Proposal and Validation of a New Index to Assess the Difficulty of Lower Third Molar Extraction
Abstract
:1. Introduction
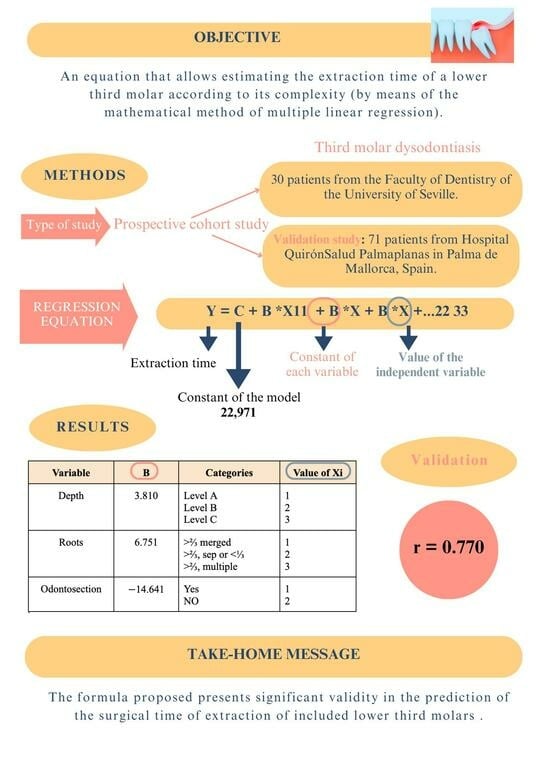
2. Materials and Methods
2.1. Type of Study
2.2. Selection of Patients
2.3. Surgical Procedure
2.4. Statistical Analysis
2.5. Validation
3. Results
3.1. Participants and Characteristics
3.2. Variables Related to the Lower Wisdom Teeth Operated on
3.3. Regression Equation
3.4. Validation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jaroń, A.; Trybek, G. The pattern of mandibular third molar impaction and assessment of surgery difficulty: A retrospective study of radiographs in east Baltic population. Int. J. Environ. Res. Public Health 2021, 18, 6016. [Google Scholar] [CrossRef]
- Zou, R.; Qiao, Y.; Lin, Y.; Piao, Z.; Zhao, T.; Wu, Q.; Xing, L.; Zhang, J.; Ouyang, K. Is it necessary to remove bone-impacted teeth? A retrospective study. J. Stomatol. Oral Maxillofac. Surg. 2023, 124, 101304. [Google Scholar] [CrossRef]
- Santosh, P. Impacted mandibular third molars: Review of literature and a proposal of a combined clinical and radiological classification. Ann. Med. Health Sci. Res. 2015, 5, 229–234. [Google Scholar] [CrossRef]
- Jeyashree, T.; Kumar, M.P.S. Evaluation of difficulty index of impacted mandibular third molar extractions. J. Adv. Pharm. Technol. Res. 2022, 13 (Suppl. S1), S98–S101. [Google Scholar]
- Bhansali, S.P.; Bhansali, S.; Tiwari, A. Review of difficulty indices for removal of impacted third molars and a new classification of difficulty indices. J. Maxillofac. Oral Surg. 2021, 20, 167–179. [Google Scholar] [CrossRef] [PubMed]
- Winter, G. Impacted Mandibular Third Molars; American Medical Book Co.: St. Louis, MO, USA, 1926. [Google Scholar]
- Pell, G.J.; Gregory, G. Impacted third molars: Classifica tion and modified technique for removal. Dent. Digest. 1933, 39, 330–338. [Google Scholar]
- MacGregor, A.J. The radiological assessment of ectopic lower third molars. Ann. R. Coll. Surg. Engl. 1979, 61, 107–113. [Google Scholar]
- Pederson GWCited in: Koerner, K.R. The removal of impacted third molars-principles and procedures. Dent. Clin. N. Am. 1988, 38, 255–278. [Google Scholar] [CrossRef]
- Kharma, M.Y.; Sakka, S.; Aws, G.; Tarakji, B.; Nassani, M.Z. Reliability of Pederson scale in surgical extraction of impacted lower third molars: Proposal of new scale. J. Oral Dis. 2014, 2014, 157523. [Google Scholar] [CrossRef]
- Al-Samman, A.A. Evaluation of Kharma scale as a predictor of lower third molar extraction difficulty. Med. Oral Patol. Oral Cir. Buccal 2017, 22, e796. [Google Scholar] [CrossRef] [PubMed]
- Roy, I.; Baliga, S.D.; Louis, A.; Rao, S. Importance of clinical and radiological parameters in assessment of surgical difficulty in removal of impacted mandibular 3rd molars: A New Index. J. Maxillofac. Oral Surg. 2015, 14, 745–749. [Google Scholar] [CrossRef] [PubMed]
