Polymorphisms of Dopamine Receptor Genes and Risk of L-Dopa–Induced Dyskinesia in Parkinson’s Disease
Abstract
:1. Introduction
2. Results
Dopamine Receptor (DR) Genotypes
3. Discussion
4. Patients and Methods
4.1. Patients
4.2. Genotyping
4.3. Statistics
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Fahn, S. The spectrum of levodopa-induced dyskinesias. Ann. Neurol. 2000, 47, S2–S11. [Google Scholar] [PubMed]
- Jankovic, J. Motor fluctuations and dyskinesias in Parkinson’s disease: Clinical manifestations. Mov. Disord. 2005, 20, S11–S16. [Google Scholar] [CrossRef] [PubMed]
- Brotchie, J.M. Nondopaminergic mechanisms in levodopa-induced dyskinesia. Mov. Disord. 2005, 20, 919–931. [Google Scholar] [CrossRef] [PubMed]
- Fabbrini, G.; Brotchie, J.M.; Grandas, F.; Nomoto, M.; Goetz, G.C. Levodopa-induced dyskinesias. Mov. Disord. 2007, 22, 1379–1389. [Google Scholar] [CrossRef] [PubMed]
- Calabresi, P.; Di Filippo, M.; Ghiglieri, V.; Picconi, B. Molecular mechanisms underlying levodopa-induced dyskinesia. Mov. Disord. 2008, 23, S570–S579. [Google Scholar] [CrossRef] [PubMed]
- Thanvi, B.; Lo, N.; Robinson, T. Levodopa-induced dyskinesia in Parkinson’s disease: Clinical features, pathogenesis, prevention and treatment. Postgrad. Med. J. 2007, 83, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.H.; Buckle, C.E.; van Tol, H.H. Polymorphisms in dopamine receptors: What do they tell us? Eur. J. Pharmacol. 2000, 410, 183–203. [Google Scholar] [CrossRef]
- McAllister, T.W.; Summerall, L. Genetic polymorphisms in the expression and treatment of neuropsychiatric disorders. Curr. Psychiatry Rep. 2003, 5, 400–409. [Google Scholar] [CrossRef] [PubMed]
- Le Foll, B.; Gallo, A.; Le Strat, Y.; Lu, L.; Gorwood, P. Genetics of dopamine receptors and drug addiction: A comprehensive review. Behav. Pharmacol. 2009, 20, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Comi, C.; Marino, F.; Magistrelli, L.; de Marchi, F.; Cantello, R.; Riboldazzi, G.; Bono, G.; Cosentino, M. Polymorphisms of dopamine receptor genes and risk of visual hallucinations in Parkinson’s patients. Eur. J. Clin. Pharmacol. 2016, 72, 1335–1341. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Cho, J.; Lee, E.K.; Park, S.S.; Jeon, B.S. Differential genetic susceptibility in diphasic and peak-dose dyskinesias in Parkinson’s disease. Mov. Disord. 2011, 26, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Rieck, M.; Schumacher-Schuh, A.F.; Altmann, V.; Francisconi, C.L.; Fagundes, P.T.; Monte, T.L.; Callegari-Jacques, S.M.; Rieder, C.R.M.; Hutz, M.H. DRD2 haplotype is associated with dyskinesia induced by levodopa therapy in Parkinson’s disease patients. Pharmacogenomics 2012, 13, 1701–1710. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, N.; Vituri, A.; Korczyn, A.D.; Cohen, O.S.; Inzelberg, R.; Yahalom, G.; Kozlova, E.; Milgrom, R.; Laitman, Y.; Friedman, E.; et al. Sequence variants in SLC6A3, DRD2, and BDNF genes and time to levodopa-induced dyskinesias in Parkinson’s disease. J. Mol. Neurosci. 2014, 53, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Ma, J.Z.; Payne, T.J.; Beuten, J.; Dupont, R.T.; Li, M.D. Significant association of DRD1 with nicotine dependence. Hum. Genet. 2008, 123, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Novak, G.; LeBlanc, M.; Zai, C.; Shaikh, S.; Renou, J.; DeLuca, V.; Bulgin, N.; Kennedy, J.L.; le Foll, B. Association of polymorphisms in the BDNF, DRD1 and DRD3 genes with tobacco smoking in schizophrenia. Ann. Hum. Genet. 2010, 74, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Batel, P.; Houchi, H.; Daoust, M.; Ramoz, N.; Naassila, M.; Gorwood, P. A haplotype of the DRD1 gene is associated with alcohol dependence. Alcohol Clin. Exp. Res. 2008, 32, 567–572. [Google Scholar] [CrossRef] [PubMed]
- Ota, V.K.; Spíndola, L.N.; Gadelha, A.; dos Santos Filho, A.F.; Santoro, M.L.; Christofolini, D.M.; Melaragno, M.I. DRD1 rs4532 polymorphism: A potential pharmacogenomic marker for treatment response to antipsychotic drugs. Schizophr. Res. 2012, 142, 206–208. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.D.; Zhang, Y.; Papp, A.C.; Pinsonneault, J.K.; Lim, J.E.; Saffen, D.; Dai, Z.; Wang, D.; Sadée, W. Polymorphisms affecting gene transcription and mRNA processing in pharmacogenetic candidate genes: Detection through allelic expression imbalance in human target tissues. Pharm. Genom. 2008, 18, 781–791. [Google Scholar] [CrossRef] [PubMed]
- Duan, J.; Wainwright, M.S.; Comeron, J.M.; Saitou, N.; Sanders, A.R.; Gelertner, J.; Gejman, P.V. Synonymous mutations in the human dopamine receptor D2 (DRD2) affect mRNA stability and synthesis of the receptor. Hum. Mol. Genet. 2003, 12, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Hirvonen, M.M.; Laakso, A.; Någren, K.; Rinne, J.O.; Pohjalainen, T.; Hietala, J. C957T polymorphism of dopamine D2 receptor gene affects striatal DRD2 in vivo availability by changing the receptor affinity. Synapse 2009, 63, 907–912. [Google Scholar] [CrossRef] [PubMed]
