Clinical Impact of Tumor-Infiltrating Inflammatory Cells in Primary Small Cell Esophageal Carcinoma
Abstract
:1. Introduction
2. Results and Discussion
2.1. Patients’ Demographics, Clinico-Pathological Characteristics and Treatment
2.2. Eosinophils and Macrophages Are Increased in SmCEC (Small Cell Esophageal Carcinoma) Tissues in Comparison with Tumor Adjacent Normal Tissues
| Inflammatory Cell Type | Cell Count (Mean ± SD)/HPF | p |
|---|---|---|
| Eosinophils | ||
| SmCEC (n = 36) | 7.57 ± 4.63/HPF | <0.001 |
| Normal (n = 19) | 2.44 ± 2.46/HPF | - |
| Neutrophils | ||
| SmCEC (n = 36) | 1.93 ± 1.14/HPF | 0.095 |
| Normal (n = 19) | 1.39 ± 0.52/HPF | - |
| Lymphocytes | ||
| SmCEC (n = 36) | 89.64 ± 23.90/HPF | 0.199 |
| Normal (n = 19) | 78.94 ± 17.23/HPF | - |
| Macrophages | ||
| SmCEC (n = 36) | 15.12 ± 8.53/HPF | <0.001 |
| Normal (n = 19) | 5.25 ± 4.23/HPF | - |
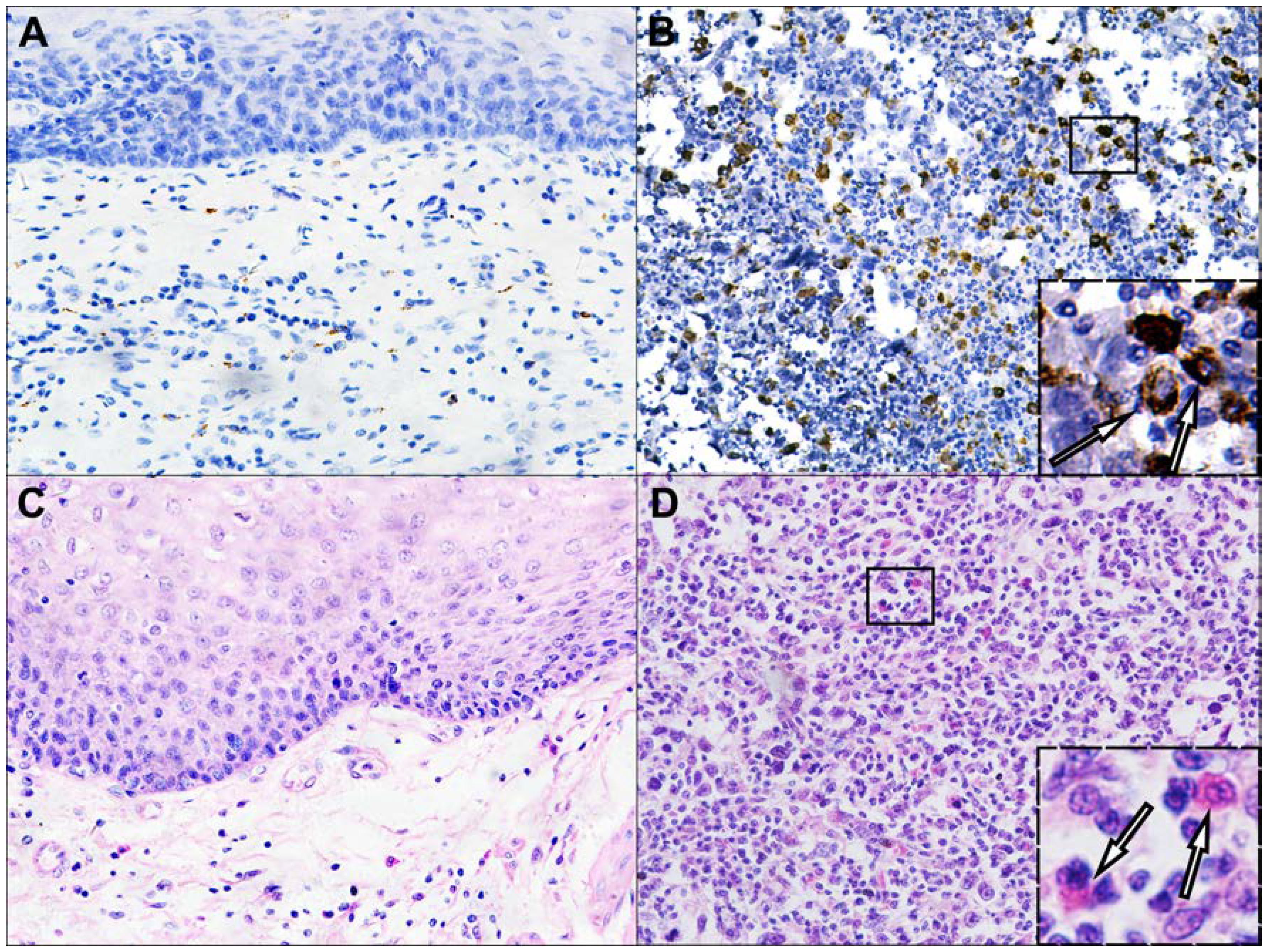
2.3. Eosinophils and Macrophages Are Increased in ESqCC (Esophageal Squamous Cell Carcinoma) Tissues in Comparison with SmCEC Tissues
2.4. Correlation of Inflammatory Cells with Clinico-Pathological Characteristics of SmCEC Patients
| Features | Macrophages | Eosinophils | Neutrophils | Lymphocytes | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | High | p | Low | High | p | Low | High | p | Low | High | p | |||||||||
| Sex | ||||||||||||||||||||
| Male | 12 | 13 | 1.000 | 12 | 13 | 1.000 | 12 | 13 | 1.000 | 13 | 12 | 1.000 | ||||||||
| Female | 6 | 5 | - | 6 | 5 | - | 6 | 5 | - | 5 | 6 | - | ||||||||
| T stage | ||||||||||||||||||||
| T1 + T2 | 9 | 13 | 0.305 | 12 | 10 | 0.733 | 11 | 11 | 1.000 | 12 | 10 | 0.733 | ||||||||
| T3 + T4 | 9 | 5 | - | 6 | 8 | - | 7 | 7 | - | 6 | 8 | - | ||||||||
| pTNM stage | ||||||||||||||||||||
| I + II | 9 | 15 | 0.075 | 13 | 11 | - | 13 | 11 | 0.725 | 13 | 11 | 0.725 | ||||||||
| III + IV | 9 | 3 | - | 5 | 7 | - | 5 | 7 | - | 5 | 7 | - | ||||||||
| Location of the primary tumor | ||||||||||||||||||||
| Lt | 5 | 5 | 1.000 | 5 | 5 | 1.000 | 5 | 5 | 0.273 | 5 | 5 | 1.000 | ||||||||
| Mt | 12 | 11 | - | 12 | 11 | - | 10 | 13 | - | 12 | 11 | - | ||||||||
| Ut | 1 | 2 | - | 1 | 2 | - | 3 | 0 | - | 1 | 2 | - | ||||||||
| Macroscopic tumor type | ||||||||||||||||||||
| Ulcerative | 8 | 6 | 0.345 | 8 | 6 | 0.922 | 8 | 6 | 0.150 | 7 | 7 | 0.056 | ||||||||
| Medullary | 8 | 6 | - | 7 | 7 | - | 4 | 10 | - | 4 | 10 | - | ||||||||
| Intraluminal | 0 | 3 | - | 1 | 2 | - | 3 | 0 | - | 3 | 0 | - | ||||||||
| Mushroom | 2 | 3 | - | 2 | 3 | - | 3 | 2 | - | 4 | 1 | - | ||||||||
| N stage | ||||||||||||||||||||
| N0 | 3 | 11 | 0.015 * | 5 | 9 | 0.305 | 7 | 7 | 1.000 | 7 | 7 | 1.000 | ||||||||
| N1+N2 | 15 | 7 | - | 13 | 9 | - | 11 | 11 | - | 11 | 11 | - | ||||||||
| Age, years | ||||||||||||||||||||
