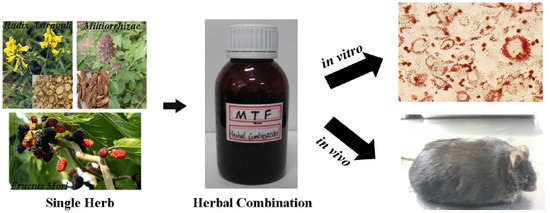
Pharmacological Effects of the Water Fraction of Key Components in the Traditional Chinese Prescription Mai Tong Fang on 3T3-L1 Adipocytes and ob/ob Diabetic Mice
Abstract
:1. Introduction
| Common Name | Voucher Specimen Number | Drug Name | Latin Name | Family |
|---|---|---|---|---|
| Milkvetch root | No. 405 | Radix Astragali | Astragalus membranaceus (Fisch.) Bunge | Leguminosae |
| Salviae miltiorrhizae | No. 1101 | Radix Salviae Miltiorrhzae | Salvia miltiorrhiza Bunge | Labiatae |
| Mulberry | No. 476 | Fructus Mori | Morus alba L. | Moraceae |
2. Results
2.1. TG Accumulation in 3T3-L1 Adipocytes


2.2. Body Weight and Food Intake

2.3. Oral Glucose Tolerance Test (OGTT) and Insulin Tolerance Test (ITT)

2.4. Serum Biomarkers
| Parameter | Vehicle | MTF 4 mg/kg | MTF 8 mg/kg | RSG 3 mg/kg |
|---|---|---|---|---|
| GLU (mM) | 23.94 ± 11.77 | 15.67 ± 3.17 ** | 12.48 ± 1.88 ** | 11.30 ± 3.46 ** |
| TG (mM) | 1.57 ± 0.13 | 1.33 ± 0.34 | 1.14 ± 0.07 * | 1.58 ± 0.20 |
| TC (mM) | 8.27 ± 0.96 | 5.57 ± 0.63 * | 5.30 ± 1.24 * | 4.46 ± 1.05 * |
| ALT (mM) | 220.0 ± 116.8 | 304.7 ± 75.1 ** | 303.0 ± 36.3 ** | 987.4 ± 160.4 ** |
| HDL-c (mM) | 1.27 ± 0.32 | 1.42 ± 0.18 | 1.14 ± 0.27 | 2.16 ± 0.28 |
| LDL-c (mM) | 0.35 ± 0.09 | 0.26 ± 0.10 | 0.31 ± 0.08 | 0.57 ± 0.08 |
2.5. Evaluation of Liver and Adipose Histopathology

