Immunohistochemical Expression of Aquaporin-1 in Fluoro-Edenite-Induced Malignant Mesothelioma: A Preliminary Report
Abstract
:1. Introduction
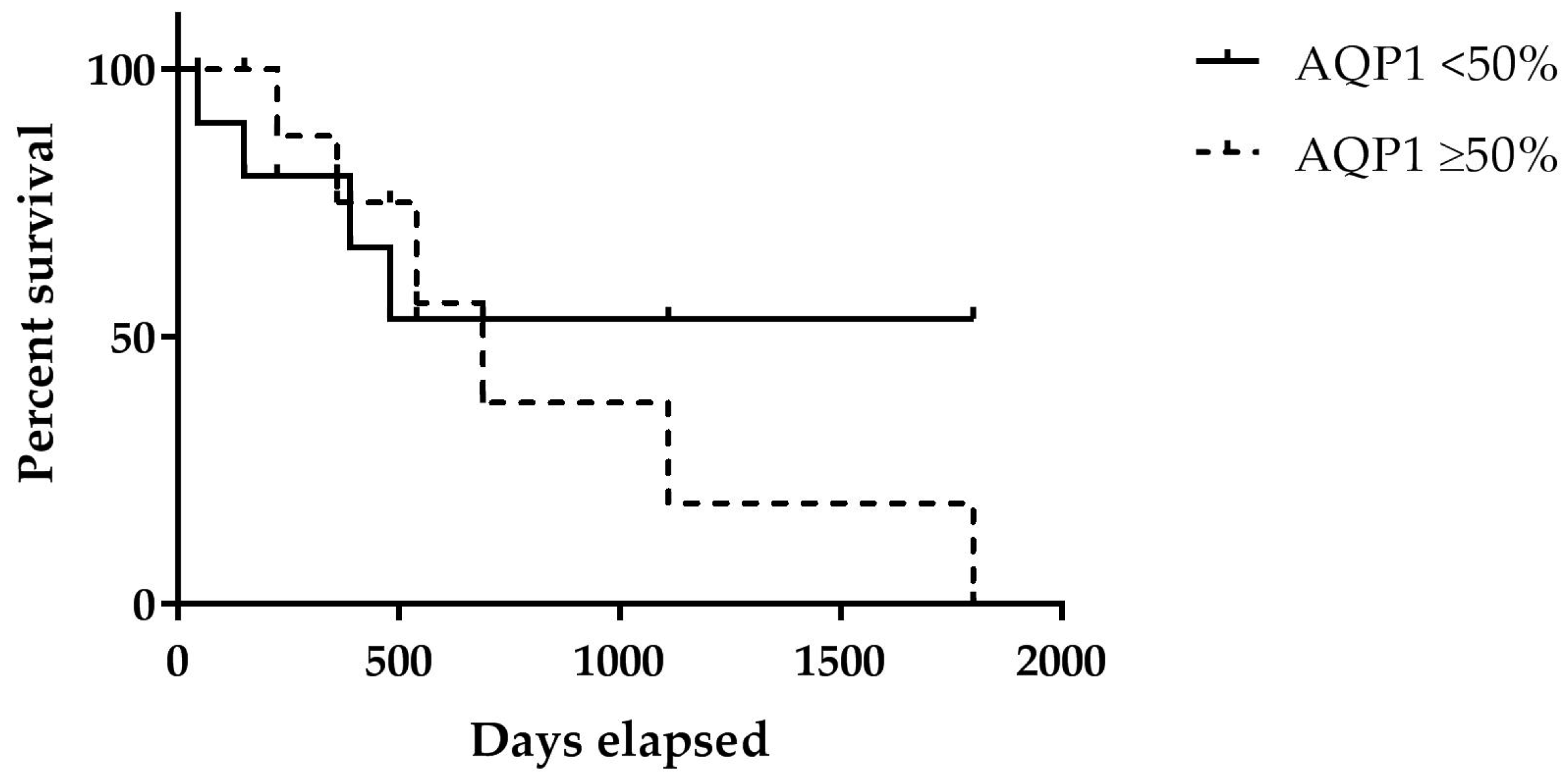
2. Results
3. Discussion
4. Materials and Methods
4.1. Sample Collection
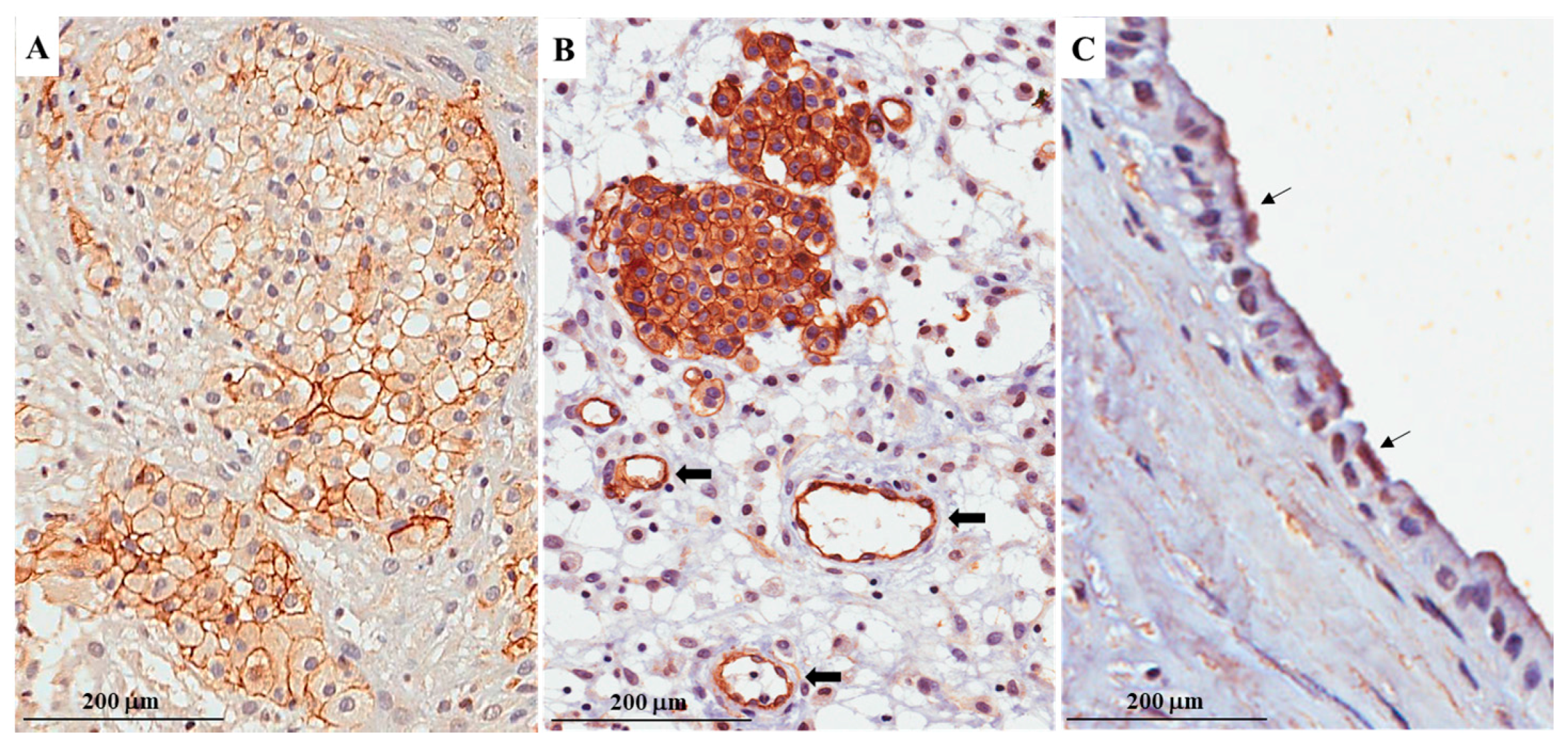
4.2. Laboratory Tests
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Conflicts of Interest
Abbreviations
| AQP1 | Aquaporin-1 |
| CI | Confidence interval |
| FE | Fluoro-edenite |
| MPM | Malignant pleural mesothelioma |
| H&E | Haematoxylin and eosin |
| WT1 | Wilms tumor protein |
| TTF1 | Thyroid transcription factor |
| OS | Overall survival |
References
- Baas, P.; Fennell, D.; Kerr, K.M.; van Schil, P.E.; Haas, R.L.; Peters, S. ESMO Guidelines Committee. Malignant pleural mesothelioma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2015, 26, v31–v39. [Google Scholar] [CrossRef] [PubMed]
- Tomasson, K.; Gudmundsson, G.; Briem, H.; Rafnsson, V. Malignant mesothelioma incidence by nation-wide cancer registry: A population-based study. J. Occup. Med. Toxicol. 2016, 11, 37. [Google Scholar] [CrossRef] [PubMed]
- Arnold, D.T.; Maskell, N.A. Biomarkers in mesothelioma. Ann. Clin. Biochem. 2017, 1, 4563217741145. [Google Scholar] [CrossRef]
- Delgermaa, V.; Takahashi, K.; Park, E.K.; Le, G.V.; Hara, T.; Sorahan, T. Global mesothelioma deaths reported to the World Health Organization between 1994 and 2008. Bull. World Health Organ. 2011, 89, 716–724. [Google Scholar] [CrossRef] [PubMed]
- Kao, S.C.; Armstrong, N.; Condon, B.; Griggs, K.; McCaughan, B.; Maltby, S.; Wilson, A.; Henderson, D.W.; Klebe, S. Aquaporin 1 is an independent prognostic factor in pleural malignant mesothelioma. Cancer 2012, 118, 2952–2961. [Google Scholar] [CrossRef] [PubMed]
- Driml, J.; Pulford, E.; Moffat, D.; Karapetis, C.; Kao, S.; Griggs, K.; Henderson, D.W.; Klebe, S. Usefulness of Aquaporin 1 as a Prognostic Marker in a Prospective Cohort of Malignant Mesotheliomas. Int. J. Mol. Sci. 2016, 17, 1041. [Google Scholar] [CrossRef] [PubMed]
- Day, R.E.; Kitchen, P.; Owen, D.S.; Bland, C.; Marshall, L.; Conner, A.C.; Bill, R.M.; Conner, M.T. Human aquaporins: Regulators of transcellular water flow. Biochim. Biophys. Acta 2014, 1840, 1492–1506. [Google Scholar] [CrossRef] [PubMed]
