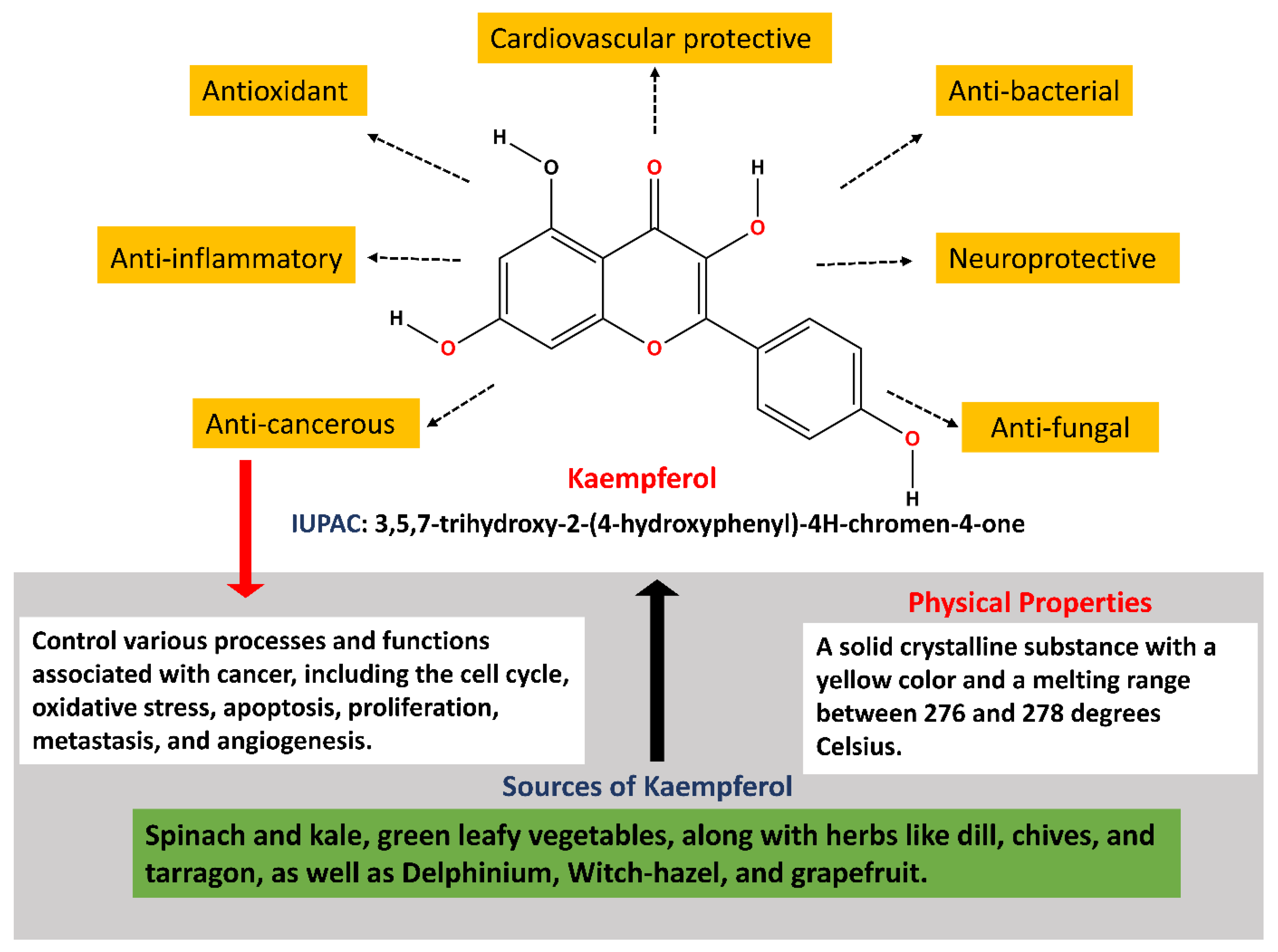
2. Chemistry and Pharmacokinetics of Kaempferol
| Properties | Details | References |
|---|---|---|
| Molecular Weight | 286.24 g/mol | |
| Classification | Flavonol | [47] |
| Solubility | Soluble in polar solvents, such as ethanol and methanol | [48] |
| Melting Point | Approximately 276–278 °C | - |
| Boiling Point | Decomposes before boiling | - |
| Color | Yellow crystalline powder | [47] |
| Odor | Odorless | [47] |
| Taste | Bitter taste | [47] |
| UV Absorption | Absorbs UV light at 266 nm and 365 nm | [49] |
| Biological Sources | Found in tea, apples, onions, grapes, broccoli, and more | [49] |
| Bioavailability | Moderate absorption in the human digestive system | [50] |
| Metabolism | Metabolized in the liver, forming various conjugates | [51] |
| Distribution in Body | Distributed in various tissues | [52] |
| Half-life in Body | Variable, influenced by factors like age and health | [53] |
| Excretion | Excreted mainly through urine | [54] |
| Biological Activities | Antioxidant, anti-inflammatory, anti-cancer, anti-microbial, and neuroprotective properties | [49] |
| Cellular Mechanisms | Modulates gene expression and signaling pathways such as Nrf2, (PI3K)/AKT, ERK/p38 MAPK, Wnt/β-Catenin. | [38] |
| Health Benefits | Enhances heart function by reducing myocardial apoptosis, fibrosis, oxidative stress, and inflammation, while maintaining mitochondrial activity and calcium homeostasis. It also provides neuroprotective advantages. | [55,56] |
| Toxicity | In vitro studies have shown that kaempferol is carcinogenic and toxic, while these effects were not reported in in vivo screenings. | [35] |
| Safety | Several in vitro studies indicate that kaempferol’s interaction with essential nutrients such as iron and folate may hinder iron bioavailability, absorption, and cellular folic acid uptake. Furthermore, a few in vitro studies demonstrate that kaempferol possesses antioxidative properties; excessive supplementation might lead to self-oxidation (pro-oxidation). However, animal studies indicate no pro-oxidation effects after oral consumption. Nevertheless, there have been no human trials investigating the potential toxicity or adverse effects of oral kaempferol consumption. | [57] |
| Medical Applications | Kaempferol may be used for the therapy of hormone-regulated cancers such as ovarian cancer, breast cancer, cervical cancer, hepatocellular carcinoma, and leukemia. | [49] |
| Regulatory Status | Considered only as a natural compound, not a regulated drug | - |
3. Implications of Kaempferol in Gastrointestinal Cancers
3.1. Esophageal Cancer
3.2. Gastric Cancer
3.3. Colorectal Cancer
3.4. Pancreatic Cancer
3.5. Liver Cancer
4. Synergistic Effect and the Significance of Nanotechnology in Kaempferol’s Therapeutic Efficacy
5. Safety Aspects of Kaempferol
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Derakhshan, M.; Yazdanbod, A.; Sadjadi, A.; Shokoohi, B.; McColl, K.; Malekzadeh, R. High incidence of adenocarcinoma arising from the right side of the gastric cardia in NW Iran. Gut 2004, 53, 1262–1266. [Google Scholar] [CrossRef]
- Sitarz, R.; Skierucha, M.; Mielko, J.; Offerhaus, G.J.A.; Maciejewski, R.; Polkowski, W.P. Gastric cancer: Epidemiology, prevention, classification, and treatment. Cancer Manag. Res. 2018, 10, 239–248. [Google Scholar] [CrossRef]
- Arnold, M.; Abnet, C.C.; Neale, R.E.; Vignat, J.; Giovannucci, E.L.; McGlynn, K.A.; Bray, F. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology 2020, 159, 335–349.e15. [Google Scholar] [CrossRef]
- Khan, M.M.; Mohsen, M.T.; Malik, M.Z.; Bagabir, S.A.; Alkhanani, M.F.; Haque, S.; Serajuddin, M.; Bharadwaj, M. Identification of potential key genes in prostate cancer with gene expression, pivotal pathways and regulatory networks analysis using integrated bioinformatics methods. Genes 2022, 13, 655. [Google Scholar] [CrossRef]
- Chirom, K.; Malik, M.Z.; Mangangcha, I.R.; Somvanshi, P.; Singh, R.B. Network medicine in ovarian cancer: Topological properties to drug discovery. Brief. Bioinform. 2022, 23, bbac085. [Google Scholar] [CrossRef]
- Ali, S.; Malik, M.Z.; Singh, S.S.; Chirom, K.; Ishrat, R.; Singh, R.B. Exploring novel key regulators in breast cancer network. PLoS ONE 2018, 13, e0198525. [Google Scholar] [CrossRef]
