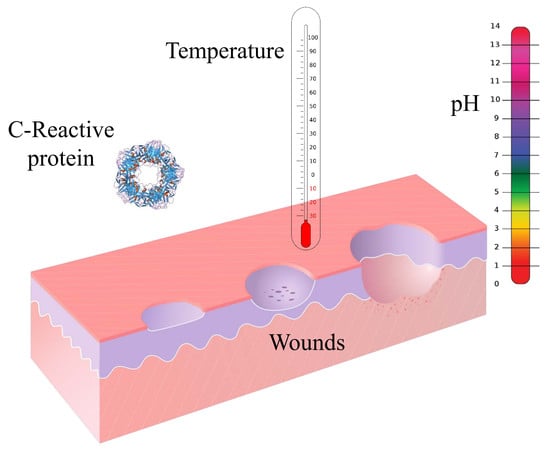
Sensors and Biosensors for C-Reactive Protein, Temperature and pH, and Their Applications for Monitoring Wound Healing: A Review
Abstract
:1. Introduction
2. Sensors for C-Reactive Protein
2.1. Field Effect Transistors
2.2. Optical Technologies
2.2.1. Surface Plasmon Resonance
2.2.2. Total Internal Reflection and Bragg Grating
2.2.3. Fluorescence
2.2.4. Chemiluminescence
2.3. Electrochemistry
2.3.1. Potentiometry
2.3.2. Amperometry
2.3.3. Electrochemical Impedance Spectroscopy
2.4. Piezoelectricity
2.4.1. Quartz Crystal Microbalances
2.4.2. Microcantilever
3. Sensors for Temperature and pH
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Salvo, P.; Dini, V.; Di Francesco, F.; Romanelli, M. The role of biomedical sensors in wound healing. Wound Med. 2015, 8, 15–18. [Google Scholar] [CrossRef]
- Medzhitov, R. Origin and physiological roles of inflammation. Nature 2008, 454, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Nathan, C. Points of control in inflammation. Nature 2002, 420, 846–852. [Google Scholar] [CrossRef] [PubMed]
- Pearson, T.A.; Mensah, G.A.; Wayne Alexander, R.; Anderson, J.L.; Cannon, R.O.; Criqui, M.; Fadl, Y.Y.; Fortmann, S.P.; Hong, Y.; Myers, G.L.; et al. Markers of Inflammation and Cardiovascular Disease. Circulation 2003, 107, 499–511. [Google Scholar] [CrossRef] [PubMed]
- Coussens, L.M.; Werb, Z. Inflammation and cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Hotamisligil, G.S. Inflammation and metabolic disorders. Nature 2006, 444, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Wellen, K.E.; Hotamisligil, G.S. Inflammation, stress, and diabetes. J. Clin. Investig. 2005, 115, 1111–1119. [Google Scholar] [CrossRef] [PubMed]
- Chiricozzi, A.; Zhang, S.; Dattola, A.; Cannizzaro, M.V.; Gabellini, M.; Chimenti, S.; Nistico, S.P. New insights into the pathogenesis of cutaneous autoimmune disorders. J. Biol. Regul. Homeost. Agents 2012, 26, 165–170. [Google Scholar] [PubMed]
- Crystal, R.G.; Bitterman, P.B.; Rennard, S.I.; Hance, A.J.; Keogh, B.A. Interstitial Lung Diseases of Unknown Cause—Disorders Characterized by Chronic Inflammation of the Lower Respiratory Tract. N. Engl. J. Med. 1984, 310, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Dini, V.; Romanelli, M.; Bertone, M.; Talarico, S.; Bombardieri, S.; Barachini, P. Improvement of idiopathic pyoderma gangrenosum during treatment with anti-tumor necrosis factor alfa monoclonal antibody. Int. J. Low Extrem. Wounds 2007, 6, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Dini, V.; Papadia, F.; Di Francesco, F.; Salvo, P.; Paolicchi, A.; Janowska, A.; Chiricozzi, A.; Oranges, T. Potential correlation of wound bed score and biomarkers in chronic lower leg wounds: An exploratory study. J. Wound Care 2017, 26, S9–S17. [Google Scholar] [CrossRef] [PubMed]
- Schultz, G.; Sibbald, G.; Falanga, V.; Ayello, E.; Dowsett, C.; Harding, K.; Romanelli, M.; Stacey, M.; Teot, L.; Vanscheidt, W. Wound bed preparation: A systematic approach to wound management. Wound Repair Regen. 2003, 11, S1–S28. [Google Scholar] [CrossRef] [PubMed]
- Pepys, M.B.; Hirschfield, G.M. C-reactive protein: A critical update. Clin. Investig. 2003, 111, 1805–1812. [Google Scholar] [CrossRef]
- Du Clos, T.W.; Mold, C. C-reactive protein: An activator of innate immunity and a modulator of adaptive immunity. Immunol. Res. 2004, 30, 261–277. [Google Scholar] [CrossRef]
- Reeves, G. C-reactive protein. Aust. Prescr. 2007, 30, 74–76. [Google Scholar] [CrossRef]
- Hennessey, H.; Afara, N.; Omanovic, S.; Padjen, A.L. Electrochemical investigations of the interaction of C-reactive protein (CRP) with a CRP antibody chemically immobilized on a gold surface. Anal. Chim. Acta 2009, 643, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Koivunen, M.E.; Krogsrud, R.L. Principles of Immunochemical Techniques Used in Clinical Laboratories. Lab. Med. 2006, 37, 490–497. [Google Scholar] [CrossRef]
- Bodman-Smith, K.B.; Gregory, R.E.; Harrison, P.T.; Raynes, J.G. FcγRIIa expression with FcγRI results in C-reactive protein and IgG-mediated phagocytosis. J. Leukoc. Biol. 2004, 75, 1029–1035. [Google Scholar] [CrossRef] [PubMed]
- Du Clos, T.W.; Mold, C. The role of C-reactive protein in the resolution of bacterial infection. Curr. Opin. Infect. Dis. 2001, 14, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Szalai, A.J. The antimicrobial activity of C-reactive protein. Microbes Infect. 2002, 4, 201–205. [Google Scholar] [CrossRef]
- Powanda, M.C.; Moyer, E.D. Plasma Proteins and Wound Healing. Surg. Gynecol. Obstet. 1981, 153, 749–755. [Google Scholar] [PubMed]
