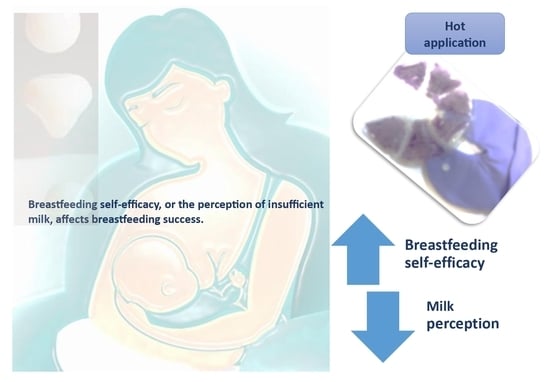
The Effect of Hot Application Applied to the Breast with the Help of the Thera Pearl in the Postpartum Period on Mothers’ Milk Perception and Postpartum Breastfeeding Self-Efficacy: A Randomized Controlled Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Sample
2.2. Data Collection
2.3. Study Procedure
2.3.1. Experimental Group
2.3.2. Control Group
2.4. Ethical Considerations
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lawrence, R.A.; Lawrence, R.M. Breastfeeding: A Guide for the Medical Professional; Elsevier: Amsterdam, The Netherlands, 2021; pp. 56–66. [Google Scholar]
- WHO. World Breastfeeding Week. 2022. Available online: https://www.emro.who.int/nutrition/campaigns/world-breastfeeding-week-2022.html (accessed on 20 April 2024).
- United Nations Children’s Fund. The State of the World’s Children 2023: For Every Child, Vaccination. 2023. Available online: https://www.unicef.org/reports/state-worlds-children-2023 (accessed on 20 April 2024).
- Turkish Population and Health Research Institute. 2019. Available online: https://www.google.com.hk/url?sa=t&source=web&rct=j&opi=89978449&url=http://www.sck.gov.tr/wp-content/uploads/2020/08/TNSA2018_ana_Rapor.pdf&ved=2ahUKEwjOq-md_vyFAxV8p1YBHSPdAqMQFnoECBgQAQ&usg=AOvVaw2n4OwcZzkLIf6mls5di0C9 (accessed on 20 April 2024).
- Santacruz-Salas, E.; Aranda-Reneo, I.; Segura-Fragoso, A.; Cobo-Cuenca, A.I.; Laredo-Aguilera, J.A.; Carmona-Torres, J.M. Mothers’ expectations and factors influencing exclusive breastfeeding during the first 6 months. Int. J. Environ. Res. Public Health 2020, 17, 77. [Google Scholar] [CrossRef] [PubMed]
- Santacruz-Salas, E.; Segura-Fragoso, A.; Cobo-Cuenca, A.I.; Carmona-Torres, J.M.; Pozuelo-Carrascosa, D.P.; Laredo-Aguilera, J.A. Factors associated with the abandonment of exclusive breastfeeding before three months. Children 2020, 7, 298. [Google Scholar] [CrossRef] [PubMed]
- Santacruz-Salas, E.; Segura-Fragoso, A.; Pozuelo-Carrascosa, D.P.; Cobo-Cuenca, A.I.; Carmona-Torres, J.M.; Laredo-Aguilera, J.A. Maintenance of maternal breastfeeding up to 6 months: Predictive models. J. Pers. Med. 2021, 11, 396. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.Y.; Lee, J.T.; Huang, C.M.; Gau, M.L. Factors related to maternal perception of milk supply while in the hospital. J. Nurs. Res. 2009, 17, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, K.; Dennis, C.L.; Tatsuoka, H.; Jimba, M. The relationship between breastfeeding self-efficacy and perceived insufficient milk among japanese mothers. J. Obstet. Gynecol. Neonatal Nurs. 2008, 37, 546–555. [Google Scholar] [CrossRef] [PubMed]
- Gatti, L. Maternal perceptions of insufficient milk supply in breastfeeding. J. Nurs. Scholarsh. 2008, 40, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Campbell, S.H. Breastfeeding Self-Efficacy: The Effects of a Breastfeeding Promotion Nursing Intervention; University of Rhode Island: Kingston, RI, USA, 1996. [Google Scholar]
- O’campo, P.; Faden, R.R.; Gielen, A.C.; Wang, M.C. Prenatal factors associated with breastfeeding duration: Recommendations for prenatal interventions. Birth 1992, 19, 195–201. [Google Scholar] [CrossRef]