- Lundstrom, K.; Turpin, M.P. Proposed schizophrenia-related gene polymorphism: Expression of the Ser9Gly mutant human dopamine D3 receptor with the Semliki Forest virus system. Biochem. Biophys. Res. Commun. 1996, 225, 1068–1072. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.G.; Lee, B.H.; Lee, J.S.; Chai, Y.G.; Ko, K.P.; Lee, H.J.; Han, D.M.; Ji, H.; Jang, G.H.; Shin, H.E. DRD3 gene rs6280 polymorphism may be associated with alcohol dependence overall and with Lesch type I alcohol dependence in Koreans. Neuropsychobiology 2014, 69, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Kuo, S.C.; Yeh, Y.W.; Chen, C.Y.; Huang, C.C.; Chang, H.A.; Yen, C.H.; Ho, P.S.; Liang, C.; Chou, H.W.; Lu, R.B.; et al. DRD3 variation associates with early-onset heroin dependence, but not specific personality traits. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2014, 51, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Vereczkei, A.; Demetrovics, Z.; Szekely, A.; Sarkozy, P.; Antal, P.; Szilagyi, A.; Sasvari-Szekely, M.; Barta, C. Multivariate analysis of dopaminergic gene variants as risk factors of heroin dependence. PLoS ONE 2013, 8, e66592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simpson, J.; Vetuz, G.; Wilson, M.; Brookes, K.J.; Kent, L. The DRD4 receptor Exon 3 VNTR and 5’ SNP variants and mRNA expression in human post-mortem brain tissue. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2010, 153, 1228–1233. [Google Scholar] [CrossRef] [PubMed]
- Ptácek, R.; Kuzelová, H.; Stefano, G.B. Dopamine D4 receptor gene DRD4 and its association with psychiatric disorders. Med. Sci. Monit. 2011, 17, RA215–RA220. [Google Scholar] [CrossRef] [PubMed]
- Bezard, E.; Ferry, S.; Mach, U.; Stark, H.; Leriche, L.; Boraud, T.; Gross, C.; Sokoloff, P. Attenuation of levodopa-induced dyskinesia by normalizing dopamine D3 receptor function. Nat. Med. 2003, 9, 762–767. [Google Scholar] [CrossRef] [PubMed]
- Lerer, B.; Segman, R.H.; Fangerau, H.; Daly, A.K.; Basile, V.S.; Cavallaro, R.; Masellis, M. Pharmacogenetics of tardive dyskinesia: Combined analysis of 780 patients supports association with dopamine D3 receptor gene Ser9Gly polymorphism. Neuropsychopharmacology 2002, 27, 105–119. [Google Scholar] [CrossRef]
- Steen, V.M.; Lovile, R.; MacEwan, T.; McCreadie, R.G. Dopamine D3-receptor gene variant and susceptibility to tardive dyskinesia in schizophrenic patients. Mol. Psychiatry 1997, 2, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Sethi, K.D.; Morgan, J.C. Drug-induced movement disorders. In Parkinson’s Disease & Movement Disorders, 5th ed.; Jankovic, J., Tolosa, E., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2007; p. 401. [Google Scholar]
- Sharma, S.; Singh, S.; Sharma, V.; Singh, V.P.; Deshmukh, R. Neurobiology of l-DOPA induced dyskinesia and the novel therapeutic strategies. Biomed. Pharmacother. 2015, 70, 283–293. [Google Scholar] [CrossRef] [PubMed]