| ≤60 | 10 | 9 | 1.000 | 9 | 10 | 1.000 | 11 | 8 | 0.505 | 12 | 7 | 0.181 | ||||||||
| >60 | 8 | 9 | - | 9 | 8 | - | 7 | 10 | - | 6 | 11 | - | ||||||||
| Tumor size, cm | ||||||||||||||||||||
| ≤4 | 8 | 12 | 0.315 | 13 | 7 | 0.092 | 10 | 10 | 1.000 | 10 | 10 | 1.000 | ||||||||
| >4 | 10 | 6 | - | 5 | 11 | - | 8 | 8 | - | 8 | 8 | - | ||||||||
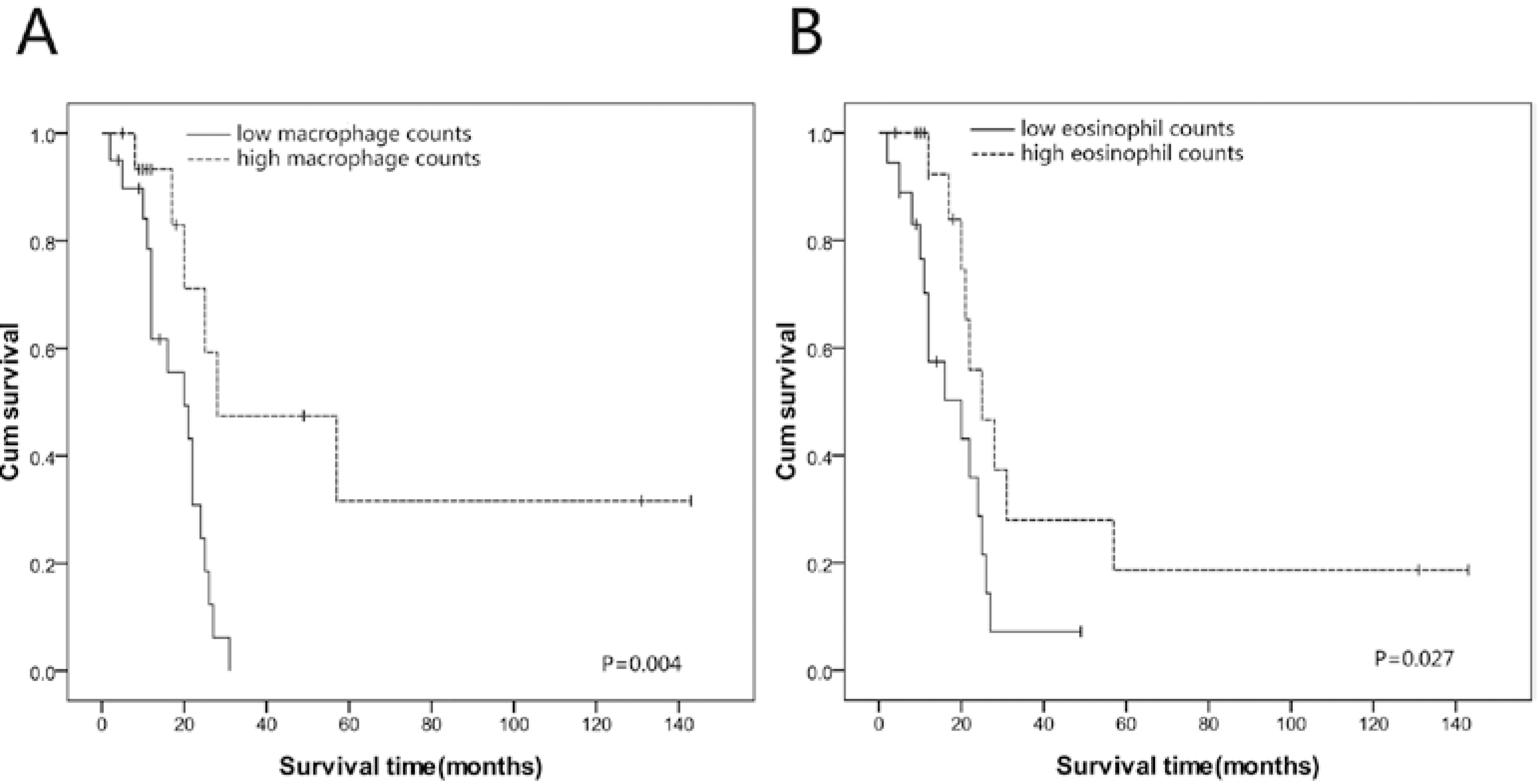
2.5. Survival Analyses
2.6. Inflammatory Cell Counts Associated with Survival in SmCEC Patients
| Feature | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | p | Hazard Ratio (95% CI) | p | |
| Macrophage counts | ||||
| Low vs. High | 0.247 (0.088–0.693) | 0.008 | - | - |
| Eosinophil counts | ||||
| Low vs. High | 0.386 (0.159–0.938) | 0.036 | 0.209 (0.078–0.559) | 0.002 |
| Chemotherapy | ||||
| Yes vs. No | 0.239 (0.092–0.623) | 0.003 | 0.133 (0.045–0.395) | 0.001 |
| pTNM stage | ||||
| I + II vs. III + IV | 1.139 (0.337–3.836) | 0.834 | - | - |
| Tumor size | ||||
| ≤4 cm vs. >4 cm | 1.096 (0.318–3.852) | 0.884 | - | - |
| Lymph node metastasis | ||||
| N0 vs. N1 + N2 | 0.847 (0.271–2.653) | 0.776 | - | - |
| Depth of invasion | ||||
| T1 + T2 vs. T3 + T4 | 1.526 (0.476–4.894) | 0.477 | - | - |
| Tumor location | ||||
| Mt vs. Ut + Lt | 1.326 (0.618–2.844) | 0.468 | - | - |
| Macroscopic tumor type | ||||
| Ulcerative + Medullary vs. Intraluminal + Mushroom | 1.082 (0.551–2.124) | 0.820 | - | - |
| Age | ||||
| ≤60 years vs. >60 years | 0.912 (0.283–2.938) | 0.877 | - | - |
| Sex | ||||
| Male vs. Female | 0.470 (0.136–1.628) | 0.234 | - | - |
2.7. Discussion
3. Experimental Section
3.1. Patients and Tissue Collection
3.2. Morphological Identification and Enumeration of Eosinophils, Neutrophils and Lymphocytes
3.3. Immunohistochemistry and Evaluation of CD68 (A Pan-Macrophage Marker)
3.4. Enumeration of Inflammatory Cells in ESqCC
3.5. Statistical Analysis
4. Conclusions
Supplementary Files
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Lv, J.; Liang, J.; Wang, J.; Wang, L.; He, J.; Xiao, Z.; Yin, W. Primary small cell carcinoma of the esophagus. J. Thorac. Oncol. 2008, 3, 1460–1465. [Google Scholar] [CrossRef]
- Lam, K.Y.; Law, S.; Tung, P.H.; Wong, J. Esophageal small cell carcinomas: Clinicopathologic parameters, p53 overexpression, proliferation marker, and their impact on pathogenesis. Arch. Pathol. Lab. Med. 2000, 124, 228–233. [Google Scholar]
- Sadanaga, N.; Morita, M.; Masuda, T.; Okada, S.; Sugiyama, M.; Ando, K.; Kakeji, Y.; Matsuura, H.; Maehara, Y. Clinical features of primary small cell carcinoma of the thoracic esophagus: A retrospective analysis of 12 surgically resected cases. Esophagus 2009, 6, 161–165. [Google Scholar] [CrossRef]