- Nugraheny, E.; Alfiah, E. Faktor penghambat dan pendorong penerapan asi eksklusif. J. Akbiduk. 2016, 2, 43. [Google Scholar]
- Fazilla, T.; Tjipta, G.; Azlin, E.; Sianturi, P. Pengaruh domperidon terhadap produksi asi pada ibu yang melahirkan bayi premature. Maj. Kedokt. Nusant. J. Med. Sch. 2013, 46, 48–52. [Google Scholar]
- Nugraheni, D.; Heryati, K. Metode speos (stimulasi pijat endorphin, oksitosin dan sugestif) dapat meningkatkan produksi asi dan peningkatan berat badan bayi. J. Kesehat. 2017, 8, 1–7. [Google Scholar] [CrossRef]
- Şenol, D.K.; Pekyiğit, A.Ç. Effects of Breastfeeding Education Given in Childbirth Preparation classes for Primipara Women on their perceived prenatal Breastfeeding Self-Efficacy. Bozok Med. J. 2021, 11, 15–21. [Google Scholar]
- Yiğit, F.; Çiğdem, Z.; Temizsoy, E.; Cingi, M.E.; Korel, Ö.; Yıldırım, E.; Ovalı, F. Does warming the breasts affect the amount of breastmilk production? Breastfeed. Med. 2012, 7, 487–488. [Google Scholar] [CrossRef] [PubMed]
- Dennis, C.L.; Faux, S. Development and psychometric testing of the Breastfeeding Self-Efficacy Scale. Res. Nurs. Health 1999, 22, 399–409. [Google Scholar] [CrossRef]
- Dennis, C.L. The breastfeeding self-efficacy scale: Psychometric assessment of the short form. J. Obstet. Gynecol. Neonatal Nurs. 2003, 32, 734–744. [Google Scholar] [CrossRef] [PubMed]
- McCarter-Spaulding, D.E.; Kearney, M.H. Parenting self-efficacy and perception of insufficient breast milk. J. Obstet. Gynecol. Neonatal Nurs. 2001, 30, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel grouprandomised trials. Int. J. Surg. 2012, 10, 28–55. [Google Scholar] [CrossRef] [PubMed]
- Zielinska, M.; Sobczak, A.; Hamulka, J. Breastfeeding knowledge and exclusive breastfeeding of infants in first six months of life. Rocz. Państwowego Zakładu Hig. 2017, 68, 51–59. [Google Scholar]
- Özsoy, S.; Dündar, T. Breastfeeding behaviors of mothers in the early postpartum period (breastfeeding in the early postpartum period). Child. J. 2022, 22, 221–228. [Google Scholar]
- Hector, D.; King, L. Interventions to encourage and support breastfeeding. N. South. Wales Public. Health Bull. 2005, 16, 56–61. [Google Scholar]
- Section on Breastfeeding; Eidelman, A.I.; Schanler, R.J. Breastfeeding and the use of human milk. Pediatrics 2012, 129, 827–841. [Google Scholar] [CrossRef]
- Raghavan, V.; Bharti, B.; Kumar, P.; Mukhopadhyay, K.; Dhaliwal, L. First hour initiation of breastfeeding and exclusive breastfeeding at six weeks: Prevalence and predictors in a tertiary care setting. Indian. J. Pediatr. 2014, 81, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Kaya Odabaş, R.; Sökmen, Y.; Taşpinar, A. Examination of postgraduate theses about non-pharmacological methods applied during breastfeeding in Turkey. Dokuz Eylül Univ. Fac. Nurs. Electron. J. 2022, 15, 56–67. [Google Scholar]
- Başer, M.; Mucuk, S.; Korkmaz, Z.; Seviğ, Ü. Determining the needs of mothers and fathers regarding newborn care in the postpartum period. J. Health Sci. 2005, 14, 54–58. [Google Scholar]
- Gölbaşı, Z. Breastfeeding behaviors of women in the first 6 months postpartum and the effect of breastfeeding attitudes in the prenatal period on breastfeeding behaviors. Hacet. Univ. Fac. Nurs. J. 2008, 15, 16–31. [Google Scholar]
