Long-Term Treatment with Citicoline Prevents Cognitive Decline and Predicts a Better Quality of Life after a First Ischemic Stroke
Abstract
:1. Introduction
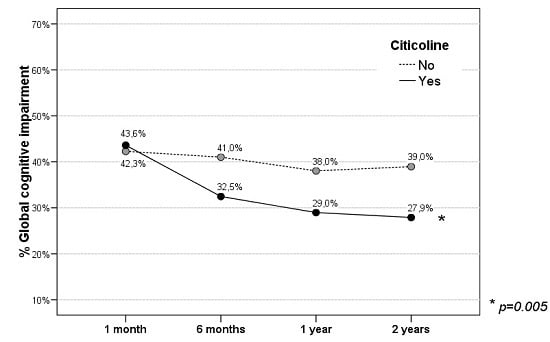
2. Results
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Quality of Life
4.3. Statistical Analysis
Author Contributions
Conflicts of Interest
Abbreviations
| QoL | Quality of Life |
| VAS | Visual Analogue Scale |
| NIHSS | National Institutes of Health Stroke Scale |
| TIA | Transient Ischemic Attack |
| PAD | Peripheral Arterial Disease |
| GCI | Global Cognitive Impairment |
References
- Feigin, V.L.; Forouzanfar, M.H.; Krishnamurthi, R.; Mensah, G.A.; Connor, M.; Bennett, D.A.; Moran, A.E.; Sacco, R.L.; Anderson, L.; Truelsen, T.; et al. Global and regional burden of stroke during 1990–2010: Findings from the Global Burden of Disease Study 2010. Lancet 2014, 383, 245–254. [Google Scholar] [CrossRef]
- Rajan, K.B.; Aggarwal, N.T.; Wilson, R.S.; Everson Rose, S.A.; Evans, D.A. Association of cognitive functioning, incident stroke, and mortality in older adults. Stroke 2014, 45, 2563–2567. [Google Scholar] [CrossRef] [PubMed]
- Barker Collo, S.; Feigin, V.L.; Parag, V.; Lawes, C.M.; Senior, H. Auckland Stroke Outcomes Study. Part 2: Cognition and functional outcomes 5 years poststroke. Neurology 2010, 75, 1608–1616. [Google Scholar] [CrossRef] [PubMed]
- Alvarez Sabín, J.; Román, G.C. Citicoline in vascular cognitive impairment and vascular dementia after stroke. Stroke 2011, 42 (Suppl. S1), S40–S43. [Google Scholar] [CrossRef] [PubMed]
- Royall, D.R.; Lauterbach, E.C.; Kaufer, D.; Malloy, P.; Coburn, K.L.; Black, K.J. The cognitive correlates of functional status: A review from the Committee on Research of the American Neuropsychiatric Association. J. Neuropsychiatr. Clin. Neurosci. 2007, 19, 249–265. [Google Scholar] [CrossRef] [PubMed]
- Gaugler, J.E.; Kane, R.L.; Kane, R.A.; Clay, T.; Newcomer, R. Caregiving and institutionalization of cognitively impaired older people: Utilizing dynamic predictors of change. Gerontologist 2003, 43, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Dhamoon, M.S.; Moon, Y.P.; Paik, M.C.; Boden Albala, B.; Rundek, T.; Sacco, R.L.; Elkind, M.S. Quality of life declines after first ischemic stroke. The Northern Manhattan Study. Neurology 2010, 75, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Dorman, P.J.; Waddell, F.; Slattery, J.; Dennis, M.; Sandercock, P. Is the EuroQol a valid measure of health-related quality of life after stroke? Stroke 1997, 28, 1876–1882. [Google Scholar] [CrossRef] [PubMed]
- Dorman, P.; Slattery, J.; Farrell, B.; Dennis, M.; Sandercock, P. Qualitative comparison of the reliability of health status assessments with the EuroQol and SF-36 questionnaires after stroke. Stroke 1998, 29, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Sturm, J.W.; Donnan, G.A.; Dewey, H.M.; Macdonell, R.A.; Gilligan, A.K.; Srikanth, V.; Thrift, A.G. Quality of life after stroke. The North East Melbourne Stroke Incidence Study (NEMESIS). Stroke 2004, 35, 2340–2345. [Google Scholar] [CrossRef] [PubMed]
- Haacke, C.; Althaus, A.; Spottke, A.; Siebert, U.; Back, T.; Dodel, R. Long-term outcome after stroke. Evaluating health-related quality of life using utility measurements. Stroke 2006, 37, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Wu, E.Q.; Zheng, Z.J.; Croft, J.B.; Greenlund, K.J.; Mensah, G.A.; Labarthe, D.R. Impact of stroke on health-related quality of life in the noninstitutionalized population in the united states. Stroke 2006, 37, 2567–2572. [Google Scholar] [CrossRef] [PubMed]