- Kreutz, R.P.; Owens, J.; Breall, J.A.; Lu, D.; von der Lohe, E.; Bolad, I.; Sinha, A.; Flockhart, D.A. C-reactive protein and fibrin clot strength measured by thrombelastography after coronary stenting. Blood Coagul. Fibrinolysis 2013, 24, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Xu, P.C.; Lin, S.; Yang, X.W.; Gu, D.M.; Yan, T.K.; Wei, L.; Wang, B.L. C-reactive protein enhances activation of coagulation system and inflammatory response through dissociating into monomeric form in antineutrophil cytoplasmic antibody-associated vasculitis. BMC Immunol. 2015, 16, 10. [Google Scholar] [CrossRef] [PubMed]
- Trengove, N.J.; Langton, S.R.; Stacey, M.C. Biochemical analysis of wound fluid from nonhealing and healing chronic leg ulcers. Wound Repair Regen. 1996, 4, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Legendre, C.; Debure, C.; Meaume, S.; Lok, C.; Golmard, J.L.; Senet, P. Impact of protein deficiency on venous ulcer healing. J. Vasc. Surg. 2008, 48, 688–693. [Google Scholar] [CrossRef] [PubMed]
- Van de Goot, F.; Krijnen, P.A.; Begieneman, M.P.; Ulrich, M.M.; Middelkoop, E.; Niessen, H.W. Acute Inflammation is Persistent Locally in Burn Wounds: A Pivotal Role for Complement and C-Reactive Protein. J. Burn Care Res. 2009, 30, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Kingsley, A.; Jones, V. Diagnosing wound infection: The use of C-reactive protein. Wounds UK 2008, 4, 32–46. [Google Scholar] [CrossRef]
- Shukla, V.K.; Shukla, D.; Tiwary, S.K.; Agrawal, S.; Rastogi, A. Evaluation of pH measurement as a method of wound assessment. J. Wound Care 2007, 16, 291–294. [Google Scholar] [CrossRef] [PubMed]
- Romanelli, M.; Gaggio, G.; Coluccia, M.; Rizzello, F.; Piaggesi, A. Technological advances in wound bed measurements. Wounds 2002, 14, 58–66. [Google Scholar]
- Robicsek, F.; Masters, T.N.; Daugherty, H.K. The value of thermography in the early diagnosis of postoperative sternal wound infections. Thorac. Cardiovasc. Surg. 1984, 32, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Romanelli, M.; Miteva, M.; Romanelli, P.; Barbanera, S.; Dini, V. Use of diagnostic in wound management. Curr. Opin. Support. Palliat. Care 2013, 7, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Power, G.; Moore, Z.; O’Connor, T. Measurement of pH, exudate composition and temperature in wound healing: A systematic review. J. Wound Care 2017, 26, 381–397. [Google Scholar] [CrossRef] [PubMed]
- Romanelli, M.; Dini, V.; Barbanera, S.; Bertone, M.S. Evaluation of the efficacy and tolerability of a solution containing propyl betaine and polihexanide for wound irrigation. Skin Pharmacol. Physiol. 2010, 23, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Ono, S.; Imai, R.; Ida, Y.; Shibata, D.; Komiya, T.; Matsumura, H. Increased wound pH as an indicator of local wound infection in second degree burns. Burns 2015, 41, 820–824. [Google Scholar] [CrossRef] [PubMed]
- Percival, S.L.; McCarty, S.; Hunt, J.A.; Woods, E.J. The effects of pH on wound healing, biofilms, and antimicrobial efficacy. Wound Repair Regen. 2014, 22, 174–186. [Google Scholar] [CrossRef] [PubMed]
- Xia, Z.; Sato, A.; Hughes, M.A.; Cherry, G.W. Stimulation of fibroblast growth in vitro by intermittent radiant warming. Wound Repair Regen. 2000, 8, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Whitney, J.D.; Salvadalena, G.; Higa, L.; Mich, M. Treatment of pressure ulcers with noncontact normothermic wound therapy: Healing and warming effects. J. Wound Ostomy Cont. Nurs. 2012, 28, 244–252. [Google Scholar] [CrossRef]
- Lavery, L.A.; Higgins, K.R.; Lanctot, D.R.; Constantinides, G.P.; Zamorano, R.G.; Armstrong, D.G.; Athanasiou, K.A.; Agrawal, C.M. Home monitoring of foot skin temperatures to prevent ulceration. Diabetes Care 2004, 27, 2642–2647. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Holtz-Neiderer, K.; Wendel, C.; Mohler, M.J.; Kimbriel, H.R.; Lavery, L.A. Skin temperature monitoring reduces the risk for diabetic foot ulceration in high-risk patients. Am. J. Med. 2007, 120, 1042–1046. [Google Scholar] [CrossRef] [PubMed]
- Houghton, V.J.; Bower, V.M.; Chant, D.C. Is an increase in skin temperature predictive of neuropathic foot ulceration in people with diabetes? A systematic review and meta-analysis. J. Foot Ankle Res. 2013, 6. [Google Scholar] [CrossRef] [PubMed]
- Dini, V.; Salvo, P.; Janowska, A.; Di Francesco, F.; Barbini, A.; Romanelli, M. Correlation between Wound Temperature Obtained with an Infrared Camera and Clinical Wound Bed Score in Venous Leg Ulcers. Wounds 2015, 27, 274–278. [Google Scholar] [PubMed]