- Kolcaba, K. Comfort Theory and Practice: A Vision for Holistic Health Care and Research; Springer: Berlin/Heidelberg, Germany, 2003. [Google Scholar]
- Işık, C.; Küğcümen, G. Examination of lactating mothers’ perception of insufficient milk in terms of different variables. Samsun Health Sci. J. 2021, 6, 491–506. [Google Scholar]


| Group | Test Statistics | p-Value | |||
|---|---|---|---|---|---|
| Control (n = 31) Mean (SD)/N (%) | Experiment (n = 33) Mean (SD)/N (%) | Total | |||
| Age | |||||
| 20–25 | 9 (29) | 14 (42.4) | 23 (35.9) | 1.694 | 0.638 |
| 26–30 | 13 (41.9) | 10 (30.3) | 23 (35.9) | ||
| 31–35 | 6 (19.4) | 7 (21.2) | 13 (20.3) | ||
| 36 and over | 3 (9.7) | 2 (6.1) | 5 (7.8) | ||
| Living Place | |||||
| City | 21 (67.7) | 17 (51.5) | 38 (59.4) | 1.760 | 0.415 |
| County | 6 (19.4) | 10 (30.3) | 16 (25) | ||
| Village | 4 (12.9) | 6 (18.2) | 10 (15.6) | ||
| Educational Status | |||||
| Primary school | 8 (25.8) | 9 (27.3) | 17 (26.6) | 1.614 | 0.656 |
| Middle school | 11 (35.5) | 8 (24.2) | 19 (29.7) | ||
| High school | 5 (16.1) | 9 (27.3) | 14 (21.9) | ||
| University | 7 (22.6) | 7 (21.2) | 14 (21.9) | ||
| Working Status | |||||
| I am working | 8 (25.8) | 6 (18.2) | 14 (21.9) | 0.189 | 0.664 |
| I am not working | 23 (74.2) | 27 (81.8) | 50 (78.1) | ||
| Family structure | |||||
| Nuclear family | 23 (74.2) | 29 (87.9) | 52 (81.3) | 1.169 | 0.280 |
| Extended family | 8 (25.8) | 4 (12.1) | 12 (18.8) | ||
| Economical situation | |||||
| Income Less Than Expenses | 4 (12.9) | 9 (27.3) | 13 (20.3) | 2.369 | 0.306 |
| Income Equals Expenditures | 24 (77.4) | 20 (60.6) | 44 (68.8) | ||
| Income More Than Expenditures | 3 (9.7) | 4 (12.1) | 7 (10.9) | ||
| Group | Test Statistics | p-Value | |||
|---|---|---|---|---|---|
| Control (n = 31) Mean (SD)/N (%) | Experiment (n = 33) Mean (SD)/N (%) | Total | |||
| Are the breasts full? | |||||
| Yes | 17 (54.8) | 16 (48.5) | 33 (51.6) | 0.067 | 0.796 |
| No | 14 (45.2) | 17 (51.5) | 31 (48.4) | ||
| Was the baby breastfed in the first half hour? | |||||
| Breastfed successfully | 16 (51.6) | 15 (45.5) | 31 (48.4) | 0.444 | 0.801 |
| Breastfed with assistance | 8 (25.8) | 11 (33.3) | 19 (29.7) | ||
| Breastfeeding could not be achieved | 7 (22.6) | 7 (21.2) | 14 (21.9) | ||
| Has the baby been given formula? | |||||
| Yes | 18 (58.1) | 23 (69.7) | 41 (64.1) | 0.502 | 0.479 |
| No | 13 (41.9) | 10 (30.3) | 23 (35.9) | ||
| If formula is given, what is the reason? | |||||
| Lack of milk secretion | 16 (88.9) | 15 (65.2) | 31 (75.6) | 6.316 | 0.177 |
| Hypoglycemia | 1 (5.6) | 4 (17.4) | 5 (12.2) | ||
| Hyperbilirubinemia | 0 (0) | 3 (13) | 3 (7.3) | ||
| Baby’s inability to latch onto the breast | 1 (5.6) | 0 (0) | 1 (2.4) | ||
| Sunken nipple | 0 (0) | 1 (4.3) | 1 (2.4) | ||
| How does the baby latch on? | |||||
| Good | 17 (54.8) | 19 (57.6) | 36 (56.3) | 0.192 | 0.908 |
| Middle | 8 (25.8) | 7 (21.2) | 15 (23.4) | ||
| Weak | 6 (19.4) | 7 (21.2) | 13 (20.3) | ||
| Has milk secretion started? | |||||
| Comes after milking by hand | 6 (19.4) | 9 (27.3) | 15 (23.4) | 0.597 | 0.742 |
