A Non-Enzymatic Method to Obtain a Fat Tissue Derivative Highly Enriched in Adipose Stem Cells (ASCs) from Human Lipoaspirates: Preliminary Results
Abstract
:1. Introduction
2. Results
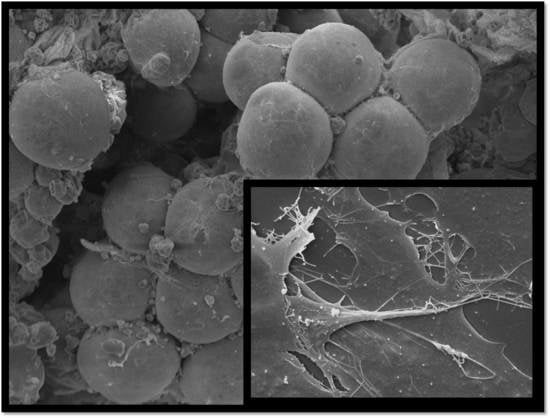
3. Discussion
4. Materials and Methods
4.1. Surgical Procedure to Harvest Adipose Tissue
4.2. Isolation, Expansion and Viability of ASCs
4.3. Growth Curve
4.4. Flow Cytometry Analysis and Phenotype Characterization
4.5. Real-Time PCR
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Abbasi-Malati, Z.; Roushandeh, A.M.; Kuwahara, Y.; Roudkenar, M.H. Mesenchymal stem cells on horizon: A new arsenal of therapeutic agents. Stem Cell Rev. 2018, 14, 484–499. [Google Scholar] [CrossRef] [PubMed]
- Verna, P.; Bansal, H.; Agrawal, A.; Leon, J.; Sundell, I.B.; Koka, P.S. Evaluation of bone marrow processing protocol for therapeutic applications via culture and characterization of mesenchymal stem cells. J. Stem Cells 2016, 11, 3–13. [Google Scholar]
- Koyama, N.; Okubo, Y.; Nakao, K.; Bessho, K. Evaluation of pluripotency in human dental pulp cells. J. Oral Maxillofac. Surg. 2009, 67, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Pozzobon, M.; Piccoli, M.; De Coppi, P. Stem cells from fetal membranes and amniotic fluid: Markers for cell isolation and therapy. Cell Tissue Bank. 2014, 15, 199–211. [Google Scholar] [CrossRef] [PubMed]
- De Francesco, F.; Ricci, G.; D’Andrea, F.; Nicoletti, G.F.; Ferraro, G.A. Human adipose stem cells: From bench to bedside. Tissue Eng. Part B Rev. 2015, 21, 572–584. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rigotti, G.; Marchi, A.; Sbarbati, A. Adipose-derived mesenchymal stem cells: Past, present, and future. Aesthet. Plast. Surg. 2009, 33, 271–273. [Google Scholar] [CrossRef] [PubMed]
- Zuk, P.A.; Zhu, M.; Ashjian, P.; De Ugarte, D.A.; Huang, J.I.; Mizuno, H.; Alfonso, Z.C.; Fraser, J.K.; Benhaim, P.; Hedrick, M.H. Human adipose tissue is a source of multipotent stem cells. Mol. Biol. Cell 2002, 13, 4279–4295. [Google Scholar] [CrossRef] [PubMed]
- Bourin, P.; Bunnell, B.A.; Casteilla, L.; Dominici, M.; Katz, A.J.; March, K.L.; Redl, H.; Rubin, J.P.; Yoshimura, K.; Gimble, J.M. Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-.derived stromal/stem cells: A joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy 2013, 15, 641–648. [Google Scholar] [PubMed]
- The American Society for Aesthetic Plastic Surgery. Cosmetic Surgery National Data Bank Statistics 2017. The American Society for Aesthetic Plastic Surgery: New York. Available online: https://surgery.org/sites/default/files/ASAPS-Stats2017.pdf (accessed on 15 July 2018).
