Significance of Matrix Metalloproteinase 9 Expression as Supporting Marker to Cytokeratin 19 mRNA in Sentinel Lymph Nodes in Breast Cancer Patients
Abstract
:1. Introduction
2. Results
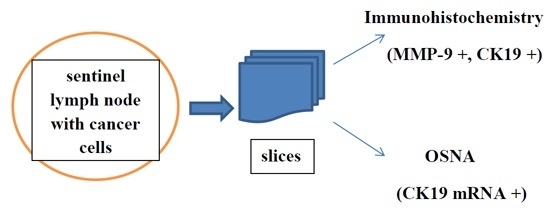
2.1. Analysis of Sentinel Lymph Nodes by Means of One-Step Nucleic Acid Amplification (OSNA)
2.1.1. Correlation of CK19 mRNA with CK19 and MMP-9 by Means of Immunohistochemistry (IHC)
2.1.2. Correlation of CK19 mRNA with Clinicopathological Data
2.2. Immunohistochemistry and Western Blot Analysis
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Sentinel Lymph Node Sampling Method
4.3. One-Step Nucleic Acid Amplification (OSNA)
4.4. Immunohistochemistry (IHC)
4.5. Western Blotting Analysis
4.6. Statistics
- κ-Values between 0.41 and 0.60 indicated moderate agreement,
- κ-Values between 0.61 and 0.80 indicated substantial agreement,
- κ-Values above 0.81 indicated almost perfect agreement.
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Veronesi, U.; Paganelli, G.; Galimberti, V.; Viale, G.; Zurrida, S.; Bedoni, M.; Costa, A.; de Cicco, C.; Geraghty, J.G.; Luini, A.; et al. Sentinel-node biopsy to avoid axillary dissection in breast cancer with clinically negative lymph-nodes. Lancet 1997, 349, 1864–1867. [Google Scholar] [CrossRef]
- Galimberti, V.; Cole, B.F.; Zurrida, S.; Viale, G.; Luini, A.; Veronesi, P.; Baratella, P.; Chifu, C.; Sargenti, M.; Intra, M.; et al. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23-01): A phase 3 randomised controlled trial. Lancet Oncol. 2013, 14, 297–305. [Google Scholar] [CrossRef]
- Giuliano, A.E.; Jones, R.C.; Brennan, M.; Statman, R. Sentinel lymphadenectomy in breast cancer. J. Clin. Oncol. 1997, 15, 2345–2350. [Google Scholar] [PubMed]
- Krag, D.N.; Anderson, S.J.; Julian, T.B.; Brown, A.M.; Harlow, S.P.; Costantino, J.P.; Ashikaga, T.; Weaver, D.L.; Mamounas, E.P.; Jalovec, L.M.; et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: Overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010, 11, 927–933. [Google Scholar] [CrossRef]
- Giuliano, A.E.; Kirgan, D.M.; Guenther, J.M.; Morton, D.L. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann. Surg. 1994, 220, 391–401. [Google Scholar] [CrossRef] [PubMed]
- Viale, G.; Bosari, S.; Mazzarol, G.; Galimberti, V.; Luini, A.; Veronesi, P.; Paganelli, G.; Bedoni, M.; Orvieto, E. Intraoperative examination of axillary sentinel lymph nodes in breast carcinoma patients. Cancer 1999, 85, 2433–2438. [Google Scholar] [CrossRef]
- Tsujimoto, M.; Nakabayashi, K.; Yoshidome, K.; Kaneko, T.; Iwase, T.; Akiyama, F.; Kato, Y.; Tsuda, H.; Ueda, S.; Sato, K.; et al. One-step nucleic acid amplification for intraoperative detection of lymph node metastasis in breast cancer patients. Clin. Cancer Res. 2007, 13, 4807–4816. [Google Scholar] [CrossRef] [PubMed]
