Design and Validation of a Low-Cost Portable Device to Quantify Postural Stability †
Abstract
:1. Introduction
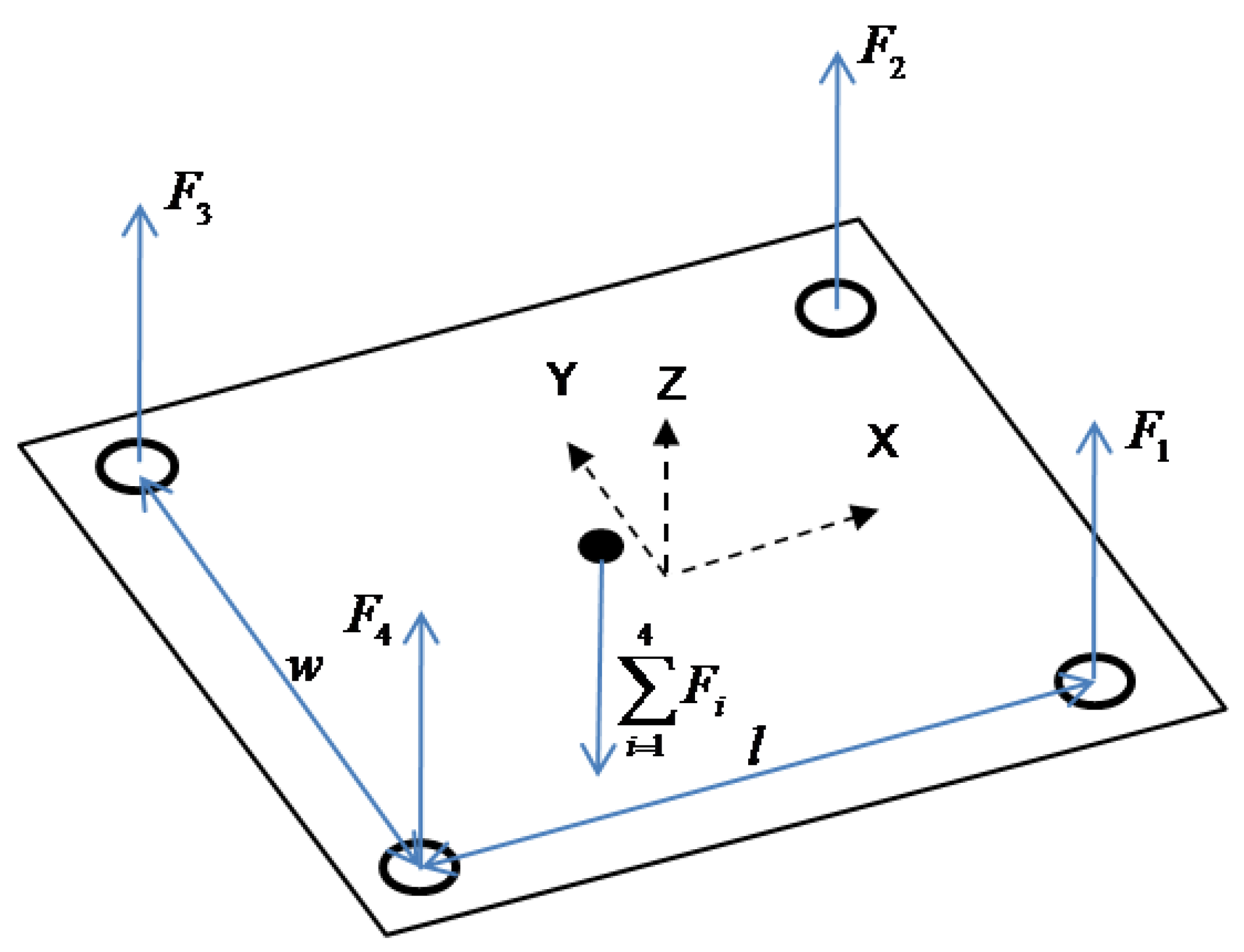
2. Related Work
2.1. Center-of-Pressure (COP)
2.2. Approximate Entropy (ApEn)
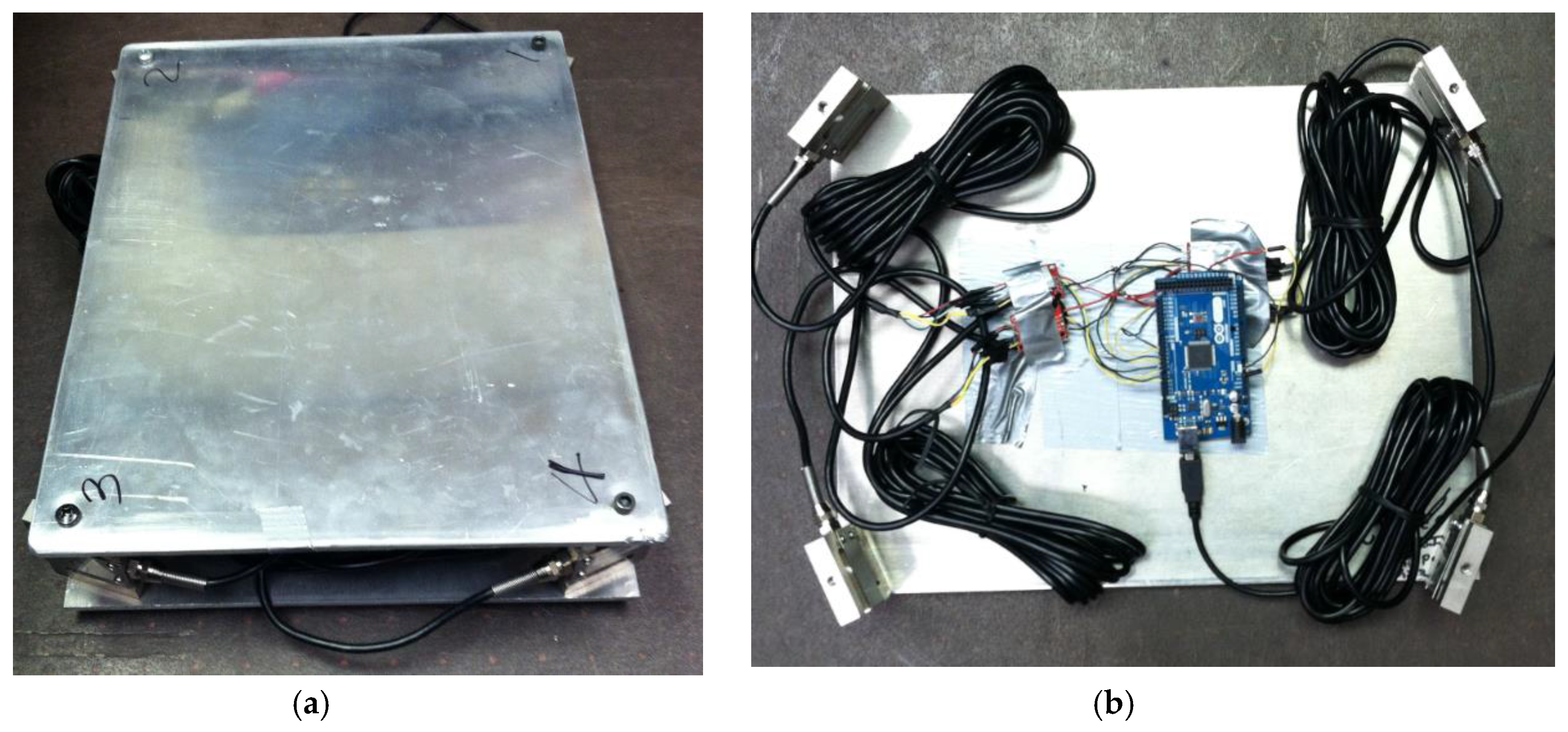
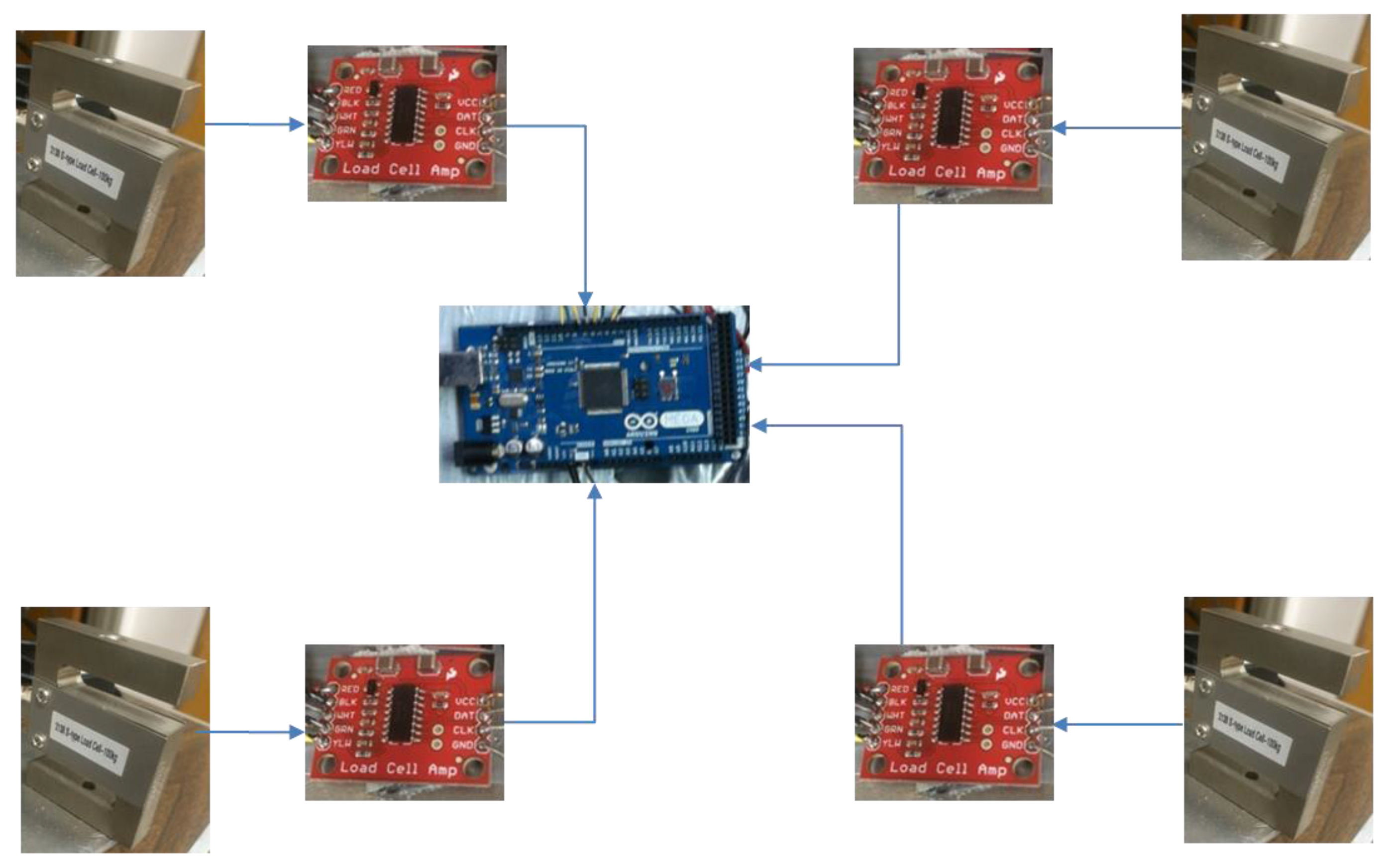
3. Materials and Methods
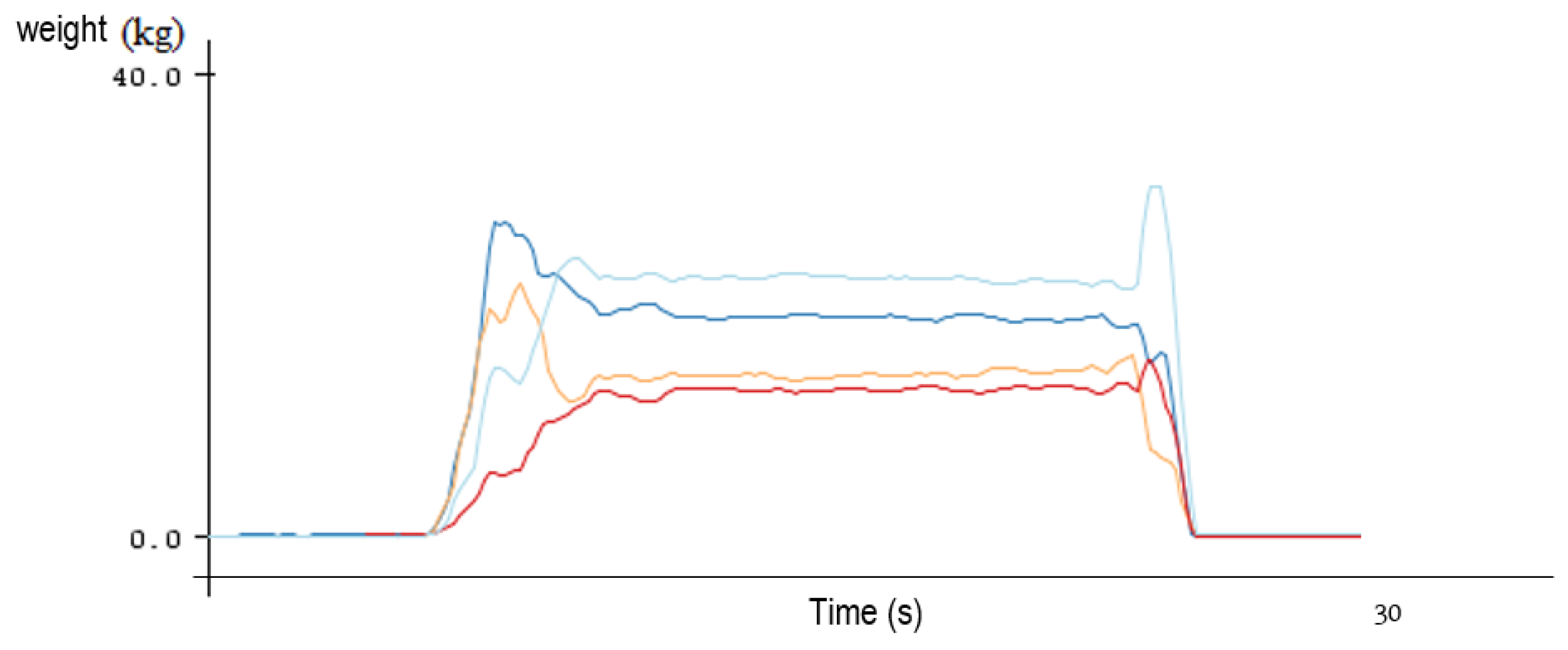
4. Results
5. Discussion
Acknowledgments
Conflicts of Interest
References
- Buckley, T.A.; Oldham, J.R.; Caccese, J.B. Postural control deficits identify post-concussion neurological deficits. J. Sport Health Sci. 2016, 5, 61–69. [Google Scholar] [CrossRef]
- Abrahamova, D.; Hlavacka, F. Age-related changes of human balance during quiet stance. Physiol. Res. 2008, 57, 957–964. [Google Scholar] [PubMed]
- Strang, A.J.; DiDomenico, A.T. Postural control: Age-related changes in working-age men. Prof. Safety 2010, 55, 27–32. [Google Scholar]