- Alvira-Gonzalez, J.; Figueiredo, R.; Valmaseda-Castellon, E.; Quesada-Gomez, C.; Gay-Escoda, C. Predictive factors of difficulty in lower third molar extraction: A prospective cohort study. Med. Oral Patol. Oral Cir. Bucal. 2017, 22, e108. [Google Scholar] [CrossRef] [PubMed]
- Le, S.H.; Tonami, K.; Umemori, S.; Nguyen, L.B.; Ngo, L.Q.; Araki, K.; Nitta, H. Relationship between preoperative dental anxiety and short-term inflammatory response following oral surgery. Aust. Dent. J. 2021, 66, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Bhuju, K.G.; Shrestha, S.; Karki, R.; Aryal, S. Effect of age, gender, side and impaction types on surgical difficulty during mandibular third molar extraction. Med. J. Shree Birendra Hosp. 2018, 17, 11. [Google Scholar] [CrossRef]
- Tenglikar, P.; Munnangi, A.; Mangalgi, A.; Uddin, S.F.; Mathpathi, S.; Shah, K. An assessment of factors influencing the difficulty in third molar surgery. Ann. Maxillofac. Surg. 2017, 7, 45–50. [Google Scholar] [CrossRef]
- Sánchez Jorge, M.I.; Ocaña, R.A.; Valle Rodríguez, C.; Peyró Fernández-Montes, B.; Rico-Romano, C.; Bazal-Bonelli, S.; Sánchez-Labrador, L. Mandibular third molar extraction: Perceived surgical difficulty in relation to professional training. BMC Oral Health 2023, 23, 485. [Google Scholar] [CrossRef] [PubMed]
- Juodzbalys, G.; Daugela, P. Mandibular third molar impaction: Review of literature and a proposal of a classification. J. Oral Maxillofac. Res. 2013, 4, e1. [Google Scholar]
- Gay-Escoda, C.; Sánchez-Torres, A.; Borrás-Ferreres, J.; Valmaseda-Castellón, E. Third molar surgical difficulty scales: Systematic review and preoperative assessment form. Med. Oral Patol. Oral Cir. Bucal. 2022, 27, e68–e76. [Google Scholar] [CrossRef]
- Antonelli, A.; Barone, S.; Bennardo, F.; Giudice, A. Three-dimensional facial swelling evaluation of pre-operative single-dose of prednisone in third molar surgery: A split-mouth randomized controlled trial. BMC Oral Health 2023, 23, 614. [Google Scholar] [CrossRef]
- Pippi, R. Evaluation capability of surgical difficulty in the extraction of impacted mandibular third molars: A retrospective study from a post-graduate institution. Ann. Stomatol. 2014, 5, 7–14. [Google Scholar] [CrossRef]
- Barreiro-Torres, J.; Diniz-Freitas, M.; Lago-Méndez, L.; Gude-Sampedro, F.; Gándara-Rey, J.-M.; García-García, A. Evaluation of the surgical difficulty in lower third molar extraction. Med. Oral Patol. Oral Cir. Bucal. 2010, 15, e869–e874. [Google Scholar] [CrossRef] [PubMed]
- Ferrús-Torres, E.; Gargallo-Albiol, J.; Berini-Aytés, L.; Gay-Escoda, C. Diagnostic predictability of digital versus conventional panoramic radiographs in the presurgical evaluation of impacted mandibular third molars. Int. J. Oral Maxillofac. Surg. 2009, 38, 1184–1187. [Google Scholar] [CrossRef] [PubMed]