| Baby breastfeeds easily | 16 (51.6) | 16 (48.5) | 32 (50) | ||
| No milk release | 9 (29) | 8 (24.2) | 17 (26.6) | ||
| Group | Test Statistics | p-Value * | ||||
|---|---|---|---|---|---|---|
| Control | Experiment | |||||
| Mean ± S.D. | Mean (Min–Max) | Mean ± S.D. | Mean (Min–Max) | |||
| After birth (in the first 24 h) | 47.29 ± 18.18 | 57 (14–68) | 44.12 ± 18.79 | 42 (14–70) | 462 | 0.506 |
| 2–7 days after birth | 43.58 ± 15.47 | 42 (14–75) | 46.64 ± 15.27 | 46 (14–70) | 443.5 | 0.361 |
| 10–15 days after birth | 46.94 ± 19.05 | 47 (14–70) | 59.3 ± 12.84 | 62 (14–70) | 328.5 | 0.013 |
| Test statistics | 1.556 | 24.555 | ||||
| p ** | 0.459 | <0.001 | ||||
| Group | Test Statistics | p-Value * | ||||
|---|---|---|---|---|---|---|
| Control | Experiment | |||||
| Mean ± S.D. | Mean (Min–Max) | Mean ± S.D. | Mean (Min–Max) | |||
| After birth (in the first 24 h) | 26.87 ± 15.99 | 28 (0–50) | 21.85 ± 14.63 | 19 (0–47) | 415 | 0.195 |
| 2–7 days after birth | 26.97 ± 14.52 | 24 (1–50) | 29.7 ± 14.35 | 28 (3–50) | 444 | 0.364 |
| 10–15 days after birth | 30.06 ± 17.96 | 34 (0–50) | 39.45 ± 12.22 | 43 (7–50) | 384 | 0.083 |
| Test statistics | 1.322 | 34.063 | ||||
| p ** | 0.516 | <0.001 * | ||||
| β1 (%95 CI) | S. D. | β2 | Test Statistics | p | VIF | F; p | R2 | Adjusted R2 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| BSS (2–7 days after birth) | Stationary | −13.008 (−28.529–2.514) | 7.731 | −1.682 | 0.099 | 2.691; 0.007 | 0.388 | 0.244 | ||
| Group (Reference: Control) | −6.411 (−14.22–1.397) | 3.889 | −0.197 | −1.648 | 0.105 | 1.188 | ||||
| Age (Reference: 20–25) 26–30 | −1.502 (−10.393–7.389) | 4.429 | −0.044 | −0.339 | 0.736 | 1.420 | ||||
| 31 and over | 8.234 (−2.051–18.519) | 5.123 | 0.227 | 1.607 | 0.114 | 1.668 | ||||
| Educational Status (Reference: Primary School) | ||||||||||
| Middle school | 8.523 (−1.668–18.713) | 5.076 | 0.239 | 1.679 | 0.099 | 1.691 | ||||
| High school | 11.885 (0.662–23.107) | 5.590 | 0.302 | 2.126 | 0.038 | 1.679 | ||||
| University | 21.115 (8.886–33.344) | 6.091 | 0.536 | 3.466 | 0.001 | 1.994 | ||||
| Income status (Income less than expenses) | ||||||||||
| Income equals expenses | −2.458 (−12.368–7.452) | 4.936 | −0.070 | −0.498 | 0.621 | 1.646 | ||||
| Income exceeds expenses | −14.518 (−30.97–1.935) | 8.195 | −0.278 | −1.771 | 0.082 | 2.057 | ||||
| BSS (10–15 days after birth) | Stationary | −9.238 (−26.338–7.862) | 8.518 | −1.085 | 0.283 | 3.424; 0.001 | 0.446 | 0.316 | ||
| Group (Reference: Control) | −17.561 (−26.163–8.958) | 4.285 | −0.465 | −4.098 | <0.001 | 1.188 | ||||
| Age (Reference: 20–25) 26–30 | −6.209 (−16.004–3.586) | 4.879 | −0.158 | −1.273 | 0.209 | 1.420 | ||||
| 31 and over | 5.408 (−5.923–16.739) | 5.644 | 0.129 | 0.958 | 0.342 | 1.668 | ||||
| Educational Status (Reference: Primary School) | ||||||||||
| Middle school | 7.7 (−3.527–18.927) | 5.592 | 0.187 | 1.377 | 0.175 | 1.691 | ||||
| High school | 11.551 (−0.812–23.915) | 6.158 | 0.253 | 1.876 | 0.066 | 1.679 | ||||
| University | 23.703 (10.23–37.175) | 6.711 | 0.520 | 3.532 | 0.001 | 1.994 | ||||
| Income status (Income less than expenses) | ||||||||||