- Brenner, B.; Tang, L.H.; Shia, J.; Klimstra, D.S.; Kelsen, D.P. Small cell carcinomas of the gastrointestinal tract: clinopathological features and treatment approach. Semin. Oncol. 2007, 34, 43–50. [Google Scholar] [CrossRef]
- He, H.; Tian, D.; Guo, J.; Liu, M.; Chen, Z.; Hamdy, F.C.; Helleday, T.; Su, M.; Ying, S. DNA damage response in peritumoral regions of oesophageal cancer microenvironment. Carcinogenesis 2013, 34, 139–145. [Google Scholar] [CrossRef]
- Achyut, B.R.; Bader, D.A.; Robles, A.I.; Wangsa, D.; Harris, C.C.; Reid, T.; Yang, L. Inflammation-mediated genetic and epigenetic alterations drive cancer development in the neighboring epithelium upon stromal abrogation of TGF-β signaling. PLoS Genet. 2013, 9, e1003251. [Google Scholar]
- Shen, N.; Liu, Y.; Wang, Q.Y.; Shi, X.T.; Lu, C.D.; Ke, Y. Gene expression profiling study of HPV-16 positive and HPV-negative esophageal squamous cell carcinoma. Chin. J. Gastrointest. Surg. 2011, 14, 723–726. (In Chinese) [Google Scholar]
- Nguyen, G.H.; Schetter, A.J.; Chou, D.B.; Bowman, E.D.; Zhao, R.; Hawkes, J.E.; Mathe, E.A.; Kumamoto, K.; Zhao, Y.; Budhu, A.; et al. Inflammatory and microRNA gene expression as prognostic classifier of Barrett's-associated esophageal adenocarcinoma. Clin. Cancer Res. 2010, 16, 5824–5834. [Google Scholar] [CrossRef]
- Zhang, G.H.; Su, M.; Tian, D.P. Effect of chronic inflammation-induced basement membrane changes on esophageal carcinogenesis. Chin. J. Cancer 2005, 24, 1071–1075. (In Chinese) [Google Scholar]
- Shigeoka, M.; Urakawa, N.; Nakamura, T.; Nishio, M.; Watajima, T.; Kuroda, D.; Komori, T.; Kakeji, Y.; Semba, S.; Yokozaki, H. Tumor associated macrophage expressing CD204 is associated with tumor aggressiveness of esophageal squamous cell carcinoma. Cancer Sci. 2013, 104, 1112–1119. [Google Scholar] [CrossRef]
- Dutta, S.; Going, J.J.; Crumley, A.B.; Mohammed, Z.; Orange, C.; Edwards, J.; Fullarton, G.M.; Horgan, P.G.; McMillan, D.C. The relationship between tumour necrosis, tumour proliferation, local and systemic inflammation, microvessel density and survival in patients undergoing potentially curative resection of oesophageal adenocarcinoma. Br. J. Cancer 2012, 106, 702–710. [Google Scholar] [CrossRef]
- Guo, S.J.; Lin, D.M.; Li, J.; Liu, R.Z.; Zhou, C.X.; Wang, D.M.; Ma, WB; Zhang, Y.H.; Zhang, S.R. Tumor-associated macrophages and CD3-zeta expression of tumor-infiltrating lymphocytes in human esophageal squamous-cell carcinoma. Dis. Esophagus 2007, 20, 107–116. [Google Scholar] [CrossRef]
- Ishibashi, S.; Ohashi, Y.; Suzuki, T.; Miyazaki, S.; Moriya, T.; Satomi, S.; Sasano, H. Tumor-associated tissue eosinophilia in human esophageal squamous cell carcinoma. Anticancer Res. 2006, 26, 1419–1424. [Google Scholar]