- Barone, S.; Antonelli, A.; Averta, F.; Diodati, F.; Muraca, D.; Bennardo, F.; Giudice, A. Does mandibular gonial angle influence the eruption pattern of the lower third molar? A three-dimensional study. J. Clin. Med. 2021, 10, 4057. [Google Scholar] [CrossRef] [PubMed]
- Jeevitha, J.Y.; Thiagarajan, A.; Sivalingam, B. Influence and impact of mandibular Ramal dimensions on the incidence of lower third molar impaction: A prospective study. J. Pharm. Bioallied Sci. 2022, 14 (Suppl. S1), S364–S368. [Google Scholar] [CrossRef] [PubMed]
- Bin Rubaia’an, M.A.; Neyaz, A.; Talic, F.; Alkhamis, A.; Alghabban, A.; Assari, A. The association between skeletal facial types and third molars impaction in a Saudi Arabian subpopulation: A CBCT study. Clin. Cosmet. Investig. Dent. 2023, 15, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Kindler, S.; Ittermann, T.; Bulow, R.; Holtfreter, B.; Klausenitz, C.; Metelmann, P. Does craniofacial morphology affect third molars impaction? Results from a populationbased study in northeastern Germany. PLoS ONE 2019, 14, e0225444. [Google Scholar] [CrossRef]
- Renton, T.; Smeeton, N.; McGurk, M. Factors predictive of difficulty of mandibular third molar surgery. Br. Dent. J. 2001, 190, 607–610. [Google Scholar] [CrossRef]
- Sekhar, M.R.; Singh, S.; Valluri, R. Correlation of variables for WHARFE assessment and Pederson difficulty index for impacted mandibular third molar surgery-A prospective clinical study. J. Maxillofac. Oral Surg. 2021, 20, 502–506. [Google Scholar] [CrossRef]
- Akadiri, O.A.; Obiechina, A.E. Assessment of difficulty in third molar surgery-a systematic review. J. Oral Maxillofac. Surg. 2009, 67, 771–774. [Google Scholar] [CrossRef]
- Bali, A.; Bali, D.; Sharma, A.; Verma, G. Is Pederson index a true predictive difficulty index for impacted mandibular third molar surgery? A meta-analysis. J. Maxillofac. Oral Surg. 2013, 12, 359–364. [Google Scholar] [CrossRef]
- Chuang, S.K.; Perrott, D.H.; Susarla, S.M.; Dodson, T.B. Age as a risk factor for third molar surgery complications. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2007, 65, 1685–1692. [Google Scholar] [CrossRef] [PubMed]
- Bisson, G.B.; Segantin, J.D.F.; Chihara, L.L.; Ciaramicolo ND, O.; Ferreira Júnior, O. Anxiety and variation of clinical parameters during third molar surgery. Res. Soc. Dev. 2022, 11, e97111436095. [Google Scholar] [CrossRef]
- Sainz de Baranda, B.; Silvestre, F.J.; Márquez-Arrico, C.F.; Silvestre-Rangil, J. Surgical difficulty and postoperative course of the third molar extraction under general anesthesia: An intervention trial. J. Stomatol. Oral Maxillofac. Surg. 2023, 125, 101663. [Google Scholar] [CrossRef] [PubMed]
- Sainz de Baranda, B.; Silvestre, F.-J.; Silvestre-Rangil, J. Relationship between surgical difficulty of third molar extraction under local anesthesia and the postoperative evolution of clinical and blood parameters. J. Oral Maxillofac. Surg. 2019, 77, 1337–1345. [Google Scholar] [CrossRef] [PubMed]