3. Discussion
4. Experimental Section
4.1. Preparation of Herbal Extracts
4.2. HPLC-MS Analysis

| Peak | Predicted Compound | MW | [M−H]− | Milkvetch Root | Salviae Miltiorrhizae | Mulberry |
|---|---|---|---|---|---|---|
| 1 | Danshensu | 198 | 197 |  | ||
| 2 | Formononetin-7-O-β-gluco-pyranoside | 516 | 515 |  | ||
| 3 | Cafleoylquinic acid | 354 | 353 |  | ||
| 4 | Unknown | 375 |  | |||
| 5 | Salvianolic acid J | 537 | 536 |  | ||
| 6 | Rosmarimic acid | 360 | 359 |  | ||
| 7 | Salvianolic acid A | 494 | 493 |  | ||
| 8 | Calycosin | 284 | 283 |  | ||
| 9 | Formononetin | 268 | 267 |  | ||
| 10 | Carnosol | 330 | 329 |  | ||
| 11 | Asp | 515 | 514 |  | ||
| 12 | Val | 499 | 498 |  |
4.3. Cell Culture
4.4. Oil Red O Staining
4.5. Cytotoxicity Assay
4.6. Animals
4.7. Oral Glucose Tolerance Test (OGTT) and Insulin Tolerance Test (ITT)
4.8. Measurements of Serum Parameters in ob/ob Mice
4.9. Histopathological Analysis
4.10. Statistical Analysis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Panunti, B.; Jawa, A.A.; Fonseca, V.A. Mechanisms and therapeutic targets in type 2 diabetes mellitus. Drug Discov. Today 2004, 1, 151–157. [Google Scholar] [CrossRef]
- Hoffman, W.H.; Helman, S.W.; Passmore, G. Acute activation of peripheral lymphocytes during treatment of diabetic ketoacidosis. J. Diabetes Complicat. 2011, 15, 144–149. [Google Scholar] [CrossRef]
- Kamenov, Z.A.; Parapunova, R.A.; Georgieva, R.T. Earlier development of diabetic neuropathy in men than in women with type 2 diabetes mellitus. Gender Med. 2010, 7, 600–615. [Google Scholar] [CrossRef]
- Inukai, T.; Fujiwara, Y.; Tayama, K.; Aso, Y.; Takemura, Y. Serum levels of carboxy-terminal propeptide of human type I procollagen are an indicator for the progression of diabetic nephropathy in patients with Type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 2000, 48, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Alan, C.; Karin, E.B. Diabetes and atherosclerosis: Is there a role for hyperglycemia? J. Lipid Res. 2009, 50, 335–339. [Google Scholar]
- Romero-Aroca, P.; Fernández-Balart, J.; Baget-Bernaldiz, M.; Martinez-Salcedo, I.; Méndez-Marín, I.; Salvat-Serra, M.; Buil-Calvo, J.A. Changes in the diabetic retinopathy epidemiology after 14 years in a population of Type 1 and 2 diabetic patients after the new diabetes mellitus diagnosis criteria and a more strict control of the patients. J. Diabetes Complicat. 2009, 23, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Wild, S.; Roglic, G.; Green, A.; Sicree, R.; King, H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care 2004, 27, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.Y.; Wu, H.S.; Tang, L.; Feng, C.R.; Yu, J.H.; Li, Y.; Yang, Y.S.; Yang, B.; He, Q.J. The potential insulin sensitizing and glucose lowering effects of a novel indole derivative in vitro and in vivo. Pharmacol. Res. 2007, 56, 335–343. [Google Scholar]
- Liu, R.Y.; Wang, G.Q. A survey on drugs synthesized for antidiabetes. J. Shenyang Pharm. Univ. 1996, 13, 148–153. [Google Scholar]
- Yuan, Y.M.; Gao, J.W.; Shi, Z.; Huang, P.; Lu, Y.S.; Yao, M.C.; Huang, M. Herb drug pharmacokinetic interaction between radix astragali and pioglitazone in rats. J. Ethnopharmacol. 2012, 144, 300–304. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.J.; Zhang, Q.Y.; Wu, Q.W. Effect of Astragalus membranaceus on experimental diabetic renal hypertrophy and microalbuminuria. J. Shanghai Second Med. Univ. 1997, 17, 357–359. [Google Scholar]
- Gao, Y.; Wang, G.X.; Yang, X.; He, S.C.; Zhao, B. Effect of Astragaluson prevention and treatment of nerve conduction velocity decrease in diabetic animals. J. Norman Bethune Univ. Med. Sci. 1998, 24, 372–373. [Google Scholar]
- Ye, H.Y.; Yu, M.H.; You, L.; Yan, Y.Q.; Yang, X.F. Effects of Astragalus polysaccharide on metabolism and heart function of rats with streptozocin-induced diabetes. J. Shanghai Med. Univ. 2000, 27, 357–358. [Google Scholar]
- Chen, W.; Liu, F.; Yu, M.H.; Zhu, Q.Y.; Zhu, X.X. Astragalus polysaccharide prevention of type 1 diabetes in nonobese diabetic mice. Exp. Clin. Endocrinol. Diabetes 2001, 28, 57–60. [Google Scholar]