- Pelagalli, A.; Squillacioti, C.; Mirabella, N.; Meli, R. Aquaporins in Health and Disease: An Overview Focusing on the Gut of Different Species. Int. J. Mol. Sci. 2016, 17, 1213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pulford, E.; McEvoy, J.; Hocking, A.; Prabhakaran, S.; Griggs, K.; Klebe, S. The Effect of Aquaporin 1-Inhibition on Vasculogenic Mimicry in Malignant Mesothelioma. Int. J. Mol. Sci. 2017, 18, 2293. [Google Scholar] [CrossRef] [PubMed]
- Jagirdar, R.M.; Apostolidou, E.; Molyvdas, P.A.; Gourgoulianis, K.I.; Hatzoglou, C.; Zarogiannis, S.G. Influence of AQP1 on cell adhesion, migration, and tumor sphere formation in malignant pleural mesothelioma is substratum- and histological-type dependent. Am. J. Physiol. Lung Cell. Mol. Physiol. 2016, 310, L489–L495. [Google Scholar] [CrossRef] [PubMed]
- Klebe, S.; Griggs, K.; Cheng, Y.; Driml, J.; Henderson, D.W.; Reid, G. Blockade of aquaporin 1 inhibits proliferation, motility, and metastatic potential of mesothelioma in vitro but not in an in vivo model. Dis. Mark. 2015, 2015, 286719. [Google Scholar] [CrossRef] [PubMed]
- Tomita, Y.; Dorward, H.; Yool, A.J.; Smith, E.; Townsend, A.R.; Price, T.J.; Hardingham, J.E. Role of Aquaporin 1 Signalling in Cancer Development and Progression. Int. J. Mol. Sci. 2017, 18, 299. [Google Scholar] [CrossRef] [PubMed]
- Rapisarda, V.; Ledda, C.; Ricceri, V.; Arena, F.; Musumeci, A.; Marconi, A.; Fago, L.; Bracci, M.; Santarelli, L.; Ferrante, M. Detection of pleural plaques in workers exposed to inhalation of natural fluoro-edenitefibres. Oncol. Lett. 2015, 9, 2046–2052. [Google Scholar] [CrossRef] [PubMed]
- Rapisarda, V.; Ledda, C.; Migliore, M.; Salemi, R.; Musumeci, A.; Bracci, M.; Marconi, A.; Loreto, C.; Libra, M. FBLN-3 as a biomarker of pleural plaques in workers occupationally exposed to carcinogenic fibers: A pilot study. Future Oncol. 2015, 11, 35–37. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Loreto, C.; Pomara, C.; Rapisarda, G.; Fiore, M.; Ferrante, M.; Bracci, M.; Santarelli, L.; Fenga, C.; Rapisarda, V. Sheep lymph-nodes as a biological indicator of environmental exposure to fluoro-edenite. Environ. Res. 2016, 147, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Pomara, C.; Bracci, M.; Mangano, D.; Ricceri, V.; Musumeci, A.; Ferrante, M.; Musumeci, G.; Loreto, C.; Fenga, C.; et