Enhanced and Extended Anti-Hypertensive Effect of VP5 Nanoparticles
Abstract
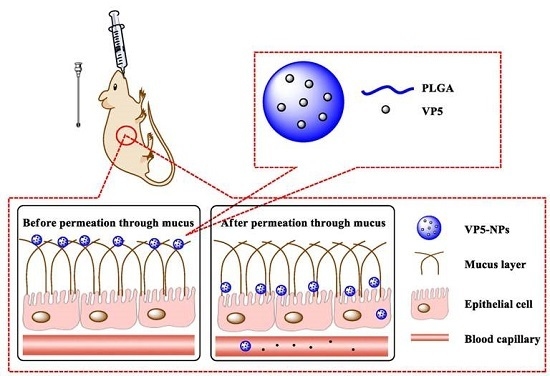
:1. Introduction
2. Results
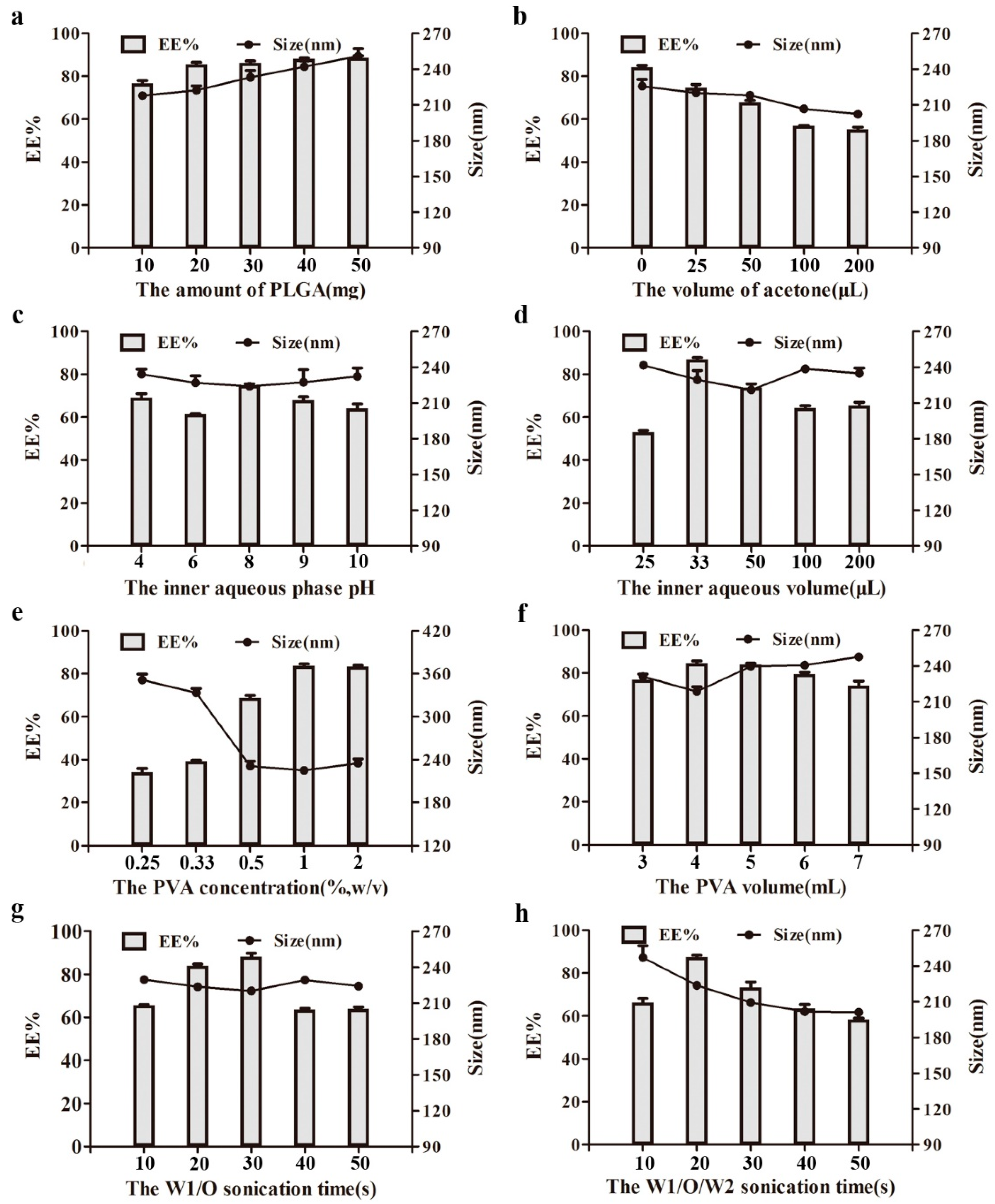
2.1. Optimization of Preparation Variables of VP5-NPs
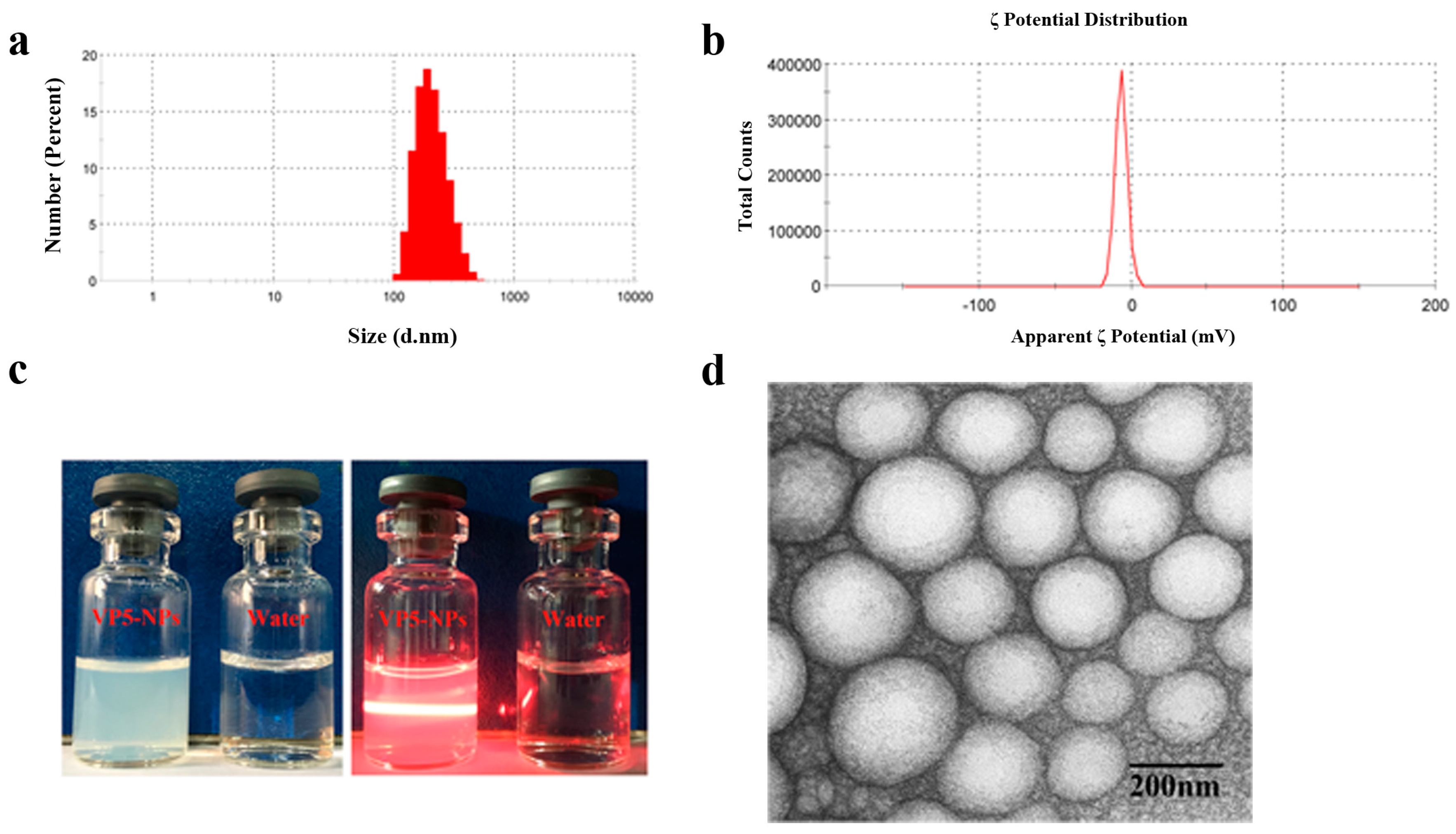
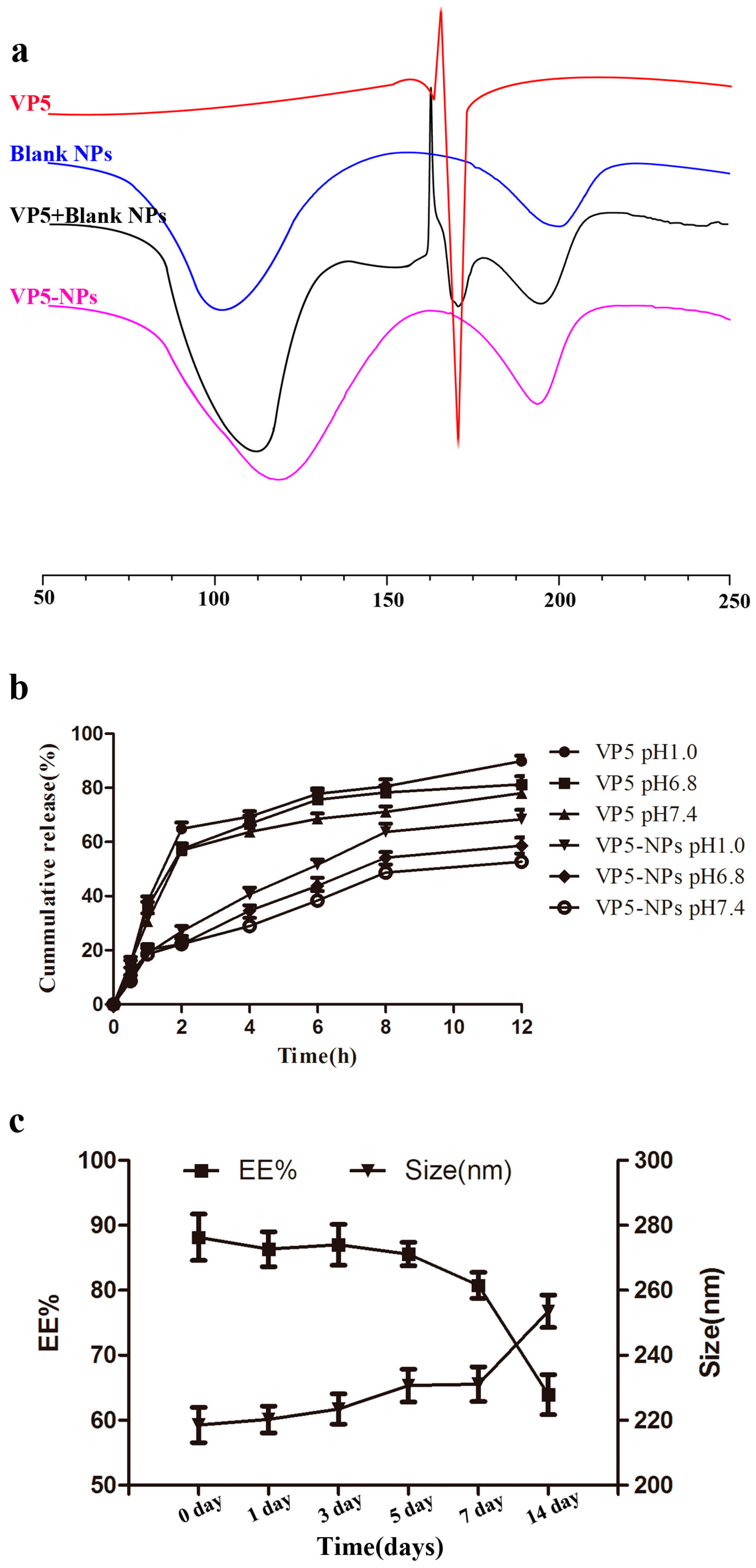
2.2. Characterization of VP5-NPs
2.3. In Vivo Antihypertensive Efficacy
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Preparation of VP5-NPs
4.3. Characterization of VP5-NPs
4.3.1. Particle Size and ζ Potential
4.3.2. Entrapment Efficiency and Drug Loading
4.3.3. Appearance
4.3.4. Differential Scanning Calorimetry (DSC)
4.3.5. In Vitro Release
4.3.6. Stability
4.4. In Vivo Antihypertensive Efficacy
4.5. Statistical Analysis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ACE | Angiotensin converting enzyme |
| VP5 | Val-Leu-Pro-Val-Pro |
| RAAS | Renin-angiotensin-aldosterone system |
| ARB | Angiotensin receptor blocker |
| SBP | Systolic blood pressure |
| DBP | Diastolic blood pressure |
| IPP | Ile-Pro-Pro |
| VPP | Val-Pro-Pro |
| GI | Gastrointestinal |
| BPL | Blood pressure-lowering |
References
- World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis—World Health Day 2013; WHO Press: Geneva, Switzerland, 2013. [Google Scholar]
- Soltani, Z.; Washco, V.; Morse, S.; Reisin, E. The impacts of obesity on the cardiovascular and renal systems: Cascade of events and therapeutic approaches. Curr. Hypertens. Rep. 2015, 17, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Geng, X.; Tian, G.; Zhang, W.; Zhao, Y.; Zhao, L.; Wang, H.; Ng, T.B. A Tricholoma matsutake peptide with angiotensin converting enzyme inhibitory and antioxidative activities and antihypertensive effects in spontaneously hypertensive rats. Sci. Rep. 2016, 6, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Marques, C.; Amorim, M.M.; Pereira, J.O.; Guardão, L.; João, M.M.; Pintado, E.M.; Moura, D.; Calhau, C.; Pinheiro, H. In vitro, ACE-inhibitory peptide KGYGGVSLPEW facilitates noradrenaline release from sympathetic