Visualization of Alternative Functional Configurations of Influenza Virus Hemagglutinin Facilitates Rapid Selection of Complementing Vaccines in Emergency Situations
Abstract
:1. Introduction
2. Results and Discussion
2.1. Hypothesis Developoment
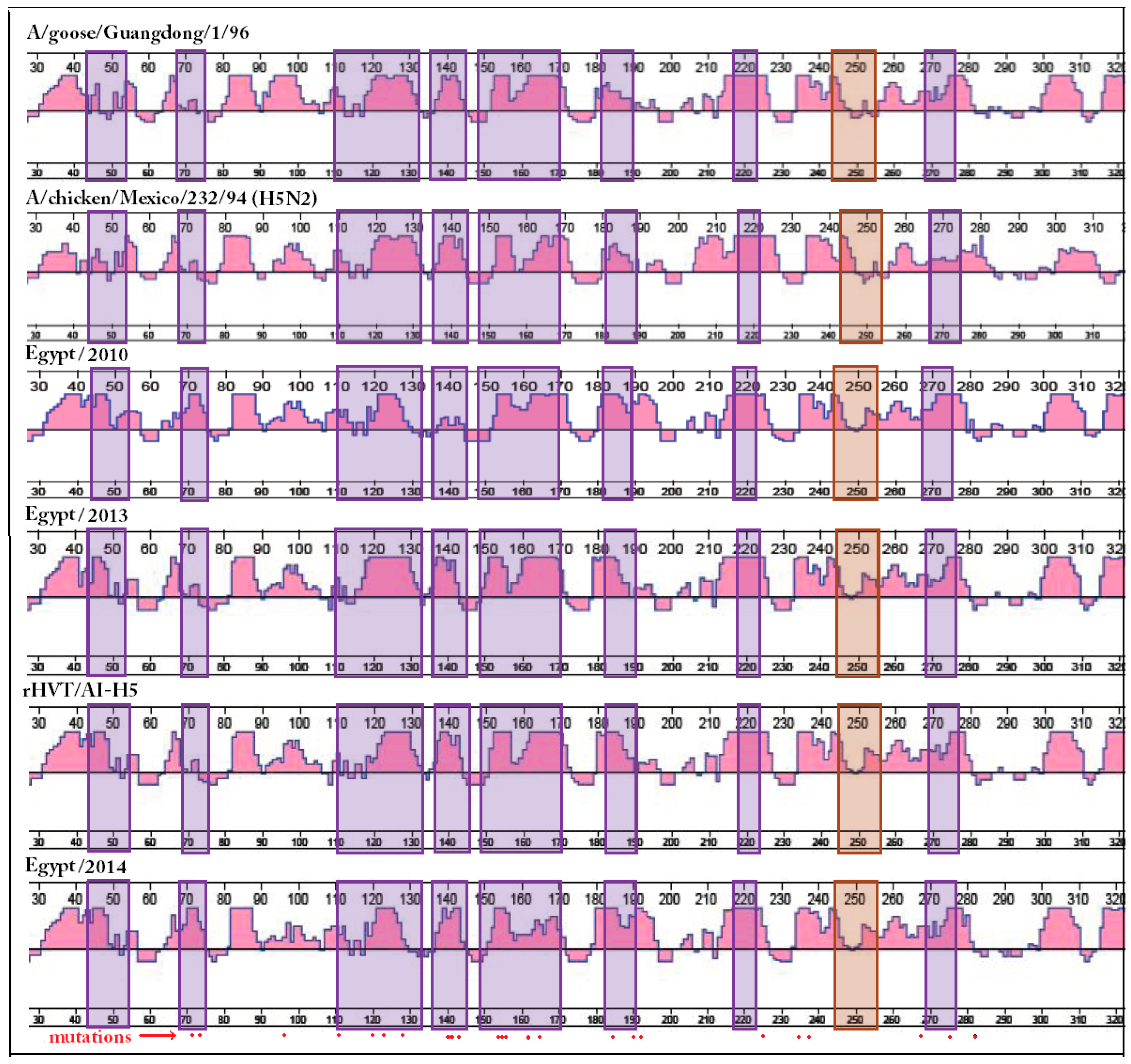
2.2. One-Dimensional Analysis Is Not Appropriate for Alternative Functional Configurations (AFC) Recognition
2.3. Two-Dimensional Analysis Is Not Suitable for AFC Definition
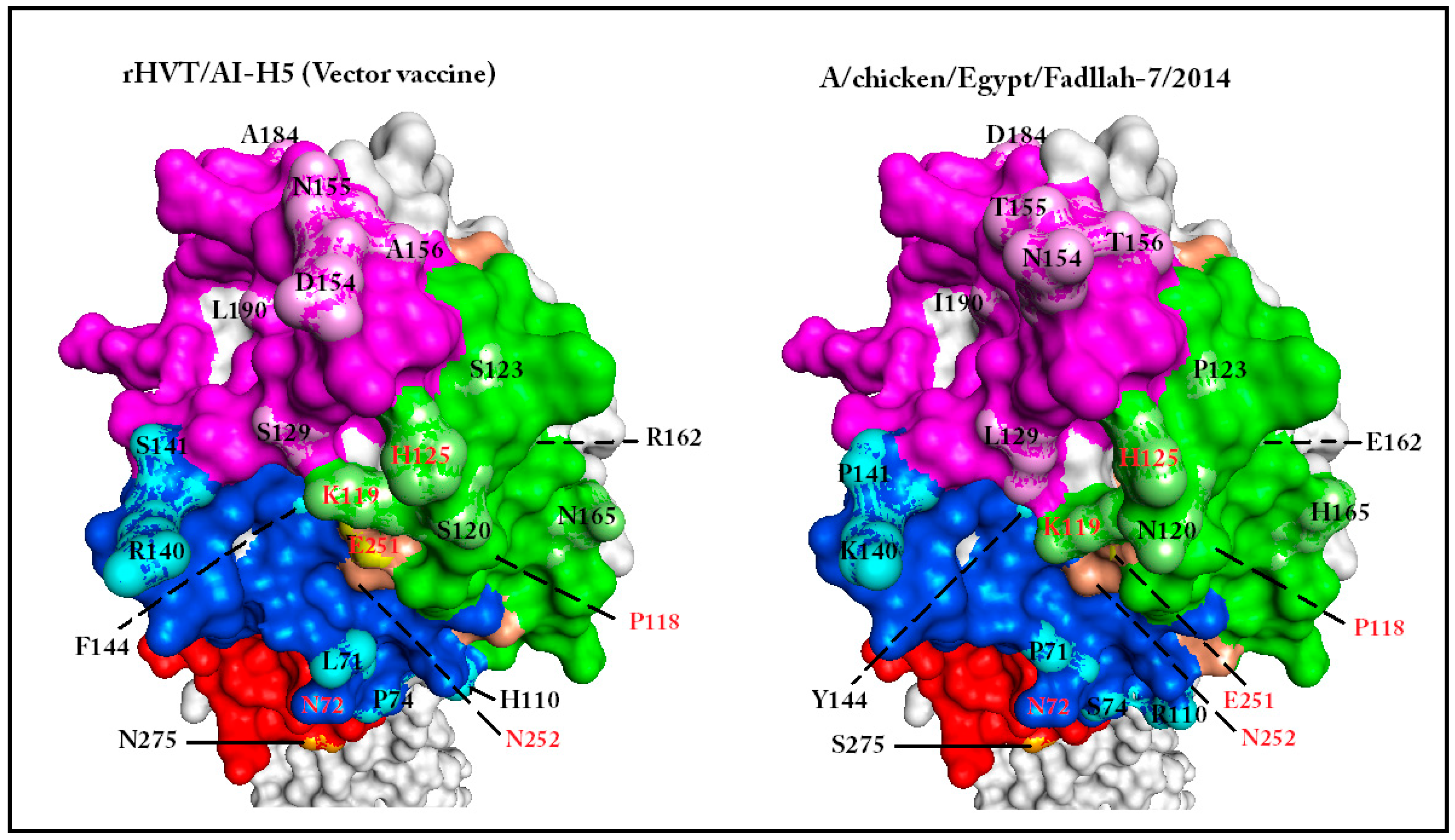
2.4. Three-Dimensional (3D) Homology-Based Modeling That Conserves the Backbone of the Template Used for Comparison Can Be Used to Visualize the Effect of Cis- and Trans- Mutations on HA1 Surface Topology Elements
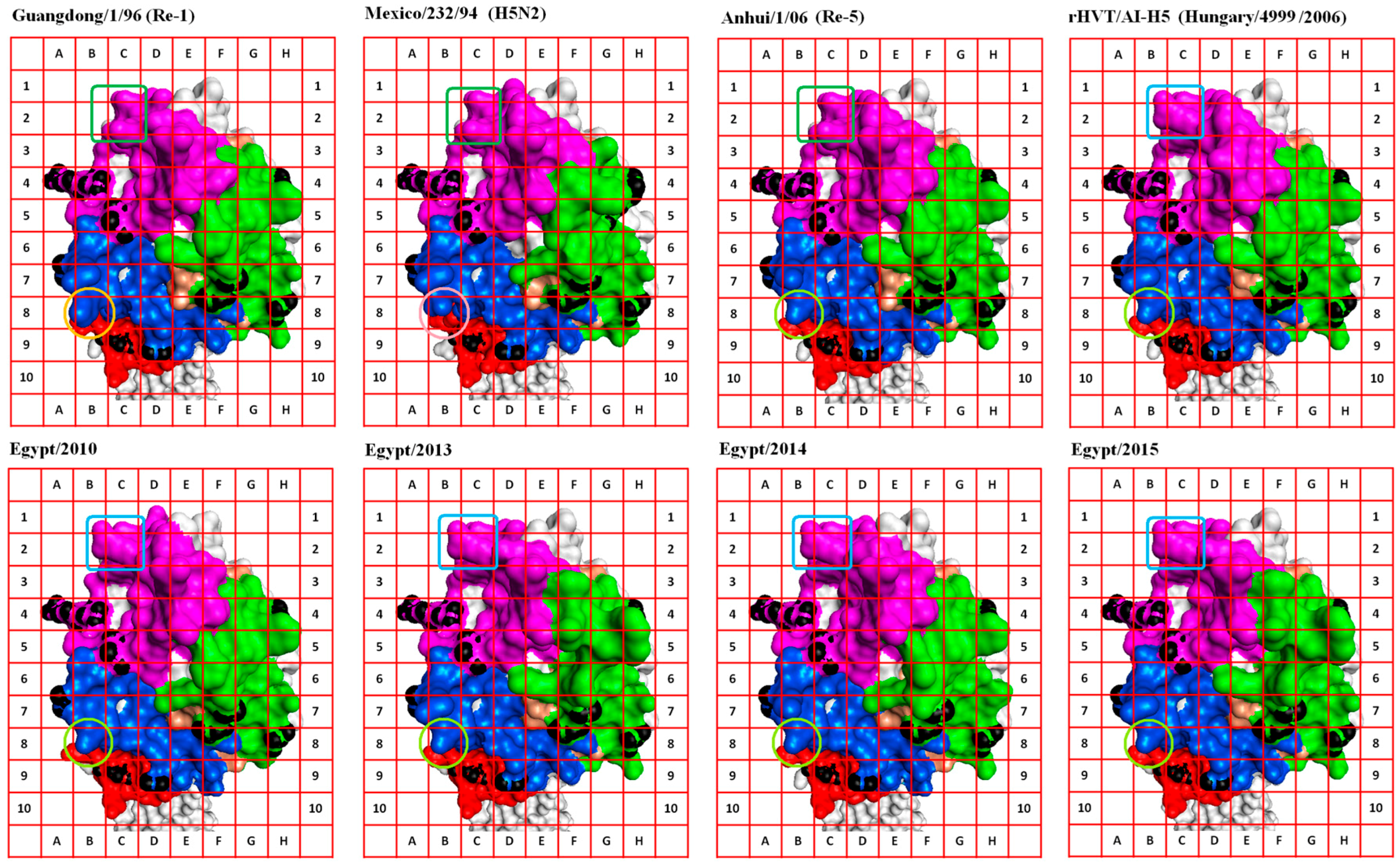
2.5. Alternative Functional Configurations (AFC) Can Be Visualized Using Anchored Homology-Based 3D Models in Solvent Accessibility View
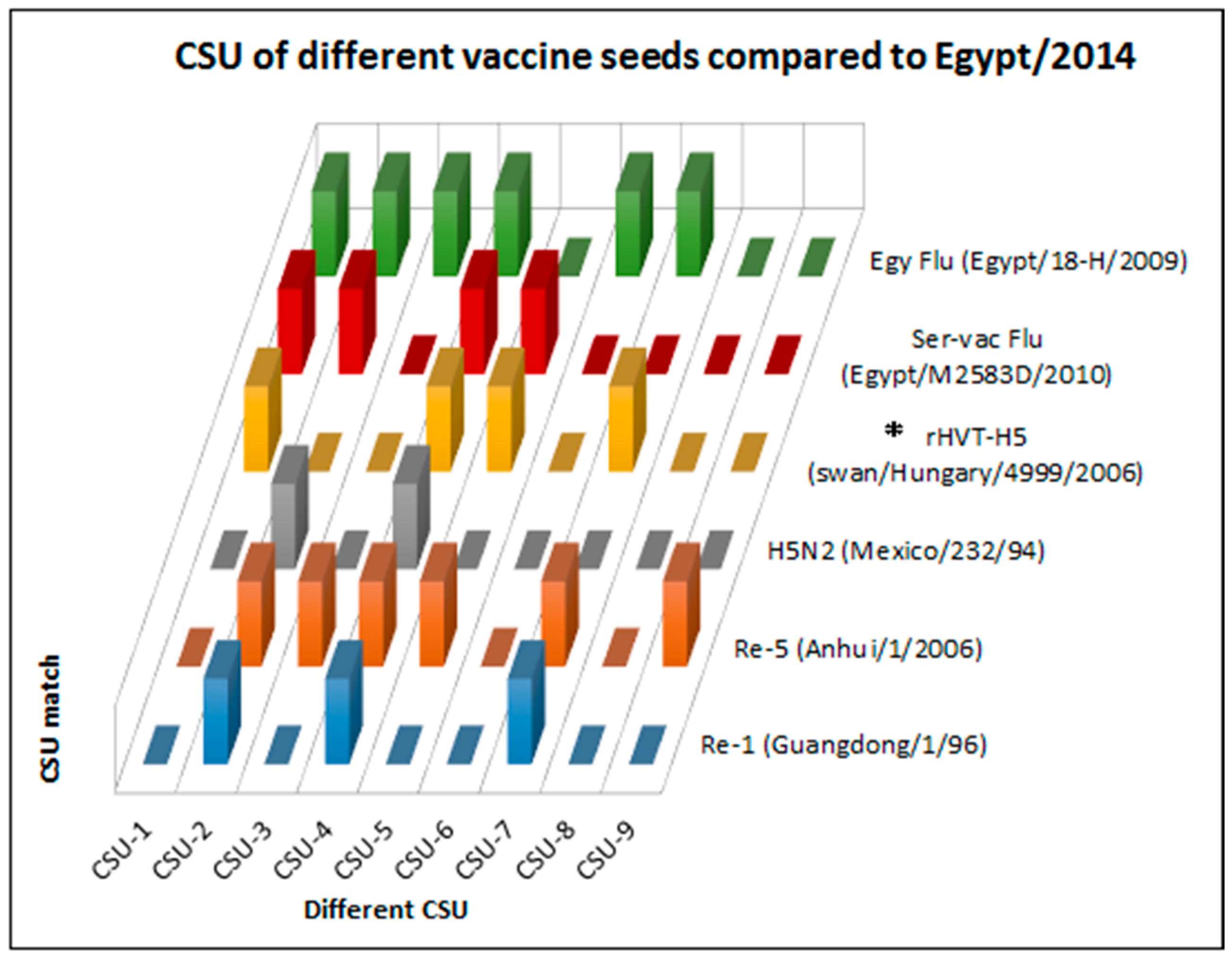
2.6. Visualization of Hemagglutinin (HA) AFC Facilitates Complementing Structural Units (CSU) Selection from Available Vaccines to Protect against Emerging Avian Influenza Virus (AIV) Strains
3. Materials and Methods
3.1. Field Cases of Highly Pathogenic (HP) Avian Influenza (AI) in Vaccinated Flocks