- Pinto, E.B.; Maso, I.; Pereira, J.L.; Fukuda, T.G.; Seixas, J.C.; Menezes, D.F.; Cincura, C.; Neville, I.S.; Jesus, P.A.; Oliveira-Filho, J. Differential aspects of stroke and congestive heart failure in quality of life reduction: A case series with three comparison groups. Health Qual. Life Outcomes 2011, 9, 65. [Google Scholar] [CrossRef] [PubMed]
- Hansson, E.E.; Beckman, A.; Wihlborg, A.; Persson, S.; Troein, M. Satisfaction with rehabilitation in relation to self-perceived quality of life and function among patients with stroke—A 12 month follow-up. Scand. J. Caring Sci. 2013, 27, 373–379. [Google Scholar] [CrossRef] [PubMed]
- López-Bastida, J.; Oliva Moreno, J.; Worbes Cerezo, M.; Perestelo Perez, L.; Serrano-Aguilar, P.; Montón-Alvarez, F. Social and economic costs and health-related quality of life in stroke survivors in the Canary Islands, Spain. BMC Health Serv. Res. 2012, 12, 315. [Google Scholar] [CrossRef] [PubMed]
- Hornslien, A.G.; Sandset, E.C.; Bath, P.M.; Wyller, T.B.; Berge, E. Effects of Candesartan in acute stroke on cognitive function and quality of life: Results from the Scandinavian candesartan acute stroke trial. Stroke 2013, 4, 2022–2024. [Google Scholar] [CrossRef] [PubMed]
- Luengo Fernandez, R.; Gray, A.M.; Bull, L.; Welch, S.; Cuthberston, F.; Rothwell, P.M. Quality of life after TIA and stroke. Ten-year results of the Oxford Vascular Study. Neurology 2013, 81, 1588–1595. [Google Scholar] [CrossRef] [PubMed]
- Sprigg, N.; Selby, J.; Fox, L.; Berge, E.; Whynes, D.; Bath, P.M.W. Very low quality of life after acute stroke: Data from the efficacy of nitric oxide in stroke trial. Stroke 2013, 44, 3458–3462. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.L.; Pan, Y.S.; Zhao, X.Q.; Wang, D.; Johnston, S.C.; Liu, L.P.; Meng, X.; Wang, A.X.; Wang, C.X.; Wang, Y.J. Recurrent stroke was associated with poor quality of life in patients with transient ischemic attack or minor stroke: Finding from the CHANCE trial. CNS Neurosci. Ther. 2014, 20, 1029–1035. [Google Scholar] [CrossRef] [PubMed]
- Golicki, D.; Niewada, M.; Karlińska, A.; Buczek, J.; Kobayashi, A.; Janssen, M.F.; Pickard, A.S. Comparing responsiveness of the EQ-5D-5L, EQ-5D-3L and EQ VAS in stroke patients. Qual. Life Res. 2014, in press. [Google Scholar]
- Bushnell, C.D.; Reeves, M.J.; Zhao, X.; Pan, W.; Prvu-Bettger, J.; Zimmer, L.; Olson, D.; Peterson, E. Sex differences in quality of life after ischemic stroke. Neurology 2014, 82, 922–931. [Google Scholar] [CrossRef] [PubMed]
- Franceschini, M.; La Porta, F.; Agosti, M.; Massucci, M. Is health-related-quality of life of stroke patients influenced by neurological impairments at one year after stroke? Eur. J. Phys. Rehab. Med. 2010, 46, 389–399. [Google Scholar]
- Fischer, U.; Anca, D.; Arnold, M.; Nedeltchev, K.; Kappeler, L.; Ballinari, P.; Schroth, G.; Mattle, H.P. Quality of life in stroke survivors after local intra-arterial thrombolysis. Cerebrovasc. Dis. 2008, 25, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Lisabeth, L.D.; Reeves, M.J.; Baek, J.; Skolarus, L.E.; Brown, D.L.; Zahuranec, D.B.; Smith, M.A.; Morgenstern, L.B. Factors influencing sex differences in poststroke functional outcome. Stroke 2015, 46, 860–863. [Google Scholar] [CrossRef] [PubMed]
