Clinical Outcomes and Co-Occurring Mutations in Patients with RUNX1-Mutated Acute Myeloid Leukemia
Abstract
:1. Introduction
2. Results
2.1. Frequency and Characteristics of RUNX1 Mutations
2.2. Association of RUNX1 with Clinical Characteristics
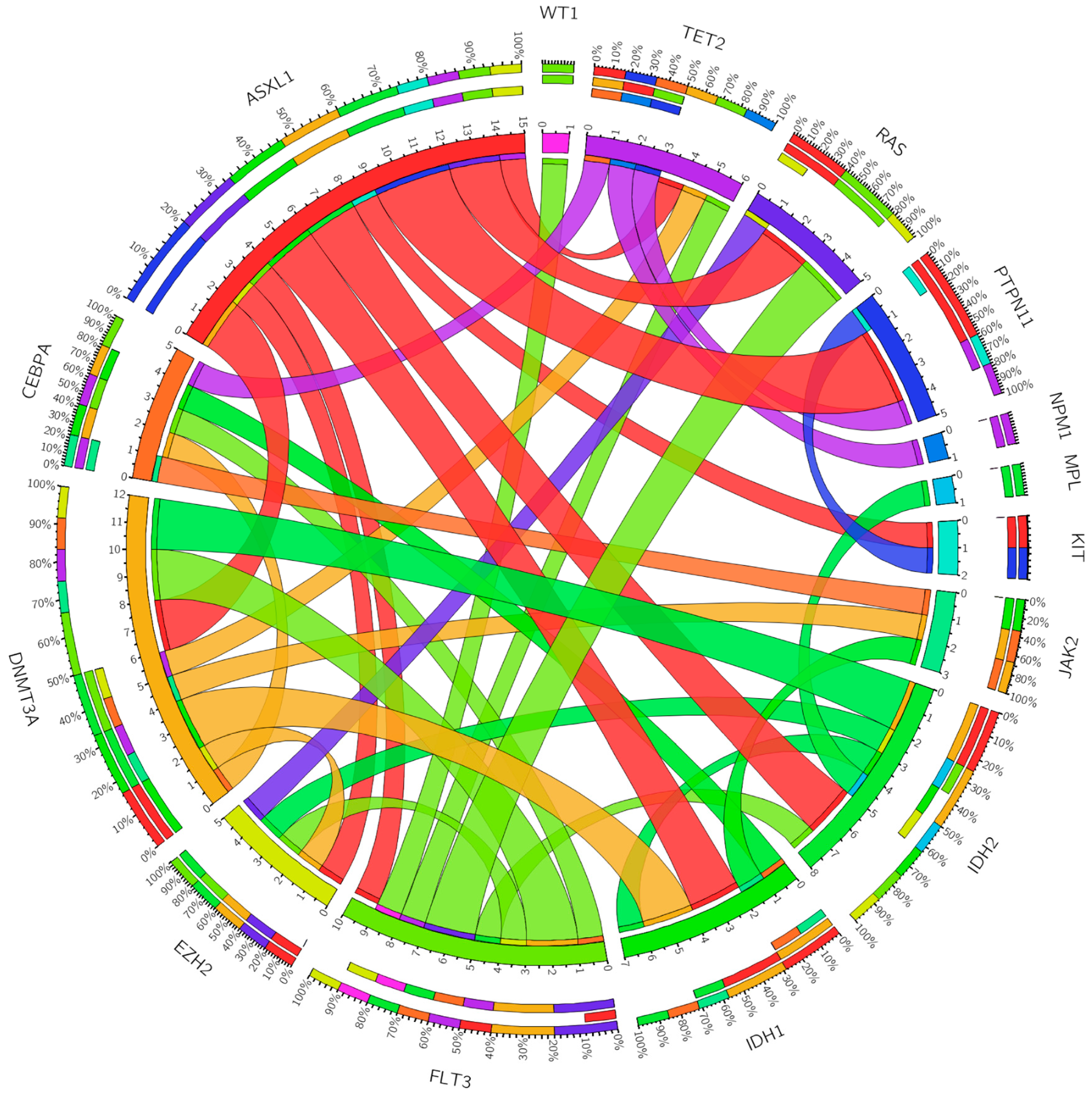
2.3. Association of RUNX1 with Co-Occurring Mutations
2.4. Association of RUNX1 with Response to Frontline AML Therapy
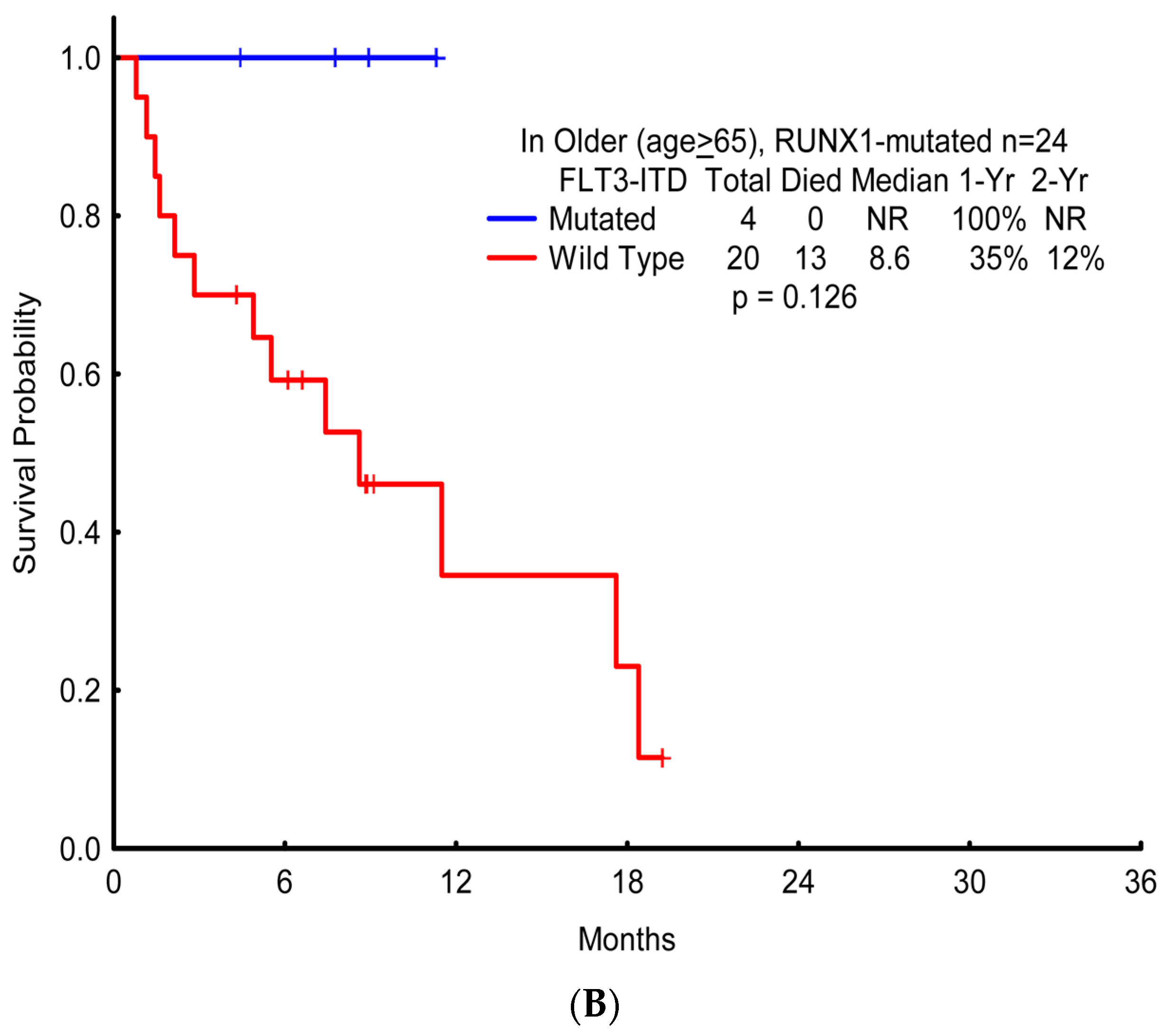
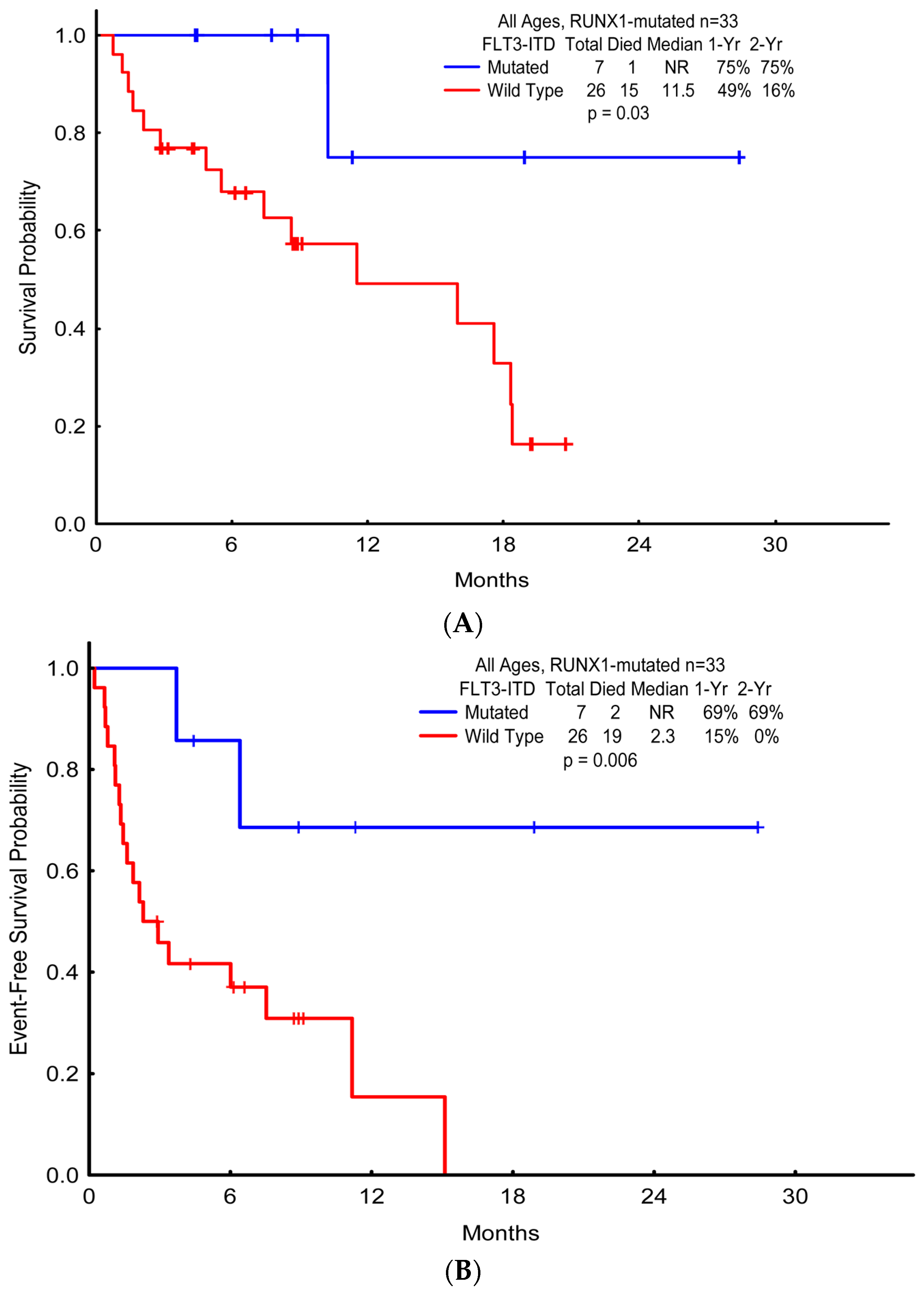
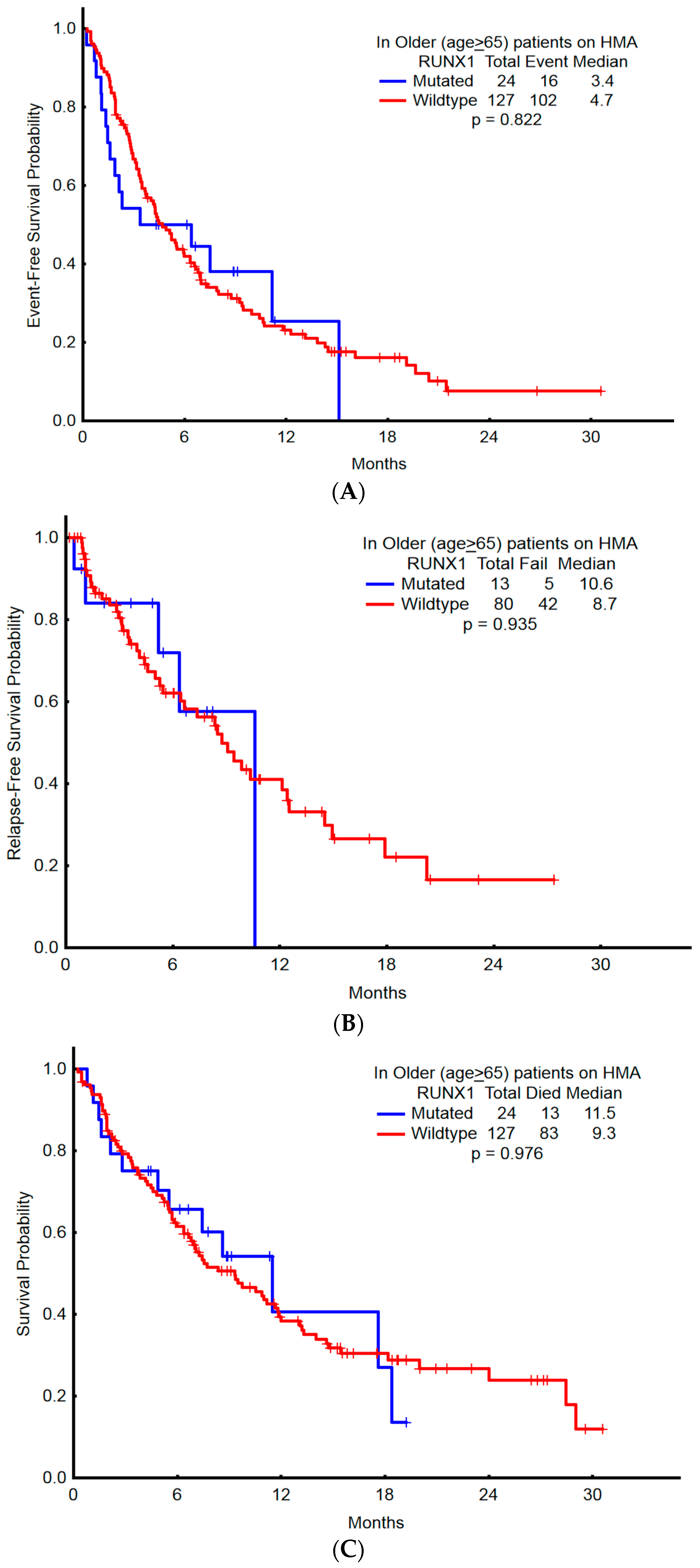
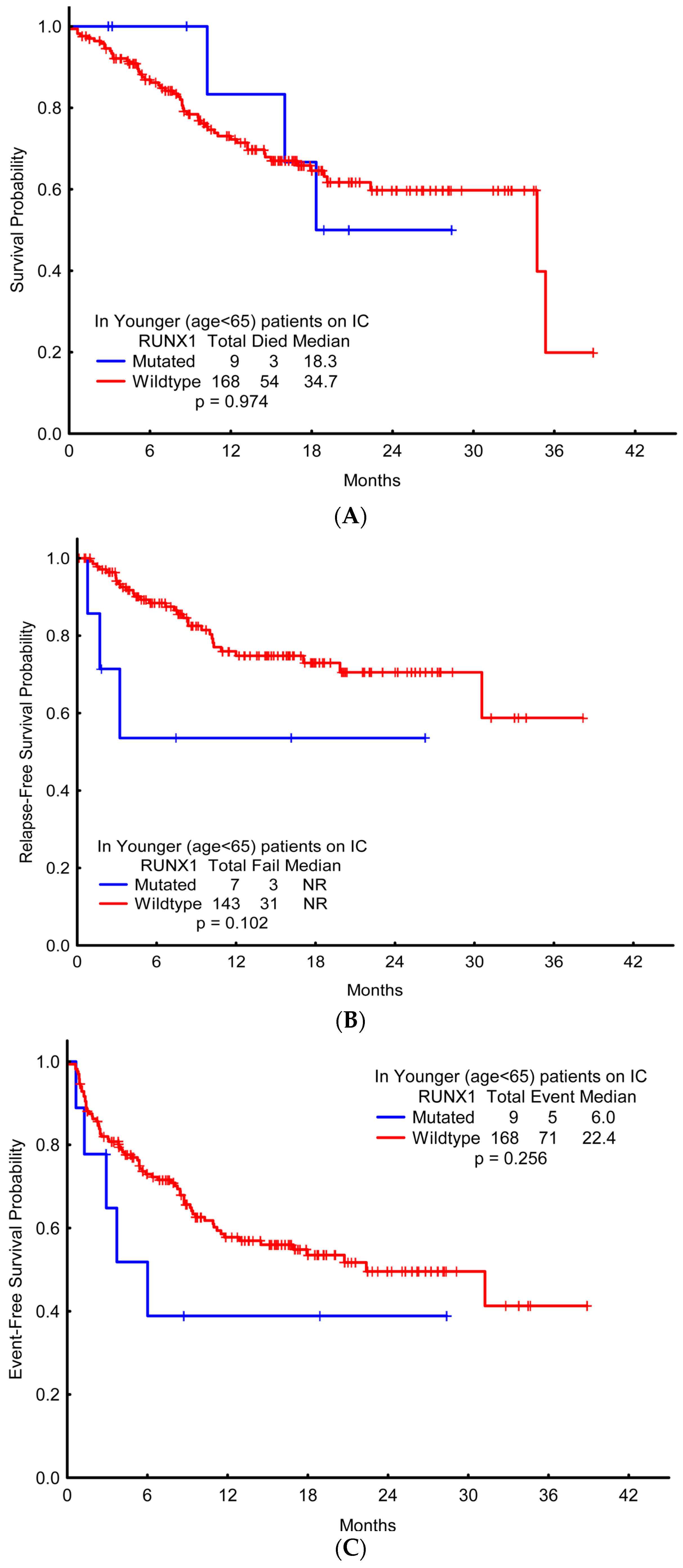
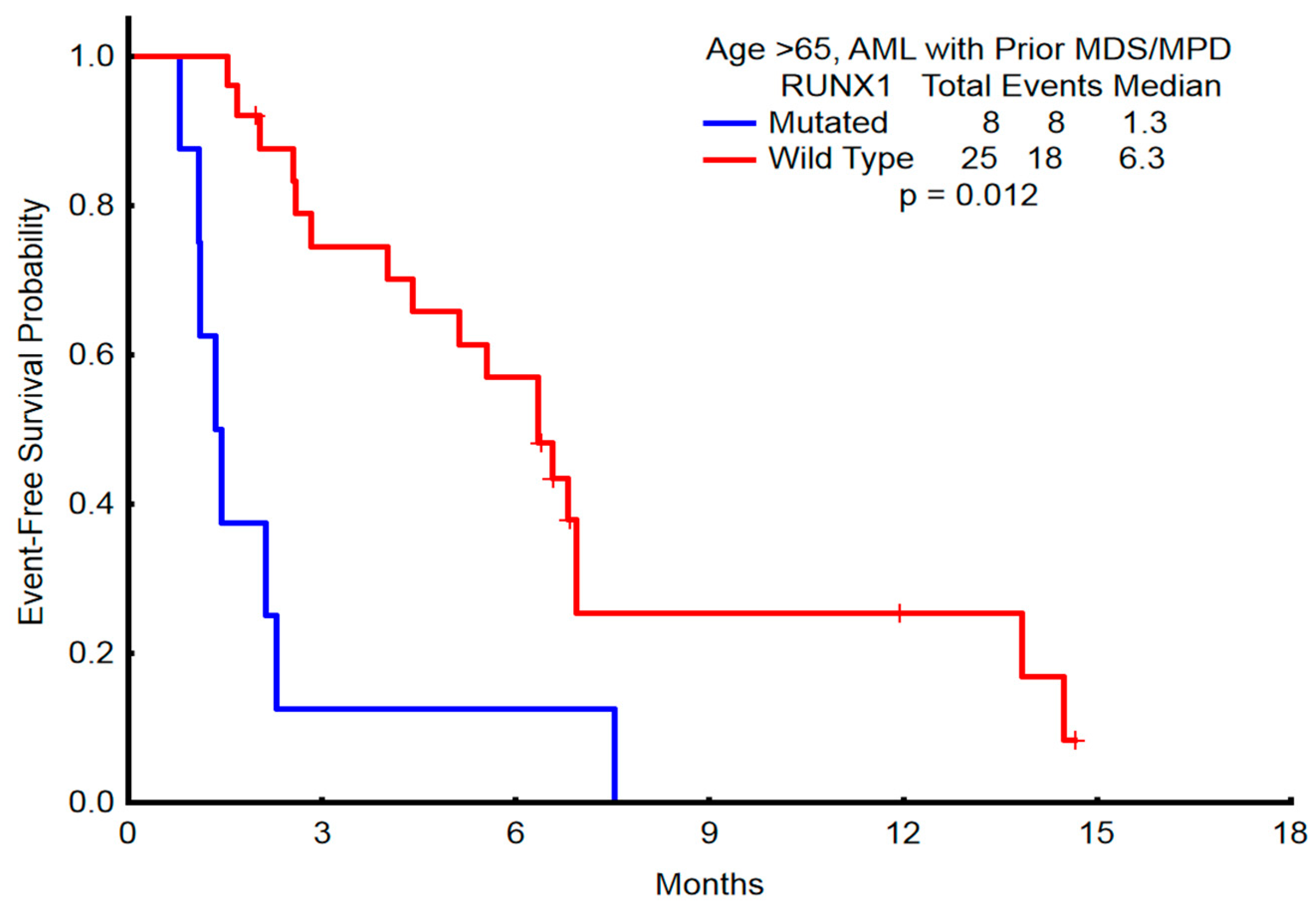
2.5. Association of RUNX1 with Clinical Outcomes
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. Molecular Analysis
4.3. Statistical Analysis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Mutation HGVS (MAF%) | Exon | Type |
|---|---|---|
| NM_001754.4 ( RUNX1):c.497G>A p.R166Q [46.4] | 5 | Missense |
| NM_001754.4 ( RUNX1):c.423_424insAAAGGGATTCT p.A142fs [5.9] | 5 | Frameshift |
| NM_001754.4 ( RUNX1):c.891_894dupCCCA p.A299fs [8.7] | 8 | Frameshift |
| NM_001754.4 ( RUNX1):c.238dupG p.E80fs [50.3] | 4 | Frameshift |
| NM_001754.4 ( RUNX1):c.900_901insTCCG p.P301fs [17.0], NM_001754.4 (RUNX1):c.987_988dupGT p.F330fs [32.3], NM_001754.4(RUNX1):c.1281_1285del p.I428fs [13.6] | “8,9” | Frameshift |
| NM_001754.4 ( RUNX1):c.292delG p.L98fs,NM_001754.4(RUNX1):c.492_493insAT p.G165fs [36.2] | “4,5” | Frameshift |
| NM_001754.4 ( RUNX1):c.368A>C p.D123A [9.2], NM_001754.4(RUNX1):c.367G>C p.D123H [9.3], NM_001754.4 (RUNX1):c.361_364del p.L121fs [10.1] | 5 | Frameshift |
| NM_001754.4( RUNX1):c.422_423insA p.A142fs [26.2] | 5 | Frameshift |
| NM_001754.4 ( RUNX1):c.418_422dupTACTC p.A142fs [21.0] | 5 | Frameshift |
| NM_001754.4 (
RUNX1):c.422dupC p.A142fs [9.5], NM_001754.4(RUNX1):c.424_425insGGTGG p.A142fs [4.4] | 5 | Frameshift |
| NM_001754.4 ( RUNX1):c.939_942dupCTCT p.A315fs [43.5] | 8 | Frameshift |
| NM_001754.4 ( RUNX1):c.593A>G p.D198G [83.0] | 6 | Missense |
| NM_001754.4 ( RUNX1):c.592G>A p.D198N [31.7] | 6 | Missense |
| NM_001754.4 ( RUNX1):c.993_1005del p.D332fs | 9 | Frameshift |
| NM_001754.4 ( RUNX1):c.402dupT p.G135fs [41.1] | 5 | Frameshift |