3.2. HA Sequences of Vaccine Seed and Egyptian Field Viruses Studied
3.3. Sequence Analysis and Phylogeny
3.4. Two Dimensional Analysis
3.5. Three-Dimensional Modeling
3.6. CSU Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Conflicts of Interest
Abbreviations
| 1D | One dimension |
| 2D | Two dimension |
| 3D | Three dimension |
| AFC | Alternative functional configurations |
| AI | Avian influenza |
| AIV | Avian influenza virus |
| AS | Anchor Sites |
| CASP | Critical Assessment of protein Structure Prediction |
| CDR | Complementarity determining regions |
| CSU | Complementing structural units |
| FC | Fitness condition |
| GISAID | Global Initiative on Sharing All Influenza data |
| GMT | Geometric mean titer |
| HA | Hemagglutinin |
| HI | Hemagglutination inhibition |
| HP | Highly pathogenic |
| IAV | Influenza A virus |
| KDa | Kilo Dalton |
| mAbs | Monoclonal antibodies |
| nAbs | Neutralizing antibodies |
| NCBI | National Center for Biotechnology Information |
| PDB | Protein Data Bank |
| RBS | Receptor binging site |
| VS | Vulnerable sites |
References
- Rushton, J.; Viscarra, R.; Bleich, E.G.; McLeod, A. Impact of avian influenza outbreaks in the poultry sectors of five South East Asian countries (Cambodia, Indonesia, Lao PDR, Thailand, Viet Nam) outbreak costs, responses and potential long term control. Worlds Poult. Sci. J. 2005, 61, 491–514. [Google Scholar] [CrossRef]
