Could −79 °C Spray-Type Cryotherapy Be an Effective Monotherapy for the Treatment of Keloid?
Abstract
:1. Introduction
2. Results
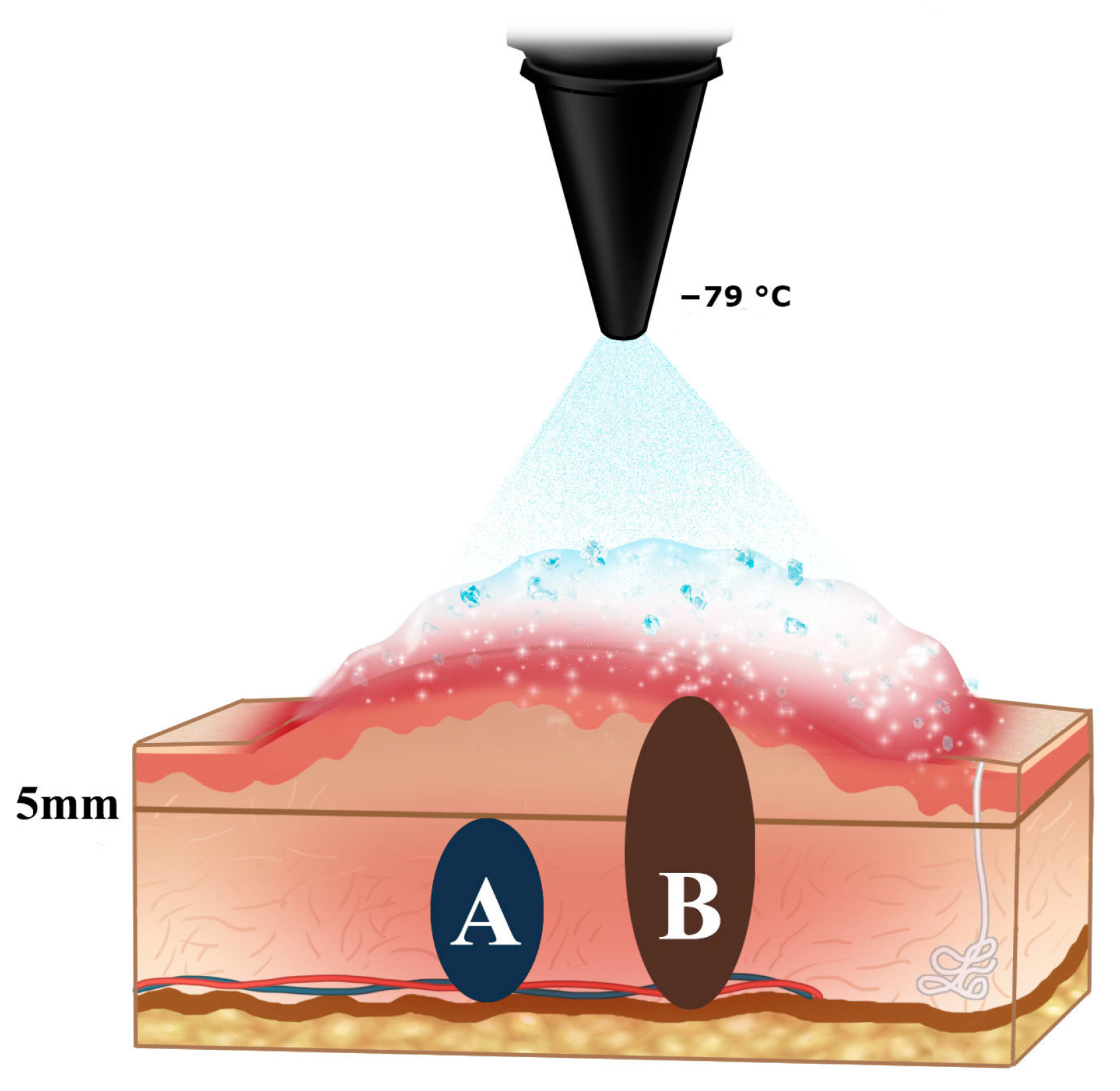
2.1. The Schematic Illustration of Tissue Sampling for Pathologic and Molecular Study
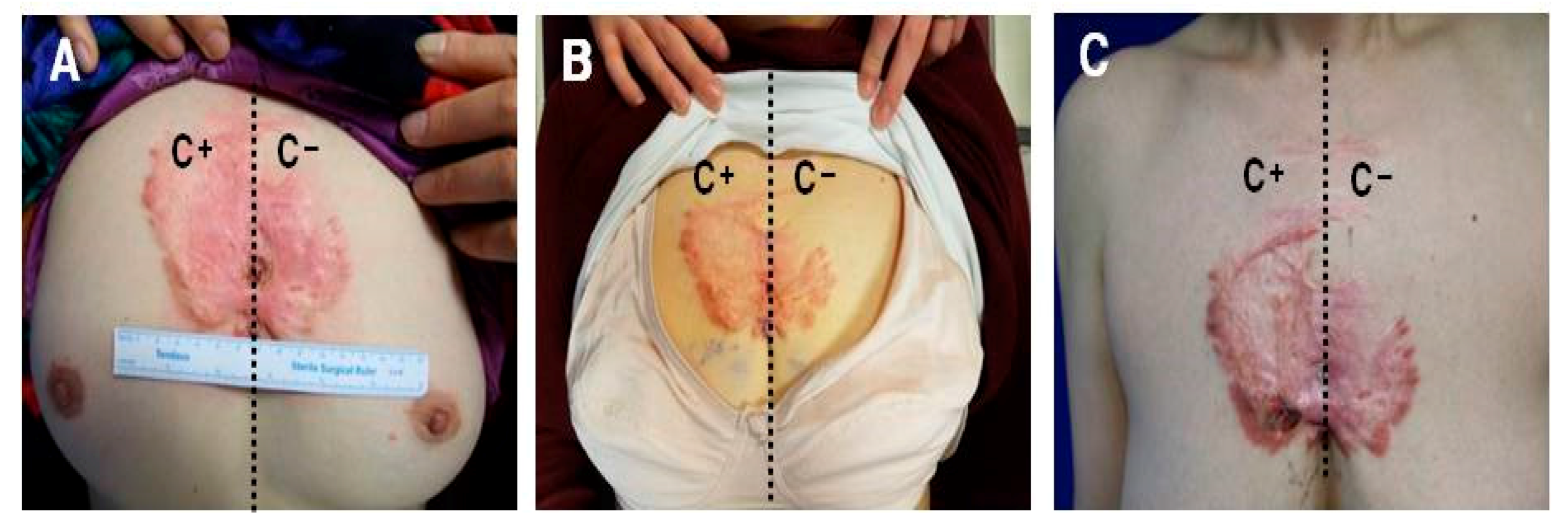
2.2. Keloids Treated with −79 °C Spray-Type CryoPen™ Rapidly Reoccurred in Clinical Trials
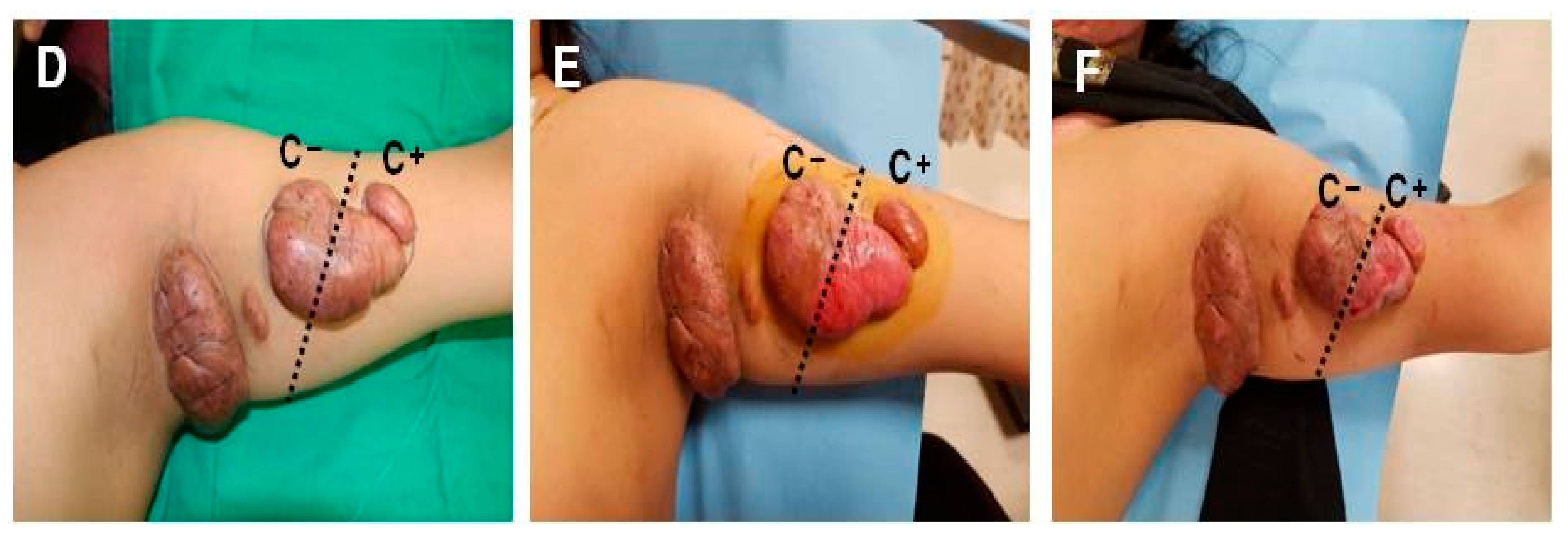
2.3. Keloid-Derived Fibroblasts Show Enhanced Proliferation and Migration Activity Following Treatment with −79 °C Spray-Type CryoPen™
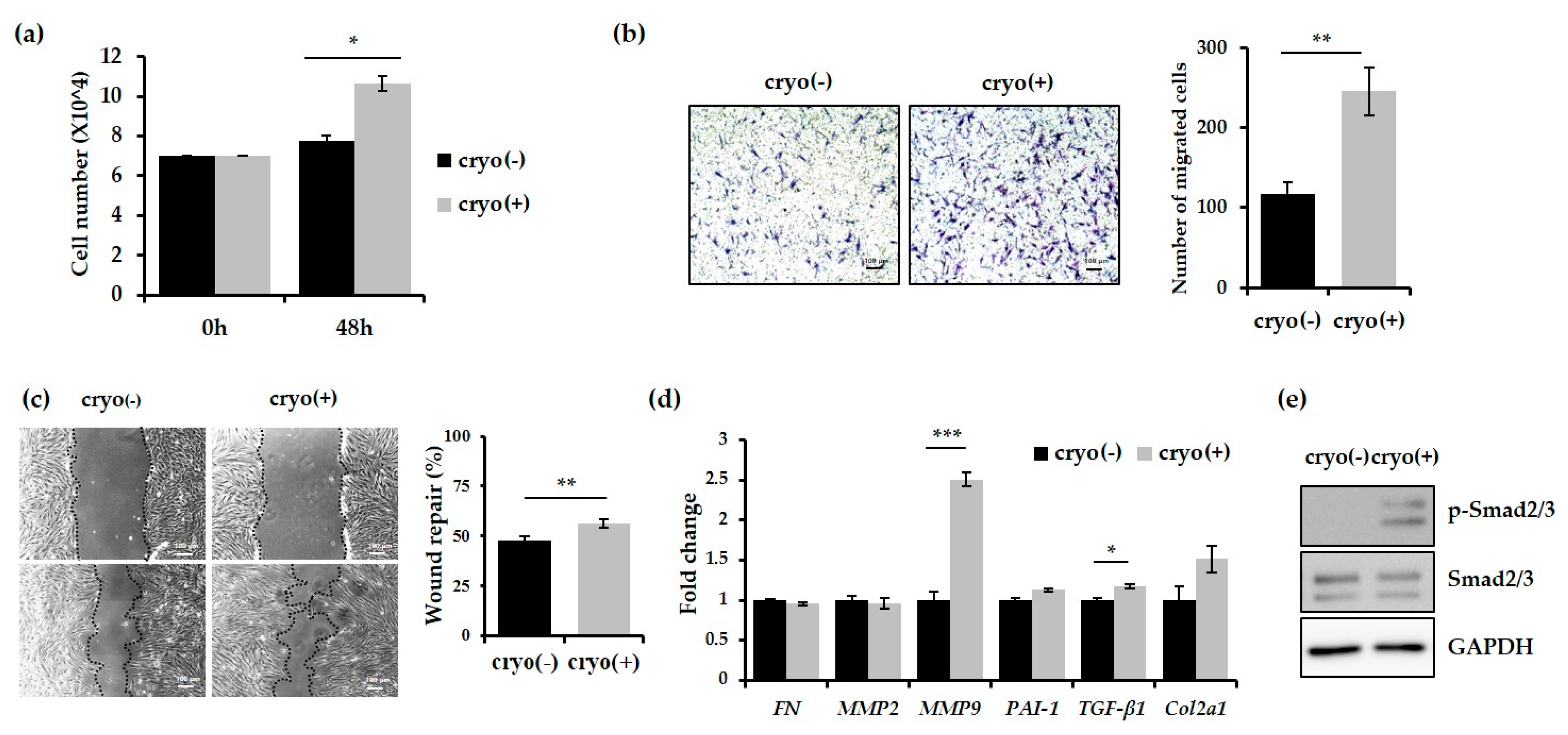
2.4. Expression of MMP9 and TGF-β1 was Increased in Keloids after Treatment with −79 °C Spray-Type CryoPen™
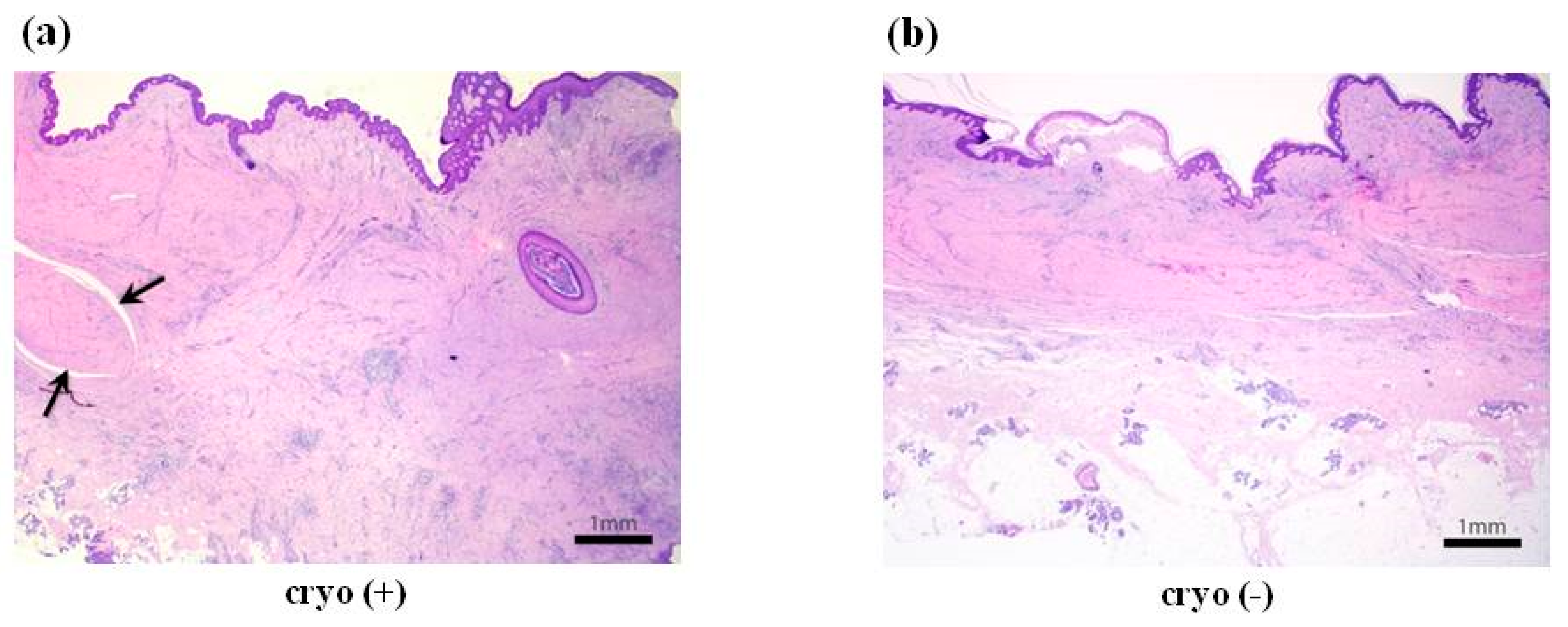
2.5. Cryotherapy-Treated Keloids Showed More Fibrosis and Extensive Lymphoplasmacytic Infiltration
3. Discussion
4. Materials and Methods
4.1. Inclusion and Exclusion Criteria and Study Design
4.2. Cryotherapy Protocol
4.3. Primary Cell Isolation, in Vitro Culture, and Cell Proliferation Assay
4.4. Wound-Healing and Transwell Assay
4.5. Quantitative Real-Time Polymerase Chain Reaction (qRT-PCR)