| NM_001754.4 ( RUNX1):c.1023_1024insC p.I342fs | 9 | Frameshift |
| NM_001754.4 ( RUNX1):c.1251_1252insC p.M418fs | 9 | Frameshift |
| NM_001754.4 ( RUNX1):c.1244_1250dupAGTTCTC p.M418fs [19.5] | 9 | Frameshift |
| NM_001754.4 ( RUNX1):c.548dupC p.P184fs [45.3] | 6 | Frameshift |
| NM_001754.4 ( RUNX1):c.256_259delinsACCCGA p.P86fs | 4 | Missense |
| NM_001754.4 ( RUNX1):c.484A>G p.R162G [70.4] | 5 | Missense |
| NM_001754.4 ( RUNX1):c.485G>A p.R162K [42.2],NM_001754.4(RUNX1):c.388G>T p.V130F [44.7] | 5 | Missense |
| NM_001754.4 ( RUNX1):c.496C>T p.R166* [39.1] | 5 | Nonsense |
| NM_001754.4 ( RUNX1):c.601C>T p.R201* [40.7] | 6 | Nonsense |
| NM_001754.4 ( RUNX1):c.955_958dupAGTC p.R320fs [49.7] | 8 | Frameshift |
| NM_001754.4 ( RUNX1):c.952del p.S318fs [29.7] | 8 | Frameshift |
| NM_001754.4 (
RUNX1):c.1352_1356dupACGTG p.V453fs [22.9], NM_001754.4 (RUNX1):c.611G>A p.R204Q [49.7] | “9,6” | Frameshift |
| NM_001754.4 ( RUNX1):c.952T>G p.S318A [14.9], NM_001754.4 (RUNX1):c.954dupC p.S319fs [14.4], NM_001754.4(RUNX1) :c.950T>G p.L317R [15.0] | 8 | Frameshift |
| NM_001754.4 ( RUNX1):c.977del p.D326fs [17.1], NM_001754.4 (RUNX1):c.352-1_352insTTTAG p.? | 9 | Frameshift, splice |
| NM_001754.4 ( RUNX1):c.492_507dupCGGTCGAAGTGGAAGA p.G170fs [30.7], NM_001754.4 (RUNX1):c.484dupA p.R162fs [3.0] | 5 | Frameshift |
| NM_001754.4 ( RUNX1):c.486dupG p.F163fs [51.2] | 5 | Frameshift |
| NM_001754.4 ( RUNX1):c.1036dupC p.R346fs [2.8] | 9 | Frameshift |
| NM_001754.4 ( RUNX1):c.167T>C p.L56S [51.5] | 4 | Missense |

References
- Gilliland, D.G.; Griffin, J.D. The roles of FLT3 in hematopoiesis and leukemia. Blood 2002, 100, 1532–1542. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, S. Current findings for recurring mutations in acute myeloid leukemia. J. Hematol. Oncol. 2011, 4, 36. [Google Scholar] [CrossRef] [PubMed]
- Greif, P.A.; Konstandin, N.P.; Metzeler, K.H.; Herold, T.; Pasalic, Z.; Ksienzyk, B.; Dufour, A.; Schneider, F.; Schneider, S.; Kakadia, P.M.; et al. RUNX1 mutations in cytogenetically normal acute myeloid leukemia are associated with a poor prognosis and up-regulation of lymphoid genes. Haematologica 2012, 97, 1909–1915. [Google Scholar] [CrossRef] [PubMed]