- Ohashi, Y.; Ishibashi, S.; Suzuki, T.; Shineha, R.; Moriya, T.; Satomi, S.; Sasano, H. Significance of tumor associated tissue eosinophilia and other inflammatory cell infiltrate in early esophageal squamous cell carcinoma. Anticancer Res. 2000, 20, 3025–3030. [Google Scholar]
- Ohta, M.; Kitadai, Y.; Tanaka, S.; Yoshihara, M.; Yasui, W.; Mukaida, N.; Haruma, K.; Chayama, K. Monocyte chemoattractant protein-1 expression correlates with macrophage infiltration and tumor vascularity in human esophageal squamous cell carcinomas. Int. J. Cancer 2002, 102, 220–224. [Google Scholar] [CrossRef]
- Fukuchi, M.; Sakurai, S.; Suzuki, M.; Naitoh, H.; tabe, Y.; Fukasawa, T.; Kiriyama, S.; Yokobori, T.; Kuwano, H. Esophageal squamous cell carcinoma with marked eosinophil infiltration. Case Rep. Gastroenterol. 2011, 5, 648–653. [Google Scholar] [CrossRef]
- Lindau, D.; Gielen, P.; Kroesen, M.; Wesseling, P.; Adema, G.J. The immunosuppressive tumour network: Myeloid-derived suppressor cells, regulatory T cells and natural killer T cells. Immunology 2013, 138, 105–115. [Google Scholar] [CrossRef]
- Zarogoulidis, K.; Ziogas, E.; Boutsikou, E.; Zarogoulidis, P.; Darwiche, K.; Kontakiotis, T.; Tsakiridis, K.; Porpodis, K.; Latsios, D.; Chatzizisi, O.; et al. Immunomodifiers in combination with conventional chemotherapy in small cell lung cancer: a phase II, randomized study. Drug Des. Devel. Ther. 2013, 23, 611–617. [Google Scholar]
- Lu, L.; Pan, K.; Zheng, H.X.; Li, J.J.; Qiu, H.J.; Zhao, J.J.; Weng, D.S.; Pan, Q.Z.; Wang, D.D.; Jiang, S.S.; et al. IL-17A promotes immune cell recruitment in human esophageal cancers and the infiltrating dendritic cells represent a positive prognostic marker for patient survival. J. Immunother. 2013, 36, 451–458. [Google Scholar]
- Schäfer, G.; Kabanda, S.; van Rooyen, B.; Marušič, M.B.; Banks, L.; Parker, M.I. The role of inflammation in HPV infection of the Oesophagus. BMC Cancer 2013, 13. [Google Scholar] [CrossRef] [Green Version]
- Yousif, N.G.; Al-Amran, F.G.; Hadi, N.; Lee, J.; Adrienne, J. Expression of IL-32 modulates NF-κB and p38 MAP kinase pathways in human esophageal cancer. Cytokine 2013, 61, 223–227. [Google Scholar] [CrossRef]
- Miyashita, T.; Shah, F.A.; Miwa, K.; Sasaki, S.; Nishijima, K.; Oyama, K.; Ninomiya, I.; Fushida, S.; Fujimura, T.; Hattori, T.; et al. Impact of inflammation-metaplasia-adenocarcinoma sequence and prevention in surgical rat models. Digestion 2013, 87, 6–11. [Google Scholar] [CrossRef]
- Abdel-Latif, M.M.; Windle, H.; Terres, A.; Eidhin, D.N.; Kelleher, D.; Reynolds, J.V. Helicobacter pylori extract induces nuclear factor-kappa B, activator protein-1, and cyclooxygenase-2 in esophageal epithelial cells. J. Gastrointest. Surg. 2006, 10, 551–562. [Google Scholar] [CrossRef]