- Huang, C.; Sue, P.; Abbod, M.F.; Jiang, B.C.; Shieh, J. Measuring center of pressure signals to quantify human balance using multivariate multiscale entropy by designing a force platform. Sensors 2013, 13, 10151–10166. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, J.T.; Mercer, V.S.; Stergiou, N. Approximate entropy detects the effect of a secondary cognitive task on postural control in healthy young adults: A methodological report. J. NeuroEng. Rehabil. 2007, 4, 42. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, J.T.; Guskiewicz, K.M.; Giuliani, C.; Marshall, S.; Mercer, V.; Stergiou, N. Detecting altered postural control after cerebral concussion in athletes with normal postural stability. Br. J. Sports Med. 2005, 39, 805–811. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, J.T.; Guskiewicz, K.M.; Giuliani, C.; Marshall, S.; Mercer, V.S.; Stergiou, N. Recovery of postural control after cerebral concussion: New insights using approximate entropy. J. Athl. Train. 2006, 41, 305–313. [Google Scholar] [PubMed]
- Guskiewicz, K.M.; Riemann, B.; Perrin, D.; Nashner, L. Alternative approaches to the assessment of mild head injury in athletes. Med. Sci. Sports Exerc. 1997, 29, 213–221. [Google Scholar] [CrossRef]
- Guskiewicz, K.M. Balance assessment in the management of sport-related concussion. Clin. Sports Med. 2011, 30, 89–102. [Google Scholar] [CrossRef] [PubMed]
- Riemann, B.L.; Guskiewicz, K.M. Effects of mild head injury on postural stability as measured through clinical balance testing. J. Athl. Train. 2000, 35, 19–25. [Google Scholar] [PubMed]
- Bartlett, R.; Gratton, C.; Rolf, C.G. Encyclopedia of International Sports Studies; Taylor & Francis: New York, NY, USA, 2010. [Google Scholar]
- García, R.B.; Corresa, S.P.; Bertomeu, J.M.B.; Suárez-Varela, M.M.M. Static posturography with dynamic tests. Usefulness of biomechanical parameters in assessing vestibular patients. Acta Otorrinolaringol. Espanola 2012, 63, 332–338. [Google Scholar]