- Peiris, J.S.; de Jong, M.D.; Guan, Y. Avian influenza virus (H5N1): A threat to human health. Clin. Microbiol. Rev. 2007, 20, 243–267. [Google Scholar] [CrossRef] [PubMed]
- Lamb, R.A.; Krug, R.M. Orthomyxoviridae: The viruses and their replication. In Fields Virology, 4th ed.; Knipe, D.M., Howley, P.M., Eds.; Lippincott: Philadelphia, PA, USA, 2001; pp. 1487–1531. [Google Scholar]
- Boltz, D.A.; Douangngeun, B.; Phommachanh, P.; Sinthasak, S.; Mondry, R.; Obert, C.; Seiler, P.; Keating, R.; Suzuki, Y.; Hiramatsu, H.; et al. Emergence of H5N1 avian influenza viruses with reduced sensitivity to neuraminidase inhibitors and novel reassortants in Lao People’s Democratic Republic. J. Gen. Virol. 2010, 91, 949–959. [Google Scholar] [CrossRef] [PubMed]
- Abdelwhab, E.M.; Hassan, M.K.; Abdel-Moneim, A.S.; Naguib, M.M.; Mostafa, A.; Hussein, I.T.M.; Arafa, A.; Erfan, A.M.; Kilany, W.H.; Agour, M.G.; et al. Introduction and enzootic of A/H5N1 in Egypt: Virus evolution, pathogenicity and vaccine efficacy ten years on. Infect. Genet. Evol. 2016, 40, 80–90. [Google Scholar] [CrossRef] [PubMed]