- Fierheller, M.; Sibbald, R.G. A Clinical Investigation into the Relationship between Increased Periwound Skin Temperature and Local Wound Infection in Patients with Chronic Leg Ulcers. Adv. Skin Wound Care 2010, 23, 369–379. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Lipsky, B.A.; Polis, A.B.; Abramson, M.A. Does dermal thermometry predict clinical outcome in diabetic foot infection? Analysis of data from the SIDESTEP. Int. Wound J. 2006, 3, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Romanò, C.L.; Romanò, D.; Dell’Oro, F.; Logoluso, N.; Drago, L. Healing of surgical site after total hip and knee replacements show similar telethermographic patterns. J. Orthop. Traumatol. 2011, 12, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Hazenberg, C.E.; van Netten, J.J.; van Baal, S.G.; Bus, S.A. Assessment of signs of foot infection in diabetes patients using photographic foot imaging and infrared thermography. Diabetes Technol. Ther. 2014, 16, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Hammond, D.J., Jr.; Singh, S.K.; Thompson, J.A.; Beeler, B.W.; Rusiñol, A.E.; Pangburn, M.K.; Potempa, L.A.; Agrawal, A. Identification of acidic pH-dependent ligands of pentameric C-reactive protein. J. Biol. Chem. 2010, 285, 36235–36244. [Google Scholar] [CrossRef] [PubMed]
- Sheu, B.C.; Lin, Y.H.; Lin, C.C.; Lee, A.S.; Chang, W.C.; Wu, J.H.; Tsai, J.C.; Lin, S. Significance of the pH-induced conformational changes in the structure of C-reactive protein measured by dual polarization interferometry. Biosens. Bioelectron. 2010, 26, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Park, H.-J.; Kim, S.K.; Park, K.; Yi, S.Y.; Chung, J.W.; Chung, B.H.; Kim, M. Monitoring of C-Reactive Protein Using Ion Sensitive Field Effect Transistor Biosensor. Sens. Lett. 2010, 8, 233–237. [Google Scholar] [CrossRef]
- Sohn, Y.-S.; Lee, S.-K.; Choi, S.-Y. Detection of C-Reactive Protein Using BioFET and Extended Gate. Sens. Lett. 2007, 5, 421–424. [Google Scholar] [CrossRef]
- Lyu, H.-K.; Choi, Y.-S.; Shin, J.-K.; Kim, J.-H. A commercial MOSFET-based biosensor with a gold extended gate electrode. In Proceedings of the SPIE Defense, Security, and Sensing, Orlando, FL, USA, 25 April 2009. [Google Scholar]
- Sohn, Y.-S.; Kim, Y.T. Field-effect-transistor type C-reactive protein sensor using cysteine-tagged protein G. Electron. Lett. 2008, 44, 955–956. [Google Scholar] [CrossRef]
- Lee, M.H.; Lee, K.N.; Jung, S.W.; Kim, W.H.; Shin, K.S.; Seong, W.K. Quantitative measurements of C-reactive protein using silicon nanowire arrays. Int. J. Nanomed. 2008, 3, 117–124. [Google Scholar] [CrossRef]
- Lee, M.H.; Lee, D.H.; Jung, S.W.; Lee, K.N.; Park, Y.S.; Seong, W.K. Measurements of serum C-reactive protein levels in patients with gastric cancer and quantification using silicon nanowire arrays. Nanomedicine 2010, 6, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.H.; Lee, K.; Jung, S.W. Multiplexed detection of protein markers with silicon nanowire FET and sol-gel matrix. In Proceedings of the 34th Annual International Conference of the IEEE EMBS, San Diego, CA, USA, 28 August–1 September 2012. [Google Scholar]
- Ahn, J.-H.; Kim, J.-Y.; Im, M.; Han, J.-W.; Choi, Y.-K. A nanogap-embedded nanowire field effect transistor for sensor applications: Immunosensor and humidity sensor. In Proceedings of the 14th International Conference on Miniaturized Systems for Chemistry and Life Sciences 2010 (MicroTAS 2010), Groningen, The Netherlands, 3–7 October 2010; pp. 1301–1303. [Google Scholar]
- Kwon, S.M.; Kang, G.B.; Kim, Y.T.; Kim, Y.H.; Ju, B.K. In-situ detection of C-reactive protein using silicon nanowire field effect transistor. J. Nanosci. Nanotechnol. 2011, 11, 1511–1514. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Kwon, H.C.; Yeom, S.H.; Kwon, D.H.; Kang, S.W. MOSFET-BJT hybrid mode of the gated lateral bipolar junction transistor for C-reactive protein detection. Biosens. Bioelectron. 2011, 28, 434–437. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.H.; Ahn, J.H.; Kim, J.Y.; Choi, J.M.; Lim, K.C.; Park, T.J.; Heo, N.S.; Lee, H.G.; Kim, J.W.; Choi, Y.K. CRP detection from serum for chip-based point-of-care testing system. Biosens. Bioelectron. 2013, 41, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Justino, C.I.; Freitas, A.C.; Amaral, J.P.; Rocha-Santos, T.A.; Cardoso, S.; Duarte, A.C. Disposable immunosensors for C-reactive protein based on carbon nanotubes field effect transistors. Talanta 2013, 108, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Sinha, N.; Ma, J.; Yeow, J.T. Carbon nanotube-based sensors. J. Nanosci. Nanotechnol. 2006, 6, 573–590. [Google Scholar] [CrossRef] [PubMed]
- Pioggia, G.; Di Francesco, F.; Ferro, M.; Sorrentino, F.; Salvo, P.; Ahluwalia, A. Characterization of a carbon nanotube polymer composite sensor for an impedimetric electronic tongue. Microchim. Acta 2008, 163, 57–62. [Google Scholar] [CrossRef]
- Lee, H.H.; Bae, M.; Jo, S.H.; Shin, J.K.; Son, D.H.; Won, C.H.; Jeong, H.M.; Lee, J.H.; Kang, S.W. AlGaN/GaN High Electron Mobility Transistor-Based Biosensor for the Detection of C-Reactive Protein. Sensors 2015, 15, 18416–18426. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.H.; Bae, M.; Jo, S.H.; Shin, J.K.; Son, D.H.; Won, C.H.; Lee, J.H. Differential-mode HEMT-based biosensor for real-time and label-free detection of C-reactive protein. Sens. Actuators B Chem. 2016, 234, 316–323. [Google Scholar] [CrossRef]