- Cramm, J.M.; Strating, M.M.H.; Nieboer, A.P. Satisfaction with care as a quality-of-life predictor for stroke patients and their caregivers. Qual. Life Res. 2012, 21, 1719–1725. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Sabín, J.; Ortega, G.; Jacas, C.; Santamarina, E.; Maisterra, O.; Ribo, M.; Molina, C.; Quintana, M.; Román, G.C. Long-term treatment with citicoline may improve poststroke vascular cognitive impairment. Cerebrovasc. Dis. 2013, 35, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Sabín, J.; Román, G.C. The role of citicoline in neuroprotection and neurorepair in ischemic stroke. Brain Sci. 2013, 3, 1395–1414. [Google Scholar] [CrossRef] [PubMed]
- Hurtado, O.; Cárdenas, A.; Pradillo, J.M.; Morales, J.R.; Ortego, F.; Castillo, J.; Moro, M.A.; Lizasoain, I. A chronic treatment with CDP-choline improves functional recovery and increases neuronal plasticity after experimiental stroke. Neurobiol. Dis. 2007, 26, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Rosell, A.; Barceló, V.; García-Bonilla, L.; Delgado, P.; Fernández-Cadenas, I.; Hernández-Guillamon, M.; Montaner, J. Neurorepair potencial of CDP-Choline altercerebral ischemia in mice. Cerebrovasc. Dis. 2012, 33 (Suppl. S2), 419–420. [Google Scholar]
- Sobrino, T.; Rodríguez-González, R.; Blanco, M.; Brea, D.; Pérez-Mato, M.; Rodríguez-Yáñez, M.; Leira, R.; Castillo, J. CDP-choline treatment increases circulating endotelial progenitor cells in acute ischemic stroke. Neurol. Res. 2011, 33, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Fernández, M.; Rodriguez-Frutos, B.; Fuentes, B.; Vallejo-Cremades, M.T.; Alvarez-Grech, J.; Expósito-Alcaide, M.; Díez-Tejedor, E. CDP-choline treatment induces brain plasticity markers expression in experimental animal stroke. Neurochem. Int. 2012, 60, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Diederich, K.; Frauenknecht, K.; Minnerup, J.; Schneider, B.K.; Schmidt, A.; Altach, E.; Eggert, V.; Sommer, C.J.; Schäbitz, W.R. Citicoline enhances neuroregenerative processes after experimental stroke in rats. Stroke 2012, 43, 1931–1940. [Google Scholar] [CrossRef] [PubMed]
- Kuprinski, J.; Abudawood, M.; Matou-Nasri, S.; Al-Baradie, R.; Petcu, E.B.; Justicia, C.; Planas, A.; Liu, D.; Rovira, N.; Grau-Slevin, M.; Secades, J.; Slevin, M. Citicoline induces angiogenesis improving survival of vascular/human brain microvessel endothelial cells through pathways involving ERK1/2 and insulin receptor substrate-1. Vasc. Cell 2012, 4, 20. [Google Scholar] [Green Version]
- Bramanti, V.; Campisi, A.; Tomassoni, D.; Li Volti, G.; Caccamo, D.; Cannavò, G.; Currò, M.; Raciti, G.; Napoli, M.; Ientile, R.; Vanella, A.; Amenta, F.; Avola, R. Effect of acetylcholine precursors on proliferation and differentiation of astroglial cells in primary cultures. Neurochem. Res. 2008, 33, 2601–2608. [Google Scholar] [CrossRef] [PubMed]
- Osman, A.M.; Porritt, M.J.; Nilsson, M.; Kuhn, H.G. Long-term stimulation of neural progenitor cell migration after cortical ischemia in mice. Stroke 2011, 42, 3559–3565. [Google Scholar] [CrossRef] [PubMed]
- Badia, X.; Roset, M.; Montserrat, S.; Herdman, M.; Segura, A. La versión española de la EuroQol: Descripción y aplicaciones. Med. Clin. 1999, 112 (Suppl. S1), 79–86. [Google Scholar]