al. Natural carcinogenicfiber and pleuralplaquesassessment in a general population: A cross-sectionalstudy. Environ. Res. 2016, 150, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Loreto, C.; Matera, S.; Massimino, N.; Cannizzaro, E.; Musumeci, A.; Migliore, M.; Fenga, C.; Pomara, C.; Rapisarda, V. Early effects of fluoro-edenite: Correlation between IL-18 serum levels and pleural and parenchymal abnormalities. Future Oncol. 2016, 12, 59–62. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Loreto, C.; Bracci, M.; Mangano, D.; Migliore, M.; Ricceri, V.; Musumeci, A.; Costa, C.; Pomara, C.; Rapisarda, V. High risk of pleural plaques and parenchymal abnormalities in women living in biancavilla (Italy). Future Oncol. 2016, 12, 63–65. [Google Scholar] [CrossRef] [PubMed]
- Rapisarda, V.; Caltabiano, R.; Musumeci, G.; Castrogiovanni, P.; Ferrante, M.; Ledda, C.; Lombardo, C.; Graziano, A.C.E.; Cardile, V.; Loreto, C. Analysis of fibulin-3 afterexposure to asbestos-likefibers. Environ. Res. 2017, 156, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Costa, C.; Matera, S.; Puglisi, B.; Costanzo, V.; Bracci, M.; Fenga, C.; Rapisarda, V.; Loreto, C. Immunomodulatory effects in workers exposed to naturally occurring asbestos fibers. Mol. Med. Rep. 2017, 15, 3372–3378. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Caltabiano, R.; Loreto, C.; Cinà, D.; Senia, P.; Musumeci, A.; Ricceri, R.; Pomara, C.; Rapisarda, V. Prevalence of anti-nuclear autoantibodies in subjects exposed to natural asbestiform fibers: A cross-sectional study. J. Immunotoxicol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Rapisarda, V.; Loreto, C.; Castorina, S.; Romano, G.; Garozzo, S.F.; Musumeci, A.; Migliore, M.; Avola, R.; Cinà, D.; Pomara, C.; et al. Occupational exposure to Fluoro-edenite and prevalence of anti-nuclearautoantibodies. Future Oncol. 2018. [Google Scholar] [CrossRef]
- Caltabiano, R.; Loreto, C.; Vitale, E.; Matera, S.; Miozzi, E.; Migliore, M.; Angelico, G.; Tumino, R.; Ledda, C.; Rapisarda, V. Fibulin-3 immunoexpression in malignantmesothelioma due to Fluoro-edenite: A preliminary report. Future Oncol. 2018. [Google Scholar] [CrossRef]