nerve terminals: Relationship with the lack of antihypertensive effect on spontaneous hypertensive rats. Peptides 2015, 71, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Cicero, A.F.; Aubin, F.; Az6kiais-Braesco, V.; Borghi, C. Do the lactotripeptides isoleucine-proline-proline and valine-proline-proline reduce systolic blood pressure in European subjects? A meta-analysis of randomized controlled trials. Am. J. Hypertens. 2013, 26, 442–449. [Google Scholar] [PubMed]
- Muheem, A.; Shakeel, F.; Jahangir, M.A.; Anwar, M.; Mallick, N.; Jain, G.K.; Warsi, M.H.; Ahmad, F.J. A review on the strategies for oral delivery of proteins and peptides and their clinical perspectives. Saudi Pharm. J. 2016, 24, 413–428. [Google Scholar] [CrossRef] [PubMed]
- Niu, Z.; Conejos-Sánchez, I.; Griffin, B.T.; O’Driscoll, C.M.; Alonso, M.J. Lipid-based nanocarriers for oral peptide delivery. Adv. Drug. Deliv. Rev. 2016. [Google Scholar] [CrossRef] [PubMed]
- García-Díaz, M.; Foged, C.; Nielsen, H.M. Improved insulin loading in poly (lactic-co-glycolic) acid (PLGA) nanoparticles upon self-assembly with lipids. Int. J. Pharm. 2015, 482, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Sheng, J.; Han, L.; Jing, Q.; Ru, G.; Li, R.; Wu, L.; Cui, D.; Yang, P.; He, Y.; Wang, J. N-Trimethyl chitosan chloride-coated PLGA nanoparticles overcoming multiple barriers to oral insulin absorption. ACS. Appl. Mater. Interfaces 2015, 7, 15430–15441. [Google Scholar] [CrossRef] [PubMed]
- Yan, L.; Wang, H.; Jiang, Y.; Liu, J.; Wang, Z.; Yang, Y.; Huang, S.; Huang, Y. Cell-penetrating peptide-modified PLGA nanoparticles for enhanced nose-to-brain macromolecular delivery. Macromol. Res. 2013, 21, 435–441. [Google Scholar] [CrossRef]
- Wang, H.; Zhao, Y.; Wang, H.; Gong, J.; He, H.; Shin, M.C.; Yang, V.C.; Huang, Y. Low-molecular-weight protamine-modified PLGA nanoparticles for overcoming drug-resistant breast cancer. J. Control. Release 2014, 192, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Hiremath, J.; Kang, K.I.; Xia, M.; Elaish, M.; Binjawadagi, B.; Ouyang, K.; Dhakal, S.; Arcos, J.; Torrelles, J.B.; Jiang, X.; et