- Magliulo, M.; De Tullio, D.; Vikholm-Lundin, I.; Albers, W.M.; Munter, T.; Manoli, K.; Palazzo, G.; Torsi, L. Label-free C-reactive protein electronic detection with an electrolyte-gated organic field-effect transistor-based immunosensor. Anal. Bioanal. Chem. 2016, 408, 3943–3952. [Google Scholar] [CrossRef] [PubMed]
- Homola, J.; Yee, S.S.; Gauglitz, G. Surface plasmon resonance sensors: Review. Sens. Actuators B Chem. 1999, 54, 3–15. [Google Scholar] [CrossRef]
- Homola, J. Surface plasmon resonance sensors for detection of chemical and biological species. Chem. Rev. 2008, 108, 462–493. [Google Scholar] [CrossRef] [PubMed]
- Casa, E.; Kurosawa, C.; Kurosawa, S.; Aizawa, H.; Park, J.-W.; Suzuki, H. Immunosensor Using Surface Plasmon Resonance for C-Reactive Protein Detection. Electrochemistry 2006, 74, 153–155. [Google Scholar] [CrossRef]
- Meyer, M.H.; Hartmann, M.; Keusgen, M. SPR-based immunosensor for the CRP detection—A new method to detect a well known protein. Biosens. Bioelectron. 2006, 21, 1987–1990. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.P.; Hsu, H.Y.; Chiou, A.; Tseng, K.Y.; Lin, H.Y.; Chang, G.L.; Chen, S.J. Immunodetection of pentamer and modified C-reactive protein using surface plasmon resonance biosensing. Biosens. Bioelectron. 2006, 21, 1631–1637. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.H.; Jung, J.W.; Suh, I.B.; Yuk, J.S.; Kim, W.J.; Choi, E.Y.; Kim, Y.M.; Ha, K.S. Analysis of C-reactive protein on amide-linked N-hydroxysuccinimide-dextran arrays with a spectral surface plasmon resonance biosensor for serodiagnosis. Anal. Chem. 2007, 79, 5703–5710. [Google Scholar] [CrossRef] [PubMed]
- Bini, A.; Centi, S.; Tombelli, S.; Minunni, M.; Mascini, M. Development of an optical RNA-based aptasensor for C-reactive protein. Anal. Bioanal. Chem. 2008, 390, 1077–1086. [Google Scholar] [CrossRef] [PubMed]
- Vance, S.A.; Sandros, M.G. Zeptomole Detection of C-Reactive Protein in Serum by a Nanoparticle Amplified Surface Plasmon Resonance Imaging Aptasensor. Sci. Rep. 2014, 4. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Wang, Y.; Wang, K.; Wang, Q.; Wang, P.; Lin, W.; Chen, N.; Tan, Y. DNA aptamer-based surface plasmon resonance sensing of human C-reactive protein. RSC Adv. 2014, 4, 30934–30937. [Google Scholar] [CrossRef]
- Matsuura, R.; Tawa, K.; Kitayama, Y.; Takeuchi, T. A plasmonic chip-based bio/chemical hybrid sensing system for the highly sensitive detection of C-reactive protein. Chem. Commun. 2016, 52, 3883–3886. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Jiang, R.; Wang, Q.; Huang, J.; Yang, X.; Wang, K.; Li, W.; Chen, N.; Li, Q. Detection of C-reactive protein using nanoparticle-enhanced surface plasmon resonance using an aptamer-antibody sandwich assay. Chem. Commun. 2016, 52, 3568–3571. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.-H.; Ko, H.; Lee, G.-Y.; Chang, S.-Y.; Chang, Y.-W.; Kang, M.-J.; Pyun, J.-C. Development of a sensitive SPR biosensor for C-reactive protein (CRP) using plasma-treated parylene-N film. Sens. Actuators B Chem. 2015, 207, 133–138. [Google Scholar] [CrossRef]
- Aray, A.; Chiavaioli, F.; Arjmand, M.; Trono, C.; Tombelli, S.; Giannetti, A.; Cennamo, N.; Soltanolkotabi, M.; Zeni, L.; Baldini, F. SPR-based plastic optical fibre biosensor for the detection of C-reactive protein in serum. J. Biophotonics 2016, 9, 1077–1084. [Google Scholar] [CrossRef] [PubMed]
- Chou, C.; Hsu, H.Y.; Wu, H.T.; Tseng, K.Y.; Chiou, A.; Yu, C.J.; Lee, Z.Y.; Chan, T.S. Fiber optic biosensor for the detection of C-reactive protein and the study of protein binding kinetics. J. Biomed. Opt. 2007, 12, 024025. [Google Scholar] [CrossRef] [PubMed]
- Sridevi, S.; Vasu, K.S.; Asokan, S.; Sood, A.K. Sensitive detection of C-reactive protein using optical fiber Bragg gratings. Biosens. Bioelectron. 2015, 65, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Wolf, M.; Juncker, D.; Michel, B.; Hunziker, P.; Delamarche, E. Simultaneous detection of C-reactive protein and other cardiac markers in human plasma using micromosaic immunoassays and self-regulating microfluidic networks. Biosens. Bioelectron. 2004, 19, 1193–1202. [Google Scholar] [CrossRef] [PubMed]
- Christodoulides, N.; Mohanty, S.; Miller, C.S.; Langub, M.C.; Floriano, P.N.; Dharshan, P.; Ali, M.F.; Bernard, B.; Romanovicz, D.; Anslyn, E.; et al. Application of microchip assay system for the measurement of C-reactive protein in human saliva. Lab Chip 2005, 5, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Ghimenti, S.; Lomonaco, T.; Onor, M.; Murgia, L.; Paolicchi, A.; Fuoco, R.; Ruocco, L.; Pellegrini, G.; Trivella, M.G.; Di Francesco, F. Measurement of Warfarin in the Oral Fluid of Patients Undergoing Anticoagulant Oral Therapy. PLoS ONE 2011, 6, e28182. [Google Scholar] [CrossRef] [PubMed]