- Gaidzik, V.I.; Teleanu, V.; Papaemmanuil, E.; Weber, D.; Paschka, P.; Hahn, J.; Wallrabenstein, T.; Kolbinger, B.; Köhne, C.H.; Horst, H.A.; et al. RUNX1 mutations in acute myeloid leukemia are associated with distinct clinico-pathologic and genetic features. Leukemia 2016, 30, 2282. [Google Scholar] [CrossRef] [PubMed]
- Harada, H.; Harada, Y.; Niimi, H.; Kyo, T.; Kimura, A.; Inaba, T. High incidence of somatic mutations in the AML1/RUNX1 gene in myelodysplastic syndrome and low blast percentage myeloid leukemia with myelodysplasia. Blood 2004, 103, 2316–2324. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Lin, L.I.; Tang, J.L.; Ko, B.S.; Tsay, W.; Chou, W.C.; Yao, M.; Wu, S.J.; Tseng, M.H.; Tien, H.F.; et al. RUNX1 gene mutation in primary myelodysplastic syndrome—The mutation can be detected early at diagnosis or acquired during disease progression and is associated with poor outcome. Br. J. Haematol. 2007, 139, 405–414. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.L.; Hou, H.A.; Chen, C.Y.; Liu, C.Y.; Chou, W.C.; Tseng, M.H.; Huang, C.F.; Lee, F.Y.; Liu, M.C.; Yao, M.; et al. AML1/RUNX1 mutations in 470 adult patients with de novo acute myeloid leukemia: Prognostic implication and interaction with other gene alterations. Blood 2009, 114, 5352–5361. [Google Scholar] [CrossRef] [PubMed]
- Chou, W.C.; Huang, H.H.; Hou, H.A.; Chen, C.Y.; Tang, J.L.; Yao, M.; Tsay, W.; Ko, B.S.; Wu, S.J.; Huang, S.Y.; et al. Distinct clinical and biological features of de novo acute myeloid leukemia with additional sex comb-like 1 (ASXL1) mutations. Blood 2010, 116, 4086–4094. [Google Scholar] [CrossRef] [PubMed]
- Schnittger, S.; Eder, C.; Alpermann, T.; Fasan, A.; Grossmann, V.; Kohlmann, A.; Kern, W.; Haferlach, C.; Haferlach, T. ASXL1 exon 12 mutations are frequent in AML with intermediate risk karyotype and are independently associated with an adverse outcome. Leukemia 2013, 27, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Gaidzik, V.I.; Bullinger, L.; Schlenk, R.F.; Zimmermann, A.S.; Rock, J.; Paschka, P.; Corbacioglu, A.; Krauter, J.; Schlegelberger, B.; Ganser, A.; et al. RUNX1 mutations in acute myeloid leukemia: Results from a comprehensive genetic and clinical analysis from the AML study group. J. Clin. Oncol. 2011, 29, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Osato, M. Point mutations in the RUNX1/AML1 gene: Another actor in RUNX leukemia. Oncogene 2004, 23, 4284–4296. [Google Scholar] [CrossRef] [PubMed]