- Malik, M.Z.; Chirom, K.; Ali, S.; Ishrat, R.; Somvanshi, P.; Singh, R.B. Methodology of predicting novel key regulators in ovarian cancer network: A network theoretical approach. BMC Cancer 2019, 19, 1129. [Google Scholar] [CrossRef]
- Hansson, L.-E.; Nyrén, O.; Hsing, A.W.; Bergström, R.; Josefsson, S.; Chow, W.-H.; Fraumeni, J.F., Jr.; Adami, H.-O. The risk of stomach cancer in patients with gastric or duodenal ulcer disease. N. Engl. J. Med. 1996, 335, 242–249. [Google Scholar] [CrossRef]
- Shah, M.A.; Kelsen, D.P. Gastric cancer: A primer on the epidemiology and biology of the disease and an overview of the medical management of advanced disease. J. Natl. Compr. Cancer Netw. 2010, 8, 437–447. [Google Scholar] [CrossRef]
- Guggenheim, D.E.; Shah, M.A. Gastric cancer epidemiology and risk factors. J. Surg. Oncol. 2013, 107, 230–236. [Google Scholar] [CrossRef]
- Chakraborty, S.; Rahman, T. The difficulties in cancer treatment. Ecancermedicalscience 2012, 6, ed16. [Google Scholar]
- Al-Ishaq, R.K.; Overy, A.J.; Büsselberg, D. Phytochemicals and gastrointestinal cancer: Cellular mechanisms and effects to change cancer progression. Biomolecules 2020, 10, 105. [Google Scholar] [CrossRef]
- Majrashi, T.A.; Alshehri, S.A.; Alsayari, A.; Muhsinah, A.B.; Alrouji, M.; Alshahrani, A.M.; Shamsi, A.; Atiya, A. Insight into the biological roles and mechanisms of phytochemicals in different types of cancer: Targeting cancer therapeutics. Nutrients 2023, 15, 1704. [Google Scholar] [CrossRef]
- Bharti, A.C.; Singh, T.; Bhat, A.; Pande, D.; Jadli, M. Therapeutic startegies for human papillomavirus infection and associated cancers. Front. Biosci.-Elite 2018, 10, 15–73. [Google Scholar] [CrossRef]
- Liang, Z.; Xu, Y.; Zhang, Y.; Zhang, X.; Song, J.; Jin, J.; Qian, H. Anticancer applications of phytochemicals in gastric cancer: Effects and molecular mechanism. Front. Pharmacol. 2023, 13, 1078090. [Google Scholar] [CrossRef]
- Aggarwal, N.; Yadav, J.; Chhakara, S.; Janjua, D.; Tripathi, T.; Chaudhary, A.; Chhokar, A.; Thakur, K.; Singh, T.; Bharti, A.C. Phytochemicals as potential chemopreventive and chemotherapeutic agents for emerging human papillomavirus–driven head and neck cancer: Current evidence and future prospects. Front. Pharmacol. 2021, 12, 699044. [Google Scholar] [CrossRef]
- Singh Tuli, H.; Rath, P.; Chauhan, A.; Sak, K.; Aggarwal, D.; Choudhary, R.; Sharma, U.; Vashishth, K.; Sharma, S.; Kumar, M. Luteolin, a potent anticancer compound: From chemistry to cellular interactions and synergetic perspectives. Cancers 2022, 14, 5373. [Google Scholar] [CrossRef]
- Kumar, A.; Prajapati, S.; Sharma, M.; Singh, T.; Choudhary, N.; Bharti, A.C.; Sharma, R.; Gupta, P. Quantitative assessment of antioxidant potential of selected homeopathic preparations in clinical practice. Drug Metab. Pers. Ther. 2022, 38, 179–190. [Google Scholar] [CrossRef]
- Tuli, H.S.; Garg, V.K.; Kumar, A.; Aggarwal, D.; Anand, U.; Parashar, N.C.; Saini, A.K.; Mohapatra, R.K.; Dhama, K.; Kumar, M. Anticancer potential of oroxylin A: From mechanistic insight to synergistic perspectives. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2023, 396, 191–212. [Google Scholar] [CrossRef]
- Singh, T.; Aggarwal, N.; Thakur, K.; Chhokar, A.; Yadav, J.; Tripathi, T.; Jadli, M.; Bhat, A.; Kumar, A.; Narula, R.H. Evaluation of therapeutic potential of selected plant-derived homeopathic medicines for their action against cervical cancer. Homeopathy 2023, 112, 262–274. [Google Scholar] [CrossRef]
- Tuli, H.S.; Sak, K.; Garg, V.K.; Kumar, A.; Adhikary, S.; Kaur, G.; Parashar, N.C.; Parashar, G.; Mukherjee, T.K.; Sharma, U. Ampelopsin targets in cellular processes of cancer: Recent trends and advances. Toxicol. Rep. 2022, 9, 1614–1623. [Google Scholar] [CrossRef]
- Bhat, A.; Yadav, J.; Thakur, K.; Aggarwal, N.; Tripathi, T.; Chhokar, A.; Singh, T.; Jadli, M.; Bharti, A.C. Exosomes from cervical cancer cells facilitate pro-angiogenic endothelial reconditioning through transfer of Hedgehog–GLI signaling components. Cancer Cell Int. 2021, 21, 319. [Google Scholar] [CrossRef]