- Gaerlan, M.G. The Role of Visual, Vestibular, and Somatosensory Systems in Postural Balance. Master’s Thesis, University of Nevada Las Vegas, Las Vegas, NV, USA, 2010. [Google Scholar]
- Jáuregui-Renaud, K. Postural Balance and Peripheral Neuropathy; InTech: Rijeka, Croatia, 2013. [Google Scholar]
- Donker, S.F.; Roerdink, M.; Greven, A.J.; Beek, P.J. Regularity of center-of-pressure trajectories depends on the amount of attention invested in postural control. Exp. Brain Res. 2007, 181, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Roerdink, M.; Hlavackova, P.; Vuillerme, N. Center-of-pressure regularity as a marker for attentional investment in postural control: A comparison between sitting and standing postures. Hum. Mov. Sci. 2011, 30, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Lamoth, C.J.C.; van Lummel, R.C.; Beek, P.J. Athletic skill level is reflected in body sway: A test case for accelometry in combination with stochastic dynamics. Gait Posture 2009, 20, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Stins, J.F.; Roerdink, M.; Beek, P.J. To freeze or not to freeze? Affective and cognitive perturbations have markedly different effects on postural control. Hum. Mov. Sci. 2011, 30, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Hasan, S.S.; Lichtenstein, M.J.; Shiavi, R.G. Effect of loss of balance on biomechanics platform measures of sway: Influence of stance and a method for adjustment. J. Biomech. 1990, 23, 783–789. [Google Scholar] [CrossRef]
- Raymakers, J.A.; Samson, M.M.; Verhaar, H.J.J. The assessment of body sway and the choice of the stability parameter(s). Gait Posture 2005, 21, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Pincus, S.M. Approximate entropy as a measure of system complexity. Proc. Natl. Acad. Sci. USA 1991, 88, 2297–2301. [Google Scholar] [CrossRef] [PubMed]
- Richman, J.S.; Moorman, J.R. Physiological time-series analysis using approximate entropy and sample entropy. Am. J. Phys. Heart Circ. Phys. 2000, 278, 2039–2049. [Google Scholar]
- Johnson, M.L.; Brand, L. Numerical Computer Methods; Elsevier: San Diego, CA, USA, 2004; Volume 384. [Google Scholar]