- Mendler, J.H.; Maharry, K.; Radmacher, M.D.; Mrozek, K.; Becker, H.; Metzeler, K.H.; Schwind, S.; Whitman, S.P.; Khalife, J.; Kohlschmidt, J.; et al. RUNX1 mutations are associated with poor outcome in younger and older patients with cytogenetically normal acute myeloid leukemia and with distinct gene and MicroRNA expression signatures. J. Clin. Oncol. 2012, 30, 3109–3118. [Google Scholar] [CrossRef] [PubMed]
- Hann, I.M.; Stevens, R.F.; Goldstone, A.H.; Rees, J.K.; Wheatley, K.; Gray, R.G.; Burnett, A.K. Randomized comparison of DAT versus ADE as induction chemotherapy in children and younger adults with acute myeloid leukemia. Results of the Medical Research Council’s 10th AML trial (MRC AML10). Adult and Childhood Leukaemia Working Parties of the Medical Research Council. Blood 1997, 89, 2311–2318. [Google Scholar] [PubMed]
- Al-Ali, H.K.; Jaekel, N.; Niederwieser, D. The role of hypomethylating agents in the treatment of elderly patients with AML. J. Geriatr. Oncol. 2014, 5, 89–105. [Google Scholar] [CrossRef] [PubMed]
- Krzywinski, M.; Schein, J.; Birol, I.; Connors, J.; Gascoyne, R.; Horsman, D.; Jones, S.J.; Marra, M.A. Circos: An information aesthetic for comparative genomics. Genome Res. 2009, 19, 1639–1645. [Google Scholar] [CrossRef] [PubMed]
- Schneider, F.; Hoster, E.; Schneider, S.; Dufour, A.; Benthaus, T.; Kakadia, P.M.; Bohlander, S.K.; Braess, J.; Heinecke, A.; Sauerland, M.C.; et al. Age-dependent frequencies of NPM1 mutations and FLT3-ITD in patients with normal karyotype AML (NK-AML). Ann Hematol. 2012, 91, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Zhang, W.; Chen, Y.; Guo, W.; Zhang, J.; Tang, H.; Xu, Z.; Zhang, H.; Tao, Y.; Wang, F.; et al. Impaired DNA double-strand break repair contributes to the age-associated rise of genomic instability in humans. Cell Death Differ. 2016, 23, 1765–1777. [Google Scholar] [CrossRef] [PubMed]