- Comba, P.; Gianfagna, A.; Paoletti, L. Pleuralmesotheliomacases in Biancavilla are related to a new fluoro-edenite fibrousamphibole. Arch. Environ. Health 2003, 58, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Paoletti, L.; Batisti, D.; Bruno, C.; di Paola, M.; Gianfagna, A.; Mastrantonio, M.; Nesti, M.; Comba, P. Unusually high incidence of malignant pleural mesothelioma in a town of eastern Sicily: An epidemiological and environmental study. Arch. Environ. Health 2000, 55, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Putzu, M.G.; Bruno, C.; Zona, A.; Massiccio, M.; Pasetto, R.; Piolatto, P.G.; Comba, P. Fluoro-edeniticfibres in the sputum of subjects from Biancavilla (Sicily): A pilot study. Environ. Health 2006, 5, 20. [Google Scholar] [CrossRef] [PubMed]
- Loreto, C.; Rapisarda, V.; Carnazza, M.L.; Musumeci, G.; Valentino, M.; Fenga, C.; Martinez, G. Fluoro-edenite fibres induce lungcellapoptosis: An in vivo study. Histol. Histopathol. 2008, 23, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Grosse, Y.; Loomis, D.; Guyton, K.Z.; Lauby-Secretan, B.; El Ghissassi, F.; Bouvard, V.; Benbrahim-Tallaa, L.; Guha, N.; Scoccianti, C.; Mattock, H.; et al. International Agency for Research on Cancer Monograph Working Group. Carcinogenicity of fluoro-edenite, silicon carbide fibres and whiskers, and carbon nanotubes. Lancet Oncol. 2014, 15, 1427–1428. [Google Scholar] [CrossRef]
- Galateau-Salle, F.; Churg, A.; Roggli, V.; Travis, W.D. World Health Organization CoMMittee for Tumors of the Pleura. The 2015 World Health Organization Classification of Tumors of the Pleura: Advances since the 2004 Classification. J. Thorac. Oncol. 2016, 11, 142–154. [Google Scholar] [CrossRef] [PubMed]
- Jagirdar, R.; Solenov, E.I.; Hatzoglou, C.; Molyvdas, P.A.; Gourgoulianis, K.I.; Zarogiannis, S.G. Gene expression profile of aquaporin 1 and associated interactors in malignant pleural mesothelioma. Gene 2013, 517, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Qin, F.; Zhang, H.; Shao, Y.; Liu, X.; Yang, L.; Huang, Y.; Fu, L.; Gu, F.; Ma, Y. Expression of aquaporin1, a water channel protein, in cytoplasm is negatively correlated with prognosis of breast cancer patients. Oncotarget 2016, 7, 8143–8154. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Yoon, G. Overexpression of aquaporin-1 is a prognostic factor for biochemical recurrence in prostate adenocarcinoma. Pathol. Oncol. Res. 2016, 23, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Yun, S.; Sun, P.L.; Jin, Y.; Kim, H.; Park, E.; Park, S.Y.; Lee, K.; Lee, K.; Chung, J.H. Aquaporin 1 Is an Independent Marker of Poor Prognosis in Lung Adenocarcinoma. J. Pathol. Transl. Med. 2016, 50, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Maugeri, R.; Schiera, G.; di Liegro, C.M.; Fricano, A.; Iacopino, D.G.; di Liegro, I. Aquaporins and Brain Tumors. Int. J. Mol. Sci. 2016, 17, 1029. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Shi, Y.; Amiduo, R.; Tuokan, T.; Suzuk, L. Expression and prognostic value of aquaporin 1, 3 in cervical carcinoma in women of Uygur ethnicity from Xinjiang, China. PLoS ONE 2014, 9, e98576. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.J.; Hu, D.H.; Wu, H.; Xiao, H.; Lu, M.D.; Guo, W.J.; Huang, H.; Yu, Y.J.; Hu, T.Y.; Zheng, Z.Q. Expression of AQP1 Was Associated with Apoptosis and Survival of Patients in Gastric Adenocarcinoma. Dig. Surg. 2016, 33, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Magro, G.; Salvatorelli, L.; Alaggio, R.; D’Agata, V.; Nicoletti, F.; di Cataldo, A.; Parenti, R. Diagnostic utility of cyclin D1 in the diagnosis of small round blue cell tumors in children and adolescents. Hum. Pathol. 2017, 60, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Rapisarda, V. Malignant pleural mesothelioma: The need to move from research to clinical practice. Arch. Med. Res. 2016, 47, 407. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Chae, Y.S.; Lee, S.J.; Kang, B.W.; Kim, J.G.; Kim, W.W.; Jung, J.H.; Park, H.J.; Jeong, J.H.; Jeong, J.Y.; et al. Aquaporin 3 Expression Predicts Survival in Patients with HER2-positive Early Breast Cancer. Anticancer Res. 2015, 35, 2775–2782. [Google Scholar] [PubMed]
- Byung Woog, K.; Jong Gwang, K.; Yee Soo, C.; Min Kyu, J.; Yun-Jin, J.; Ohkyoung, K.; Ghil Suk, Y. AQP1 expression predicts survival in patients with colon cancer. Ann. Oncol. 2014, 25, ii14–ii104. [Google Scholar] [CrossRef]
- Sekine, S.; Shimada, Y.; Nagata, T.; Moriyama, M.; Omura, T.; Watanabe, T.; Hori, R.; Yoshioka, I.; Okumura, T.; Sawada, S.; et al. Prognostic significance of aquaporins in human biliary tract carcinoma. Oncol. Rep. 2012, 27, 1741–1747. [Google Scholar] [CrossRef] [PubMed]