- Yentes, J.M.; Hunt, N.; Schmid, K.K.; Kaipust, J.P.; McGrath, D.; Stergiou, N. The appropriate use of approximate entropy and sample entropy with short data sets. Ann. Biomed. Eng. 2013, 41, 349–365. [Google Scholar] [CrossRef] [PubMed]
- Borg, F.G.; Laxaback, G. Entropy of balance—Some recent results. J. NeuroEng. Rehabil. 2010, 7, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chon, K.H.; Scully, C.G.; Lu, S. Approximate entropy for all signals: Is the recommended threshold value R appropriate? IEEE Eng. Med. Biol. Mag. 2009, 28, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Valle, M.S.; Casabona, A.; Fiumara, A.; Castiglione, D.; Sorge, G.; Cioni, M. Quantitative analysis of upright standing in adult with late-onset Pompe disease. Sci. Rep. 2016, 6, 37040. [Google Scholar] [CrossRef] [PubMed]
- Ghomashchi, H.; Esteki, A.; Nasrabadi, A.M.; Sprott, J.C.; BahrPeymaInt, F. Dynamic patterns of postural fluctuations during quiet standing: A recurrence quantification approach. J. Bifurc. Chaos 2011, 21, 1163–1172. [Google Scholar] [CrossRef]
- Horak, F.B. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing 2006, 35 (Suppl. 2), ii7–ii11. [Google Scholar] [CrossRef] [PubMed]
- Balasubramaniam, R.; Riley, M.A.; Turvey, M.T. Specificity of postural sway to the demands of a precision task. Gait Posture 2000, 11, 12–14. [Google Scholar] [CrossRef]
- Eduardo, L.; Lizama, C.; Pijnappels, M.; Peter Reeves, N.; Verschueren, S.M.P.; van Dieën, J.H. Can explicit visual feedback of postural sway efface the effects of sensory manipulations on mediolateral balance performance? J. Neurophysiol. 2016, 115, 907–914. [Google Scholar]
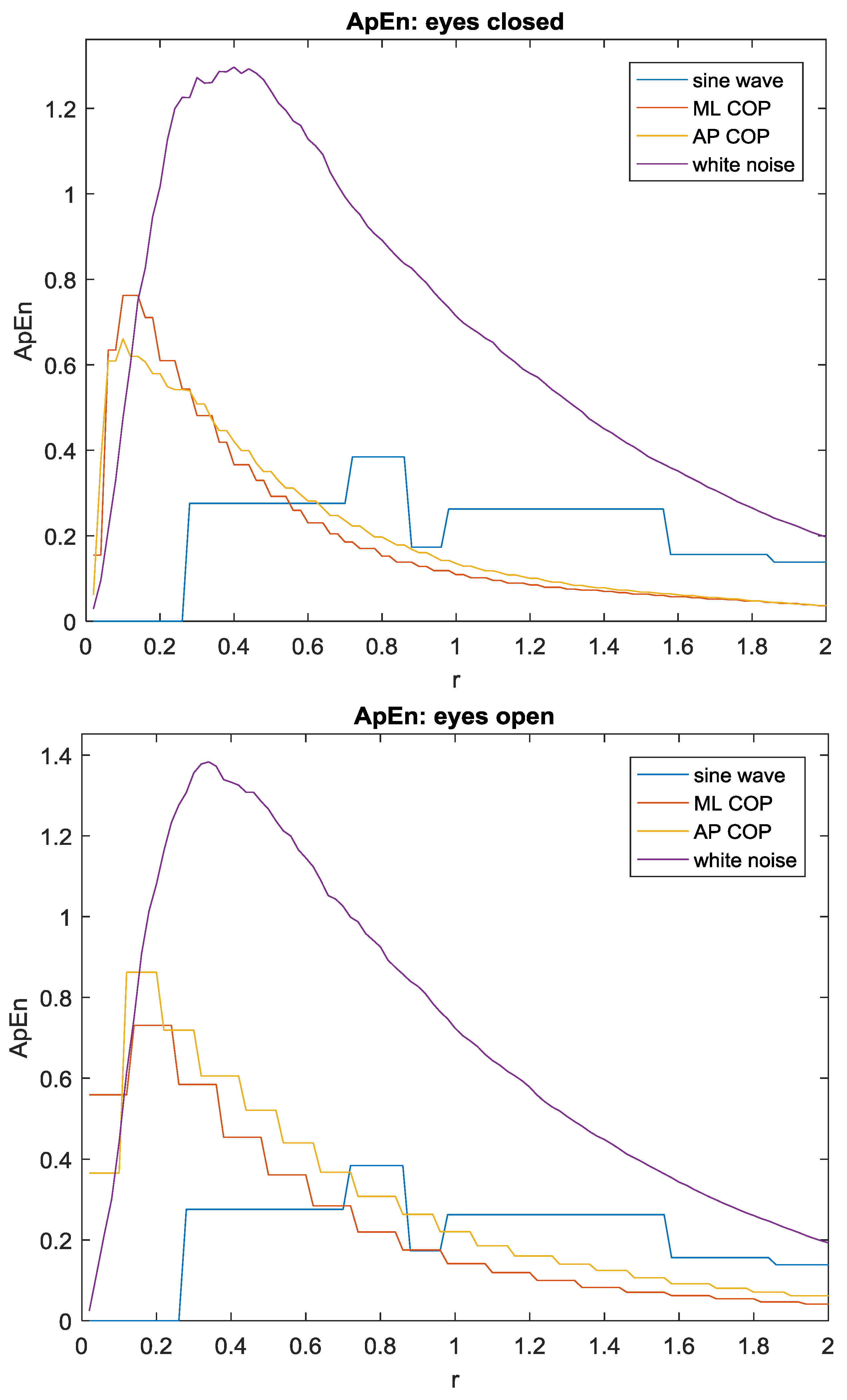
| Direction | Eyes | ApEn |
|---|---|---|
| ML | Closed | 0.64 |
| AP | Closed | 0.55 |
| ML | Open | 0.71 |
| AP | Open | 0.80 |
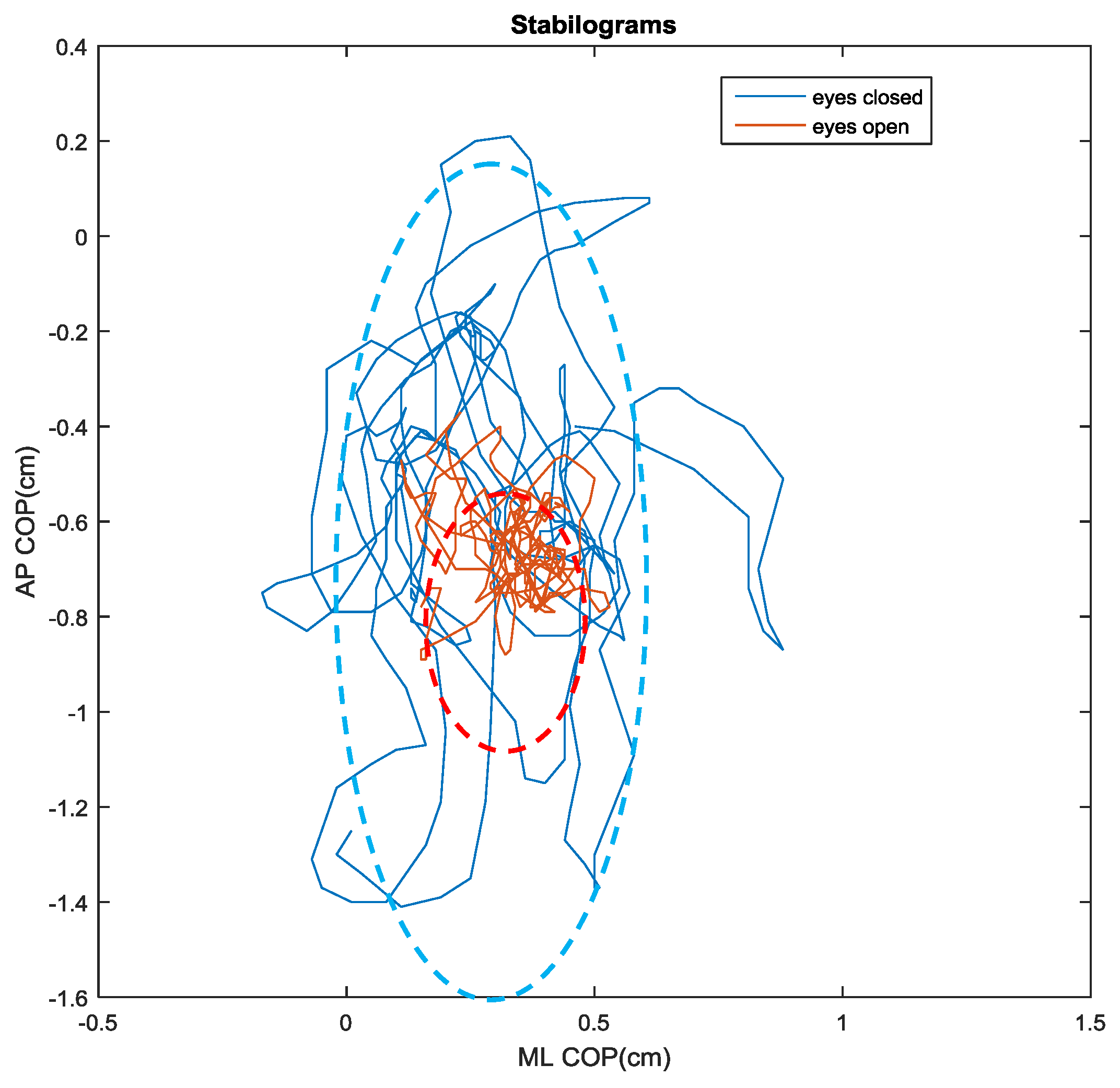
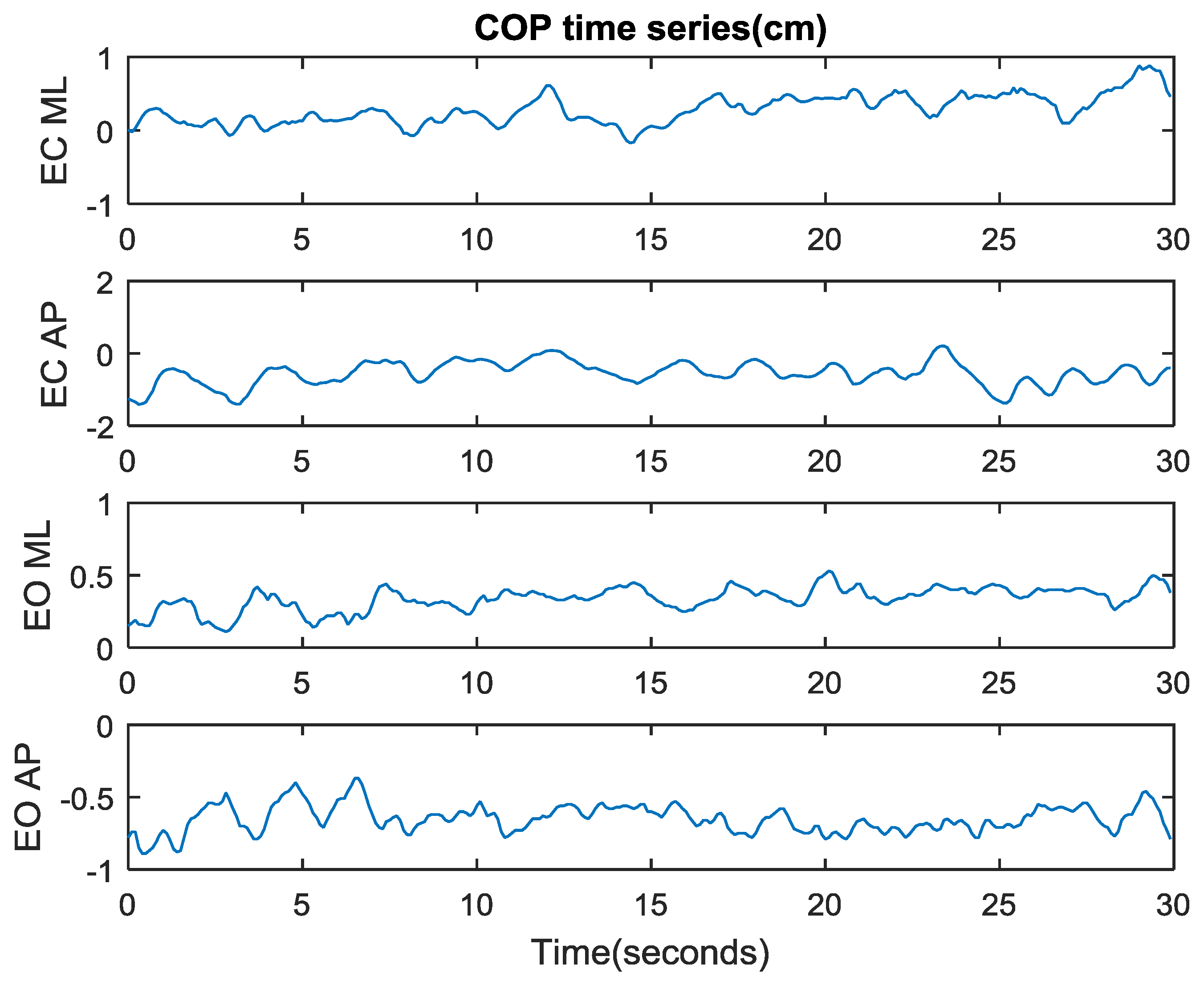
| Direction | Eyes | Maximum (cm) | Minimum (cm) | Range (cm) |