- Domingo, E.; Sheldon, J.; Perales, C. Viral Quasispecies Evolution. Microbiol. Mol. Biol. Rev. 2012, 76, 159–216. [Google Scholar] [CrossRef] [PubMed]
- Grund, C.; Abdelwhab, S.M.; Arafa, A.S.; Ziller, M.; Hassan, M.K.; Aly, M.M.; Hafez, H.M.; Harder, T.C.; Beer, M. Highly pathogenic avian influenza virus H5N1 from Egypt escapes vaccine-induced immunity but confers clinical protection against a heterologous clade 2.2.1 Egyptian isolate. Vaccine 2011, 29, 5567–5573. [Google Scholar] [CrossRef] [PubMed]
- Naguib, M.M.; Abdelwhab, E.M.; Harder, T.C. Evolutionary features of influenza A/H5N1 virus populations in Egypt: Poultry and human health implications. Arch. Virol. 2016, 161, 1963–1967. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, T.; Lambrecht, B.; Marché, S.; Steensels, M.; van Borm, S.; Bublo, M. Influenza vaccines and vaccination strategies in birds. Comp. Immunol. Microbiol. Infect. Dis. 2008, 31, 121–165. [Google Scholar] [CrossRef] [PubMed]
- Swayne, D.E. Avian influenza vaccines and therapies for poultry. Comp. Immunol. Microbiol. Infect. Dis. 2009, 32, 351–363. [Google Scholar] [CrossRef] [PubMed]
- Terrestrial Manual, Chapter 2.3.4—Avian Influenza. Available online: http://www.oie.int/international-standard-setting/terrestrial-manual/access-online/ (accessed on 22 December 2016).