al. Entrapment of H1N1 influenza virus derived conserved peptides in PLGA nanoparticles enhances T cell response and vaccine efficacy in pigs. PLoS ONE 2016, 11, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Hosseininasab, S.; Pashaei-Asl, R.; Khandaghi, A.A.; Nasrabadi, H.T.; Nejati-Koshki, K.; Akbarzadeh, A.; Joo, S.W.; Hanifehpour, Y.; Davaran, S. Synthesis, characterization, and in vitro studies of PLGAPEG nanoparticles for oral insulin delivery. Chem. Biol. Drug Des. 2014, 84, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Reix, N.; Parat, A.; Seyfritz, E.; van Der Werf, R.; Epure, V.; Ebel, N.; Danicher, L.; Marchioni, E.; Jeandidier, N.; Pinget, M.; et al. In vitro uptake evaluation in Caco-2 cells and in vivo results in diabetic rats of insulin-loaded PLGA nanoparticles. Int. J. Pharm. 2012, 437, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.Y.; Fang, K.W.; Liu, D. The acute antihypertensive effects of recombinant angiotensin converting enzyme inhibitory peptides on spontaneously hypertensive rats. Chin. J. Hypertens. 2010, 18, 91–94. [Google Scholar]
- Xu, B.; Jin, Q.S.; Zeng, J.; Yu, T.; Chen, Y.; Li, S.Z.; Gong, D.Q.; He, L.L.; Tan, X.Y.; Li, Y.; et al. Combined tumor- and neovascular- “dual targeting” gene/chemo-therapy suppresses tumor growth and angiogenesis. ACS. Appl. Mater. Interfaces 2016, 8, 25753–25769. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, T.C.; Kulak, N.; Pridgen, E.M.; Farokhzad, O.C.; Langer, R.; Lippard, S.J. Nanoparticle encapsulation of mitaplatin and the effect thereof on in vivo properties. ACS Nano 2013, 7, 5675–5683. [Google Scholar] [CrossRef] [PubMed]
- Turk, C.T.; Oz, U.C.; Serim, T.M.; Hascicek, C. Formulation and optimization of nonionic surfactants emulsified nimesulide-loaded PLGA-based nanoparticles by design of experiments. AAPS Pharm. Sci. Tech. 2014, 15, 161–176. [Google Scholar] [CrossRef] [PubMed]