| Income equals expenses | −6.104 (−17.022–4.814) | 5.438 | −0.150 | −1.122 | 0.267 | 1.646 | ||||
| Income exceeds expenses | −19.511 (−37.637–1.385) | 9.029 | −0.323 | −2.161 | 0.035 | 2.057 | ||||
| IMPS (2–7 days after birth) | Stationary | −10.074 (−23.146–2.998) | 6.511 | −1.547 | 0.128 | 2.482; 0.012 | 0.369 | 0.220 | ||
| Group (Reference: Control) | −7.989 (−14.565–1.413) | 3.276 | −0.296 | −2.439 | 0.018 | 1.188 | ||||
| Age (Reference: 20–25) 26–30 | −3.607 (−11.095–3.881) | 3.730 | −0.128 | −0.967 | 0.338 | 1.420 | ||||
| 31 and over | 5.118 (−3.544–13.78) | 4.315 | 0.170 | 1.186 | 0.241 | 1.668 | ||||
| Educational Status (Reference: Primary School) | ||||||||||
| Middle school | 8.506 (−0.076–17.089) | 4.275 | 0.288 | 1.990 | 0.052 | 1.691 | ||||
| High school | 11.34 (1.889–20.791) | 4.708 | 0.347 | 2.409 | 0.020 | 1.679 | ||||
| University | 16.456 (6.157–26.755) | 5.130 | 0.504 | 3.208 | 0.002 | 1.994 | ||||
| Income status (Income less than expenses) | ||||||||||
| Income equals expenses | −3.534 (−11.88–4.812) | 4.157 | −0.121 | −0.850 | 0.399 | 1.646 | ||||
| Income exceeds expenses | −14.43 (−28.286–−0.574) | 6.902 | −0.334 | −2.091 | 0.042 | 2.057 | ||||
| IMPS (10–15 days after birth) | Stationary | −12.083 (−27.847–3.681) | 7.852 | −1.539 | 0.130 | 2.875; 0.004 | 0.404 | 0.263 | ||
| Group (Reference: Control) | −15.174 (−23.104–7.243) | 3.950 | −0.453 | −3.841 | <0.001 | 1.188 | ||||
| Age (Reference: 20–25) 26–30 | −3.967 (−12.997–5.063) | 4.498 | −0.114 | −0.882 | 0.382 | 1.420 | ||||
| 31 and over | 8.806 (−1.64–19.251) | 5.203 | 0.236 | 1.692 | 0.097 | 1.668 | ||||
| Educational Status (Reference: Primary School) | ||||||||||
| Middle school | 7.188 (−3.162–17.538) | 5.155 | 0.196 | 1.394 | 0.169 | 1.691 | ||||
| High school | 6.808 (−4.59–18.206) | 5.677 | 0.168 | 1.199 | 0.236 | 1.679 | ||||
| University | 13.253 (0.833–25.673) | 6.187 | 0.327 | 2.142 | 0.037 | 1.994 | ||||
| Income status (Income less than expenses) | ||||||||||
| Income equals expenses | −6.024 (−16.089–4.041) | 5.013 | −0.167 | −1.202 | 0.235 | 1.646 | ||||
| Income exceeds expenses | −17.146 (−33.856–0.437) | 8.323 | −0.320 | −2.060 | 0.045 | 2.057 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ozkan, H.; Uzun Ozer, B.; Arı, O. The Effect of Hot Application Applied to the Breast with the Help of the Thera Pearl in the Postpartum Period on Mothers’ Milk Perception and Postpartum Breastfeeding Self-Efficacy: A Randomized Controlled Study. Healthcare 2024, 12, 968. https://doi.org/10.3390/healthcare12100968
Ozkan H, Uzun Ozer B, Arı O. The Effect of Hot Application Applied to the Breast with the Help of the Thera Pearl in the Postpartum Period on Mothers’ Milk Perception and Postpartum Breastfeeding Self-Efficacy: A Randomized Controlled Study. Healthcare. 2024; 12(10):968. https://doi.org/10.3390/healthcare12100968
Chicago/Turabian StyleOzkan, Hava, Betül Uzun Ozer, and Ozlem Arı. 2024. "The Effect of Hot Application Applied to the Breast with the Help of the Thera Pearl in the Postpartum Period on Mothers’ Milk Perception and Postpartum Breastfeeding Self-Efficacy: A Randomized Controlled Study" Healthcare 12, no. 10: 968. https://doi.org/10.3390/healthcare12100968