- Marcq, E.; Siozopoulou, V.; de Waele, J.; van Audenaerde, J.; Zwaenepoel, K.; Santermans, E.; Hens, N.; Pauwels, P.; van Meerbeeck, J.P.; Smits, E.L. Prognostic and predictive aspects of the tumor immune microenvironment and immune checkpoints in malignant pleural mesothelioma. Oncoimmunology 2016, 6, e1261241. [Google Scholar] [CrossRef] [PubMed]
- Hill, B.S.; Pelagalli, A.; Passaro, N.; Zannetti, A. Tumor-educated mesenchymal stem cells promote pro-metastatic phenotype. Oncotarget 2017, 8, 73296–73311. [Google Scholar] [CrossRef] [PubMed]

| Case | Age | Sex | Pathological Subtype | Survival Time (Months) | Aquaporin-1 Expression |
|---|---|---|---|---|---|
| 1 | 69 | M | Epithelioid | 1.5 | <50% |
| 2 | 50 | M | Biphasic 20% epithelioid, 80% sarcomatoid | 16 | <50% |
| 3 | 69 | F | Sarcomatoid | 5 | <50% |
| 4 | 74 | F | Epithelioid | 13 | <50% |
| 5 | 85 | M | Epithelioid | 23 | ≥50% |
| 6 | 93 | F | Biphasic 40% epithelioid, 60% sarcomatoid | 7.5 | ≥50% |
| 7 | 58 | F | Epithelioid | 18 | ≥50% |
| 8 | 55 | M | Epithelioid | 37 | ≥50% |
| 9 | 75 | M | Biphasic 40% epithelioid, 60% sarcomatoid | 60 | ≥50% |
| 10 | 56 | M | Epithelioid | 12 | ≥50% |
| Univariate Analysis HR (95% CI) | p-Value | Multivariate Analysis HR (95% CI) | p-Value | |
|---|---|---|---|---|
| <50% | 1 | <0.05 | 1 | <0.05 |
| ≥50% | 1.5 (0.43–5.15) | 1.8 (0.85–4.72) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angelico, G.; Caltabiano, R.; Loreto, C.; Ieni, A.; Tuccari, G.; Ledda, C.; Rapisarda, V. Immunohistochemical Expression of Aquaporin-1 in Fluoro-Edenite-Induced Malignant Mesothelioma: A Preliminary Report. Int. J. Mol. Sci. 2018, 19, 685. https://doi.org/10.3390/ijms19030685
Angelico G, Caltabiano R, Loreto C, Ieni A, Tuccari G, Ledda C, Rapisarda V. Immunohistochemical Expression of Aquaporin-1 in Fluoro-Edenite-Induced Malignant Mesothelioma: A Preliminary Report. International Journal of Molecular Sciences. 2018; 19(3):685. https://doi.org/10.3390/ijms19030685
Chicago/Turabian StyleAngelico, Giuseppe, Rosario Caltabiano, Carla Loreto, Antonio Ieni, Giovanni Tuccari, Caterina Ledda, and Venerando Rapisarda. 2018. "Immunohistochemical Expression of Aquaporin-1 in Fluoro-Edenite-Induced Malignant Mesothelioma: A Preliminary Report" International Journal of Molecular Sciences 19, no. 3: 685. https://doi.org/10.3390/ijms19030685