- Taccioli, C.; Chen, H.; Jiang, Y.; Liu, X.P.; Huang, K.; Smalley, K.J.; Farber, J.L.; Croce, C.M.; Fong, L.Y. Dietary zinc deficiency fuels esophageal cancer development by inducing a distinct inflammatory signature. Oncogene 2012, 31, 4550–4558. [Google Scholar] [CrossRef]
- Rauser, S.; Langer, R.; Tschernitz, S.; Gais, P.; Jütting, U.; Feith, M.; Höfler, H.; Walch, A. High number of CD45RO+ tumor infiltrating lymphocytes is an independent prognostic factor in non-metastasized (stage I-IIA) esophageal adenocarcinoma. BMC Cancer 2010, 10. [Google Scholar] [CrossRef]
- Eerola, A.K.; Soini, Y.; Paakko, P. A high number of tumor-infiltrating lymphocytes are associated with a small tumor size, low tumor stage, and a favorable prognosis in operated small cell lung carcinoma. Clin. Cancer Res. 2000, 6, 1875–1881. [Google Scholar]
- Fridman, W.H.; Pagès, F.; Sautès-Fridman, C.; Galon, J. The immune contexture in human tumours: Impact on clinical outcome. Nat. Rev. Cancer 2012, 12, 298–306. [Google Scholar] [CrossRef]
- Stein, H.J.; Feith, M.; Bruecher, B.L.; Naehrig, J.; Sarbia, M.; Siewert, J.R. Early esophageal cancer: pattern of lymphatic spread and prognostic factors for long-term survival after surgical resection. Ann. Surg. 2005, 242, 566–573. [Google Scholar]
- Mariette, C.; Finzi, L.; Piessen, G.; van Seuningen, I.; Triboulet, J.P. Esophageal carcinoma: Prognostic differences between squamous cell carcinoma and adenocarcinoma. World J. Surg. 2005, 29, 39–45. [Google Scholar] [CrossRef]
- Alidina, A.; Gaffar, A.; Hussain, F.; Islam, M.; Vaziri, I.; Burney, I.; Valimohd, A.; Jafri, W. Survival data and prognostic factors seen in Pakistani patients with esophageal cancer. Ann. Oncol. 2004, 15, 118–122. [Google Scholar] [CrossRef]
- Noguchi, T.; Takeno, S.; Kato, T.; Wada, S.; Noguchi, T.; Uchida, Y.; Kashima, K.; Yokoyama, S. Small cell carcinoma of the esophagus; clinicopathological and immunohistochemical analysis of six cases. Dis. Esophagus 2003, 16, 252–258. [Google Scholar] [CrossRef]
- Siveen, K.S.; Kuttan, G. Role of macrophages in tumour progression. Immunol. Lett. 2009, 123, 97–102. [Google Scholar] [CrossRef]
- Solinas, G.; Germano, G.; Mantovani, A.; Allavena, P. Tumor-associated macrophages (TAM) as major players of the cancer-related inflammation. J. Leukoc. Biol. 2009, 86, 1065–1073. [Google Scholar] [CrossRef]
- Murdoch, C.; Giannoudis, A.; Lewis, C.E. Mechanisms regulating the recruitment of macrophages into hypoxic areas of tumors and other ischemic tissues. Blood 2004, 104, 2224–2234. [Google Scholar] [CrossRef]
- Balkwill, F. Cancer and the chemokine network. Nat. Rev. Cancer 2004, 4, 540–550. [Google Scholar] [CrossRef]
- Allavena, P.; Sica, A.; Solinas, G.; Porta, C.; Mantovani, A. The inflammatory micro-environment in tumor progression: the role of tumor-associated macrophages. Crit. Rev. Oncol. Hematol. 2008, 66, 1–9. [Google Scholar]