|---|---|---|---|---|
| ML | Open | 0.53 | 0.11 | 0.42 |
| AP | Open | −0.37 | −0.89 | 0.52 |
| ML | Closed | 0.88 | −0.17 | 1.05 |
| AP | Closed | 0.21 | −1.41 | 1.62 |
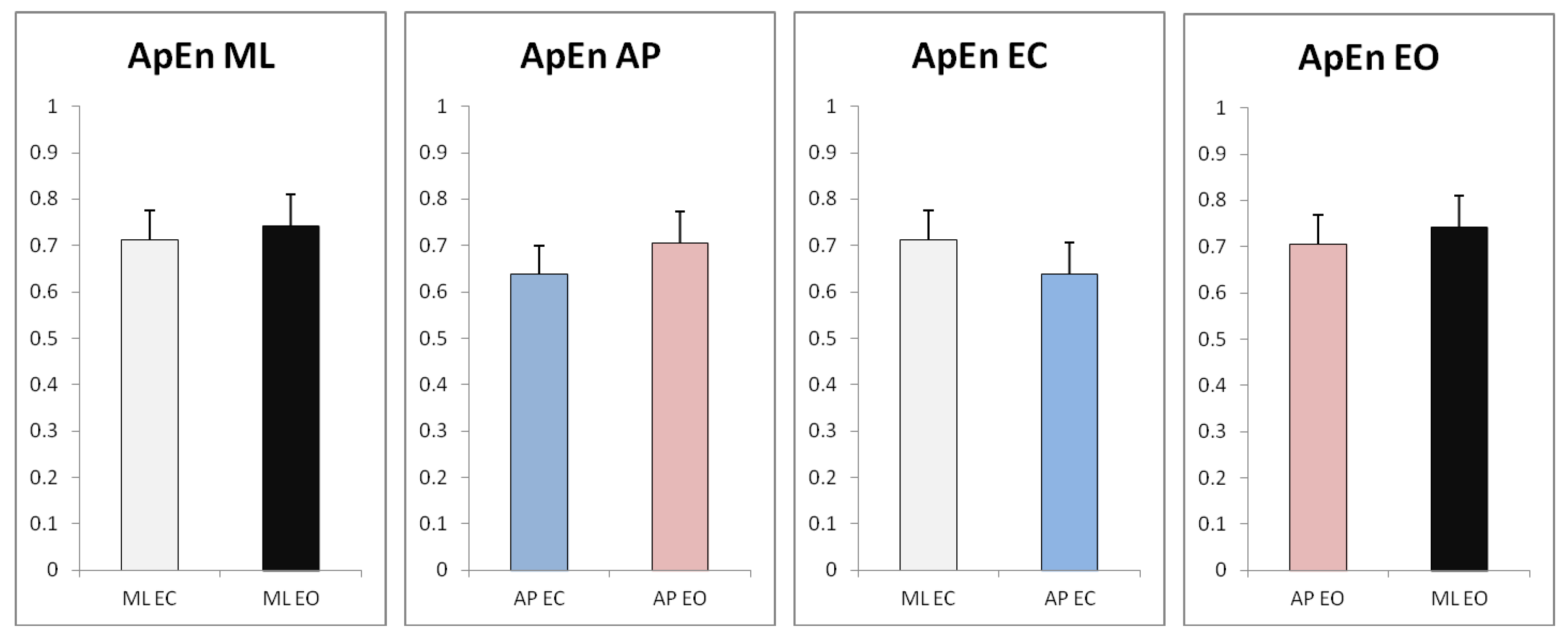
| Direction | Eyes | n | Mean | Standard Deviation |
|---|---|---|---|---|
| ML | Open | 30 | 0.742 | 0.068 |
| AP | Open | 30 | 0.705 | 0.075 |
| ML | Closed | 30 | 0.712 | 0.063 |
| AP | Closed | 30 | 0.637 | 0.054 |
© 2017 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, Y. Design and Validation of a Low-Cost Portable Device to Quantify Postural Stability. Sensors 2017, 17, 619. https://doi.org/10.3390/s17030619
Zhu Y. Design and Validation of a Low-Cost Portable Device to Quantify Postural Stability. Sensors. 2017; 17(3):619. https://doi.org/10.3390/s17030619
Chicago/Turabian StyleZhu, Yong. 2017. "Design and Validation of a Low-Cost Portable Device to Quantify Postural Stability" Sensors 17, no. 3: 619. https://doi.org/10.3390/s17030619