- Herdman, M.; Badia, X.; Berra, S. El EuroQol-5D: Una alternativa sencilla para la medición de la calidad de vida relacionada con la salud en atención primaria. Aten. Prim. 2001, 28, 425–429. [Google Scholar] [CrossRef]
- Christensen, M.C.; Mayer, S.; Ferran, J.M. Quality of life after intracerebral hemorrhage: Results of the factor seven for acute hemorrhagic stroke (FAST) trial. Stroke 2009, 40, 1677–1682. [Google Scholar] [CrossRef] [PubMed]




| Parameters | Citicoline | p | |
|---|---|---|---|
| Yes (n = 86) | No (n = 77) | ||
| Sex (female) | 54.7% | 46.8% | 0.314 |
| Age | 68.5 ± 9.8 | 66.4 ± 11.4 | 0.200 |
| Years of education | 5.8 ± 3.7 | 5.1 ± 3.3 | 0.173 |
| Smoking | 24.4% | 35.1% | 0.137 |
| Alcohol | 17.4% | 24.7% | 0.256 |
| Dyslipidaemia | 34.9% | 46.8% | 0.123 |
| Diabetes mellitus | 38.4% | 24.7% | 0.061 |
| Hypertension | 59.3% | 61%) | 0.821 |
| Atrial Fib. | 12.8% | 11.7% | 0.830 |
| Coronary heart disease | 4.7% | 10.4% | 0.161 |
| AMI | 11.6% | 14.3% | 0.613 |
| PAD | 4.7% | 5.2% | 1.000 |
| Baseline NIHSS | 13 (10–16) | 14 (10–16.5) | 0.518 |
| Parameters | Utility | p | |
|---|---|---|---|
| Sex | Male | 0.67 ± 0.27 | 0.030 |
| Female | 0.58 ± 0.29 | ||
| Age | R: −0.156 | 0.046 | |
| Years of education | R: 0.081 | 0.306 | |
| Smoking | No | 0.62 ± 0.27 | 0.670 |
| Yes | 0.64 ± 0.31 | ||
| Alcohol | No | 0.64 ± 0.29 | 0.306 |
| Yes | 0.58 ± 0.27 | ||
| Dyslipidaemia | No | 0.63 ± 0.26 | 0.763 |
| Yes | 0.62 ± 0.31 | ||
| Diabetes mellitus | No | 0.64 ± 0.28 | 0.316 |
| Yes | 0.59 ± 0.29 | ||
| Hypertension | No | 0.67 ± 0.26 | 0.078 |
| Yes | 0.59 ± 0.29 | ||
| Atrial Fib. | No | 0.64 ± 0.27 | 0.199 |
| Yes | 0.53 ± 0.35 | ||
| Coronaryheart disease | No | 0.62 ± 0.29 | 0.521 |
| Yes | 0.68 ± 0.24 | ||
| AMI | No | 0.62 ± 0.28 | 0.465 |
| Yes | 0.67 ± 0.30 | ||
| PAD | No | 0.64 ± 0.28 | 0.047 |
| Yes | 0.43 ± 0.30 | ||
| Baseline NIHSS | R: −0.188 | 0.016 | |
| Parameters | Quality of Life | p | |
|---|---|---|---|
| Good/Acceptable | Poor/Very Poor | ||
| Sex (female) | 46.8% | 64.9% | 0.054 |
| Age | 66.6 ± 10.2 | 70.7 ± 12.1 | 0.039 |
| Years of education | 5.7 ± 3.6 | 4.8 ± 3.2 | 0.152 |
| Smoking | 29.4% | 29.7% | 0.966 |
| Alcohol | 19.8% | 24.3% | 0.555 |
| Dyslipidaemia | 40.5% | 40.5% | 0.994 |
| Diabetes mellitus | 31.0% | 35.1% | 0.631 |
| Hypertension | 56.3% | 73.0% | 0.069 |
| Atrial Fib. | 10.3% | 18.9% | 0.161 |
| Coronary heart disease | 7.9% | 5.4% | 0.604 |
| AMI | 13.5% | 10.8% | 0.669 |
| PAD | 3.2% | 10.8% | 0.079 |
| Baseline NIHSS | 13 (10–16) | 14 (11–17) | 0.301 |
| Study | Year | Country | Follow-up | n | Stroke Type | Utility or Equivalent | VAS | Sex | Age | NIHSS | Multivariate (Worse Quality of Life) | Other |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sturm, J.W., et al. [10] | 2004 | Australia | 2 years | 225 | Ischaemic and haemorrhagic | 0.47 (95% CI 0.42–0.52) | N.A. | Females worse (sig.) | Old age worse (sig.) | Worse with higher NIHSS (sig.) | Age, sex, NIHSS, and socioecon. status | – |
| Haacke, C., et al. [11] | 2006 | Germany | 4 years | 54 | Ischaemic | 0.68 ± 0.33 | 56.5 | Females worse (n.s.) | Old age worse (sig.) | N.A. | IB, anal continence, continence and depression. | Worse with lower IB, higher mRS, impairment (MMSE) and depression. |
| Xie, J., et al. [12] | 2006 | USA | >1 year | 1040 | Stroke | 0.69 (SE 0.01) | 61.6 (SE 0.08) | Females worse | Worse in old age | N.A. | N.A. | – |