- Osako, T.; Iwase, T.; Kimura, K.; Yamashita, K.; Horii, R.; Yanagisawa, A.; Akiyama, F. Intraoperative molecular assay for sentinel lymph node metastases in early stage breast cancer: A comparative analysis between one-step nucleic acid amplification whole node assay and routine frozen section histology. Cancer 2011, 117, 4365–4374. [Google Scholar] [CrossRef] [PubMed]
- Sagara, Y.; Ohi, Y.; Matsukata, A.; Yotsumoto, D.; Baba, S.; Tamada, S.; Sagara, Y.; Matsuyama, Y.; Ando, M.; Rai, Y.; et al. Clinical application of the one-step acid amplification method to detect sentinel node metastases in breast cancer. Breast Cancer 2013, 20, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Guillen-Paredes, M.P.; Carrasco-González, L.; Cháves-Benito, A.; Campillo-Soto, A.; Carrillo, A.; Aguayo-Albasini, J.L. One-step nucleic acid amplification (OSNA) assay for sentinel lymph node metastases as an alternative to conventional postoperative histology in breast cancer: A cost-benefit analysis. Cir. Esp. 2011, 89, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Classe, J.M.; Baffert, S.; Sigal-Zafrani, B.; Fall, M.; Rousseau, C.; Alran, S.; Rouanet, P.; Belichard, C.; Mignotte, H.; Ferron, G.; et al. Cost comparison of axillary sentinel lymph node detection and axillary lymphadenectomy in early breast cancer. A national study based on a prospective multi-institutional series of 985 patients “on behalf of the group of surgeons from the French Unicancer Federation”. Ann. Oncol. 2012, 23, 1170–1177. [Google Scholar] [PubMed]
- Lohrisch, C.; Paltiel, C.; Gelmon, K.; Speers, C.; Taylor, S.; Barnett, J.; Olivotto, I.A. Impact on survival of time from definitive surgery to initiation of adjuvant chemotherapy for early-stage breast cancer. J. Clin. Oncol. 2006, 24, 4888–4894. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.Y.; Sereika, S.M.; Linkov, F.; Brufsky, A.; Weissfeld, J.L.; Rosenzweig, M. The effect of delays in treatment for breast cancer metastasis on survival. Breast Cancer Res. Treat. 2011, 130, 953–964. [Google Scholar] [CrossRef] [PubMed]
- Gainer, S.M.; Hunt, K.K.; Beitsch, P.; Caudle, A.S.; Mittendorf, E.A.; Lucci, A. Changing behavior in clinical practice in response to the ACOSOG Z0011 trial: A survey of the American Society of Breast Surgeons. Ann. Surg. Oncol. 2012, 19, 3152–3158. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.B.; Ni, J.S.; Wu, P.; Bao, Y.L.; Liu, T.; Li, M.; Fan, C.; Zhang, W.J.; Sun, L.G.; Huang, Y.X.; et al. Testes-specific protease 50 promotes cell invasion and metastasis by increasing NF-κB-dependent matrix metalloproteinase-9 expression. Cell Death Dis. 2015, 6. [Google Scholar] [CrossRef] [PubMed]