- Papamichos-Chronakis, M.; Peterson, C.L. Chromatin and the genome integrity network. Nat. Rev. Genet. 2013, 14, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Harada, H.; Harada, Y.; Tanaka, H.; Kimura, A.; Inaba, T. Implications of somatic mutations in the AML1 gene in radiation-associated and therapy-related myelodysplastic syndrome/acute myeloid leukemia. Blood 2003, 101, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Zharlyganova, D.; Harada, H.; Harada, Y.; Shinkarev, S.; Zhumadilov, Z.; Zhunusova, A.; Tchaizhunusova, N.J.; Apsalikov, K.N.; Kemaikin, V.; Zhumadilov, K.; et al. High frequency of AML1/RUNX1 point mutations in radiation-associated myelodysplastic syndrome around Semipalatinsk nuclear test site. J. Radiat. Res. 2008, 49, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Genovese, G.; Kähler, A.K.; Handsaker, R.E.; Lindberg, J.; Rose, S.A.; Bakhoum, S.F.; Chambert, K.; Mick, E.; Neale, B.M.; Fromer, M.; et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. NEJM 2014, 371, 2477–2487. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Lu, C.; Wang, J.; McLellan, M.D.; Johnson, K.J.; Wendl, M.C.; McMichael, J.F.; Schmidt, H.K.; Yellapantula, V.; Miller, C.A.; et al. Age-related mutations associated with clonal hematopoietic expansion and malignancies. Nat. Med. 2014, 20, 1472–1478. [Google Scholar] [CrossRef] [PubMed]
- Klein, K.; Kaspers, G.; Harrison, C.J.; Beverloo, H.B.; Reedijk, A.; Bongers, M.; Cloos, J.; Pession, A.; Reinhardt, D.; Zimmerman, M.; et al. Clinical Impact of Additional Cytogenetic Aberrations, cKIT and RAS Mutations, and Treatment Elements in Pediatric t(8;21)-AML: Results From an International Retrospective Study by the International Berlin-Frankfurt-Münster Study Group. J. Clin. Oncol. 2015, 33, 4247–4258. [Google Scholar] [CrossRef] [PubMed]
- Matsuno, N.; Osato, M.; Nanri, T.; Shigesada, K.; Fukushima, T.; Motoji, T.; Kusumoto, S.; Naoe, T.; Ohno, R.; Mitsuya, H.; et al. Dual mutations in the AML1 and FLT3 genes are associated with leukemogenesis in acute myeloblastic leukemia of the M0 type. Leukemia 2003, 17, 2492–2499. [Google Scholar] [CrossRef] [PubMed]
- Schnittger, S.; Dicker, F.; Kern, W.; Wendland, N.; Sundermann, J.; Alpermann, T.; Haferlach, C.; Haferlach, T. RUNX1 mutations are frequent in de novo AML with noncomplex karyotype and confer an unfavorable prognosis. Blood 2011, 117, 2348–2357. [Google Scholar] [CrossRef] [PubMed]