- Singh, T.; Chhokar, A.; Thakur, K.; Aggarwal, N.; Pragya, P.; Yadav, J.; Tripathi, T.; Jadli, M.; Bhat, A.; Gupta, P. Targeting aberrant expression of STAT3 and AP-1 oncogenic transcription factors and HPV oncoproteins in cervical cancer by Berberis aquifolium. Front. Pharmacol. 2021, 12, 757414. [Google Scholar] [CrossRef]
- Vijh, D.; Imam, M.A.; Haque, M.M.U.; Das, S.; Islam, A.; Malik, M.Z. Network pharmacology and bioinformatics approach reveals the therapeutic mechanism of action of curcumin in Alzheimer disease. Metab. Brain Dis. 2023, 38, 1205–1220. [Google Scholar] [CrossRef]
- Nejabati, H.R.; Roshangar, L. Kaempferol: A potential agent in the prevention of colorectal cancer. Physiol. Rep. 2022, 10, e15488. [Google Scholar] [CrossRef]
- Amjad, E.; Sokouti, B.; Asnaashari, S. A systematic review of anti-cancer roles and mechanisms of kaempferol as a natural compound. Cancer Cell Int. 2022, 22, 260. [Google Scholar] [CrossRef]
- Riahi-Chebbi, I.; Souid, S.; Othman, H.; Haoues, M.; Karoui, H.; Morel, A.; Srairi-Abid, N.; Essafi, M.; Essafi-Benkhadir, K. The Phenolic compound Kaempferol overcomes 5-fluorouracil resistance in human resistant LS174 colon cancer cells. Sci. Rep. 2019, 9, 195. [Google Scholar] [CrossRef]
- Song, H.; Bao, J.; Wei, Y.; Chen, Y.; Mao, X.; Li, J.; Yang, Z.; Xue, Y. Kaempferol inhibits gastric cancer tumor growth: An in vitro and in vivo study. Oncol. Rep. 2015, 33, 868–874. [Google Scholar] [CrossRef]
- Kovalev, V.; Seraya, L. Flavonoids of Glycine hispida. Chem. Nat. Compd. 1984, 20, 626–627. [Google Scholar] [CrossRef]
- Tsao, R. Chemistry and biochemistry of dietary polyphenols. Nutrients 2010, 2, 1231–1246. [Google Scholar] [CrossRef]
- M Calderon-Montano, J.; Burgos-Morón, E.; Pérez-Guerrero, C.; López-Lázaro, M. A review on the dietary flavonoid kaempferol. Mini Rev. Med. Chem. 2011, 11, 298–344. [Google Scholar] [CrossRef] [PubMed]
- DuPont, M.; Day, A.; Bennett, R.; Mellon, F.; Kroon, P. Absorption of kaempferol from endive, a source of kaempferol-3-glucuronide, in humans. Eur. J. Clin. Nutr. 2004, 58, 947–954. [Google Scholar] [CrossRef] [PubMed]
- Akiyama, M.; Mizokami, T.; Ito, H.; Ikeda, Y. A randomized, placebo-controlled trial evaluating the safety of excessive administration of kaempferol aglycone. Food Sci. Nutr. 2023, 11, 5427–5437. [Google Scholar] [CrossRef] [PubMed]
- Del Rio, D.; Rodriguez-Mateos, A.; Spencer, J.P.; Tognolini, M.; Borges, G.; Crozier, A. Dietary (poly) phenolics in human health: Structures, bioavailability, and evidence of protective effects against chronic diseases. Antioxid. Redox Signal. 2013, 18, 1818–1892. [Google Scholar] [CrossRef] [PubMed]
- Alam, W.; Khan, H.; Shah, M.A.; Cauli, O.; Saso, L. Kaempferol as a dietary anti-inflammatory agent: Current therapeutic standing. Molecules 2020, 25, 4073. [Google Scholar] [CrossRef] [PubMed]
- Barve, A.; Chen, C.; Hebbar, V.; Desiderio, J.; Saw, C.L.L.; Kong, A.N. Metabolism, oral bioavailability and pharmacokinetics of chemopreventive kaempferol in rats. Biopharm. Drug Dispos. 2009, 30, 356–365. [Google Scholar] [CrossRef] [PubMed]
- Ullah, A.; Munir, S.; Badshah, S.L.; Khan, N.; Ghani, L.; Poulson, B.G.; Emwas, A.-H.; Jaremko, M. Important flavonoids and their role as a therapeutic agent. Molecules 2020, 25, 5243. [Google Scholar] [CrossRef]
- Almatroudi, A.; Allemailem, K.S.; Alwanian, W.M.; Alharbi, B.F.; Alrumaihi, F.; Khan, A.A.; Almatroodi, S.A.; Rahmani, A.H. Effects and Mechanisms of Kaempferol in the Management of Cancers through Modulation of Inflammation and Signal Transduction Pathways. Int. J. Mol. Sci. 2023, 24, 8630. [Google Scholar] [CrossRef]
- Chen, A.Y.; Chen, Y.C. A review of the dietary flavonoid, kaempferol on human health and cancer chemoprevention. Food Chem. 2013, 138, 2099–2107. [Google Scholar] [CrossRef]
- Rho, H.S.; Ghimeray, A.K.; Yoo, D.S.; Ahn, S.M.; Kwon, S.S.; Lee, K.H.; Cho, D.H.; Cho, J.Y. Kaempferol and kaempferol rhamnosides with depigmenting and anti-inflammatory properties. Molecules 2011, 16, 3338–3344. [Google Scholar] [CrossRef]
- Imran, M.; Salehi, B.; Sharifi-Rad, J.; Aslam Gondal, T.; Saeed, F.; Imran, A.; Shahbaz, M.; Tsouh Fokou, P.V.; Umair Arshad, M.; Khan, H. Kaempferol: A key emphasis to its anticancer potential. Molecules 2019, 24, 2277. [Google Scholar] [CrossRef] [PubMed]