- Bellagambi, F.G.; Degano, I.; Ghimenti, S.; Lomonaco, T.; Dini, V.; Romanelli, M.; Mastorci, F.; Gemignani, A.; Salvo, P.; Fuoco, R.; et al. Determination of salivary α-amylase and cortisol in psoriatic subjects undergoing the Trier Social Stress Test. Microchem. J. 2018, 136, 177–184. [Google Scholar] [CrossRef]
- Bellagambi, F.G.; Baraket, A.; Longo, A.; Vatteroni, M.; Zine, N.; Baussells, J.; Fuoco, R.; Di Francesco, F.; Salvo, P.; Karanasiou, G.S.; et al. Electrochmical biosensor platform for TNF-α cytokines detection in both artificial and real human saliva: Heart Failure. Sens. Actuators B Chem. 2017, 251, 1026–1033. [Google Scholar] [CrossRef]
- Baldini, F.; Carloni, A.; Giannetti, A.; Porro, G.; Trono, C. An optical PMMA biochip based on fluorescence anisotropy: Application to C-reactive protein assay. Sens. Actuators B Chem. 2009, 139, 64–68. [Google Scholar] [CrossRef]
- Algarra, M.; Campos, B.B.; Gomes, D.; Alonso, B.; Casado, C.M.; Arrebola, M.M.; Diez de los Rios, M.J.; Herrera-Gutiérrez, M.E.; Seller-Pérez, G.; Esteces da Silva, J.C.G. Thiolated DAB dendrimer/ZnSe nanoparticles for C-reactive protein recognition in human serum. Talanta 2012, 99, 574–579. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Harris, E.; Shi, J.; Chen, A.; Parajuli, S.; Jing, X.; Miao, W. Electrogenerated chemiluminescence determination of C-reactive protein with carboxyl CdSe/ZnS core/shell quantum dots. Phys. Chem. Chem. Phys. 2010, 12, 10073–10080. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.-B.; Chen, Y.-H.; Lin, H.-I.; Shiesh, S.-C.; Lee, G.-B. An integrated microfluidic system for fast; automatic detection of C-reactive protein. Sens. Actuators B Chem. 2011, 157, 710–721. [Google Scholar] [CrossRef]
- Pohanka, M.; Skladal, P. Electrochemical biosensors-principles and applications. J. Appl. Biomed. 2008, 6, 57–64. [Google Scholar]
- Zhu, J.-J.; Xu, J.-Z.; He, J.-T.; Wang, Y.-J.; Miao, Q.; Chen, H.-Y. An Electrochemical Immunosensor for Assays of C-Reactive Protein. Anal. Lett. 2003, 36, 1547–1556. [Google Scholar] [CrossRef]
- Ibupoto, Z.H.; Jamal, N.; Khun, K.; Willander, M. Development of a disposable potentiometric antibody immobilized ZnO nanotubes based sensor for the detection of C-reactive protein. Sens. Actuators B Chem. 2012, 166–167, 809–814. [Google Scholar] [CrossRef]
- Fakanya, W.M.; Tothill, I.E. Detection of the Inflammation Biomarker C-Reactive Protein in Serum Samples: Towards an Optimal Biosensor Formula. Biosensors 2014, 4, 340–357. [Google Scholar] [CrossRef] [PubMed]
- Kokkinos, C.; Prodromidis, M.; Economou, A.; Petrou, P.; Kakabakos, S. Disposable integrated bismuth citrate-modified screen-printed immunosensor for ultrasensitive quantum dot-based electrochemical assay of C-reactive protein in human serum. Anal. Chim. Acta 2015, 886, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Buch, M.; Rishpon, J. An Electrochemical Immunosensor for C-Reactive Protein Based on Multi-Walled Carbon Nanotube-Modified Electrodes. Electroanalysis 2008, 20, 2592–2594. [Google Scholar] [CrossRef]
- Esteban-Fernández de Ávila, B.; Escamilla-Gómez, V.; Campuzano, S.; Pedrero, M.; Salvador, J.-P.; Marco, M.-P.; Pingarrón, J.M. Ultrasensitive amperometric magnetoimmunosensor for human C-reactive protein quantification in serum. Sens. Actuators B Chem. 2013, 188, 212–220. [Google Scholar] [CrossRef]
- Daniels, J.S.; Pourmand, N. Label-Free Impedance Biosensors: Opportunities and Challenges. Electroanalysis 2007, 19, 1239–1257. [Google Scholar] [CrossRef] [PubMed]
- Songjaroen, T.; Feeny, R.M.; Mensack, M.M.; Laiwattanapaisal, W.; Henry, C.S. Label-free detection of C-reactive protein using an electrochemical DNA immunoassay. Sens. Biosens. Res. 2016, 8, 14–19. [Google Scholar] [CrossRef]
- Salvo, P.; Henry, O.Y.; Dhaenens, K.; Acero Sanchez, J.L.; Gielen, A.; Werne Solnestam, B.; Lundeberg, J.; O’Sullivan, C.K.; Vanfleteren, J. Fabrication and functionalization of PCB gold electrodes suitable for DNA-based electrochemical sensing. Biomed. Mater. Eng. 2014, 24, 1705–1714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, R.K.; Periyakaruppan, A.; Meyyappan, M.; Koehne, J.E. Label-free detection of C-reactive protein using a carbon nanofiber based biosensor. Biosens. Bioelectron. 2014, 59, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Dineva, P.S.; Gross, D.; Müller, R.; Rangelov, T. Piezoelectric Materials. In Dynamic Fracture of Piezoelectric Materials: Solutions of Time-Harmonic Problems via BIEM; Springer: Cham, Switzerland, 2014; Volume 212, pp. 7–32. ISBN 978-3-319-03961-9. [Google Scholar]
- Pramanik, S.; Pingguan-Murphy, B.; Abu Osman, N.A. Developments of Immobilized Surface Modified Piezoelectric Crystal Biosensors for Advanced Applications. Int. J. Electrochem. Sci. 2013, 8, 8863–8892. [Google Scholar]