4.6. Western Blotting
4.7. Pathologic Study
5. Conclusions
Acknowledgments
Conflicts of Interest
Abbreviations
| DMEM | Dulbecco’s modified Eagle’s medium |
| GAPDH | Glyceraldehyde 3-phosphate dehydrogenase |
| MMP9 | Matrix metallopeptidase 9 |
| PBS | Phosphate-buffered saline |
| qRT-PCR | Quantitative real-time polymerase chain reaction |
| TGF-β1 | Transforming growth factor β1 |
References
- Kafka, M.; Collins, V.; Kamolz, L.P.; Rappl, T.; Branski, L.K.; Wurzer, P. Evidence of invasive and noninvasive treatment modalities for hypertrophic scars: A systematic review. Wound Repair Regen. Off. Publ. Wound Heal. Soc. Eur. Tissue Repair Soc. 2017, 25, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Bijlard, E.; Timman, R.; Verduijn, G.M.; Niessen, F.B.; Van Neck, J.W.; Busschbach, J.J.; Mureau, M.A. Intralesional cryotherapy versus excision and corticosteroids or brachytherapy for keloid treatment: Study protocol for a randomised controlled trial. Trials 2013, 14, 439. [Google Scholar] [CrossRef] [PubMed]
- Park, T.H.; Park, J.H.; Tirgan, M.H.; Halim, A.S.; Chang, C.H. Clinical implications of single-versus multiple-site keloid disorder: A retrospective study in an Asian population. Ann. Plast. Surg. 2015, 74, 248–251. [Google Scholar] [CrossRef] [PubMed]
- Savion, Y.; Sela, M. Prefabricated pressure earring for earlobe keloids. J. Prosthet. Dent. 2008, 99, 406–407. [Google Scholar] [CrossRef]
- Guan, H.; Zhao, Z.; He, F.; Zhou, Q.; Meng, Q.; Zhu, X.; Zheng, Z.; Hu, D.; Chen, B. The effects of different thawing temperatures on morphology and collagen metabolism of −20 degrees C dealt normal human fibroblast. Cryobiology 2007, 55, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, R. Keloid and Hypertrophic Scars Are the Result of Chronic Inflammation in the Reticular Dermis. Int. J. Mol. Sci. 2017, 18, 606. [Google Scholar] [CrossRef] [PubMed]
- Van Leeuwen, M.C.; Bulstra, A.E.; van der Veen, A.J.; Bloem, W.B.; van Leeuwen, P.A.; Niessen, F.B. Comparison of two devices for the treatment of keloid scars with the use of intralesional cryotherapy: An experimental study. Cryobiology 2015, 71, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Tirgan, M. Massive ear keloids: Natural history, evaluation of risk factors and recommendation for preventive measures—A retrospective case series. F1000Research 2016, 5, 2517. [Google Scholar] [CrossRef] [PubMed]
- Weshahy, A.H. Intralesional cryosurgery. A new technique using cryoneedles. J. Dermatol. Surg. Oncol. 1993, 19, 123–126. [Google Scholar] [CrossRef] [PubMed]
- Collier, I.E.; Wilhelm, S.M.; Eisen, A.Z.; Marmer, B.L.; Grant, G.A.; Seltzer, J.L.; Kronberger, A.H.E.C.; He, C.S.; Bauer, E.A.; Goldberg, G.I. H-ras oncogene-transformed human bronchial epithelial cells (TBE-1) secrete a single metalloprotease capable of degrading basement membrane collagen. J. Biol. Chem. 1988, 263, 6579–6587. [Google Scholar] [PubMed]
- Senior, R.M.; Griffin, G.L.; Fliszar, C.J.; Shapiro, S.D.; Goldberg, G.I.; Welgus, H.G. Human 92- and 72-kilodalton type IV collagenases are elastases. J. Biol. Chem. 1991, 266, 7870–7875. [Google Scholar] [PubMed]
- Opdenakker, G.; Van den Steen, P.E.; Van Damme, J. Gelatinase B: A tuner and amplifier of immune functions. Trends Immunol. 2001, 22, 571–579. [Google Scholar] [CrossRef]