- Kao, H.W.; Liang, D.C.; Wu, J.H.; Kuo, M.C.; Wang, P.N.; Yang, C.P.; Shih, Y.S.; Lin, T.H.; Huang, Y.H.; Shih, L.Y.; et al. Gene mutation patterns in patients with minimally differentiated acute myeloid leukemia. Neoplasia 2014, 16, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Green, C.L.; Evans, C.M.; Zhao, L.; Hills, R.K.; Burnett, A.K.; Linch, D.C.; Gale, R.E. The prognostic significance of IDH2 mutations in AML depends on the location of the mutation. Blood 2011, 118, 409–412. [Google Scholar] [CrossRef] [PubMed]
- Bejar, R.; Lord, A.; Stevenson, K.; Bar-Natan, M.; Pérez-Ladaga, A.; Zaneveld, J.; Wang, H.; Caughey, B.; Stojanov, P.; Getz, G.; et al. TET2 mutations predict response to hypomethylating agents in myelodysplastic syndrome patients. Blood 2014, 124, 2705–2712. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, E.L.; Meier, P. Nonparametric estimation from incomplete observations. J. Am. Stat. Assoc. 1958, 53, 457–481. [Google Scholar] [CrossRef]
- Cheson, B.D.; Bennett, J.M.; Kopecky, K.J.; Büchner, T.; Willman, C.L.; Estey, E.H.; Schiffer, C.A.; Doehner, H.; Tallman, M.S.; Lister, T.A.; et al. Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J. Clin. Oncol. 2003, 21, 4642–4649. [Google Scholar] [CrossRef] [PubMed]
- Casaril, A.E.; de Oliveira, L.P.; Alonso, D.P.; de Oliveira, E.F.; Barrios, S.P.G.; Infran, J.D.O.M.; de Souza Fernandes, W.; Oshiro, E.T.; Ferreira, A.M.T.; Ribolla, P.E.M.; et al. Standardization of DNA extraction from sand flies: Application to genotyping by next generation sequencing. Exp. Parasitol. 2017, 177, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Warren, M.; Luthra, R.; Yin, C.C.; Ravandi, F.; Cortes, J.E.; Kantarjian, H.M.; Medeiros, L.J.; Zuo, Z. Clinical impact of change of FLT3 mutation status in acute myeloid leukemia patients. Mod. Pathol. 2012, 25, 1405–1412. [Google Scholar] [CrossRef] [PubMed]