| Pinto, E.B., et al. [13] | 2011 | Brazil | 2 years | 67 | Stroke | 0.52 ± 0.36 | N.A. | N.A. | No correlation with age (n.s.) | Worse with higher NIHSS (sig.) | N.A. | – |
| Hansson, E.E., et al. [14] | 2012 | Sweden | 1 year | 283 | Stroke | 0.5 ± 0.39 | 62.5 ± 21.8 | N.A. | N.A. | N.A. | N.A. | – |
| López-Bastida, J., et al. [15] | 2012 | Canary Islands, Spain | 1 year | 94 | Stroke | 0.49 ± 0.42 | 56 ± 27 | N.A. | N.A. | N.A. | N.A. | Quality of life does not change in 1–2–3 years. |
| 2 years | 205 | 0.47 ± 0.44 | 51.6 ± 27 | |||||||||
| 3 years | 149 | 0.46 ± 0.45 | 55 ± 25 | |||||||||
| Hornslien, A.G., et al. [16] (SCAST) | 2012 | Northern Europe | 6 months | 870 | Stroke: Candesartan Placebo | 0.74 (0.59–0.88) 0.78 (0.62–0.88) | 66 ± 20 | N.A. | N.A. | N.A. | N.A. | MMSE: 28 (25–29); Does not compare it with quality of life. |
| 882 | 67.3 ± 19 | |||||||||||
| Luengo-Fernández, R., et al. [17] (OXVASC) | 2013 | UK | 1 month | 314 | Ischaemic stroke | 0.64 ± 0.33 | N.A. | Females worse (sig.) | Old age worse (sig.) | Worse with higher NIHSS (sig.) | Sex, Age, NIHSS, risk factors, stroke type | Does not vary in 1–5 years. |
| 1 year | 0.70 ± 0.27 | |||||||||||
| 2 years | 0.66 ± 0.29 | |||||||||||
| 5 years | 0.67 ± 0.31 | |||||||||||
| Sprigg, N., et al. [18] (ENOS) | 2013 | Countries worldwide | 3 months | 2238 | Ischaemic and haemorrhagic | N.A. | 65.8 ± 22.4 | N.A. | N.A. | N.A. | N.A. | Worse with lower IB, higher mRS, impairment (MMSE) and depression. |
| Wang, Y.-L., et al. [19] (CHANCE) | 2014 | China | 3 months | 5104 | TIAs | 0.88 ± 0.21 | 84 ± 15 | Females worse (sig.) | Old age worse (sig.) | Worse with higher NIHSS (sig.) | Age, hypertension, DM, NIHSS, and various treatments | Worse at higher mRS. |
| 89 (80–85) | ||||||||||||
| Golicki, D., et al. [20] | 2014 | Poland | 4 months | 112 | Stroke | 0.691 ± 0.267 | 60.7 ± 22.4 | N.A. | N.A. | N.A. | N.A. | Correlation with Barthel and mRS |
| 60 (45.5–80) | ||||||||||||
| Bushnell, C.D., et al. [21] | 2014 | USA | 1 year | 1370 | Ischaemic (including TIAs) | 0.83 (0.74–1) | N.A. | Females worse (sig.) | N.A. | Worse with higher NIHSS (sig.) | NIHSS and sex | No changes in quality of life during 1 year |
| Current study | 2015 | Spain | 2 years | 163 | First ischaemic stroke | 0.63 ± 0.28 | 64.4 ± 25 70 (50–85) | Females worse (sig.) | Old age worse (sig.) | Worse with higher NIHSS (sig.) | Age, treatment with citicoline | – |
| 0.70 (0.59–0.79) |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alvarez-Sabín, J.; Santamarina, E.; Maisterra, O.; Jacas, C.; Molina, C.; Quintana, M. Long-Term Treatment with Citicoline Prevents Cognitive Decline and Predicts a Better Quality of Life after a First Ischemic Stroke. Int. J. Mol. Sci. 2016, 17, 390. https://doi.org/10.3390/ijms17030390
Alvarez-Sabín J, Santamarina E, Maisterra O, Jacas C, Molina C, Quintana M. Long-Term Treatment with Citicoline Prevents Cognitive Decline and Predicts a Better Quality of Life after a First Ischemic Stroke. International Journal of Molecular Sciences. 2016; 17(3):390. https://doi.org/10.3390/ijms17030390
Chicago/Turabian StyleAlvarez-Sabín, Jose, Estevo Santamarina, Olga Maisterra, Carlos Jacas, Carlos Molina, and Manuel Quintana. 2016. "Long-Term Treatment with Citicoline Prevents Cognitive Decline and Predicts a Better Quality of Life after a First Ischemic Stroke" International Journal of Molecular Sciences 17, no. 3: 390. https://doi.org/10.3390/ijms17030390