- Kaminski, D.A.; Lee, F.E. Antibodies against conserved antigens provide opportunities for reform in influenza vaccine design. Front. Immunol. 2011, 2, 76. [Google Scholar] [CrossRef] [PubMed]
- Mair, C.M.; Ludwig, K.; Herrmann, A.; Sieben, C. Receptor binding and pH stability—How influenza A virus hemagglutinin affects host-specific virus infection. Biochim. Biophys. Acta 2013, 1838, 1153–1168. [Google Scholar] [CrossRef] [PubMed]
- Skehel, J.J.; Wiley, D.C. Receptor binding and membrane fusion in virus entry: The influenza hemagglutinin. Annu. Rev. Biochem. 2000, 69, 531–569. [Google Scholar] [CrossRef] [PubMed]
- Zou, W.; Ke, J.; Zhu, J.; Zhou, H.; Jin, M. The antigenic property of the H5N1 avian influenza viruses isolated in central China. Virol. J. 2012, 9, 148. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.G.; Jiang, W.M.; Liu, S.; Hou, G.Y.; Li, J.P.; Wang, Z.Y.; Chen, J.M. Increased substitution rate in H5N1 avian influenza viruses during mass vaccination of poultry. Sci. Bull. 2012, 57, 2419–2424. [Google Scholar] [CrossRef]
- Zuo, T.; Sun, J.; Wang, G.; Jiang, L.; Zuo, Y.; Li, D.; Shi, X.; Liu, X.; Fan, S.; Ren, H.; et al. Comprehensive analysis of antibody recognition in convalescent humans from highly pathogenic avian influenza H5N1 infection. Nat. Commun. 2015, 6, 8855. [Google Scholar] [CrossRef] [PubMed]
- Shore, D.A.; Yang, H.; Balish, A.L.; Shepard, S.S.; Carney, P.J.; Chang, J.C.; Davis, C.T.; Donis, R.O.; Villanueva, J.M.; Klimov, A.I.; et al. Structural and Antigenic Variation among Diverse Clade 2 H5N1 Viruses. PLoS ONE 2013, 8, e75209. [Google Scholar]
- Kayali, G.; Kandeil, A.; El-Shesheny, R.; Kayed, A.S.; Maatouq, A.M.; Cai, Z.; McKenzie, P.; Webby, R.J.; El Refaey, S.; Kandeel, A.; et al. Avian influenza A (H5N1) virus in Egypt. Emerg. Infect. Dis. 2016, 22, 379–388. [Google Scholar] [CrossRef] [PubMed]
- Read, A.F.; Baigent, S.J.; Powers, C.; Kgosana, L.B.; Blackwell, L.; Smith, L.P.; Kennedy, D.A.; Walkden-Brown, S.W.; Nair, V.K. Imperfect vaccination can enhance the transmission of highly virulent pathogens. PLoS Biol. 2015, 13, e1002198. [Google Scholar] [CrossRef] [PubMed]
- Aly, M.M.; Arafa, A.; Hassan, M.K. Epidemiological findings of outbreaks of disease caused by highly pathogenic H5N1 avian influenza virus in poultry in Egypt during 2006. Avian Dis. 2008, 52, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Ibrahim, M.S.; Ellakany, H.F.; Kawashita, N.; Daidoji, T.; Takagi, T.; Yasunaga, T.; Nakaya, T.; Ikuta, K. Antigenic analysis of highly pathogenic avian influenza virus H5N1 sublineages co-circulating in Egypt. J. Gen. Virol. 2012, 93 Pt 10, 2215–2226. [Google Scholar] [CrossRef] [PubMed]
- Beato, M.S.; Mancin, M.; Yang, J.; Buratin, A.; Ruffa, M.; Maniero, S.; Fusaro, A.; Terregino, C.; Wan, X.F.; Capua, I. Antigenic characterization of recent H5N1 highly pathogenic avian influenza viruses circulating in Egyptian poultry. Virology 2013, 435, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Hoper, D.; Kalthoff, D.; Hoffmann, B.; Beer, M. Highly pathogenic avian influenza virus subtype H5N1 escaping neutralization: More than HA variation. J. Virol. 2012, 86, 1394–1404. [Google Scholar] [CrossRef] [PubMed]
- Arafa, A.; Suarez, D.; Kholosy, S.G.; Hassan, M.K.; Nasef, S.; Selim, A.; Dauphin, G.; Kim, M.; Yilma, J.; Swayne, D.; et al. Evolution of highly pathogenic avian influenza H5N1 viruses in Egypt indicating progressive adaptation. Arch. Virol. 2012, 157, 1931–1947. [Google Scholar] [CrossRef] [PubMed]
- Peyre, M.; Samaha, H.; Makonnen, Y.J.; Saad, A.; Abd-Elnabi, A.; Galal, S.; Ettel, T.; Dauphin, G.; Lubroth, J.; Roger, F.; et al. Avian influenza vaccination in Egypt: Limitations of the current strategy. J. Mol. Genet. Med. 2009, 3, 198–204. [Google Scholar] [PubMed]