- Brecht, A.; Göpel, W. Quartz crystal microbalances for quantitative biosensing and characterizing protein multilayers. Biosens. Bioelectron. 1997, 12, 567–575. [Google Scholar] [CrossRef]
- Raiteri, R.; Grattarola, M.; Butt, H.-J.; Skládal, P. Micromechanical cantilever-based biosensors. Sens. Actuators B Chem. 2001, 79, 115–126. [Google Scholar] [CrossRef]
- Gan, N.; Xiong, P.; Wang, J.; Li, T.; Hu, F.; Cao, Y.; Zheng, L. A Novel Signal-Amplified Immunoassay for the Detection of C-Reactive Protein Using HRP-Doped Magnetic Nanoparticles as Labels with the Electrochemical Quartz Crystal Microbalance as a Detector. J. Anal. Methods Chem. 2013, 2013, 482316. [Google Scholar] [CrossRef] [PubMed]
- Ding, P.; Liu, R.; Liu, S.; Mao, X.; Hu, R.; Li, G. Reusable gold nanoparticle enhanced QCM immunosensor for detecting C-reactive protein. Sens. Actuators B Chem. 2013, 188, 1277–1283. [Google Scholar] [CrossRef]
- Aizawa, H.; Kurosawa, S.; Ogawa, K.; Yoshimoto, M.; Miyake, J.; Tanaka, H. Conventional diagnosis of C-reactive protein in serum using latex piezoelectric immunoassay. Sens. Actuators B Chem. 2001, 76, 173–176. [Google Scholar] [CrossRef]
- Kim, N.; Kim, D.-K.; Cho, Y.-J. Development of indirect-competitive quartz crystal microbalance immunosensor for C-reactive protein. Sens. Actuators B Chem. 2009, 143, 444–448. [Google Scholar] [CrossRef]
- Kim, N.; Kim, D.-K.; Cho, Y.-J. Gold nanoparticle-based signal augmentation of quartz crystal microbalance immunosensor measuring C-reactive protein. Curr. Appl. Phys. 2010, 10, 1227–1230. [Google Scholar] [CrossRef]
- Lee, J.H.; Yoon, K.H.; Hwang, K.S.; Park, J.; Ahn, S.; Kim, T.S. Label free novel electrical detection using micromachined PZT monolithic thin film cantilever for the detection of C-reactive protein. Biosens. Bioelectron. 2004, 20, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Wee, K.W.; Kang, G.Y.; Park, J.; Kang, J.Y.; Yoon, D.S.; Park, J.H.; Kim, T.S. Novel electrical detection of label-free disease marker proteins using piezoresistive self-sensing micro-cantilevers. Biosens. Bioelectron. 2005, 20, 1932–1938. [Google Scholar] [CrossRef] [PubMed]
- Yen, Y.K.; Lai, Y.C.; Hong, W.T.; Pheanpanitporn, Y.; Chen, C.S.; Huang, L.S. Electrical detection of C-reactive protein using a single free-standing; thermally controlled piezoresistive microcantilever for highly reproducible and accurate measurements. Sensors 2013, 13, 9653–9668. [Google Scholar] [CrossRef] [PubMed]
- Dargaville, T.R.; Farrugia, B.L.; Broadbent, J.A.; Pace, S.; Upton, Z.; Voelcker, N.H. Sensors and imaging for wound healing: A review. Biosens. Bioelectron. 2013, 41, 30–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McNeill, J.; Sen, D.; Mendelson, Y.; Crivello, M.; Mazumder, S.; Agdeppa, A.; Hussain, S.A.; Kim, H.; Loehle, V.; Dunn, R.; et al. Wearable Wireless Sensor Patch for Continuous Monitoring of Skin Temperature, Pressure, and Relative Humidity. In Proceedings of the 2017 IEEE International Symposium on Circuits and Systems (ISCAS), Baltimore, MD, USA, 28–31 May 2017. [Google Scholar]
- Yamamoto, Y.; Yamamoto, D.; Takada, M.; Naito, H.; Arie, T.; Akita, S.; Takei, K. Efficient Skin Temperature Sensor and Stable Gel-Less Sticky ECG Sensor for a Wearable Flexible Healthcare Patch. Adv. Healthc. Mater. 2017, 6, 1700495. [Google Scholar] [CrossRef] [PubMed]
- Nakata, S.; Arie, T.; Akita, S.; Takei, K. Wearable, Flexible, and Multifunctional Healthcare Device with an ISFET Chemical Sensor for Simultaneous Sweat pH and Skin Temperature Monitoring. ACS Sens. 2017, 2, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Trung, T.Q.; Ramasundaram, S.; Hwang, B.U.; Lee, N.E. An All-Elastomeric Transparent and Stretchable Temperature Sensor for Body-Attachable Wearable Electronics. Adv. Mater. 2016, 28, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Giuliani, A.; Placidi, M.; Di Francesco, F.; Pucci, A. A new polystyrene-based ionomer/MWCNT nanocomposite for wearable skin temperature sensors. React. Funct. Polym. 2014, 76, 57–62. [Google Scholar] [CrossRef] [Green Version]
- Calisi, N.; Giuliani, A.; Alderighi, M.; Schnorr, J.M.; Swager, T.M.; Di Francesco, F.; Pucci, A. Factors affecting the dispersion of MWCNTs in electrically conducting SEBS nanocomposites. Eur. Polym. J. 2013, 49, 1471–1478. [Google Scholar] [CrossRef]
- Calisi, N.; Salvo, P.; Melai, B.; Paoletti, C.; Pucci, A.; Di Francesco, F. Effects of thermal annealing on SEBS/MWCNTs temperature-sensitive nanocomposites for the measurement of skin temperature. Mater. Chem. Phys. 2017, 186, 456–461. [Google Scholar] [CrossRef]
- Salvo, P.; Calisi, N.; Melai, B.; Cortigiani, B.; Mannini, M.; Caneschi, A.; Lorenzetti, G.; Paoletti, C.; Lomonaco, T.; Paolicchi, A.; et al. Temperature and pH sensors based on graphenic materials. Biosens. Bioelectron. 2017, 91, 870–877. [Google Scholar] [CrossRef] [PubMed]