- Senrung, A.; Tripathi, T.; Aggarwal, N.; Janjua, D.; Chhokar, A.; Yadav, J.; Chaudhary, A.; Thakur, K.; Singh, T.; Bharti, A.C. Anti-angiogenic Potential of Trans-chalcone in an In Vivo Chick Chorioallantoic Membrane Model: An ATP Antagonist to VEGFR with Predicted Blood-brain Barrier Permeability. Cardiovasc. Hematol. Agents Med. Chem. 2024, 22, 187–211. [Google Scholar] [CrossRef]
- Mierziak, J.; Kostyn, K.; Kulma, A. Flavonoids as important molecules of plant interactions with the environment. Molecules 2014, 19, 16240–16265. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, E.; Watson, D.; Grant, M. Metabolism of quercetin and kaempferol by rat hepatocytes and the identification of flavonoid glycosides in human plasma. Xenobiotica 2002, 32, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Zabela, V.; Sampath, C.; Oufir, M.; Moradi-Afrapoli, F.; Butterweck, V.; Hamburger, M. Pharmacokinetics of dietary kaempferol and its metabolite 4-hydroxyphenylacetic acid in rats. Fitoterapia 2016, 115, 189–197. [Google Scholar] [CrossRef]
- López-Lázaro, M. A new view of carcinogenesis and an alternative approach to cancer therapy. Mol. Med. 2010, 16, 144–153. [Google Scholar] [CrossRef]
- Silva dos Santos, J.; Goncalves Cirino, J.P.; de Oliveira Carvalho, P.; Ortega, M.M. The pharmacological action of kaempferol in central nervous system diseases: A review. Front. Pharmacol. 2021, 11, 565700. [Google Scholar] [CrossRef] [PubMed]
- Bohm, B.A. Introduction to Flavonoids; Harwood Academic Publishers: New York, NY, USA, 1998. [Google Scholar]
- Singh, D.; Kumari, K.; Ahmed, S. Natural herbal products for cancer therapy. In Understanding Cancer; Elsevier: Amsterdam, The Netherlands, 2022; pp. 257–268. [Google Scholar]
- Ma, Y.; Liu, Y.; Sun, A.; Du, Y.; Ye, M.; Pu, X.; Qi, X. Intestinal absorption and neuroprotective effects of kaempferol-3-O-rutinoside. RSC Adv. 2017, 7, 31408–31416. [Google Scholar] [CrossRef]
- Mullen, W.; Edwards, C.A.; Crozier, A. Absorption, excretion and metabolite profiling of methyl-, glucuronyl-, glucosyl-and sulpho-conjugates of quercetin in human plasma and urine after ingestion of onions. Br. J. Nutr. 2006, 96, 107–116. [Google Scholar] [CrossRef]
- Zhang, Y.; Lei, X.; Xu, H.; Liu, G.; Wang, Y.; Sun, H.; Geng, F.; Zhang, N. Tissue Distribution of Total Flavonoids Extracts of Drynariae Rhizoma in Young and Old Rats by UPLC–MS/MS Determination. J. Anal. Methods Chem. 2022, 2022, 2447495. [Google Scholar] [CrossRef]
- Al-Tannak, N.F.; Al-Hasawi, N.A.; Novotny, L. UHPLC-UV analysis of morin and structurally related flavonoids with potential anticancer activity. Curr. Pharm. Anal. 2019, 15, 295–304. [Google Scholar] [CrossRef]
- O’Leary, K.A.; Day, A.J.; Needs, P.W.; Sly, W.S.; O’Brien, N.M.; Williamson, G. Flavonoid glucuronides are substrates for human liver β-glucuronidase. FEBS Lett. 2001, 503, 103–106. [Google Scholar] [CrossRef] [PubMed]
- Kamisah, Y.; Jalil, J.; Yunos, N.M.; Zainalabidin, S. Cardioprotective Properties of Kaempferol: A Review. Plants 2023, 12, 2096. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Chen, C.; Wang, L.-F.; Kuang, X.; Liu, K.; Zhang, H.; Du, J.-R. Neuroprotective effect of kaempferol glycosides against brain injury and neuroinflammation by inhibiting the activation of NF-κB and STAT3 in transient focal stroke. PLoS ONE 2013, 8, e55839. [Google Scholar] [CrossRef] [PubMed]
- Dabeek, W.M.; Marra, M.V. Dietary quercetin and kaempferol: Bioavailability and potential cardiovascular-related bioactivity in humans. Nutrients 2019, 11, 2288. [Google Scholar] [CrossRef] [PubMed]
- Mármol, I.; Sánchez-de-Diego, C.; Pradilla Dieste, A.; Cerrada, E.; Rodriguez Yoldi, M.J. Colorectal carcinoma: A general overview and future perspectives in colorectal cancer. Int. J. Mol. Sci. 2017, 18, 197. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-A.; Chen, K.-W.; Hsu, C.-Y. Prediction model for pancreatic cancer—A population-based study from NHIRD. Cancers 2022, 14, 882. [Google Scholar] [CrossRef] [PubMed]
- Liver Cancer: Statistics. Available online: https://www.cancer.net/cancer-types/liver-cancer/statistics (accessed on 25 February 2024).