- Bottino, J.; Gelaleti, G.B.; Maschio, L.B.; Jardim-Perassi, B.V.; de Campos Zuccari, D.A. Immunoexpression of ROCK-1 and MMP-9 as prognostic markers in breast cancer. Acta Histochem. 2014, 116, 1367–1373. [Google Scholar] [CrossRef] [PubMed]
- Mylona, E.; Nomikos, A.; Magkou, C.; Kamberou, M.; Papassideri, I.; Keramopoulos, A.; Nakopoulou, L. The clinicopathological and prognostic significance of membrane type 1 matrix metalloproteinase (MT1-MMP) and MMP-9 according to their localization in invasive breast carcinoma. Histopathology 2007, 50, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Ranogajec, I.; Jakic-Razumovic, J.; Puzovic, V.; Gabrilovac, J. Prognostic value of matrix metalloproteinase-2 (MMP-2), matrix metalloproteinase-9 (MMP-9) and aminopeptidase N/CD13 in breast cancer patients. Med. Oncol. 2012, 29, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Choi, J.Y.; Lee, S.A.; Lee, K.M.; Han, S.; Jeon, S.; Song, M.; Lee, Y.; Park, S.K.; Yoo, K.Y.; et al. The association between the preoperative serum levels of lipocalin-2 and matrix metalloproteinase-9 (MMP-9) and prognosis of breast cancer. BMC Cancer 2012, 12. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.; Liu, C.; Dong, B.; Li, Y.; Jiang, B.; Xu, Y.; Meng, L.; Wu, J.; Qu, L.; Shou, C. Inverse correlation between Naa10p and MMP-9 expression and the combined prognostic value in breast cancer patients. Med. Oncol. 2013, 30, 562. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Ma, W.; Zhang, M.; Tang, D.; Shi, Q.; Xu, S.; Zhang, X.; Liu, Y.; Song, Y.; Liu, L.; et al. High expression of CD147 and MMP-9 is correlated with poor prognosis of triple-negative breast cancer (TNBC) patients. Med. Oncol. 2013, 30. [Google Scholar] [CrossRef] [PubMed]
- Santaballa, A.; de La Cueva, H.; Salvador, C.; García-Martínez, A.M.; Guarín, M.J.; Lorente, D.; Palomar, L.; Aznar, I.; Dobón, F.; Bello, P. Advantages of one step nucleic acid amplification (OSNA) whole node assay in sentinel lymph node (SLN) analysis in breast cancer. SpringerPlus 2013, 2. [Google Scholar] [CrossRef] [PubMed]
- Tamaki, Y.; Sato, N.; Homma, K.; Takabatake, D.; Nishimura, R.; Tsujimoto, M.; Yoshidome, K.; Tsuda, H.; Kinoshita, T.; Kato, H.; et al. Routine clinical use of the one-step nucleic acid amplification assay for detection of sentinel lymph node metastases in breast cancer patients: Results of a multicenter study in Japan. Cancer 2012, 118, 3477–3483. [Google Scholar] [CrossRef] [PubMed]
- Ruano, M.A.; Lopez-Bonet, E.; Buxó, M.; Tuca-Rodríguez, F.; Vila-Camps, E.; Alvarez, E.; Martin-Castillo, B.; Menendez, J.A. An improved axillary staging system using the OSNA assay does not modify the therapeutic management of breast cancer patients. Sci. Rep. 2014, 18. [Google Scholar] [CrossRef] [PubMed]