- Capua, I.; Marangon, S. The challenge of controlling notifiable avian influenza by means of vaccination. Avian Dis. 2007, 51, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Ng, Q.; Jia, Q.; Kwang, J.; He, F. A novel humanized antibody neutralizes H5N1 influenza virus via two different mechanisms. J. Virol. 2015, 89, 3712–3722. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Zeng, Q.; Glisson, J.R.; Jackwood, M.W.; Cheng, I.H.; Wang, C. Sequence analysis of Pasteurella multocida major outer membrane protein (OmpH) and application of synthetic peptides in vaccination of chickens against homologous strain challenge. Vaccine 1999, 17, 821–831. [Google Scholar] [CrossRef]
- Xiong, X.; Corti, D.; Liu, J.; Pinna, D.; Foglierini, M.; Calder, L.J.; Skehel, J.J. Structures of complexes formed by H5 influenza hemagglutinin with a potent broadly neutralizing human monoclonal antibody. Proc. Natl. Acad. Sci. USA 2015, 112, 9430–9435. [Google Scholar] [CrossRef] [PubMed]
- Jameson, B.A.; Wolf, H. The antigenic index: A novel algorithm for predicting antigenic determinants. Comput. Appl. Biosci. 1988, 4, 181–186. [Google Scholar] [CrossRef]
- Li, J.; Wang, Y.; Liang, Y.; Ni, B.; Wan, Y.; Liao, Z.; Chan, K.H.; Yuen, K.Y.; Fu, X.; Shang, X.; et al. Fine antigenic variation within H5N1 influenza virus hemagglutinin’s antigenic sites defined by yeast cell surface display. Eur. J. Immunol. 2009, 39, 3498–3510. [Google Scholar] [CrossRef] [PubMed]
- Prabakaran, M.; Prabhu, N.; He, F.; Hongliang, Q.; Ho, H.; Qiang, J.; Meng, T.; Goutama, M.; Kwang, J. Combination therapy using chimeric monoclonal antibodies. PLoS ONE 2009, 4, e5672. [Google Scholar] [CrossRef] [PubMed]
- Schwede, T. Protein modeling: What happened to the “protein structure gap”? Structure 2013, 21, 1531–1540. [Google Scholar] [CrossRef] [PubMed]
- Ingale, A.G. In silico homology modeling and epitope prediction of nucleocapsid protein region from Japanese encephalitis virus. J. Comput. Sci. Syst. Biol. 2010, 3, 53–58. [Google Scholar]
- Kelley, L.A.; Mezulis, S.; Yates, C.M.; Wass, M.N.; Sternberg, M.J. The Phyre2 web portal for protein modeling, prediction and analysis. Nat. Protoc. 2015, 10, 845–858. [Google Scholar] [CrossRef] [PubMed]
- PDB, Protein Data Bank. Available online: http://www.rcsb.org/pdb/ (accessed on 14 December 2015).
- Berman, H.M.; Westbrook, J.; Feng, Z.; Gilliland, G.; Bhat, T.N.; Weissig, H.; Shindyalov, I.N.; Bourne, P.E. The protein data bank. Nucleic Acids Res. 2000, 28, 235–242. [Google Scholar] [CrossRef] [PubMed]
- CASP, Protein Structure Prediction Center. Available online: http://predictioncenter.org/index.cgi (accessed on 11 March 2016).
- I-TASSER. Available online: http://zhanglab.ccmb.med.umich.edu/I-TASSER/ (accessed on 9 April 2016).
- CASP11. Available online: http://www.predictioncenter.org/casp11/index.cgi (accessed on 11 March 2016).
- Roy, A.; Kucukural, A.; Zhang, Y. I-TASSER: A unified platform for automated protein structure and function prediction. Nat. Protoc. 2010, 5, 725–738. [Google Scholar] [CrossRef] [PubMed]
- Lodish, H.; Berk, A.; Zipursky, S.L. Section 3.1, Hierarchical Structure of Proteins. In Molecular Cell Biology, 4th ed.; Freeman, W.H.: New York, NY, USA, 2000. Available online: http://www.ncbi.nlm.nih.gov/books/NBK21581/ (accessed on 16 April 2016).
- Solvent Accessibility Dialog, Discovery Studio 4.1. Available online: file:///C:/Program%20Files/Accelrys/Discovery%20Studio%204.1/share/doc/DSV/DSV.htm#DocDS\Client\dl_solvent-accessibility.htm (accessed on 6 May 2016).