- Ren, J.; Lu, Y.; Qian, Y.; Chen, B.; Wu, T.; Ji, G. Recent progress regarding kaempferol for the treatment of various diseases. Exp. Ther. Med. 2019, 18, 2759–2776. [Google Scholar] [CrossRef]
- Xu, X.; Jiang, F.; Guo, Y.; Chen, H.; Qian, J.; Wu, L.; Xie, D.; Chen, G. Clinical-Pathological Characteristics of Adenosquamous Esophageal Carcinoma: A Propensity-Score-Matching Study. J. Pers. Med. 2023, 13, 468. [Google Scholar] [CrossRef]
- Tu, L.Y.; Bai, H.H.; Cai, J.Y.; Deng, S.P. The mechanism of kaempferol induced apoptosis and inhibited proliferation in human cervical cancer SiHa cell: From macro to nano. Scanning 2016, 38, 644–653. [Google Scholar] [CrossRef] [PubMed]
- Aichler, M.; Motschmann, M.; Jütting, U.; Luber, B.; Becker, K.; Ott, K.; Lordick, F.; Langer, R.; Feith, M.; Siewert, J.R. Epidermal growth factor receptor (EGFR) is an independent adverse prognostic factor in esophageal adenocarcinoma patients treated with cisplatin-based neoadjuvant chemotherapy. Oncotarget 2014, 5, 6620. [Google Scholar] [CrossRef] [PubMed]
- Gates, M.A.; Tworoger, S.S.; Hecht, J.L.; De Vivo, I.; Rosner, B.; Hankinson, S.E. A prospective study of dietary flavonoid intake and incidence of epithelial ovarian cancer. Int. J. Cancer 2007, 121, 2225–2232. [Google Scholar] [CrossRef] [PubMed]
- Yao, S.; Wang, X.; Li, C.; Zhao, T.; Jin, H.; Fang, W. Kaempferol inhibits cell proliferation and glycolysis in esophagus squamous cell carcinoma via targeting EGFR signaling pathway. Tumor Biol. 2016, 37, 10247–10256. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Si, L.; Jia, Y.; Jian, W.; Yu, Q.; Wang, M.; Lin, R. Kaempferol exerts anti-proliferative effects on human ovarian cancer cells by inducing apoptosis, G0/G1 cell cycle arrest and modulation of MEK/ERK and STAT3 pathways. J. Buon 2019, 24, 975–981. [Google Scholar] [PubMed]
- Hu, G.; Liu, H.; Wang, M.; Peng, W. IQ motif containing GTPase-activating protein 3 (IQGAP3) inhibits kaempferol-induced apoptosis in breast cancer cells by extracellular signal-regulated kinases 1/2 (ERK1/2) signaling activation. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 7666. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zhao, X.-H.; Wang, Z.-J. Flavones and flavonols exert cytotoxic effects on a human oesophageal adenocarcinoma cell line (OE33) by causing G2/M arrest and inducing apoptosis. Food Chem. Toxicol. 2008, 46, 2042–2053. [Google Scholar] [CrossRef] [PubMed]
- Smyth, E.; Nilsson, M.; Grabsch, H.; van Grieken, N.T.; Lordick, F. Gastric Cancer. Lancet 2020, 396, 635–648. [Google Scholar]
- Kim, T.W.; Lee, S.Y.; Kim, M.; Cheon, C.; Ko, S.-G. Kaempferol induces autophagic cell death via IRE1-JNK-CHOP pathway and inhibition of G9a in gastric cancer cells. Cell Death Dis. 2018, 9, 875. [Google Scholar] [CrossRef]
- Alzahrani, S.M.; Al Doghaither, H.A.; Al-Ghafari, A.B. General insight into cancer: An overview of colorectal cancer. Mol. Clin. Oncol. 2021, 15, 271. [Google Scholar] [CrossRef]
- Majumdar, S.R.; Fletcher, R.H.; Evans, A.T. How does colorectal cancer present? Symptoms, duration, and clues to location. Am. J. Gastroenterol. 1999, 94, 3039–3045. [Google Scholar] [CrossRef]
- Narayan, S.; Roy, D. Role of APC and DNA mismatch repair genes in the development of colorectal cancers. Mol. Cancer 2003, 2, 41. [Google Scholar] [CrossRef] [PubMed]
- Roncucci, L.; Mariani, F. Prevention of colorectal cancer: How many tools do we have in our basket? Eur. J. Intern. Med. 2015, 26, 752–756. [Google Scholar] [CrossRef] [PubMed]
- Yamagishi, H.; Kuroda, H.; Imai, Y.; Hiraishi, H. Molecular pathogenesis of sporadic colorectal cancers. Chin. J. Cancer 2016, 35, 4. [Google Scholar] [CrossRef] [PubMed]
- Grivennikov, S.I.; Cominelli, F. Colitis-associated and sporadic colon cancers: Different diseases, different mutations? Gastroenterology 2016, 150, 808–810. [Google Scholar] [CrossRef] [PubMed]
- Issa, I.A.; Noureddine, M. Colorectal cancer screening: An updated review of the available options. World J. Gastroenterol. 2017, 23, 5086. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Du, J.e.; Li, C.; Li, H.; Guo, H.; Li, Z. Kaempferol can reverse the 5-Fu resistance of colorectal cancer cells by inhibiting PKM2-mediated glycolysis. Int. J. Mol. Sci. 2022, 23, 3544. [Google Scholar] [CrossRef] [PubMed]