- Wendt, F.R.; Zeng, X.; Churchill, J.D.; King, J.L.; Budowle, B. Analysis of Short Tandem Repeat and Single Nucleotide Polymorphism Loci From Single-Source Samples Using a Custom HaloPlex Target Enrichment System Panel. Am. J. Forensic Med. Pathol. 2016, 37, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.P.; Newberry, K.J.; Luthra, R.; Jabbour, E.; Pierce, S.; Cortes, J.; Singh, R.; Mehrotra, M.; Routbort, M.J.; Luthra, M.; et al. Correlation of mutation profile and response in patients with myelofibrosis treated with ruxolitinib. Blood 2015, 126, 790–797. [Google Scholar] [CrossRef] [PubMed]
| Clinical Characteristics | Younger Cohort (Chemotherapy) | p-Value | Elderly Cohort (HMA) | p-Value | ||
|---|---|---|---|---|---|---|
| Median (Range) | Median (Range) | |||||
| RUNX1mut | RUNX1WT | RUNX1mut | RUNX1WT | |||
| (n = 9) | (n = 168) | (n = 24) | (n = 127) | |||
| Age, year | 56 (31–63) | 51 (17–64) | 0.14 | 77 (65–92) | 73 (65–91) | 0.01 * |
| WBC, ×109/L | 4.95 (1.3–17.2) | 6.9 (0.5–378.4) | 0.43 | 3.2 (0.6–36.5) | 3.2 (0.3–164.5) | 0.98 |
| Platelet count, ×109/L | 57.5 (28–213) | 30 (1–584) | 0.05 | 61 (7–416) | 42 (3–324) | 0.20 |
| Hemoglobin, g/dL | 8.95 (7.4–12.1) | 9.3 (5.1–13.0) | 0.38 | 9.4 (5.8–13.1) | 9.4 (7.5–13.2) | 0.37 |
| Peripheral blood blasts, % | 28 (1–86) | 25.5 (0–97) | 0.61 | 7 (0–90) | 11 (0–95) | 0.51 |
| Neutrophils, % | 14.5 (0–45) | 12 (0–98) | 0.93 | 21 (0–81) | 21 (0–73.3) | 0.95 |
| Bone marrow blasts, % | 51 (28–93) | 54 (2–96) | 0.66 | 50 (12–84) | 44 (1–90) | 0.80 |
| Cytogenetic | 0.94 | 0.02 | ||||
| Complex | 2 | 37 | 2 | 47 | ||
| Diploid | 3 | 65 | 14 | 50 | ||
| ^ Intermediate | 4 | 66 | 8 | 30 | ||
| LDH, U/L | 668.5 | 888 | 0.10 | 532 | 650 | 0.44 |
| (526–1649) | (310–12,489) | (276–2314) | (210–3921) | |||
| t-AML | 0 | 10 | 0.45 | 4 | 18 | 0.75 |
| Prior MDS/MPD | 1 | 6 | 0.26 | 8 | 25 | 0.14 |
| Response | Younger Cohort (Chemotherapy) | Elderly Cohort (HMA) | ||||
|---|---|---|---|---|---|---|
| n (%) | n (%) | |||||
| RUNX1WT | RUNX1mut | p-Value | RUNX1WT | RUNX1mut | p-Value | |
| (n = 168) | (n = 9) | (n = 127) | (n = 24) | |||
| Complete remission | 128 (76.2) | 3 (33.3) | 0.004 * | 48 (37.8) | 9 (37.5) | 0.976 |
| Complete remission with incomplete platelet recovery | 9 (5.4) | 3 (33.3) | 0.271 | 11 (8.7) | 1 (4.2) | 0.667 |
| Hematological improvement | 4 (2.4) | 1 (11.1) | 0.631 | 17 (13.4) | 3 (12.5) | 0.603 |
| Partial remission | 2 (1.2) | 0 (0.0) | 4 (3.1) | 0 (0.0) | ||