- Osako, T.; Tsuda, H.; Horii, R.; Iwase, T.; Yamauchi, H.; Yagata, H.; Tsugawa, K.; Suzuki, K.; Kinoshita, T.; Akiyama, F.; et al. Molecular detection of lymph node metastasis in breast cancer patients treated with preoperative systemic chemotherapy: A prospective multicentre trial using the one-step nucleic acid amplification assay. Br. J. Cancer 2013, 109, 1693–1698. [Google Scholar] [CrossRef] [PubMed]
- Ohi, Y.; Umekita, Y.; Sagara, Y.; Rai, Y.; Yotsumoto, D.; Matsukata, A.; Baba, S.; Tamada, S.; Matsuyama, Y.; Ando, M.; et al. Whole sentinel lymph node analysis by a molecular assay predicts axillary node status in breast cancer. Br. J. Cancer 2012, 107, 1239–1243. [Google Scholar] [CrossRef] [PubMed]
- Heo, D.S.; Choi, H.; Yeom, M.Y.; Song, B.J.; Oh, S.J. Serum levels of matrix metalloproteinase-9 predict lymph node metastasis in breast cancer patients. Oncol. Rep. 2014, 31, 1567–1572. [Google Scholar] [PubMed]
- Decock, J.; Hendrickx, W.; Wildiers, H.; Christiaens, M.R.; Neven, P.; Drijkoningen, M.; Paridaens, R. Plasma gelatinase levels in patients with primary breast cancer in relation to axillary lymph node status, Her2/neu expression and other clinicopathological variables. Clin. Exp. Metastasis 2005, 22, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Pellikainen, J.M.; Ropponen, K.M.; Kataja, V.V.; Kellokoski, J.K.; Eskelinen, M.J.; Kosma, V.M. Expression of matrix metalloproteinase (MMP)-2 and MMP-9 in breast cancer with a special reference to activator protein-2, HER2, and prognosis. Clin. Cancer Res. 2004, 10, 7621–7628. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.W.; Yang, Q.M.; Huang, Y.F.; She, H.Q.; Liang, J.; Yang, Q.L.; Zhang, Z.M. Expression and clinical significance of matrix metalloproteinase-9 in lymphatic invasiveness and metastasis of breast cancer. PLoS ONE 2014, 9, e97804. [Google Scholar] [CrossRef] [PubMed]
- Tang, D.; Piao, Y.; Zhao, S.; Mu, X.; Li, S.; Ma, W.; Song, Y.; Wang, J.; Zhao, W.; Zhang, Q. Expression and correlation of matrix metalloproteinase-9 and heparanase in patients with breast cancer. Med. Oncol. 2014, 31. [Google Scholar] [CrossRef] [PubMed]
- Sullu, Y.; Demirag, G.G.; Yildirim, A.; Karagoz, F.; Kandemir, B. Matrix metalloproteinase-2 (MMP-2) and MMP-9 expression in invasive ductal carcinoma of the breast. Pathol. Res. Pract. 2011, 207, 747–753. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Ang, L.; Liu, M.Q.; Hu, H.G.; Wang, J.; Zou, Q.; Zhao, Y.; Zheng, L.; Zhao, M.; Wu, Z.S. Serum and tissue expression of gelatinase and Twist in breast cancer. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 2662–2669. [Google Scholar] [PubMed]
- Sobin, L.H.; Gospodarowicz, M.K.; Wittekind, C. (Eds.) UICC TNM Classification of Malignant Tumours, 7th ed.; Wiley-Liss: New York, NY, USA, 2009.