- Coleman, S.R.; Lam, S.; Cohen, S.R.; Bohluli, B.; Nahai, F. Fat grafting: Challenges and debates. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2018, 26, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, S.C.; Bohluli, B.; Consky, E.K. Current techniques in fat grafting. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2018, 26, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Oberbauer, E.; Steffenhagen, C.; Wurzer, C.; Gabriel, C.; Redl, H.; Wolbank, S. Enzymatic and non-enzymatic isolation systems for adipose tissue-derived cells: Current state of the art. Cell Regen. 2015, 4, 7. [Google Scholar] [CrossRef] [PubMed]
- Heo, J.S.; Choi, Y.; Kim, H.S.; Kim, H.O. Comparison of molecular profiles of human mesenchymal stem cells derived from bone marrow, umbilical cord blood, placenta and adipose tissue. Int. J. Mol. Med. 2016, 37, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Bai, J.; Ji, X.; Li, R.; Xuan, Y.; Wang, Y. Comprehensive characterization of four different populations of human mesenchymal stem cells as regards their immune properties, proliferation and differentiation. Int. J. Mol. Med. 2014, 34, 695–704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strioga, M.; Viswanathan, S.; Darinskas, A.; Slaby, O.; Michalek, J. Same or not the same? Comparison of adipose tissue-derived versus bone marrow-derived mesenchymal stem and stromal cells. Stem Cells Dev. 2012, 21, 2724–2752. [Google Scholar] [CrossRef] [PubMed]
- Strem, B.M.; Hicok, K.C.; Zhu, M.; Wulur, I.; Alfonso, Z.; Schreiber, R.E.; Fraser, J.K.; Hedrick, M.H. Multipotential differentiation of adipose tissue-derived stem cells. Keio J. Med. 2005, 54, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, G.A.; De Francesco, F.; Nicoletti, G.; Paino, F.; Desiderio, V.; Tirino, V.; D’Andrea, F. Human adipose CD34+ CD90+ stem cells and collagen scaffold constructs grafted in vivo fabricate loose connective and adipose tissues. J. Cell. Biochem. 2013, 114, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- Gardin, C.; Bressan, E.; Ferroni, L.; Nalesso, E.; Vindigni, V.; Stellini, E.; Pinton, P.; Sivolella, S.; Zavan, B. In vitro concurrent endothelial and osteogenic commitment of adipose-derived stem cells and their genomical analyses through comparative genomic hybridization array: Novel strategies to increase the successful engraftment of tissue-engineered bone grafts. Stem Cells Dev. 2012, 21, 767–777. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.; Lee, A.; Kim, K. The effect of serum types on chondrogenic differentiation of adipose-derived stem cells. Biomater. Res. 2018, 22. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Wang, Z.Q.; Deng, J.Q.; Liao, J.Y.; Wang, X.; Xie, J.; Deng, M.M.; Lu, M.H. Adipose-derived stem cells: A candidate for liver regeneration. J. Dig. Dis. 2015, 16, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Salehi, H.; Amirpour, N.; Niapour, A.; Razavi, S. An overview of neural differentiation potential of human adipose derived stem cells. Stem Cell Rev. 2016, 12, 26–41. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, S.C.; Kim, S.J.; Lee, H.; Jung, E.J.; Jung, S.H.; Han, D.J. Differentiation of human adipose tissue-derived stem cells into aggregates of insulin-producing cells through the overexpression of pancreatic and duodenal homebox gene-1. Cell Transpl. 2013, 22, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- De Francesco, F.; Tirino, V.; Desiderio, V.; Ferraro, G.; D’Andrea, F.; Giuliano, M.; Libondi, G.; De Rosa, A.; Papaccio, G. Human CD34/CD90 ASCs are capable of growing as sphere clusters, producing high levels of VEGF and forming capillaries. PLoS ONE 2009, 4, e6537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guilak, F.; Estes, B.T.; Diekman, B.O.; Moutos, F.T.; Gimble, J.M. 2010 Nicolas Andry Award: Multipotent adult stem cells from adipose tissue for musculoskeletal tissue engineering. Clin. Orthop. Relat. Res. 2010, 468, 2530–2540. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Zachar, V.; Pennisi, C.P.; Fink, T.; Maeda, Y.; Emmersen, J. Hypoxia enhances differentiation of adipose tissue-derived stem cells toward the smooth muscle phenotype. Int. J. Mol. Sci. 2018, 19. [Google Scholar] [CrossRef] [PubMed]
- Shaik, S.; Devireddy, R. Cryopreservation protocols for human adipose tissue derived adult stem cells. Methods Mol. Biol. 2018, 1773, 231–259. [Google Scholar] [PubMed]