- Coffelt, S.B.; Scandurro, A.B. Tumors sound the alarmin (s). Cancer Res. 2008, 68, 6482–6485. [Google Scholar] [CrossRef]
- Dorta, R.G.; Landman, G.; Kowalski, L.P.; Lauris, J.R.; Latorre, M.R.; Oliveira, D.T. Tumour-associated tissue eosinophilia as a prognostic factor in oral squamous cell carcinomas. Histopathology 2002, 41, 152–157. [Google Scholar]
- Nielsen, H.J.; Hansen, U.; Christensen, I.J.; Reimert, C.M.; Brünner, N.; Moesgaard, F. Independent prognostic value of eosinophil and mast cell infiltration in colorectal cancer tissue. J. Pathol. 1999, 189, 487–495. [Google Scholar] [CrossRef]
- Teruya-Feldstein, J.; Jaffe, E.S.; Burd, P.R.; Kingma, D.W.; Setsuda, J.E.; Tosato, G. Differential chemokine expression in tissues involved by Hodgkin’s disease: direct correlation of eotaxin expression and tissue eosinophilia. Blood 1999, 93, 2463–2470. [Google Scholar]
- Looi, L.M. Tumor-associated tissue eosinophilia in nasopharyngeal carcinoma. A pathologic study of 422 primary and 138 metastatic tumors. Cancer 1987, 59, 466–470. [Google Scholar] [CrossRef]
- Lorena, S.C.; Oliveira, D.T.; Dorta, R.G.; Landman, G.; Kowalski, L.P. Eotaxin expression in oral squamous cell carcinomas with and without tumour associated tissue eosinophilia. Oral Dis. 2003, 9, 279–283. [Google Scholar] [CrossRef]
- Gulubova, M.; Ananiev, J.; Yovchev, Y.; Julianov, A.; Karashmalakov, A.; Vlaykova, T. The density of macrophages in colorectal cancer is inversely correlated to TGF-β1 expression and patients’ survival. J. Mol. Histol. 2013, 44, 679–692. [Google Scholar] [CrossRef]
- Mantovani, A.; Sica, A. Macrophages, innate immunity and cancer: balance, tolerance, and diversity. Curr. Opin. Immunol. 2010, 22, 231–237. [Google Scholar] [CrossRef]
- Qian, B.Z.; Pollard, J.W. Macrophage diversity enhances tumor progression and metastasis. Cell 2010, 141, 39–51. [Google Scholar] [CrossRef]
- Kurahara, H.; Takao, S.; Maemura, K.; Mataki, Y.; Kuwahata, T.; Maeda, K.; Sakoda, M.; Iino, S.; Ishigami, S.; Ueno, S.; et al. M2-polarized tumor-associated macrophage infiltration of regional lymph nodes is associated with nodal lymphangiogenesis and occult nodal involvement in pN0 pancreatic cancer. Pancreas 2013, 42, 155–159. [Google Scholar] [CrossRef]
- Algars, A.; Irjala, H.; Vaittinen, S.; Huhtinen, H.; Sundström, J.; Salmi, M.; Ristamäki, R.; Jalkanen, S. Type and location of tumor-infiltrating macrophages and lymphatic vessels predict survival of colorectal cancer patients. Int. J. Cancer 2012, 131, 864–873. [Google Scholar] [CrossRef]