- Bar-Shalom, R.; Bergman, M.; Grossman, S.; Azzam, N.; Sharvit, L.; Fares, F. Inula viscosa extract inhibits growth of colorectal cancer cells in vitro and in vivo through induction of apoptosis. Front. Oncol. 2019, 9, 227. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.J.; Park, J.H.Y. Kaempferol induces cell cycle arrest in HT-29 human colon cancer cells. J. Cancer Prev. 2013, 18, 257. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Cui, M.; Li, C.; Li, H.; Dai, Y.; Cui, K.; Li, Z. Kaempferol reverses aerobic glycolysis via miR-339-5p-mediated PKM alternative splicing in colon cancer cells. J. Agric. Food Chem. 2021, 69, 3060–3068. [Google Scholar] [CrossRef]
- Goral, V. Pancreatic cancer: Pathogenesis and diagnosis. Asian Pac. J. Cancer Prev. 2015, 16, 5619–5624. [Google Scholar] [CrossRef]
- Gillen, S.; Schuster, T.; Meyer zum Büschenfelde, C.; Friess, H.; Kleeff, J. Preoperative/neoadjuvant therapy in pancreatic cancer: A systematic review and meta-analysis of response and resection percentages. PLoS Med. 2010, 7, e1000267. [Google Scholar] [CrossRef] [PubMed]
- Doulabi, M.S.H.; Ghaedi, K.; Ranji, N.; Koohpar, Z.K. rs5745676 of HGF 3’UTR associates with hsa-miR-340-5p binding potential in breast cancer and gastric cancer in Isfahan population. Hum. Gene 2022, 33, 201075. [Google Scholar] [CrossRef]
- Lee, J.; Kim, J.H. Kaempferol inhibits pancreatic cancer cell growth and migration through the blockade of EGFR-related pathway in vitro. PLoS ONE 2016, 11, e0155264. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Wang, L.; Qu, C.; Chen, L.; Geng, Y.; Cheng, C.; Yu, S.; Wang, D.; Yang, L.; Meng, Z. Kaempferol induces ROS-dependent apoptosis in pancreatic cancer cells via TGM2-mediated Akt/mTOR signaling. BMC Cancer 2021, 21, 396. [Google Scholar] [CrossRef] [PubMed]
- Verma, G.; Vishnoi, K.; Tyagi, A.; Jadli, M.; Singh, T.; Goel, A.; Sharma, A.; Agarwal, K.; Prasad, S.C.; Pandey, D. Characterization of key transcription factors as molecular signatures of HPV-positive and HPV-negative oral cancers. Cancer Med. 2017, 6, 591–604. [Google Scholar] [CrossRef] [PubMed]
- Khanduja, K.; Bhardwaj, A. Stable free radical scavenging and antiperoxidative properties of resveratrol compared in vitro with some other bioflavonoids. Indian J. Biochem. Biophys. 2003, 40, 416–422. [Google Scholar] [PubMed]
- Tatsimo, S.J.N.; Tamokou, J.d.D.; Havyarimana, L.; Csupor, D.; Forgo, P.; Hohmann, J.; Kuiate, J.-R.; Tane, P. Antimicrobial and antioxidant activity of kaempferol rhamnoside derivatives from Bryophyllum pinnatum. BMC Res. Notes 2012, 5, 158. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, A.Y.; Li, M.; Chen, C.; Yao, Q. Ginkgo biloba extract kaempferol inhibits cell proliferation and induces apoptosis in pancreatic cancer cells. J. Surg. Res. 2008, 148, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Harris, D.; Besselink, E.; Henning, S.; Go, V.; Heber, D. Phytoestrogens induce differential estrogen receptor alpha-or beta-mediated responses in transfected breast cancer cells. Exp. Biol. Med. 2005, 230, 558–568. [Google Scholar] [CrossRef]
- Ogunwobi, O.O.; Harricharran, T.; Huaman, J.; Galuza, A.; Odumuwagun, O.; Tan, Y.; Ma, G.X.; Nguyen, M.T. Mechanisms of hepatocellular carcinoma progression. World J. Gastroenterol. 2019, 25, 2279. [Google Scholar] [CrossRef]
- Alqahtani, A.; Khan, Z.; Alloghbi, A.S.; Said Ahmed, T.; Ashraf, M.; M. Hammouda, D. Hepatocellular carcinoma: Molecular mechanisms and targeted therapies. Medicina 2019, 55, 526. [Google Scholar] [CrossRef] [PubMed]
- Mylonis, I.; Lakka, A.; Tsakalof, A.; Simos, G. The dietary flavonoid kaempferol effectively inhibits HIF-1 activity and hepatoma cancer cell viability under hypoxic conditions. Biochem. Biophys. Res. Commun. 2010, 398, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Langeswaran, K.; Revathy, R.; Kumar, S.G.; Vijayaprakash, S.; Balasubramanian, M.P. Kaempferol ameliorates aflatoxin B1 (AFB1) induced hepatocellular carcinoma through modifying metabolizing enzymes, membrane bound ATPases and mitochondrial TCA cycle enzymes. Asian Pac. J. Trop. Biomed. 2012, 2, S1653–S1659. [Google Scholar] [CrossRef]
- Ee, Y.Y.; Hoong, C.C. Downregulation in the mRNA expression of nuclear hormone receptor liver-X-receptor alpha (LXR-α) by TNF-α is abolished by the antioxidant kaempferol, but not ascorbic acid, in human hepatocarcinoma HepG2 cells. Asian Biomed. 2012, 6, 585–589. [Google Scholar]