- Kiss, N.; Brenn, G.; Pucher, H.; Wieser, J.; Scheler, S.; Jennewein, H.; Suzzi, D.; Khinast, J. Formation of O/W emulsions by static mixers for pharmaceutical applications. Chem. Eng. Sci. 2011, 66, 5084–5094. [Google Scholar] [CrossRef]
- Sun, D.; Xue, A.; Zhang, B.; Xue, X.; Zhang, J.; Liu, W. Enhanced oral bioavailability of acetylpuerarin by poly (lactide-co-glycolide) nanoparticles optimized using uniform design combined with response surface methodology. Drug Des. Dev. Ther. 2016, 10, 2029–2039. [Google Scholar] [CrossRef] [PubMed]
- Anarjan, N.; Tan, C.; Ling, T.; Lye, K.L.; Malmiri, H.J.; Nehdi, I.A.; Cheah, Y.K.; Mirhosseini, H.; Baharin, B.S. Effect of organic-phase solvents on physicochemical properties and cellular uptake of astaxanthin nanodispersions. J. Agric. Food Chem. 2011, 59, 8733–8741. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Xia, S.; Wang, F.Z.; Jin, Q.S.; Yu, T.; He, L.L.; Chen, Y.; Liu, Y.M.; Li, S.Z.; Tan, X.Y.; et al. Polymeric nanomedicine for combined gene/chemotherapy elicits enhanced tumor suppression. Mol. Pharm. 2016, 13, 663–676. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Anderko, A. Modeling interfacial tension in liquid-liquid systems containing electrolytes. Ind. Eng. Chem. Res. 2013, 52, 6822–6840. [Google Scholar] [CrossRef]
- Fang, D.; Chen, Y.; Xu, B.; Ren, K.; He, Z.; He, L.; Lei, Y.; Fan, C.; Song, X. Development of lipid-shell and polymer core nanoparticles with water-soluble salidroside for anti-cancer therapy. Int. J. Mol. Sci. 2014, 15, 3373–3388. [Google Scholar] [CrossRef] [PubMed]
- Chitkara, D.; Kumar, N. BSA-PLGA-based core-shell nanoparticles as carrier system for water-soluble drugs. Pharm. Res. 2013, 30, 2396–2409. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.L.; Rosalia, R.A.; Sazak, A.; Carstens, M.G.; Ossendorp, F.; Oostendorp, J.; Jiskoot, W. Optimization of encapsulation of a synthetic long peptide in PLGA nanoparticles: Low-burst release is crucial for efficient CD8+, T cell activation. Eur. J. Pharm. Biopharm. 2013, 83, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Sang, C.L. Effect of volume ratio of internal aqueous phase to organic membrane phase (W/O ratio) of water-in-oil emulsion on penicillin G extraction by emulsion liquid membrane. J. Memb. Sci. 1999, 163, 193–201. [Google Scholar]