- Wolff, A.C.; Hammond, M.E.; Hicks, D.G.; Dowsett, M.; McShane, L.M.; Allison, K.H.; Allred, D.C.; Bartlett, J.M.; Bilous, M.; Fitzgibbons, P.; et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J. Clin. Oncol. 2013, 31, 3997–4013. [Google Scholar] [CrossRef] [PubMed]
- Allred, D.C.; Harvey, J.M.; Berardo, M.; Clark, G.M. Prognostic and predictive factors in breast cancer by immunohistochemical analysis. Mod. Pathol. 1998, 11, 155–168. [Google Scholar] [PubMed]


| No. | Age | Receptors | CK19 mRNA | CK19 | MMP-9 | Staging pTNM | G |
|---|---|---|---|---|---|---|---|
| 1 | 71 | ER(3+) PR(−) HER2(+) | + | + | + | T2N1aMXL0B0 | 3 |
| 2 | 53 | ER(1+) PR(3+) HER2(−) | + | − | + | T1N0MXL0B0 | 1 |
| 3 | 49 | ER(1+) PR(2+) HER2(−) | − | − | − | T1cN0MXL0B0 | 1 |
| 4 | 45 | ER(1+) PR(2+) HER2(−) | + | + | + | T1bN2aMXL0B0 | 3 |
| 5 | 57 | ER(3+) PR(3+) HER2(−) | − | − | − | T1cN0MXL0B0 | 3 |
| 6 | 43 | ER(2+) PR(2+) HER2(+) | − | − | − | T1cN0MXL0B0 | 2 |
| 7 | 54 | ER(3+) PR(−) HER2(−) | − | − | − | T1aN0MXL0B0 | 1 |
| 8 | 37 | ER(−) PR(−) HER2(−) | − | − | − | T1cN0MXL0B0 | 3 |
| 9 | 64 | ER(3+) PR(2+) HER2(+) | + | − | + | T1cN0MXL0B0 | 3 |
| 10 | 68 | ER(1+) PR(+) HER2(−) | + | + | + | T2N1aMXL0B0 | 2 |
| 11 | 82 | ER(3+) PR(3+) HER2(−) | − | − | − | T2N0MXL0B0 | 3 |
| 12 | 66 | ER(−) PR(−) HER2(−) | − | − | − | T1cN0MXL0B0 | 1 |
| 13 | 51 | ER(1+) PR(3+) HER2(−) | − | − | − | T1cN0MXL0B0 | 3 |
| 14 | 57 | ER(2+) PR(3+) HER2(−) | + | + | + | T1bN3aMXL0B0 | 2 |
| 15 | 74 | ER(−) PR(−) HER2(+) | − | − | − | T1N0MXL0B0 | 2 |
| 16 | 54 | ER(2+) PR(−) HER2(−) | − | − | − | T1cN0MXL0B0 | 3 |
| 17 | 40 | ER(−) PR(−) HER2(−) | − | − | − | T1cN0MXL0B0 | 1 |
| 18 | 67 | ER(3+) PR(3+) HER2(−) | − | − | − | T2N0MXL0B0 | 1 |
| 19 | 59 | ER(1+) PR(3+) HER2(−) | + | − | + | T1cN0MXL0B0 | 3 |
| 20 | 59 | ER(−) PR(−) HER2(+) | − | − | − | T2N0MXL0B0 | 3 |
| 21 | 70 | ER(3+) PR(3+) HER2(−) | + | − | + | T1cN0MXL0B0 | 2 |
| 22 | 38 | ER(1+) PR(3+) HER2(−) | − | − | − | T1cN0MXL0B0 | 1 |
| 23 | 57 | ER(3+) PR(2+) HER2(−) | + | + | − | T1bN1aMXL0B0 | 1 |
| 24 | 65 | ER(3+) PR(3+) HER2(−) | − | − | − | T1bN0MXL0B0 | 1 |
| 25 | 79 | ER(2+) PR(3+) HER2(−) | + | − | + | T2N0MXL0B0 | 2 |
| 26 | 46 | ER(1+) PR(1+) HER2(+) | − | − | − | T1N0MXL0B0 | 1 |
| 27 | 52 | ER(3+) PR(2+) HER2(−) | − | − | − | T1cN0MXL0B0 | 1 |
| 28 | 57 | ER(3+) PR(2+) HER2(−) | − | − | − | T1cN0MXL0B0 | 2 |
| 29 | 62 | ER(3+) PR(2+) HER2(+) | − | − | − | T1bN0MXL0B0 | 1 |
| 30 | 62 | ER(3+) PR(3+) HER2(−) | + | + | + | T2N1MXL0B0 | 2 |
| 31 | 66 | ER(3+) PR(−) HER2(+) | − | − | − | T2N0MXL0B0 | 1 |
| 32 | 59 | ER(3+) PR(3+)HER2(−) | + | − | + | T1bN0MXL0B0 | 3 |
| 33 | 67 | ER(3+) PR(3+) HER2(−) | − | − | − | T2N0MXL0B0 | 1 |
| 34 | 76 | ER(2+) PR(3+) HER2(−) | + | + | − | T2N1MXL0B0 | 2 |
| 35 | 56 | ER(1+) PR(1+) HER2(−) | − | − | − | T1bN0MXL0B0 | 1 |