- Schonbeck, U.; Mach, F.; Libby, P. Generation of biologically active IL-1β by matrix metalloproteinases: A novel caspase-1-independent pathway of IL-1 beta processing. J. Immunol. 1998, 161, 3340–3346. [Google Scholar] [PubMed]
- Van den Steen, P.E.; Proost, P.; Wuyts, A.; Van Damme, J.; Opdenakker, G. Neutrophil gelatinase B potentiates interleukin-8 tenfold by aminoterminal processing, whereas it degrades CTAP-III, PF-4, and GRO-alpha and leaves RANTES and MCP-2 intact. Blood 2000, 96, 2673–2681. [Google Scholar] [PubMed]
- Li, H.; Nahas, Z.; Feng, F.; Elisseeff, J.H.; Boahene, K. Tissue engineering for in vitro analysis of matrix metalloproteinases in the pathogenesis of keloid lesions. JAMA Facial Plast. Surg. 2013, 15, 448–456. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, Y.; Li, N.; Teng, W.; Wang, M.; Zhang, Y.; Xiao, Z. TGF-beta1 promotes scar fibroblasts proliferation and transdifferentiation via up-regulating MicroRNA-21. Sci. Rep. 2016, 6, 32231. [Google Scholar] [CrossRef] [PubMed]