- Chen, W.; Yu, M.H.; Li, Y.M.; Chen, W.J.; Xia, Y.P. Beneficial effects of astragalus polysaccharides treatment on cardiac chymase activities and cardiomyopathy in diabetic hamsters. Acta diabetologica 2010, 47, 35–46. [Google Scholar] [PubMed]
- Hikino, H.; Mizuno, T.; Oshima, Y.; Konno, C. Isolation and hypoglycemic activity of Morans A, a glycoprotein of Morus alba root barks. Planta Med. 1985, 51, 159–160. [Google Scholar] [CrossRef]
- Li, W.L.; Zheng, H.C.; Bukuru, J.; de Kimpe, N. Natural medicines used in the traditional Chinese medical system for therapy of diabetes mellitus. J. Ethnopharmacol. 2004, 92, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Qi, L.G.; Wang, Y.S.; Guan, Q.B.; Li, Y.B. Effects of Maitongfang on platelet function and femoral artery endothelium conformation of DM rats induced by high-sugar, high-fat and high-cholesterol diet. Chin. J. Cur. Tradit. West. Med. 2004, 2, 9–11. [Google Scholar]
- Qi, L.G.; Liu, G.Y.; Zhu, D.P.; Wang, J.; Liu, Q. Clinial study of Mai Tong Fang for treatment of the fourth stage diabetic nephropathy. Chin. Arch. Tradit. Chin. Med. 2007, 25, 1548–1550. [Google Scholar]
- Wu, M.R.; Hou, M.H.; Lin, Y.L.; Kuo, C.F. 2,4,5-TMBA, a natural inhibitor of cyclooxygenase-2, suppresses adipogenesis and promotes lipolysis in 3T3-L1 adipocytes. J. Agric. Food Chem. 2012, 60, 7262–7269. [Google Scholar] [CrossRef] [PubMed]
- Heffner, S.M.; Miettinen, H. Insulin resistance implications for type II diabetes mellitus and coronary heart disease. Am. J. Med. 1997, 103, 152–162. [Google Scholar] [CrossRef] [PubMed]
- Ahren, B.; Pacini, G. Importance of quantifying insulin secretion in relation to insulin sensitivity to accurately assess beta cell function in clinical studies. Eur. J. Endocrinol. 2004, 150, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Liou, S.S.; Liu, I.M.; Hsu, J.H.; Wu, Y.C.; Hsu, S.F.; Chen, J.T. Release of acetylcholine by Die-Huang-Wan to enhance insulin secretion for lowering plasma glucose in Wistar rats. Auton. Neurosci.-Basic Clin. 2002, 100, 21–26. [Google Scholar]
- Cox, K.L.; Burke, V.; Morton, A.R.; Beilin, L.J.; Puddey, I.B. Independent and additive effects of energy restriction and exercise on glucose and insulin concentrations in sedentary overweight men. Am. J. Clin. Nutr. 2004, 80, 308–316. [Google Scholar] [PubMed]
- Zeng, X.Y.; Zhou, X.; Xu, J.; Chan, S.M.; Xue, C.L.; Molero, J.C.; Ye, J.M. Screening for the efficacy on lipid accumulation in 3T3-L1 cells is an effective tool for the identification of new anti-diabetic compounds. Biochem. Pharmacol. 2012, 84, 830–837. [Google Scholar] [CrossRef] [PubMed]
- Kinkel, A.D.; Fernyhough, M.E.; Helterline, D.L.; Vierck, J.L.; Oberg, K.S.; Vance, T.J. Oil red-O stains non-adipogenic cells: A precautionary note. Cytotechnology 2004, 46, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Institute of Laboratory Animal Resources (US). Guide for the Care and Use of Laboratory Animals; National Academies Press: Washington, DC, USA, 1996. [Google Scholar]
- Sample availability: Samples are available from the authors.
© 2014 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license ( http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Ma, L.; Huang, L.; Pei, H.; Liu, Z.; Xie, C.; Lei, L.; Chen, X.; Ye, H.; Peng, A.; Chen, L. Pharmacological Effects of the Water Fraction of Key Components in the Traditional Chinese Prescription Mai Tong Fang on 3T3-L1 Adipocytes and ob/ob Diabetic Mice. Molecules 2014, 19, 14687-14698. https://doi.org/10.3390/molecules190914687
Ma L, Huang L, Pei H, Liu Z, Xie C, Lei L, Chen X, Ye H, Peng A, Chen L. Pharmacological Effects of the Water Fraction of Key Components in the Traditional Chinese Prescription Mai Tong Fang on 3T3-L1 Adipocytes and ob/ob Diabetic Mice. Molecules. 2014; 19(9):14687-14698. https://doi.org/10.3390/molecules190914687
Chicago/Turabian StyleMa, Liang, Li Huang, Heying Pei, Zhuowei Liu, Caifeng Xie, Lei Lei, Xiaoxin Chen, Haoyu Ye, Aihua Peng, and Lijuan Chen. 2014. "Pharmacological Effects of the Water Fraction of Key Components in the Traditional Chinese Prescription Mai Tong Fang on 3T3-L1 Adipocytes and ob/ob Diabetic Mice" Molecules 19, no. 9: 14687-14698. https://doi.org/10.3390/molecules190914687