- Forssell, J.; Oberg, A.; Henriksson, M.L.; Stenling, R.; Jung, A.; Palmqvist, R. High macrophage infiltration along the tumor front correlates with improved survival in colon cancer. Clin. Cancer Res. 2007, 13, 1472–1479. [Google Scholar] [CrossRef]
- Oberg, A.; Samii, S.; Stenling, R.; Lindmark, G. Different occurrence of CD8+, CD45R0+, and CD68+ immune cells in regional lymph node metastases from colorectal cancer as potential prognostic predictors. Int. J. Colorectal Dis. 2002, 17, 25–29. [Google Scholar] [CrossRef]
- Sica, A.; Schioppa, T.; Mantovani, A.; Allavena, P. Tumour associated macrophages are distinct M2 polarised population promoting tumour progression: potential targets of anti-cancer therapy. Eur. J. Cancer 2006, 42, 717–727. [Google Scholar] [CrossRef]
- Ladoire, S.; Martin, F.; Ghiringhelli, F. Prognostic role of FOXP3+ regulatory T cells infiltrating human carcinomas: The paradox of colorectal cancer. Cancer Immunol. Immunother. 2011, 60, 909–918. [Google Scholar] [CrossRef]
- Ohno, S.; Inagawa, H.; Dhar, D.K.; Fujii, T.; Ueda, S.; Tachibana, M.; Suzuki, N.; Inoue, M.; Soma, G.; Nagasue, N. The degree of macrophage infiltration into the cancer cell nest is a significant predictor of survival in gastric cancer patients. Anticancer Res. 2003, 23, 5015–5022. [Google Scholar]
- Fiumara, A.; Belfiore, A.; Russo, G.; Salomone, E.; Santonocito, G.M.; Ippolito, O.; Vigneri, R.; Gangemi, P. In situ evidence of neoplastic cell phagocytosis by macrophages in papillary thyroid cancer. J. Clin. Endocrinol. Metab. 1997, 82, 1615–1620. [Google Scholar]
- Mukhtar, R.A.; Moore, A.P.; Tandon, V.J.; Nseyo, O.; Twomey, P.; Adisa, C.A.; Eleweke, N.; Au, A.; Baehner, F.L.; Moore, D.H.; et al. Elevated levels of proliferating and recently migrated tumor associated macrophages confer increased aggressiveness and worse outcomes in breast cancer. Ann. Surg. Oncol. 2012, 19, 3979–3986. [Google Scholar] [CrossRef]
- Nonomura, N.; Takayama, H.; Nakayama, M.; Nakai, Y.; Kawashima, A.; Mukai, M.; Nagahara, A.; Aozasa, K.; Tsujimura, A. Infiltration of tumour-associated macrophages in prostate biopsy specimens is predictive of disease progression after hormonal therapy for prostate cancer. BJU Int. 2011, 107, 1918–1922. [Google Scholar] [CrossRef]
- Caruso, R.A.; Fedele, F.; Parisi, A.; Paparo, D.; Bonanno, A.; Finocchiaro, G.; Branca, G.; Scardigno, M.; Rigoli, L. Chronic allergic-like inflammation in the tumor stroma of human gastric carcinomas: an ultrastructural study. Ultrastruct. Pathol. 2012, 36, 139–144. [Google Scholar] [CrossRef]
- Cuschieri, A.; Talbot, I.C.; Weeden, S. MRC Upper GI Cancer Working Party: Influence of pathological tumour variables on long-term survival in resectable gastric cancer. Br. J. Cancer 2002, 86, 674–679. [Google Scholar] [CrossRef]