- Dalkowski, A.; Fimmel, S.; Beutler, C.; Zouboulis, C.C. Cryotherapy modifies synthetic activity and differentiation of keloidal fibroblasts in vitro. Exp. Dermatol. 2003, 12, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Awad, S.M.; Ismail, S.A.; Sayed, D.S.; Refaiy, A.E.; Makboul, R. Suppression of transforming growth factor-β1 expression in keloids after cryosurgery. Cryobiology 2017, 75, 151–153. [Google Scholar] [CrossRef] [PubMed]
- Har-Shai, Y.; Dujovny, E.; Rohde, E.; Zouboulis, C.C. Effect of skin surface temperature on skin pigmentation during contact and intralesional cryosurgery of keloids. J. Eur. Acad. Dermatol. Venereol. JEADV 2007, 21, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Har-Shai, Y.; Mettanes, I.; Zilberstein, Y.; Genin, O.; Spector, I.; Pines, M. Keloid histopathology after intralesional cryosurgery treatment. J. Eur. Acad. Dermatol. Venereol. JEADV 2011, 25, 1027–1036. [Google Scholar] [CrossRef] [PubMed]
- Chong, Y.; Kim, C.W.; Kim, Y.S.; Chang, C.H.; Park, T.H. Complete excision of proliferating core in auricular keloids significantly reduces local recurrence: A prospective study. J. Dermatol. 2017. Available online: http://dx.doi.org/10.1111/1346-8138.14110 (accessed on 30 October 2017).