- Li, L.; Zheng, S.; Huang, Y.; Qin, T.; Xing, J.; Niu, Y.; Bo, R.; Liu, Z.; Huang, Y.; Hu, Y.L.; et al. Preparation and characterization of Chinese yam polysaccharide PLGA nanoparticles and their immunological activity. Int. J. Pharm. 2016, 511, 140–150. [Google Scholar]
- Galindo-Rodriguez, S.; Allémann, E.; Fessi, H.; Doelker, E. Physicochemical parameters associated with nanoparticle formation in the salting-out, emulsification-diffusion, and nanoprecipitation methods. Pharm. Res. 2004, 21, 1428–1439. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Yu, Z.; Wu, W.; Bi, Y.; Cai, Z.; Chen, Q.H.; Li, Y.B.; Hou, S. PLGA nanoparticles simultaneously loaded with vincristine sulfate and verapamil hydrochloride: Systematic study of particle size and drug entrapment efficiency. Int. J. Pharm. 2008, 350, 320–329. [Google Scholar] [CrossRef] [PubMed]
- Halayqa, M.; Domańska, U. PLGA biodegradable nanoparticles containing perphenazine or chlorpromazine hydrochloride: Effect of formulation and release. Int. J. Mol. Sci. 2014, 15, 23909–23923. [Google Scholar] [CrossRef] [PubMed]
- Morales-Cruz, M.; Flores-Fernández, G.M.; Morales-Cruz, M.; Orellano, E.A.; Rodriguez-Martinez, J.A.; Ruiz, M.; Griebenow, K. Two-step nanoprecipitation for the production of protein-loaded PLGA nanospheres. Results Pharm. Sci. 2012, 2, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Gentile, P.; Nandagiri, V.K.; Pabari, R.; Daly, J.; Tonda-Turo, C.; Ciardelli, G.; Ramtoola, Z. Influence of Parathyroid Hormone-loaded PLGA Nanoparticles in porous scaffolds for bone regeneration. Int. J. Mol. Sci. 2015, 16, 20492–20510. [Google Scholar] [CrossRef] [PubMed]
- Mishra, A.; Vuddanda, P.R.; Singh, S. Intestinal lymphatic delivery of praziquantel by solid lipid Nanoparticles: Formulation Design, in vitro and in vivo Studies. J. Nanotechnol. 2014, 2014, 1–12. [Google Scholar] [CrossRef]