| 36 | 70 | ER(−) PR(−) HER2(+) | − | − | − | T1aN0MXL0B0 | 1 |
| 37 | 67 | ER(2+) PR(1+) HER2(−) | + | − | + | T1N0MXL0B0 | 2 |
| 38 | 63 | ER(−) PR(−) HER2(−) | + | − | + | T2N0MXL0B0 | 3 |
| 39 | 54 | ER(−) PR(−) HER2(−) | + | + | + | T1N1MXL0B0 | 3 |
| 40 | 46 | ER(−) PR(−) HER2(−) | + | + | + | T1aN1MXL0B0 | 2 |
| Positive Expression | N0 n = 31 | >N0 n = 9 | Fisher’s Exact Test | Accuracy |
|---|---|---|---|---|
| CK19 mRNA | 8 (25.8%) | 9 (100.0%) | p < 0.001 | 80% |
| CK19 (by IHC) | 0 (0.0%) | 9 (100.0%) | p < 0.001 | 100% |
| MMP-9 | 8 (25.8%) | 7 (71.4%) | p = 0.002 | 75% |
| Positive Expression | Grade 1 n = 16 | Grade 2 n = 11 | Grade 3 n = 13 | Pearson χ-Square | Spearman’s Coefficient of Correlation |
|---|---|---|---|---|---|
| CK19 mRNA | 2 (12.5%) | 8 (72.7%) | 7 (53.8%) | p = 0.005 | ρ = 0.385 |
| CK19 (by IHC) | 1 (6.2%) | 5 (45.4%) | 3 (23.1%) | p = 0.056 | ρ = 0.199 |
| MMP-9 | 1 (6.2%) | 7 (63.6%) | 7 (53.8%) | p = 0.003 | ρ = 0.443 |
| Positive Expression | Estrogen n = 31 | Progesterone n = 27 | HER2 n = 9 |
|---|---|---|---|
| CK19 mRNA | 14 (45.2%) | 13 (48.2%) | 2 (22.2%) |
| CK19 (by IHC) | 7 (22.6%) | 6 (22.2%) | 1 (11.1%) |
| MMP-9 | 12 (38.7%) | 11 (40.7%) | 2 (22.2%) |
| Variable | CK19 mRNA | MMP-9 | ||
|---|---|---|---|---|
| ρ | p | ρ | p | |
| Age | 0.253 | 0.114 | 0.159 | 0.321 |
| ER | −0.033 | 0.838 | −0.045 | 0.781 |
| PR | 0.090 | 0.575 | 0.120 | 0.454 |
| HER2 | −0.194 | 0.227 | −0.170 | 0.288 |
| T | 0.250 | 0.119 | 0.101 | 0.527 |
| N | 0.614 | <0.001 | 0.458 | 0.004 |
| G | 0.387 | 0.016 | 0.443 | 0.006 |
| CK19 (by IHC) | 0.625 | <0.001 | 0.448 | 0.005 |
| MMP-9 | 0.898 | <0.001 | × | × |
| CK19 mRNA | × | × | 0.898 | <0.001 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murawski, M.; Woźniak, M.; Duś-Szachniewicz, K.; Kołodziej, P.; Rzeszutko, M.; Ziółkowski, P. Significance of Matrix Metalloproteinase 9 Expression as Supporting Marker to Cytokeratin 19 mRNA in Sentinel Lymph Nodes in Breast Cancer Patients. Int. J. Mol. Sci. 2016, 17, 571. https://doi.org/10.3390/ijms17040571
Murawski M, Woźniak M, Duś-Szachniewicz K, Kołodziej P, Rzeszutko M, Ziółkowski P. Significance of Matrix Metalloproteinase 9 Expression as Supporting Marker to Cytokeratin 19 mRNA in Sentinel Lymph Nodes in Breast Cancer Patients. International Journal of Molecular Sciences. 2016; 17(4):571. https://doi.org/10.3390/ijms17040571
Chicago/Turabian StyleMurawski, Marek, Marta Woźniak, Kamila Duś-Szachniewicz, Paweł Kołodziej, Marta Rzeszutko, and Piotr Ziółkowski. 2016. "Significance of Matrix Metalloproteinase 9 Expression as Supporting Marker to Cytokeratin 19 mRNA in Sentinel Lymph Nodes in Breast Cancer Patients" International Journal of Molecular Sciences 17, no. 4: 571. https://doi.org/10.3390/ijms17040571