- Phyre2. Protein Fold Recognition Server. Available online: http://www.sbg.bio.ic.ac.uk/phyre2/ (accessed on 14 April 2016).
- Cueno, M.E.; Imai, K.; Ochiai, K. Structural insights on the potential significance of the twin Asn-residue found at the base of the hemagglutinin 2 stalk in all influenza A H1N1 strains: A computational study with clinical implications. OMICS 2013, 17, 297–301. [Google Scholar] [CrossRef] [PubMed]
- El-Shesheny, R.; Kandeil, A.; Bagato, O.; Maatouq, A.M.; Moatasim, Y.; Rubrum, A.; Song, M.S.; Webby, R.J.; Ali, M.A.; Kayali, G. Molecular characterization of avian influenza H5N1 virus in Egypt and the emergence of a novel endemic subclade. J. Gen. Virol. 2014, 95, 1444–1463. [Google Scholar] [CrossRef] [PubMed]
- Tate, M.D.; Job, E.R.; Deng, Y.M.; Gunalan, V.; Maurer-Stroh, S.; Reading, P.C. Playing hide and seek: How glycosylation of the influenza virus hemagglutinin can modulate the immune response to infection. Viruses 2013, 6, 1294–1316. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.; Blixt, O.; Tumpey, T.M.; Taubenberger, J.K.; Paulson, J.C.; Wilson, I.A. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science 2006, 312, 404–410. [Google Scholar] [CrossRef] [PubMed]
- Rudneva, I.A.; Timofeeva, T.A.; Ignatieva, A.V.; Shilov, A.A.; Krylov, P.S.; Ilyushina, N.A.; Kaverin, N.V. Pleiotropic effects of hemagglutin in amino acid substitutions of H5 influenza escape mutants. Virology 2013, 447, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Prabakaran, M.; He, F.; Meng, T.; Madhan, S.; Yunrui, T.; Jia, Q.; Kwang, J. Neutralizing epitopes of influenza virus hemagglutinin: Target for the development of a universal vaccine against H5N1 lineages. J. Virol. 2010, 84, 11822–11830. [Google Scholar] [CrossRef] [PubMed]
- Schmier, S.; Mostafa, A.; Haarmann, T.; Bannert, N.; Ziebuhr, J.; Veljkovic, V.; Dietrich, U.; Pleschka, S. In silico prediction and experimental confirmation of ha residues conferring enhanced human receptor specificity of H5N1 influenza A viruses. Sci. Rep. 2015, 5, 11434. [Google Scholar] [CrossRef] [PubMed]
- Qian, M.; Hu, H.; Zuo, T.; Wang, G.; Zhang, L.; Zhou, P. Unraveling of a neutralization mechanism by two human antibodies against conserved epitopes in the globular head of H5 hemagglutinin. J. Virol. 2013, 87, 3571–3577. [Google Scholar] [CrossRef] [PubMed]
- Rohaim, M.A.; El-Naggar, R.F.; Hamoud, M.M.; Nasr, S.A.; Ismael, E.; Laban, S.E.; Ahmed, H.A.; Munir, M. Re-emergence of a novel H5N1 avian influenza virus variant subclade 2.2.1.1 in Egypt during 2014. Transbound. Emerg. Dis. 2016. [Google Scholar] [CrossRef] [PubMed]
- Amen, O.; Vemula, S.V.; Zhao, J.; Ibrahim, R.; Hussein, A.; Hewlett, I.K.; Moussa, S.; Mittal, S.K. Identification and characterization of a highly pathogenic H5N1 avian influenza A virus during an outbreak in vaccinated chickens in Egypt. Virus Res. 2015, 210, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Ismael, E.; Hamod, M.M.; Gamal, A.M.; Badawy, M.F.; Zaki, M.M.; Nasr, S.A.E.; Samaha, H.A.; Elagrab, H.M.; Moubarak, S.T.; Zahran, O.K. Epidemiological study on the impact of vaccination programs on antigenic relatedness, genetic characterization of highly pathogenic avian influenza H5N1. Aust. J. Vic. Stud. 2014, 4, 64–73. [Google Scholar] [CrossRef]
- NCBI. Available online: http://www.ncbi.nlm.nih.gov/ (accessed on 30 November 2014).
- GISAID. Available online: http://platform.gisaid.org/ (accessed on 16 November 2015).
- Rauw, F.; Palya, V.; Gardin, Y.; Tatar-Kis, T.; Dorsey, K.M.; Lambrecht, B.; van den Berg, T. Efficacy of rHVT-AI vector vaccine in broilers with passive immunity against challenge with two antigenically divergent Egyptian clade 2.2.1 HPAI H5N1 strains. Avian Dis. 2012, 56 (Suppl. S4), 913–922. [Google Scholar] [CrossRef] [PubMed]
- European Patent, EP 2419132 B1. Available online: http://www.google.com/patents/EP2419132B1?cl=un (accessed on 14 December 2015).