| No. of Cases (n) | Age (Years) | Gender | Skin Type (Fitzpatrick) | Duration of Scar (Years) | Scar Location | Cause | Sessions (n) | Interval (Weeks) | No. of FTCs (Freeze-Thaw Cycle) (n) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 21 | F | F III-IV | 7 | Upper arm | spontaneous | 4 | 2 | 2 |
| 2 | 21 | F | F III-IV | 7 | Chest wall | spontaneous | 4 | 2 | 2 |
| 3 | 21 | F | F III-IV | 7 | pubis | spontaneous | 4 | 2 | 2 |
| 4 | 21 | F | F III-IV | 7 | Axilla | spontaneous | 4 | 2 | 2 |
| 5 | 56 | F | F I-II | 30 | chest wall | infection | 4 | 2 | 2 |
| 6 | 56 | F | F I-II | 35 | Shoulder | Vaccination | 4 | 2 | 2 |
| 7 | 26 | F | F I-II | 0.5 | Trochanter | Surgery | 4 | 2 | 2 |
| 8 | 33 | F | F I-II | 2 | Lobule | Piercing | 4 | 2 | 2 |
| 9 | 21 | F | F I-II | 3 | Helix | Piercing | 4 | 2 | 2 |
| 10 | 17 | F | F I-II | 3 | Helix | Piercing | 4 | 2 | 2 |
| No. | Gene | Direction | Sequences (5’ to 3’) |
|---|---|---|---|
| 1 | GAPDH | Forward | ACCACAGTCCATGCCATCAC |
| Reverse | TCCACCACCCTGTTGCTGTA | ||
| 2 | fibronectin | Forward | CAGTGGGAGACCTCGAGAAG |
| Reverse | TCCCTCGGAACATCAGAAAC | ||
| 3 | TGFβ1 | Forward | GGACACCAACTATTGCTTCAG |
| Reverse | TCCAGGCTCCAAATGTAGG | ||
| 4 | MMP2 | Forward | ATGACAGCTGCACCACTGAG |
| Reverse | ATTTGTTGCCCAGGAAAGTG | ||
| 5 | MMP9 | Forward | ATTCAGGGAGACGCCCATTT |
| Reverse | CTGCGT TTCCAAACCGAGTT | ||
| 6 | col 2a1 | Forward | GGGAGTAATGCAAGGACCAA |
| Reverse | ATCATCACCAGGCTTTCCAG |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, T.H.; Cho, H.-J.; Lee, J.W.; Kim, C.W.; Chong, Y.; Chang, C.H.; Park, K.-S. Could −79 °C Spray-Type Cryotherapy Be an Effective Monotherapy for the Treatment of Keloid? Int. J. Mol. Sci. 2017, 18, 2536. https://doi.org/10.3390/ijms18122536
Park TH, Cho H-J, Lee JW, Kim CW, Chong Y, Chang CH, Park K-S. Could −79 °C Spray-Type Cryotherapy Be an Effective Monotherapy for the Treatment of Keloid? International Journal of Molecular Sciences. 2017; 18(12):2536. https://doi.org/10.3390/ijms18122536
Chicago/Turabian StylePark, Tae Hwan, Hyeon-Ju Cho, Jang Won Lee, Chan Woo Kim, Yosep Chong, Choong Hyun Chang, and Kyung-Soon Park. 2017. "Could −79 °C Spray-Type Cryotherapy Be an Effective Monotherapy for the Treatment of Keloid?" International Journal of Molecular Sciences 18, no. 12: 2536. https://doi.org/10.3390/ijms18122536