| Overall response rate | 143 (85.0) | 7 (78.0) | 0.549 | 80 (63.0) | 13 (54.0) | 0.418 |
| No remission | 19 (11.3) | 2 (22.2) | 22 (17.3) | 7 (29.2) | ||
| Death | 5 (3.0) | 0 (0.0) | 22 (17.3) | 3 (12.5) | ||
| Early death ** | 1 (0.6) | 0 (0.0) | 0.818 | 3 (2.4) | 1 (4.2) | 0.617 |
| Response | Younger Cohort (Chemotherapy) | Elderly Cohort (HMA) | ||||
|---|---|---|---|---|---|---|
| n (%) | n (%) | |||||
| RUNX1WT | RUNX1mut | p-Value | RUNX1WT | RUNX1mut | p-Value | |
| (n = 6) | (n = 1) | (n = 25) | (n = 8) | |||
| Complete remission | 2 (33.3) | 1 (100.0) | 0.211 | 11 (44.0) | 1 (12.5) | 0.107 |
| Complete remission with incomplete platelet recovery | 1 (16.7) | 0 (0.0) | 4 (16.0) | 0 (0.0) | ||
| Hematological improvement | 0 (0.0) | 0 (0.0) | 4 (16.0) | 1 (12.5) | ||
| Partial remission | 1 (16.7) | 0 (0.0) | 1 (4.0) | 0 (0.0) | ||
| Overall response rate | 4 (66.7) | 1 (100.0) | 0.497 | 20 (80.0) | 2 (25.0) | 0.004 * |
| No remission | 1 (16.7) | 0 (0.0) | 1 (4.0) | 3 (37.5) | ||
| Death | 1 (16.7) | 0 (0.0) | 4 (16.0) | 2 (25.0) | ||
| Early death ** | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (12.5) | ||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, M.; Cortes, J.; Kadia, T.; Naqvi, K.; Brandt, M.; Pierce, S.; Patel, K.P.; Borthakur, G.; Ravandi, F.; Konopleva, M.; et al. Clinical Outcomes and Co-Occurring Mutations in Patients with RUNX1-Mutated Acute Myeloid Leukemia. Int. J. Mol. Sci. 2017, 18, 1618. https://doi.org/10.3390/ijms18081618
Khan M, Cortes J, Kadia T, Naqvi K, Brandt M, Pierce S, Patel KP, Borthakur G, Ravandi F, Konopleva M, et al. Clinical Outcomes and Co-Occurring Mutations in Patients with RUNX1-Mutated Acute Myeloid Leukemia. International Journal of Molecular Sciences. 2017; 18(8):1618. https://doi.org/10.3390/ijms18081618
Chicago/Turabian StyleKhan, Maliha, Jorge Cortes, Tapan Kadia, Kiran Naqvi, Mark Brandt, Sherry Pierce, Keyur P. Patel, Gautam Borthakur, Farhad Ravandi, Marina Konopleva, and et al. 2017. "Clinical Outcomes and Co-Occurring Mutations in Patients with RUNX1-Mutated Acute Myeloid Leukemia" International Journal of Molecular Sciences 18, no. 8: 1618. https://doi.org/10.3390/ijms18081618