- Claas, E.C.; Osterhaus, A.D.; van Beek, R.; de Jong, J.C.; Rimmelzwaan, G.F.; Senne, D.A.; Krauss, S.; Shortridge, K.F.; Webster, R.G. Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet 1998, 351, 472–477. [Google Scholar] [CrossRef]
- Ha, Y.; Stevens, D.J.; Skehel, J.J.; Wiley, D.C. X-ray structure of H5 avian and H9 swine influenza virus hemagglutinins bound to avian and human receptor analogs. Proc. Natl. Acad. Sci. USA 2001, 98, 11181–11186. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.D.; Higgins, D.G.; Gibson, T.J. CLUSTAL W: Improving the sensitivity of progressive multiple sequence alignment through sequence weighing position-specific gap penalties and weight matrix choice. Nucleic Acids Res. 1994, 22, 4673–4680. [Google Scholar] [CrossRef] [PubMed]
- Altschul, S.F.; Madden, T.L.; Schaffer, A.A.; Zhang, J.; Zhang, Z.; Miller, W.; Lipman, D.J. Gapped BLAST and PSI-PLAST: A new generation of protein database search program. Nucleic Acids Res. 1997, 25, 3389–3402. [Google Scholar] [CrossRef] [PubMed]
- Arafa, A.S.; Naguib, M.M.; Luttermann, C.; Selim, A.A.; Kilany, W.H.; Hagag, N.; Samy, A.; Abdelhalim, A.; Hassan, M.K.; Abdelwhab, E.M.; et al. Emergence of a novel cluster of influenza A (H5N1) virus clade 2.2.1.2 with putative human health impact in Egypt, 2014/15. Euro Surveill. 2015, 20, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.J.; Donis, R.O. Nomenclature updates resulting from the evolution of avian influenza A (H5) virus clades 2.1.3.2a, 2.2.1, and 2.3.4 during 2013–2014. Influenza Other Respir. Viruses 2015, 9, 271–276. [Google Scholar] [CrossRef] [PubMed]

| Anchor Site | Amino Acid Positions | Grid Address 1 | Reported Significance of the Region |
|---|---|---|---|
| AS-I | N220, G221, Q222 | 4A, 4B | Associated with replication, transmission, and receptor binding [49] |
| AS-II | V131 | 5B, 5C, 6C | Involved in receptor binding [50] |
| AS-III | G139 | A6, 7A | Neutralizing epitope [51] |
| AS-IV | Y271 | 9B, 9C | Adjacent to amino acid 272 which affects receptor binding affinity [52] |
| AS-V | N72 | 9D | Glycosylation site [47] |
| AS-VI | Q115, P118 | 7E, 7F, 7G, 8E, 8F | Conserved epitope involved in neutralization [53] |
| AS-VII | T167 | 8H | Part of a conserved epitope involved in neutralization [53], and glycosylation [47] |
| AS-VIII | K161 | 4H | Part of a conserved epitope involved in neutralization [53] |
| CSU | Cell Addresses/Grid Area |
|---|---|
| CSU-1 | 1B, 1C, 2B, 2C |
| CSU-2 | 2D, 2E, 3D, 3E front |
| CSU-3 | 2F, 3F, 4F |
| CSU-4 | 3B |
| CSU-5 | 8B |
| CSU-6 | 8D, 8E, 9D, 9E |
| CSU-7 | 4G, 4H, 5G, 5H |
| CSU-8 | 6F, 7F over anchor site (AS)-VI |
| CSU-9 | 6A, 6B, 7A, 7B |
| Case | A | B | C |
|---|---|---|---|
| Virus Name | A/chicken/Egypt/2010 (H5N1) | A/chicken/Egypt/13VIR3729-4/2013 (H5N1) | A/chicken/Egypt/Fadllah-7/2014 (H5N1) |
| Virus designation | Egypt/2010 | Egypt/2013 | Egypt/2014 |
| HA gene GenBank accession number | KP869097 | KF715072 | KP326324 |
| Isolation source | Layers | Broilers | Layers |
| Isolation date | Feb-2010 | Apr-2013 | Nov-2014 |
| AIV vaccine used | Inactivated H5N2 1 vaccine | Inactivated H5N2 vaccine | rHVT/AI-H5 2 |
| HI GMT before or at AI infection | 9.7 Log2 | High to homologous vaccine | 6.4 Log2 |
| Reference | [55] | [56] | [54] |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Metwally, A.; Yousif, A. Visualization of Alternative Functional Configurations of Influenza Virus Hemagglutinin Facilitates Rapid Selection of Complementing Vaccines in Emergency Situations. Int. J. Mol. Sci. 2017, 18, 766. https://doi.org/10.3390/ijms18040766
Metwally A, Yousif A. Visualization of Alternative Functional Configurations of Influenza Virus Hemagglutinin Facilitates Rapid Selection of Complementing Vaccines in Emergency Situations. International Journal of Molecular Sciences. 2017; 18(4):766. https://doi.org/10.3390/ijms18040766
Chicago/Turabian StyleMetwally, Ashraf, and Ausama Yousif. 2017. "Visualization of Alternative Functional Configurations of Influenza Virus Hemagglutinin Facilitates Rapid Selection of Complementing Vaccines in Emergency Situations" International Journal of Molecular Sciences 18, no. 4: 766. https://doi.org/10.3390/ijms18040766