- Goetz, C.G.; Burke, P.F.; Leurgans, S.; Berry-Kravis, E.; Blasucci, L.M.; Raman, R.; Zhou, L. Genetic variation analysis in Parkinson disease patients with and without hallucinations: Case-control study. Arch. Neurol. 2001, 58, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Hugher, A.J.; Daniel, S.E.; Kilford, L.; Lees, A.J. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: A clinical pathological study of 100 cases. J. Neurol. Neurosurg. Psychiatry 1992, 55, 181–184. [Google Scholar] [CrossRef]
- Tomlinson, C.L.; Stowe, R.; Patel, S.; Rick, C.; Gray, R.; Clarke, C.E. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov. Disord. 2010, 25, 2649–2653. [Google Scholar] [CrossRef] [PubMed]
- George, S.R.; Cheng, R.; Nguyen, T.; Israel, Y.; O’Dowd, B.F. Polymorphisms of the D4 dopamine receptor alleles in chronic alcoholism. Biochem. Biophys. Res. Commun. 1993, 196, 107–114. [Google Scholar] [CrossRef] [PubMed]
| Feature | No Dyskinesia | Dyskinesia | p |
|---|---|---|---|
| Number of subjects | 50 | 50 | |
| Gender, male/female | 28/22 | 28/22 | na |
| Age at onset, mean ± SD | 65.1 ± 5.6 | 63.3 ± 9.8 | ns |
| Disease duration (years) mean ± SD | 10.8 ± 4.2 | 12.1 ± 5.2 | ns |
| Dyskinesia onset (years) mean ± SD | na | 7.6 ± 4.2 | na |
| UPDRS III, mean ± SD * | |||
| ON | 24 ± 10 | 23 ± 9 | ns |
| OFF | 29 ± 13 | 28 ± 12 | ns |
| Hoehn and Yahr, median (range) * | 3 (1–4) | 3 (1–4) | na |
| L-dopa treatment duration (years) mean ± SD | 8.9 ± 3.4 | 9.6 ± 3.3 | ns |
| Medication dose LED (mg/day), mean ± SD * | 612.6 ± 242.6 | 741 ± 279.6 | ns |
| Gene | SNP | Genotype | No Dyskinesia Dyskinesia Dyskinesia | Dyskinesia | P (a) | P (b) | OR (95% CI) |
|---|---|---|---|---|---|---|---|
| DRD1 | rs4532 | A/A | 11 (22%) | 11 (22%) | ns | ns | ns |
| A/G | 21 (42%) | 20 (40%) | |||||
| G/G | 18 (36%) | 19 (38%) | |||||
| rs686 | C/C | 17 (34%) | 15 (30%) | ns | ns | ns | |
| C/T | 25 (50%) | 25 (50%) | |||||
| T/T | 8 (16%) | 10 (20%) | |||||
| DRD5 | rs6283 | T/T | 33 (66%) | 35 (70%) | ns | ns | ns |
| T/C | 13 (26%) | 15 (30%) | |||||
| C/C | 4 (8%) | 0 (0%) | |||||
| DRD2 | rs1800497 | G/G | 36 (72%) | 22 (44%) | ns | ns | ns |
| G/A | 11 (22%) | 25 (50%) | |||||
| A/A | 3 (6%) | 3 (6%) | |||||
| rs6277 | C/C | 21 (42%) | 11 (22%) | ns | ns | ns | |
| C/T | 20 (40%) | 28 (56%) | |||||
| T/T | 9 (18%) | 11 (22%) | |||||
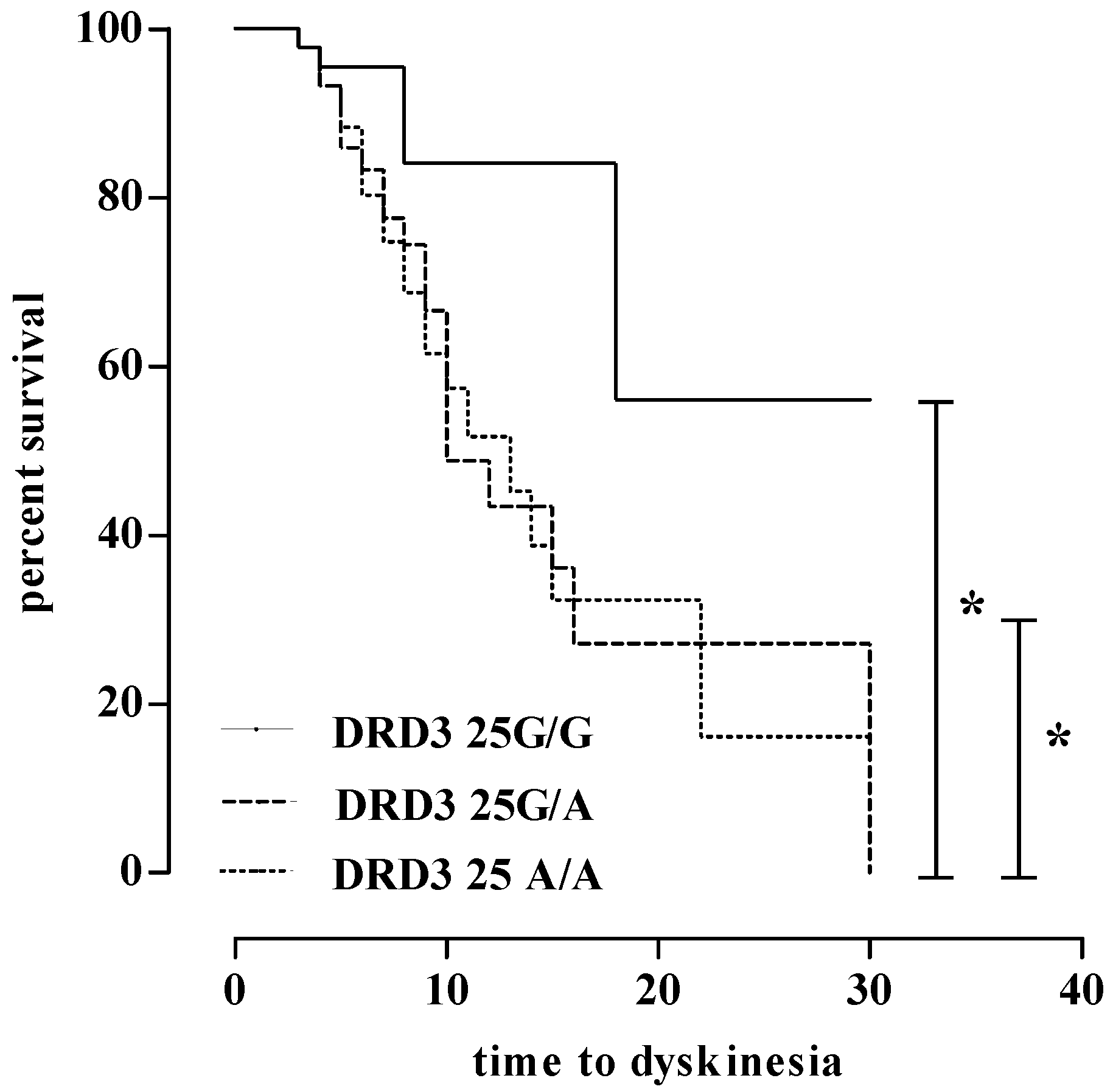
| DRD3 | rs6280 | G/G | 26 (52%) | 9 (18%) | 0.0001 | 0.0001 | 4.9 (2.0–12.2) |
| G/A | 18 (36%) | 21 (42%) | |||||
| A/A | 6 (12%) | 20 (40%) | |||||
| rs1800828 | G/G | 38 (76%) | 39 (78%) | ns | ns | ns | |
| G/C | 8 (16%) | 11 (224%) | |||||
| C/C | 4 (8%) | 0 (0%) | |||||
| DRD4 | nR VNTR 48 bp repetition | 4/4 | 33 (66%) | 31 (62%) | ns | ns | ns |
| 4/7 | 16 (32%) | 18 (36%) | |||||
| 7/7 | 1 (2%) | 1 (2%) | |||||