- Li, J.; He, Z.; Yu, S.; Li, S.; Ma, Q.; Yu, Y.; Zhang, J.; Li, R.; Zheng, Y.; He, G.; et al. Micelles based on methoxy poly (ethylene glycol)-cholesterol conjugate for controlled and targeted drug delivery of a poorly water soluble drug. J. Biomed. Nanotechnol. 2012, 8, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Mu, L.; Feng, S. A novel controlled release formulation for the anticancer drug paclitaxel (Taxol®): PLGA nanoparticles containing vitamin E TPGS. J. Control. Release 2003, 86, 33–48. [Google Scholar] [CrossRef]
- Joffe, P.; Ladefoged, S.D.; Cintin, C.; Lehmann, H. 1 α-Hydroxycholecalciferol adsorption to peritoneal dialysis bags: Influence of time, glucose concentration, temperature, and albumin. Nephrol. Dial. Transplant. 1992, 7, 1249–1251. [Google Scholar] [PubMed]
- Wei, J.; Fang, Y.; Seyednejad, H.; Chen, Z.; Hennink, W.E.; Anderson, J.M.; van den Beucken, J.J.; Jansen, J.A. Biocompatibility and degradation characteristics of PLGA-based electrospun nanofibrous scaffolds with nanoapatite incorporation. Biomaterials 2012, 33, 6604–6614. [Google Scholar]
- Voruganti, S.; Qin, J.J.; Sarkar, S.; Nag, S.; Walbi, I.A.; Wang, S.; Zhao, Y.; Wang, W.; Zhang, R. Oral nano-delivery of anticancer ginsenoside 25-OCH3-PPD, a natural inhibitor of the MDM2 oncogene: Nanoparticle preparation, characterization, in vitro and in vivo anti-prostate cancer activity, and mechanisms of action. Oncotarget 2015, 6, 21379–21394. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, M.; Gomez-Orellana, I. Challenges for the oral delivery of macromolecules. Nat. Rev. Drug Discov. 2003, 2, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Chen, S.; Gao, Y.; Guo, F.; Li, F.; Xie, B.; Zhou, J.; Zhong, H. Enhanced oral bioavailability of insulin using PLGA nanoparticles co-modified with cell-penetrating peptides and Engrailed secretion peptide (Sec). Drug Deliv. 2016, 23, 1980–1991. [Google Scholar] [CrossRef] [PubMed]