- Fernández-Aceñero, M.J.; Galindo-Gallego, M.; Sanz, J.; Aljama, A. Prognostic influence of tumor-associated eosinophilic infiltrate in colorectal carcinoma. Cancer 2000, 88, 1544–1548. [Google Scholar] [CrossRef]
- Tajima, K.; Yamakawa, M.; Inaba, Y.; Katagiri, T.; Sasaki, H. Cellular location of interleukin-5 expression in rectal carcinoma with eosinophilia. Hum. Pathol. 1998, 29, 1024–1027. [Google Scholar] [CrossRef]
- Trulson, A.; Nilsson, S.; Venge, P. The eosinophil granule proteins in serum, but not the oxidative metabolism of the blood eosinophils, are increased in cancer. Br. J. Haematol. 1997, 98, 312–314. [Google Scholar]
- Neves, J.S.; Weller, P.F. Functional extracellular eosinophil granules: novel implications in eosinophil immunobiology. Curr. Opin. Immunol. 2009, 21, 694–699. [Google Scholar] [CrossRef]
- Ellyard, J.I.; Simson, L.; Parish, C.R. Th2-mediated anti-tumour immunity: Friend or foe? Tissue Antigens 2007, 70, 1–11. [Google Scholar] [CrossRef]
- Pryor, J.G.; Simon, R.A.; Bourne, P.A.; Spaulding, B.O.; Scott, G.A.; Xu, H. Merkel cell carcinoma expresses K homology domain-containing protein overexpressed in cancer similar to other high-grade neuroendocrine carcinomas. Hum. Pathol. 2008, 40, 238–243. [Google Scholar]
- Klintrup, K.; Mäkinen, J.M.; Kauppila, S.; Väre, P.O.; Melkko, J.; Tuominen, H.; Tuppurainen, K.; Mäkelä, J.; Karttunen, T.J.; Mäkinen, M.J. Inflammation and prognosis in colorectal cancer. Eur. J. Cancer 2005, 41, 2645–2654. [Google Scholar] [CrossRef]
- Furihata, M.; Ohtsuki, Y.; Sonobe, H.; Araki, K.; Ogata, T.; Toki, T.; Ogoshi, S.; Tamiya, T. Prognostic significance of simultaneous infiltration of HLA-DR-positive dendritic cells and tumor infiltrating lymphocytes into human esophageal carcinoma. Tohoku J. Exp. Med. 1993, 169, 187–195. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Zhang, Y.; Ren, H.; Wang, L.; Ning, Z.; Zhuang, Y.; Gan, J.; Chen, S.; Zhou, D.; Zhu, H.; Tan, D.; et al. Clinical Impact of Tumor-Infiltrating Inflammatory Cells in Primary Small Cell Esophageal Carcinoma. Int. J. Mol. Sci. 2014, 15, 9718-9734. https://doi.org/10.3390/ijms15069718
Zhang Y, Ren H, Wang L, Ning Z, Zhuang Y, Gan J, Chen S, Zhou D, Zhu H, Tan D, et al. Clinical Impact of Tumor-Infiltrating Inflammatory Cells in Primary Small Cell Esophageal Carcinoma. International Journal of Molecular Sciences. 2014; 15(6):9718-9734. https://doi.org/10.3390/ijms15069718
Chicago/Turabian StyleZhang, Yuling, Hongzheng Ren, Lu Wang, Zhifeng Ning, Yixuan Zhuang, Jinfeng Gan, Shaobin Chen, David Zhou, Hua Zhu, Dongfeng Tan, and et al. 2014. "Clinical Impact of Tumor-Infiltrating Inflammatory Cells in Primary Small Cell Esophageal Carcinoma" International Journal of Molecular Sciences 15, no. 6: 9718-9734. https://doi.org/10.3390/ijms15069718