- BinMowyna, M.N.; AlFaris, N.A. Kaempferol suppresses acetaminophen-induced liver damage by upregulation/activation of SIRT1. Pharm. Biol. 2021, 59, 144–154. [Google Scholar] [CrossRef] [PubMed]
- Wonganan, O.; He, Y.-j.; Shen, X.-f.; Wongkrajang, K.; Suksamrarn, A.; Zhang, G.-l.; Wang, F. 6-Hydroxy-3-O-methyl-kaempferol 6-O-glucopyranoside potentiates the anti-proliferative effect of interferon α/β by promoting activation of the JAK/STAT signaling by inhibiting SOCS3 in hepatocellular carcinoma cells. Toxicol. Appl. Pharmacol. 2017, 336, 31–39. [Google Scholar] [CrossRef]
- Huang, W.-W.; Tsai, S.-C.; Peng, S.-F.; Lin, M.-W.; Chiang, J.-H.; Chiu, Y.-J.; Fushiya, S.; Tseng, M.T.; Yang, J.-S. Kaempferol induces autophagy through AMPK and AKT signaling molecules and causes G2/M arrest via downregulation of CDK1/cyclin B in SK-HEP-1 human hepatic cancer cells. Int. J. Oncol. 2013, 42, 2069–2077. [Google Scholar] [CrossRef] [PubMed]
- Cheah, H.-Y.; Wong, Y.-Y.; Wong, H.-K.; Lim, W.-S.; Chew, C.-H. Nicotinic acid, lauric acid and kaempferol abolish ATP-binding cassette transporter subfamily A member 1 (ABCA1) down-regulation by TNF-α in hepatocarcinoma HepG2 cell line. Biomed. Res. 2014, 25, 419–425. [Google Scholar]
- Shakya, G.; Manjini, S.; Hoda, M.; Rajagopalan, R. Hepatoprotective role of kaempferol during alcohol-and ΔPUFA-induced oxidative stress. J. Basic Clin. Physiol. Pharmacol. 2014, 25, 73–79. [Google Scholar] [CrossRef]
- Tie, F.; Ding, J.; Hu, N.; Dong, Q.; Chen, Z.; Wang, H. Kaempferol and kaempferide attenuate oleic acid-induced lipid accumulation and oxidative stress in HepG2 cells. Int. J. Mol. Sci. 2021, 22, 8847. [Google Scholar] [CrossRef]
- Malik, M.Z.; Ali, S.; Singh, S.S.; Ishrat, R.; Singh, R.B. Dynamical states, possibilities and propagation of stress signal. Sci. Rep. 2017, 7, 40596. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Xing, J.; Aikemu, B.; Sun, J.; Zheng, M. Kaempferol exhibits a synergistic effect with doxorubicin to inhibit proliferation, migration, and invasion of liver cancer. Oncol. Rep. 2021, 45, 32. [Google Scholar] [CrossRef] [PubMed]
- Liang, M.; Li, L.-D.; Li, L.; Li, S. Nanotechnology in diagnosis and therapy of gastrointestinal cancer. World J. Clin. Cases 2022, 10, 5146. [Google Scholar] [CrossRef] [PubMed]
- Kanaoujiya, R.; Porwal, D.; Srivastava, S. Applications of nanomaterials for gastrointestinal tumors: A review. Front. Med. Technol. 2022, 4, 997123. [Google Scholar] [CrossRef]
- Salapa, J.; Bushman, A.; Lowe, K.; Irudayaraj, J. Nano drug delivery systems in upper gastrointestinal cancer therapy. Nano Converg. 2020, 7, 38. [Google Scholar] [CrossRef] [PubMed]
- Nikezić, A.V.V.; Bondžić, A.M.; Vasić, V.M. Drug delivery systems based on nanoparticles and related nanostructures. Eur. J. Pharm. Sci. 2020, 151, 105412. [Google Scholar] [CrossRef] [PubMed]
- Alyami, N.M.; Alyami, H.M.; Almeer, R. Using green biosynthesized kaempferol-coated sliver nanoparticles to inhibit cancer cells growth: An in vitro study using hepatocellular carcinoma (HepG2). Cancer Nanotechnol. 2022, 13, 26. [Google Scholar] [CrossRef]
- Govindaraju, S.; Roshini, A.; Lee, M.-H.; Yun, K. Kaempferol conjugated gold nanoclusters enabled efficient for anticancer therapeutics to A549 lung cancer cells. Int. J. Nanomed. 2019, 14, 5147–5157. [Google Scholar] [CrossRef]
- Raghavan, B.S.; Kondath, S.; Anantanarayanan, R.; Rajaram, R. Kaempferol mediated synthesis of gold nanoparticles and their cytotoxic effects on MCF-7 cancer cell line. Process Biochem. 2015, 50, 1966–1976. [Google Scholar] [CrossRef]
- Aghazadeh, T.; Bakhtiari, N.; Rad, I.A.; Ramezani, F. Formulation of kaempferol in nanostructured lipid carriers (NLCs): A delivery platform to sensitization of MDA-MB468 breast cancer cells to paclitaxel. Biointerface Res. Appl. Chem. 2021, 11, 14591–14601. [Google Scholar]
- Luo, H.; Jiang, B.; Li, B.; Li, Z.; Jiang, B.-H.; Chen, Y.C. Kaempferol nanoparticles achieve strong and selective inhibition of ovarian cancer cell viability. Int. J. Nanomed. 2012, 7, 3951–3959. [Google Scholar]
- Nicoleti, L.R.; Di Filippo, L.D.; Duarte, J.L.; Luiz, M.T.; Sábio, R.M.; Chorilli, M. Development, characterization and in vitro cytotoxicity of kaempferol-loaded nanostructured lipid carriers in glioblastoma multiforme cells. Colloids Surf. B Biointerfaces 2023, 226, 113309. [Google Scholar] [CrossRef] [PubMed]