- Maisel, K.; Ensign, L.; Reddy, M.; Cone, R.; Hanes, J. Effect of surface chemistry on nanoparticle interaction with gastrointestinal mucus and distribution in the gastrointestinal tract following oral and rectal administration in the mouse. J. Control. Release 2015, 197, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Renukuntla, J.; Vadlapudi, A.D.; Patel, A.; Boddu, S.H.S.; Mitra, A.K. Approaches for enhancing oral bioavailability of peptides and proteins. Int. J. Pharm. 2013, 447, 75–93. [Google Scholar] [CrossRef] [PubMed]
- Bernkop-Schnürch, A. The use of inhibitory agents to overcome the enzymatic barrier to perorally administered therapeutic peptides and proteins. J. Control. Release 1998, 52, 1–16. [Google Scholar] [CrossRef]
- Fan, T.; Chen, C.; Guo, H.; Xu, J.; Zhang, J.; Zhu, X.; Yang, Y.; Zhou, Z.; Li, L.; Huang, Y. Design and evaluation of solid lipid nanoparticles modified with peptide ligand for oral delivery of protein drugs. Eur. J. Pharm. Biopharm. 2014, 88, 518–528. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.; Hwang, B.H.; Doshi, N.; Mitragotri, S. A permeation enhancer for increasing transport of therapeutic macromolecules across the intestine. J. Control. Release 2013, 172, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Zhang, Y.; Feng, J.; Gu, T.; Dong, Q.; Yang, X.; Sun, Y.; Wu, Y.; Chen, Y.; Kong, W. Preparation, characterization, and in vitro and in vivo investigation of chitosan-coated poly (d,l-lactide-co-glycolide) nanoparticles for intestinal delivery of exendin-4. Int. J. Nanomed. 2013, 8, 1141–1154. [Google Scholar]
- He, C.; Yin, L.; Tang, C.; Yin, C. Size-dependent absorption mechanism of polymeric nanoparticles for oral delivery of protein drugs. Biomaterials 2012, 33, 8569–8578. [Google Scholar] [CrossRef] [PubMed]
- Krishnamachari, Y.; Madan, P.; Lin, S. Development of pH-and time-dependent oral microparticles to optimize budesonide delivery to ileum and colon. Int. J. Pharm. 2007, 338, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Yamada, Y.; Matoba, N.; Usui, H.; Onishi, K.; Yoshikawa, M. Design of a highly potent anti-hypertensive peptide based on ovokinin (2–7). Biosci. Biotechnol. Biochem. 2002, 66, 1213–1217. [Google Scholar] [CrossRef] [PubMed]