- Stacchi, C.; Daugela, P.; Berton, F.; Lombardi, T.; Andriulionis, T.; Perinetti, G.; Di Lenarda, R.; Juodzbalys, G. A classification for assessing surgical difficulty in the extraction of mandibular impacted third molars: Description and clinical validation. Quintessence Int. 2018, 49, 745–753. [Google Scholar]
- Zhang, X.; Wang, L.; Gao, Z.; Li, J.; Shan, Z. Development of a New Index to assess the difficulty level of surgical removal of impacted mandibular third molars in an Asian population. J. Oral Maxillofac. Surg. 2019, 77, 1358.e1–1358.e8. [Google Scholar] [CrossRef]


| INTERVENTION TIME | ________ MINUTES |
|---|---|
| IDENTIFICATION | Left Right |
| SPATIAL RELATIONSHIP | Mesioangular Horizontal/transverse Vertical Distoangular |
| DEPTH | Level A Level B Level C |
| BRANCH/2M DISTAL FACE RATIO | Class I ClassII Class III |
| BONE AND MUCOSAL INTEGRITY | Partially covered by mucosa Partially covered by bone and mucosa Totally covered only by mucosa, not by bone Covered by mucosa and partially by bone Completely covered by mucosa and bone |
| ROOTS | More than 2/3 merged More than 2/3 separated or less than 1/3 separated More than 2/3, multiple |
| FOLLICLE SIZE | >1 mm 0 mm |
| ACTIONS (more than one box can be checked) | Osteotomy Odontosection Sutura Simple exodontia |
| Variables | Categories | Seville | Mallorca | Sign. | ||
|---|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | |||
| Sex | Man Woman | 17 | 56.7 | 27 | 38.0 | quasi |
| 13 | 43.3 | 44 | 62.0 | |||
| Age (categorized) | Up to 22 years old | 12 | 42.9 | 22 | 29.3 | |
| From 23 to 29 years old | 8 | 28.6 | 19 | 25.3 | ||
| From 30 to 39 years old | 5 | 17.9 | 13 | 17.3 | ||
| 40 or more years | 3 | 10.7 | 21 | 28.0 | ||
| Ostectomy | Yes | 25 | 80.6 | 42 | 56.0 | <0.05 |
| No | 6 | 19.4 | 33 | 44.0 | ||
| Odontosection | Yes | 24 | 77.4 | 31 | 41.3 | <0.001 |
| No | 7 | 22.6 | 44 | 58.7 | ||
| Suture | Yes | 28 | 90.3 | 66 | 88.0 | |
| No | 3 | 9.7 | 9 | 12.0 | ||
| Simple exodontia | Yes | 3 | 9.7 | 32 | 42.7 | <0.01 |
| No | 28 | 90.3 | 43 | 57.3 | ||
| Variables | Categories | Seville | Mallorca | Sign. | ||
|---|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | |||
| Spatial relationship | Mesioangular Horizontal/Angled | 8 | 25.8 | 30 | 40.0 | |
| 9 | 29.0 | 9 | 12.0 | |||
| Vertical | 13 | 41.9 | 32 | 42.7 | ||
| Distoangular | 1 | 3.2 | 4 | 5.3 | ||
| Depth | Level A | 14 | 45.2 | 41 | 54.7 | |
| Level B | 12 | 38.7 | 26 | 34.7 | ||
| Level C | 5 | 16.1 | 8 | 10.7 | ||
| Ratio branch/distal face 2M | Class I | 14 | 45.2 | 41 | 54.7 | |
| Class II | 14 | 45.2 | 26 | 34.7 | ||
| Class III | 3 | 9.7 | 8 | 10.7 | ||
| Bone and mucosal integrity | CParc. Mucosa | 16 | 51.6 | 34 | 45.3 | <0.05 |
| CParc. Hue. Y Muc. | 7 | 22.6 | 3 | 4.0 | ||