- Aronowitz, J.A.; Lockhart, R.A.; Hakakian, C.S. A method for isolation of stromal vascular fraction cells in a clinically relevant time frame. Methods Mol. Biol. 2018, 1773, 11–19. [Google Scholar] [PubMed]
- Tuin, A.J.; Domerchie, P.N.; Schepers, R.H.; Willemsen, J.C.; Dijkstra, P.U.; Spijkervet, F.K.; Vissink, A.; Jansma, J. What is the current optimal fat grafting processing technique? A systematic review. J. Craniomaxillofac. Surg. 2016, 44, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Condè-Green, A.; de Amorim, N.F.; Pitanguy, I. Influence of decantation, washing and centrifugation on adipocyte and mesenchymal stem cell content of aspirated adipose tissue: A comparative study. J. Plast. Sreconstr. Aesthet. Surg. 2010, 63, 1375–1381. [Google Scholar] [CrossRef] [PubMed]
- Agostini, F.; Rossi, F.M.; Aldinucci, D.; Battiston, M.; Lombardi, E.; Zanolin, S.; Massarut, S.; Parodi, P.C.; Da Ponte, A.; Tessitori, G.; et al. Improved GMP compliant approach to manipulate lipoaspirates, to cryopreserve stromal vascular fraction, and to expand adipose stem cells in xeno-free media. Stem Cell Res. Ther. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Raposio, E.; Ciliberti, R. Clinical use of adipose.derived stem cells: European legislative issues. Ann. Med. Surg. 2017, 24, 61–64. [Google Scholar] [CrossRef] [PubMed]
- Peroni, D.; Scambi, I.; Pasini, A.; Lisi, V.; Bifari, F.; Krampera, M.; Rigotti, G.; Sbarbati, A.; Galiè, M. Stem molecular signature of adipose-derived stromal cells. Exp. Cell Res. 2008, 314, 603–615. [Google Scholar] [CrossRef] [PubMed]
- Mushahary, D.; Spittler, A.; Kasper, C.; Weber, V.; Charwat, V. Isolation, cultivation, and characterization of human mesenchymal stem cells. Cytometry A 2018, 93, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Mildmay-White, A.; Khan, W. Cell surface markers on adipose-derived stem cells: A systematic review. Curr. Stem Cell Res. Ther. 2017, 12, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Nicoletti, G.F.; De Francesco, F.; D’Andrea, F.; Ferraro, G.A. Methods and procedures in adipose stem cells: State of the art and perspective for translation medicine. J. Cell Physiol. 2015, 230, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Ueberreiter, K.; Tanzella, U.; Cromme, F.; Doll, D.; Krapohl, B.D. One stage rescue procedure after capsular contracture of breast implants with autologous fat grafts collected by water assisted liposuction (“BEAULI Method”). GMS Interdiscip. Plast. Reconstr. Surg. DGPW 2013, 2. [Google Scholar] [CrossRef]
- Trovato, L.; Monti, M.; Del Fante, C.; Cervio, M.; Lampinem, M.; Ambrosio, L.; Redi, C.A.; Perotti, C.; Kankuri, E.; Ambrosio, G.; et al. A new medical device rigeneracons allows to obtain viable micro-grafts from mechanical disaggregation of human tissues. J. Cell Physiol. 2015, 230, 2299–2303. [Google Scholar] [CrossRef] [PubMed]
- Purpura, V.; Bondioli, E.; Graziano, A.; Trovato, L.; Melandri, D.; Ghetti, M.; Marchesini, A.; Cusella De Angelis, M.G.; Benedetti, L.; Ceccarelli, G.; et al. Tissue characterization after a new disaggregation method for skin micro-grafts generation. J. Vis. Exp. 2016, 4, e53579. [Google Scholar] [CrossRef] [PubMed]




© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Francesco, F.; Mannucci, S.; Conti, G.; Dai Prè, E.; Sbarbati, A.; Riccio, M. A Non-Enzymatic Method to Obtain a Fat Tissue Derivative Highly Enriched in Adipose Stem Cells (ASCs) from Human Lipoaspirates: Preliminary Results. Int. J. Mol. Sci. 2018, 19, 2061. https://doi.org/10.3390/ijms19072061
De Francesco F, Mannucci S, Conti G, Dai Prè E, Sbarbati A, Riccio M. A Non-Enzymatic Method to Obtain a Fat Tissue Derivative Highly Enriched in Adipose Stem Cells (ASCs) from Human Lipoaspirates: Preliminary Results. International Journal of Molecular Sciences. 2018; 19(7):2061. https://doi.org/10.3390/ijms19072061
Chicago/Turabian StyleDe Francesco, Francesco, Silvia Mannucci, Giamaica Conti, Elena Dai Prè, Andrea Sbarbati, and Michele Riccio. 2018. "A Non-Enzymatic Method to Obtain a Fat Tissue Derivative Highly Enriched in Adipose Stem Cells (ASCs) from Human Lipoaspirates: Preliminary Results" International Journal of Molecular Sciences 19, no. 7: 2061. https://doi.org/10.3390/ijms19072061