- Derman, S.; Mustafaeva, Z.A.; Abamor, E.S.; Bagirova, M.; Allahverdiyev, A. Preparation, characterization and immunological evaluation: Canine parvovirus synthetic peptide loaded PLGA nanoparticles. J. Biomed Sci. 2015, 22, 1–12. [Google Scholar] [CrossRef] [PubMed]
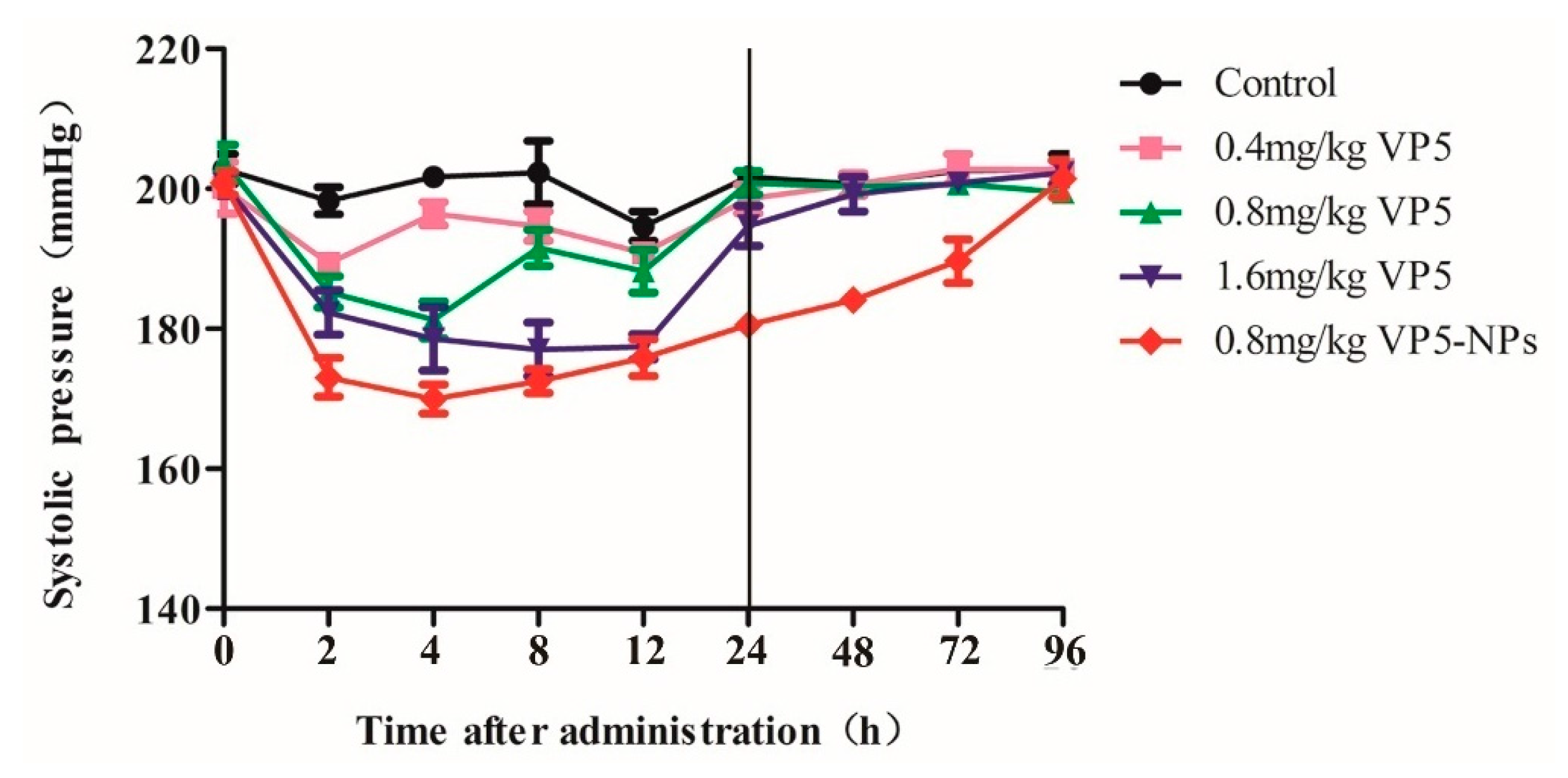
| Time | Group Control | ||||
|---|---|---|---|---|---|
| Saline Group | 0.4 mg/kg VP5 | 0.8 mg/kg VP5 | 1.6 mg/kg VP5 | 0.8 mg/kg VP5-NPs | |
| 2 h | 4.5 ± 3.2 | 10.0 ± 1.3 *** | 13.4 ± 2.2 *** | 17.7 ± 3.8 *** | 26.7 ± 3.7 *** |
| 4 h | 1.2 ± 0.6 | 5.2 ± 1.9 * | 20.2 ± 3.6 *** | 18.5 ± 5.8 *** | 31.7 ± 2.3 *** |
| 8 h | 1.0 ± 4.7 | 8.2 ± 2.6 | 12.4 ± 2.3 | 20.9 ± 4.2 *** | 28.9 ± 1.9 *** |
| 12 h | 8.2 ± 1.2 | 9.4 ± 1.3 | 15.8 ± 3.7 | 19.5 ± 3.0 *** | 23.6 ± 3.8 *** |
| 24 h | 1.2 ± 1.5 | 1.6 ± 1.6 | 3.5 ± 0.8 | 6.0 ± 3.4 | 21.5 ± 0.7 *** |
| 48 h | 2.2 ± 1.6 | −0.5 ± 1.8 | 2.4 ± 1.2 | 1.5 ± 2.5 | 20.4 ± 1.0 *** |
| 72 h | 0.3 ± 1.5 | −2.7 ± 1.1 | 3.2 ± 1.6 | −0.1 ± 1.0 | 18.7 ± 3.9 *** |
| 96 h | 0.6 ± 0.5 | −2.6 ± 2.7 | 4.4 ± 0.7 | −1.6 ± 1.4 | −0.6 ± 3.5 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, T.; Zhao, S.; Li, Z.; Wang, Y.; Xu, B.; Fang, D.; Wang, F.; Zhang, Z.; He, L.; Song, X.; et al. Enhanced and Extended Anti-Hypertensive Effect of VP5 Nanoparticles. Int. J. Mol. Sci. 2016, 17, 1977. https://doi.org/10.3390/ijms17121977
Yu T, Zhao S, Li Z, Wang Y, Xu B, Fang D, Wang F, Zhang Z, He L, Song X, et al. Enhanced and Extended Anti-Hypertensive Effect of VP5 Nanoparticles. International Journal of Molecular Sciences. 2016; 17(12):1977. https://doi.org/10.3390/ijms17121977
Chicago/Turabian StyleYu, Ting, Shengnan Zhao, Ziqiang Li, Yi Wang, Bei Xu, Dailong Fang, Fazhan Wang, Zhi Zhang, Lili He, Xiangrong Song, and et al. 2016. "Enhanced and Extended Anti-Hypertensive Effect of VP5 Nanoparticles" International Journal of Molecular Sciences 17, no. 12: 1977. https://doi.org/10.3390/ijms17121977