- Bharathi, D.; Ranjithkumar, R.; Nandagopal, J.G.T.; Djearamane, S.; Lee, J.; Wong, L.S. Green synthesis of chitosan/silver nanocomposite using kaempferol for triple negative breast cancer therapy and antibacterial activity. Environ. Res. 2023, 238, 117109. [Google Scholar] [CrossRef] [PubMed]
- Meena, D.; Vimala, K.; Kannan, S. Combined delivery of DOX and Kaempferol using PEGylated gold nanoparticles to target colon cancer. J. Clust. Sci. 2022, 33, 173–187. [Google Scholar] [CrossRef]
- Qanash, H.; Bazaid, A.S.; Aldarhami, A.; Alharbi, B.; Almashjary, M.N.; Hazzazi, M.S.; Felemban, H.R.; Abdelghany, T.M. Phytochemical Characterization and Efficacy of Artemisia judaica Extract Loaded Chitosan Nanoparticles as Inhibitors of Cancer Proliferation and Microbial Growth. Polymers 2023, 15, 391. [Google Scholar] [CrossRef]
- Li, Y.; Zhou, S.; Song, H.; Yu, T.; Zheng, X.; Chu, Q. CaCO3 nanoparticles incorporated with KAE to enable amplified calcium overload cancer therapy. Biomaterials 2021, 277, 121080. [Google Scholar] [CrossRef] [PubMed]
- Colombo, M.; Figueiró, F.; de Fraga Dias, A.; Teixeira, H.F.; Battastini, A.M.O.; Koester, L.S. Kaempferol-loaded mucoadhesive nanoemulsion for intranasal administration reduces glioma growth in vitro. Int. J. Pharm. 2018, 543, 214–223. [Google Scholar] [CrossRef]
- Shahbaz, M.; Imran, M.; Alsagaby, S.A.; Naeem, H.; Al Abdulmonem, W.; Hussain, M.; Abdelgawad, M.A.; El-Ghorab, A.H.; Ghoneim, M.M.; El-Sherbiny, M. Anticancer, antioxidant, ameliorative and therapeutic properties of kaempferol. Int. J. Food Prop. 2023, 26, 1140–1166. [Google Scholar] [CrossRef]



| S. No. | Conjugated Nanoparticles | Composition of Nanoparticle | Cancer Type (In Vitro/Vivo Model) | Outcome | Ref. |
|---|---|---|---|---|---|
| 1 | PEO-PPO-PEO nanoparticles | poly(ethylene oxide) -poly(propylene oxide) -poly(ethylene oxide) | Ovarian (OVCAR-3) | Cancer cells were inhibited but normal cell vitality was lowered as well | [115] |
| 2 | PLGA nanoparticles | Poly(DL-lactic acid-co-glycolic | Ovarian (OVCAR-3) | Effectively reduced cancer cell viability | [115] |
| 3 | Nanostructured Lipid carriers | ------- | Glioblastoma Multiforme (U-87 MG) | Elevated toxicity against cancer cells | [116] |
| 4 | Kf-CS/Ag nanocomposite | Chitosan/silver Nanocomposite | Breast (MDA MB-231) | Exhibited significant inhibitory effects on in vitro and apoptotic cell death | [117] |
| 5 | Nanomaterial (PEGylated AuNPs-DOX @kaempeferol) | Colon HT-29 & mice) | Reduction in tumor volume in mice | [118] | |
| 6 | CNPsLE | A Judaica extract and chitosan nanoparticle- loaded extract | Prostate (PC3) | CNPsLE showed enhanced selective toxicity (IC50: 20.8 µg/mL) outperforming the extract (IC50: 76.09 µg/mL) | [119] |
| 7 | K-AuNCs | Kaempferol-conjugated gold nanocluster | Lung (A549) | Nanocluster exhibited lower toxicity to normal cells and higher toxicity to cancer cells | [112] |
| 8 | M@CaCO3@KAE | KAE loaded into CaCo3 nanoparticles incorporated with the cell membrane | ------- | It responds to the tumor microenvironment, releasing KAE and calcium ions; damages mitochondrial cytoskeleton collapse, oxidative stress, apoptosis, in vivo tumor inhibition | [120] |
| 9 | KPF-MNE | KPF-loaded mucoadhesive nanoemulsion | Glioma (C6; in vivo) | Reduces cancer cell viability via induction of apoptosis | [121] |
| 10 | AgNPs | Kaempferol-coated silver nanoparticles | Liver (HepG2) | Decreases viability of cancer cells | [111] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, T.; Sharma, D.; Sharma, R.; Tuli, H.S.; Haque, S.; Ramniwas, S.; Mathkor, D.M.; Yadav, V. The Role of Phytonutrient Kaempferol in the Prevention of Gastrointestinal Cancers: Recent Trends and Future Perspectives. Cancers 2024, 16, 1711. https://doi.org/10.3390/cancers16091711
Singh T, Sharma D, Sharma R, Tuli HS, Haque S, Ramniwas S, Mathkor DM, Yadav V. The Role of Phytonutrient Kaempferol in the Prevention of Gastrointestinal Cancers: Recent Trends and Future Perspectives. Cancers. 2024; 16(9):1711. https://doi.org/10.3390/cancers16091711
Chicago/Turabian StyleSingh, Tejveer, Deepika Sharma, Rishabh Sharma, Hardeep Singh Tuli, Shafiul Haque, Seema Ramniwas, Darin Mansor Mathkor, and Vikas Yadav. 2024. "The Role of Phytonutrient Kaempferol in the Prevention of Gastrointestinal Cancers: Recent Trends and Future Perspectives" Cancers 16, no. 9: 1711. https://doi.org/10.3390/cancers16091711