- Salvo, P.; Calisi, N.; Melai, B.; Dini, V.; Paoletti, C.; Lomonaco, T.; Pucci, A.; Di Francesco, F.; Piaggesi, A.; Romanelli, M. Temperature- and pH-sensitive wearable materials for monitoring foot ulcers. Int. J. Nanomed. 2017, 12, 949–954. [Google Scholar] [CrossRef] [PubMed]
- Melai, B.; Salvo, P.; Calisi, N.; Moni, L.; Bonini, A.; Paoletti, C.; Lomonaco, T.; Mollica, V.; Fuoco, R.; Di Francesco, F. A graphene oxide pH sensor for wound monitoring. In Proceedings of the 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016. [Google Scholar]
- Salvo, P.; Melai, B.; Calisi, N.; Paoletti, C.; Bellagambi, F.; Kirchhain, A.; Trivella, M.G.; Fuoco, R.; Di Francesco, F. Graphene-based devices for measuring pH. Sens. Actuators B Chem. 2018, in press. [Google Scholar] [CrossRef]
- Zhou, J.; Zhang, L.; Tian, Y. Micro Electrochemical pH Sensor Applicable for Real-Time Ratiometric Monitoring of pH Values in Rat Brains. Anal. Chem. 2016, 88, 2113–2118. [Google Scholar] [CrossRef] [PubMed]
- Nanasaki, S.; Horiuchi, H.; Inada, H.; Nakamura, Y.; Dasai, F.; Iwata, T.; Takahashi, K.; Nabekura, J.; Sawada, K. Development of novel pH image sensor for in vivo apprication. In Proceedings of the 19th International Conference on Solid-State Sensors, Actuators and Microsystems (TRANSDUCERS), Kaohsiung, Taiwan, 18–22 June 2017; pp. 43–46. [Google Scholar]
- Rahimi, R.; Ochoa, M.; Parupudi, T.; Zhao, X.; Yazdi, I.K.; Dokmeci, M.R.; Tamayol, A.; Khademhosseini, A.; Ziaie, B. A low-cost flexible pH sensor array for wound assessment. Sens. Actuators B Chem. 2016, 229, 609–617. [Google Scholar] [CrossRef]
- Panzarasa, G.; Osypova, A.; Toncelli, C.; Buhmann, M.T.; Rottmar, M.; Ren, Q.; Maniura-Weber, K.; Rossi, R.M.; Boesel, L.F. The pyranine-benzalkonium ion pair: A promising fluorescent system for the ratiometric detection of wound pH. Sens. Actuators B Chem. 2017, 249, 156–160. [Google Scholar] [CrossRef]
- Yoon, J.H.; Hong, S.B.; Yun, S.O.; Lee, S.J.; Lee, T.J.; Lee, K.G.; Choi, B.G. High performance flexible pH sensor based on polyaniline nanopillar array electrode. J. Colloid Interface Sci. 2017, 490, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Salvo, P.; Smajda, R.; Dini, V.; Saxby, C.; Voirin, G.; Romanelli, M.; Di Francesco, F. A D-optimal design to model the performances of dressings and devices for negative pressure wound therapy. J. Tissue Viability 2016, 25, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Chen, L.H.; Dong, X.; Yang, J.; Long, H.Y.; So, P.S.; Chan, C.C. Miniature pH Optical Fiber Sensor Based on Fabry–Perot Interferometer. IEEE J. Sel. Top. Quantum Electron. 2016, 22, 331–335. [Google Scholar] [CrossRef]
- Cerveró-Ferragut, S.; López-Riquelme, N.; Martín-Tomás, E.; Massa-Domínguez, B.; Pomares-Vicente, J.; Soler-Pérez, M.; Sánchez-Hernández, J.F. Quantitative analysis of blood cells and inflammatory factors in wounds. J. Wound Care 2017, 26, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Yang, F.; Li, Z.; Yi, C.; Bai, X. A Prospective Pilot Study to Evaluate Wound Outcomes and Levels of Serum C-reactive Protein and Interleukin-6 in the Wound Fluid of Patients with Trauma-related Chronic Wounds. Ostomy Wound Manag. 2014, 60, 30–37. [Google Scholar]
- Chapman, G.; Holton, J.; Chapman, A. A threshold for concern? C-reactive protein levels following operatively managed neck of femur fractures can detect infectious complications with a simple formula. Clin. Biochem. 2016, 49, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Jeandrot, A.; Richard, J.L.; Combescure, C.; Jourdan, N.; Finge, S.; Rodier, M.; Corbeau, P.; Sotto, A.; Lavigne, J.P. Serum procalcitonin and C-reactive protein concentrations to distinguish mildly infected from non-infected diabetic foot ulcers: A pilot study. Diabetologia 2008, 51, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Goodfield, M.J. C-reactive protein levels in venous ulceration: An indication of infection? J. Am. Acad. Dermatol. 1988, 18, 1048–1052. [Google Scholar] [CrossRef]
- Van Asten, S.A.; Jupiter, D.C.; Mithani, M.; La Fontaine, J.; Davis, K.E.; Lavery, L.A. Erythrocyte sedimentation rate and C-reactive protein to monitor treatment outcomes in diabetic foot osteomyelitis. Int. Wound J. 2017, 14, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Fujii, T.; Tabe, Y.; Yajima, R.; Tsutsumi, S.; Asao, T.; Kuwano, H. Relationship between C-reactive protein levels and wound infections in elective colorectal surgery: C-reactive protein as a predictor for incisional SSI. Hepatogastroenterology 2011, 58, 752–755. [Google Scholar] [PubMed]





| Measurement Technique/Device | Detection Layer | Medium | Range | Measurement Time (Excluding Preparation) | Sensitivity | Reference |
|---|---|---|---|---|---|---|
| FET | ||||||
| EGFET | anti-CRP | PBS | 3–10 mg/L | N.A. | N.A. | [49] |
| FET | Cysteine-tagged protein G + anti-CRP | PBS | 3–20 mg/L | ≈10 min | ≈ 0.01 µg/mL/(A/A) | [51] |