| rs747302 | C/C | 39 (78%) | 42 (84%) | ns | ns | ns | |
| C/G | 11 (22%) | 8 (16%) | |||||
| G/G | 0 (26.4%) | 0 (0%) |
| Receptor | Gene | Variant | Change | Frequency | Effects | Score |
|---|---|---|---|---|---|---|
| D1-like | ||||||
| D1 | DRD1 | rs4532 | −48A>G | 60 (%) | Association with nicotine dependence [14], tobacco smoking in schizophrenia [15], and alcohol dependence [16] and resistance to schizophrenia treatment [17]. | +1 |
| rs686 | 62C>T | 55 (%) | Higher DRD1 gene expression and association with nicotine dependence [14], alcohol dependence [17], and tobacco smoking in schizophrenia [15]. | +1 | ||
| D5 | DRD5 | rs6283 | 978T>C | 30 (%) | na | na |
| D2-like | ||||||
| D2 | DRD2 | rs1800497 | 2137G>A (Taq1A) | 15 (%) | Lower striatal DR D2 density in healthy [18]. | +1 |
| rs6277 | 957C>T | 50 (%) | Decreased DR D2 mRNA stability and translation, and reduced dopamine-induced up-regulation of DR D2 membrane expression in vitro [19], and lower DR D2 expression in cortex and thalamus of healthy subjects [20]. | +1 | ||
| D3 | DRD3 | rs6280 | 25G>A (Ser9Gly) | 60 (%) | Higher dopamine binding affinity in vitro [21], association with alcohol dependence [22] and heroin dependence [23]. | −1 |
| rs1800828 | −712G>C | 20 (%) | na | na | ||
| D4 | DRD4 | rs747302 | −616C>G | 10 (%) | No effect on DR D4 mRNA expression in human post-mortem brain tissue samples [23], and no association with heroin dependence [24]. | na |
| 7 48-base pair VNTR | 20 (%) | Trend toward reduced DR D4 mRNA expression in human post-mortem brain tissue samples [25], lower response to stimulants and requirements of higher doses of methylphenidate [26]. | +1 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Comi, C.; Ferrari, M.; Marino, F.; Magistrelli, L.; Cantello, R.; Riboldazzi, G.; Bianchi, M.L.E.; Bono, G.; Cosentino, M. Polymorphisms of Dopamine Receptor Genes and Risk of L-Dopa–Induced Dyskinesia in Parkinson’s Disease. Int. J. Mol. Sci. 2017, 18, 242. https://doi.org/10.3390/ijms18020242
Comi C, Ferrari M, Marino F, Magistrelli L, Cantello R, Riboldazzi G, Bianchi MLE, Bono G, Cosentino M. Polymorphisms of Dopamine Receptor Genes and Risk of L-Dopa–Induced Dyskinesia in Parkinson’s Disease. International Journal of Molecular Sciences. 2017; 18(2):242. https://doi.org/10.3390/ijms18020242
Chicago/Turabian StyleComi, Cristoforo, Marco Ferrari, Franca Marino, Luca Magistrelli, Roberto Cantello, Giulio Riboldazzi, Maria Laura Ester Bianchi, Giorgio Bono, and Marco Cosentino. 2017. "Polymorphisms of Dopamine Receptor Genes and Risk of L-Dopa–Induced Dyskinesia in Parkinson’s Disease" International Journal of Molecular Sciences 18, no. 2: 242. https://doi.org/10.3390/ijms18020242