| CTot. Muc. No Hue. | 1 | 3.2 | 4 | 5.3 | ||
| C Muc and Parc. Hue | 4 | 12.9 | 18 | 24.0 | ||
| CTot. Muc. and Bone | 3 | 9.7 | 16 | 21.3 | ||
| Roots | >2/3, merged | 14 | 45.2 | 41 | 54.7 | |
| >2/3, sep or <1/3 | 14 | 45.2 | 32 | 42.7 | ||
| >2/3, multiple | 3 | 9.7 | 2 | 2.7 | ||
| Follicle size | >1 mm | 22 | 71.0 | 49 | 65.3 | |
| 0 mm | 9 | 29.0 | 26 | 34.7 | ||
| Difficulty index (categorized) | Not very difficult | 13 | 41.9 | 33 | 44.0 | |
| Difficult | 16 | 51.6 | 34 | 45.3 | ||
| Very difficult | 2 | 6.5 | 8 | 10.7 | ||
| Difficulty index (dichotomous) | Not very difficult | 13 | 41.9 | 33 | 44.0 | |
| Difficult or Very Difficult | 18 | 58.1 | 42 | 56.0 | ||
| Variable | Non-Standardized Coefficients | Coef. Est. | t | Sig (p) | |
|---|---|---|---|---|---|
| B | Error | Beta | |||
| (Constant) | 22.971 | 6.410 | 3.584 | 0.001 | |
| IQ: Depth | 3.810 | 2.155 | 0.237 | 1.768 | 0.088 |
| CI: Roots | 6.751 | 2.403 | 0.376 | 2.810 | 0.009 |
| Odontosection | −14.641 | 3.448 | −0.524 | −4.247 | 0.000 |
| Variable | Categories | Value of Xi |
|---|---|---|
| Depth | Level A | 1 |
| Level B | 2 | |
| Level C | 3 | |
| Roots | >2/3, merged | 1 |
| >2/3, sep or <1/3 | 2 | |
| >2/3, multiple | 3 | |
| Odontosection | No | 1 |
| Yes | 2 |
| Forecast | Forecast Error (Actual Value—Estimate) | |||||
|---|---|---|---|---|---|---|
| Media | Standard Deviation | Media | Standard Deviation | Q1 | Q2 | Q3 |
| 22.65 | 9.14 | 0.00 | −2.73 | 5.89 | 2.70 | −0.55 |
| Forecast | Forecast Error (Actual Value—Estimate) | |||||
|---|---|---|---|---|---|---|
| Media | Standard Deviation | Media | Standard Deviation | Q1 | Q2 | Q3 |
| 15.67 | 10.88 | −0.94 | 6.86 | −5.00 | 0.19 | 2.75 |
| R | R Square | Adjusted R-Squared | Standard Error of the Estimate |
|---|---|---|---|
| 0.770 | 0.593 | 0.548 | 7.981 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hermida-Cabrera, P.; Lima-Sánchez, B.; Montoya-Salazar, V.; Oliveros-López, L.-G.; Alomar-Velasco, P.; Gutiérrez-Pérez, J.-L.; Torres-Lagares, D.; Baus-Domínguez, M. Proposal and Validation of a New Index to Assess the Difficulty of Lower Third Molar Extraction. Dent. J. 2024, 12, 138. https://doi.org/10.3390/dj12050138
Hermida-Cabrera P, Lima-Sánchez B, Montoya-Salazar V, Oliveros-López L-G, Alomar-Velasco P, Gutiérrez-Pérez J-L, Torres-Lagares D, Baus-Domínguez M. Proposal and Validation of a New Index to Assess the Difficulty of Lower Third Molar Extraction. Dentistry Journal. 2024; 12(5):138. https://doi.org/10.3390/dj12050138
Chicago/Turabian StyleHermida-Cabrera, Paula, Belén Lima-Sánchez, Vanessa Montoya-Salazar, Luis-Guillermo Oliveros-López, Pedro Alomar-Velasco, José-Luis Gutiérrez-Pérez, Daniel Torres-Lagares, and María Baus-Domínguez. 2024. "Proposal and Validation of a New Index to Assess the Difficulty of Lower Third Molar Extraction" Dentistry Journal 12, no. 5: 138. https://doi.org/10.3390/dj12050138