| SiNW-FET | anti-CRP | PBS | 1 fM–1 nM | ≈200 s | N.A. | [52] |
| SiNW-FET | anti-CRP | Serum | 3.2–10.4 mg/L | N.A. | N.A. | [53] |
| SiNW-FET | Sol-gel + anti-CRP | Serum | 0.12–10 µg/L | N.A. | N.A. | [54] |
| NG-SiNW-FET | anti-CRP | PBS | 100 mg/L | N.A. | N.A. | [55] |
| SiNW-FET | anti-CRP | PBS | 0.1–10 mg/L | <100 s | 16–39% of conductance variation | [56] |
| MOSFET-BJT | anti-CRP | PBS | 1 pmol/L–1 µmol/L | N.A. | 0.80 µA/decade @ base current = −10 µA for BJT | [57] |
| NG-FET | SBP-spA + anti-CRP | Serum | 100 µg/L | N.A. | 3.4 V/g/mL | [58] |
| NTFET | anti-CRP | PBS | 10−4–102 mg/L | N.A. | 0.2% of current variation/0.1% CRP concentration | [59] |
| Differential mode-HEMT | anti-CRP | PBS | 0.01–1000 µg/L | ≈100 s | N.A. | [63] |
| EGOFET | P3HT + anti-CRP | PBS | 220 ng/L–200 mg/L | N.A. | N.A. | [64] |
| Optical | ||||||
| SPR | anti-CRP | PBS | 1–10 mg/L | 10 min | N.A. | [67] |
| SPR | Biotinylated anti-CRP | PBS | 2–5 mg/L | <1 h | ~10.7 A.U./(µg/mL) | [68] |
| SPR | Protein G + anti-CRP | Tris buffered saline–calcium | 1–26 mg/L | 10 min | N.A. | [69] |
| SPR | amide-linked NHS-dextran + anti-CRP | Serum | 0.1–50 mg/L | N.A. | N.A. | [70] |
| SPR | RNA aptamer | Serum | 0.005–0.1 ppm | 15 min | ~2827 Resonance unit/ppm | [71] |
| SPR | Aptamer + QDs | Serum | 5–5000 pg/L | ~20 min | N.A. | [72] |
| SPR | DNA aptamers | N.A. | 0.35–12.5 nmol/L | N.A. | 0.0044 degree shift/nmol/L | [73] |
| SPR | PMPC | Serum | 10–1000 pM | N.A. | N.A. | [74] |
| SPR | Aptamer | Serum | 10 pM–100 nM | N.A. | N.A. | [75] |
| SPR | Parylene-N + anti-CRP | N.A. | 1–1000 µg/L | ~20 min | N.A. | [76] |
| SPR + optical fiber | anti-CRP | Serum | 9 µg/L–70 mg/L | ~10 min | 104 nm/RIU | [77] |
| Optical fiber | anti-CRP | PBS | 5–12.5 mg/L | 10 min | 107 s−1/molar for pCRP; ~317 × 103 s−1/molar for mCRP | [78] |
| Fiber Bragg grating | GO + anti-CRP | Serum | 0.01–100 mg/L | N.A. | N.A. | [79] |
| Fluorescence | anti-CRP | Plasma | 0.03–5 mg/L | 180 s | N.A. | [80] |
| Fluorescence | anti-CRP | Saliva | 10 pg/L–10 ng/L | 12 min | N.A. | [81] |
| Fluorescence | anti-CRP | HEPES | 0.1–50 mg/L (LOD 0.004 mg/L) | ~26 min | N.A. | [85] |
| Fluorescence | S-DAB–ZnSe–PEA QDs + anti-CRP | Serum | 0.5–10 mg/L | N.A. | −2 × 10−8 A.U./log(mg/L) | [86] |
| Chemiluminescence | CdSe/ZnS/PEG-COOH QDs + anti-CRP | PBS | 1–10 mg/L | >3 h | N.A. | [87] |
| Chemiluminescence | ssDNA | PBST | 0.0125–10 mg/L | 30 min | ≈ 171/ | [88] |
| Electrochemistry | ||||||
| Potentiometry | Cysteamine + Au NPs + anti-CRP | NaCl | 5–25 mg/L | 10 min | N.A. | [90] |
| Potentiometry | ZnO + anti-CRP | PBS | 10−6–1 mg/L | <10 s | ~13 V/log[Conc.(mg/L)] | [91] |
| Amperometry | anti-CRP | Serum | 2.6–100 µg/L | 200 s | 0.026 µA/(ng/mL) in 2.6–50 ng/mL | [92] |
| Amperometry | anti-CRP + lead sulfide QDs | HNO3 | 0.2–100 µg/L, LOD 0.05 µg/L | >2 h | N.A. | [93] |
| Amperometry | anti-CRP + HRP + TMB | PBS | 0.5–200 µg/L | 10 min | N.A. | [94] |
| Amperometry | HOOC-MBs + anti-CRP | Serum | 0.07–1000 µg/L, LOD 0.021 µg/L | 90 min | 2 × 10−7 A | [95] |
| EIS | ssDNA + anti-CRP | Serum | 12–25 mg/L | >10 min | 0.0067 Ω/(mg/L) in 3.125–25 mg/L | [97] |
| EIS | anti-CRP | PBS | ~0.4–42 nM, LOD 11 µg/L | >1 h | N.A. | [99] |
| Piezoelectricity | ||||||
| QCM | Fe3O4 and Au NPs + anti-CRP | PBS | 0.003–200 µg/L, LOD 1 ng/L | 30 min | N.A. | [104] |
| QCM | Au NPs + anti-CRP | PBS | 0.02–30 mg/L | >1 h | 11 Hz/(µg/mL) | [105] |
| QCM | anti-CRP | Serum | ~170–667 µg/L | ~60 min | ~10 Hz/(µg/dL) | [106] |
| QCM | SA-coated Au NPs + anti-CRP | PBS | 0.1 pM–0.53 nM | ~25 min | N.A. | [108] |
| Microcantilever | anti-CRP | PBS | 100 µg/L and 1 mg/L | >15 min | N.A. | [110] |
| Microcantilever | anti-CRP | PBS | 1–200 mg/L, linear in 10–100 mg/L | ~50 min | N.A. | [111] |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salvo, P.; Dini, V.; Kirchhain, A.; Janowska, A.; Oranges, T.; Chiricozzi, A.; Lomonaco, T.; Di Francesco, F.; Romanelli, M. Sensors and Biosensors for C-Reactive Protein, Temperature and pH, and Their Applications for Monitoring Wound Healing: A Review. Sensors 2017, 17, 2952. https://doi.org/10.3390/s17122952
Salvo P, Dini V, Kirchhain A, Janowska A, Oranges T, Chiricozzi A, Lomonaco T, Di Francesco F, Romanelli M. Sensors and Biosensors for C-Reactive Protein, Temperature and pH, and Their Applications for Monitoring Wound Healing: A Review. Sensors. 2017; 17(12):2952. https://doi.org/10.3390/s17122952
Chicago/Turabian StyleSalvo, Pietro, Valentina Dini, Arno Kirchhain, Agata Janowska, Teresa Oranges, Andrea Chiricozzi, Tommaso Lomonaco, Fabio Di Francesco, and Marco Romanelli. 2017. "Sensors and Biosensors for C-Reactive Protein, Temperature and pH, and Their Applications for Monitoring Wound Healing: A Review" Sensors 17, no. 12: 2952. https://doi.org/10.3390/s17122952