Inertial Measurement Units for Clinical Movement Analysis: Reliability and Concurrent Validity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Participants and Setting
2.2. Raters
2.3. Experimental Protocol
2.4. Data Collection
2.5. Data Processing
2.6. Data Analysis
2.6.1. Reliability
2.6.2. Concurrent Validity
3. Results
3.1. Demographics and Descriptive
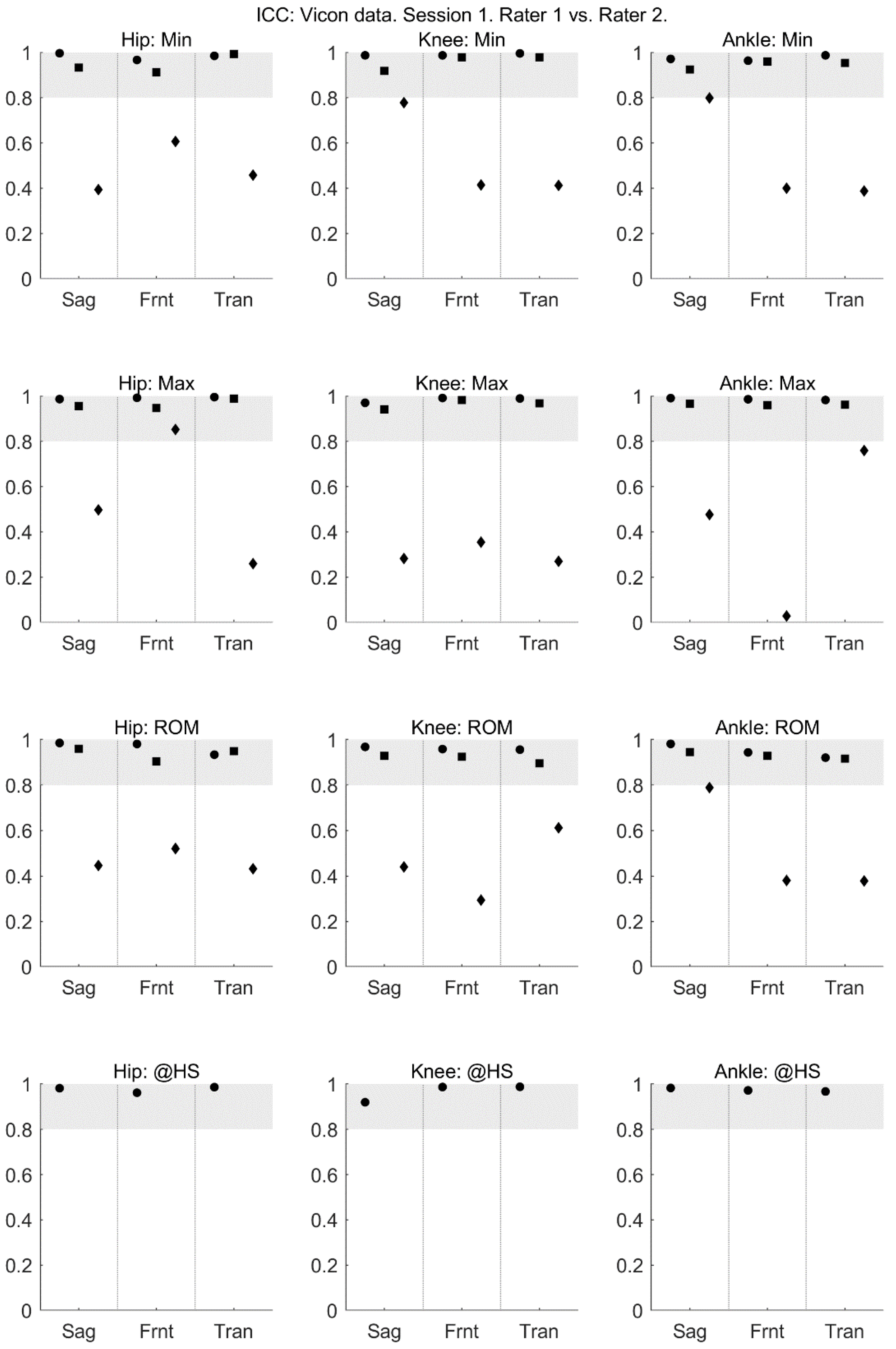
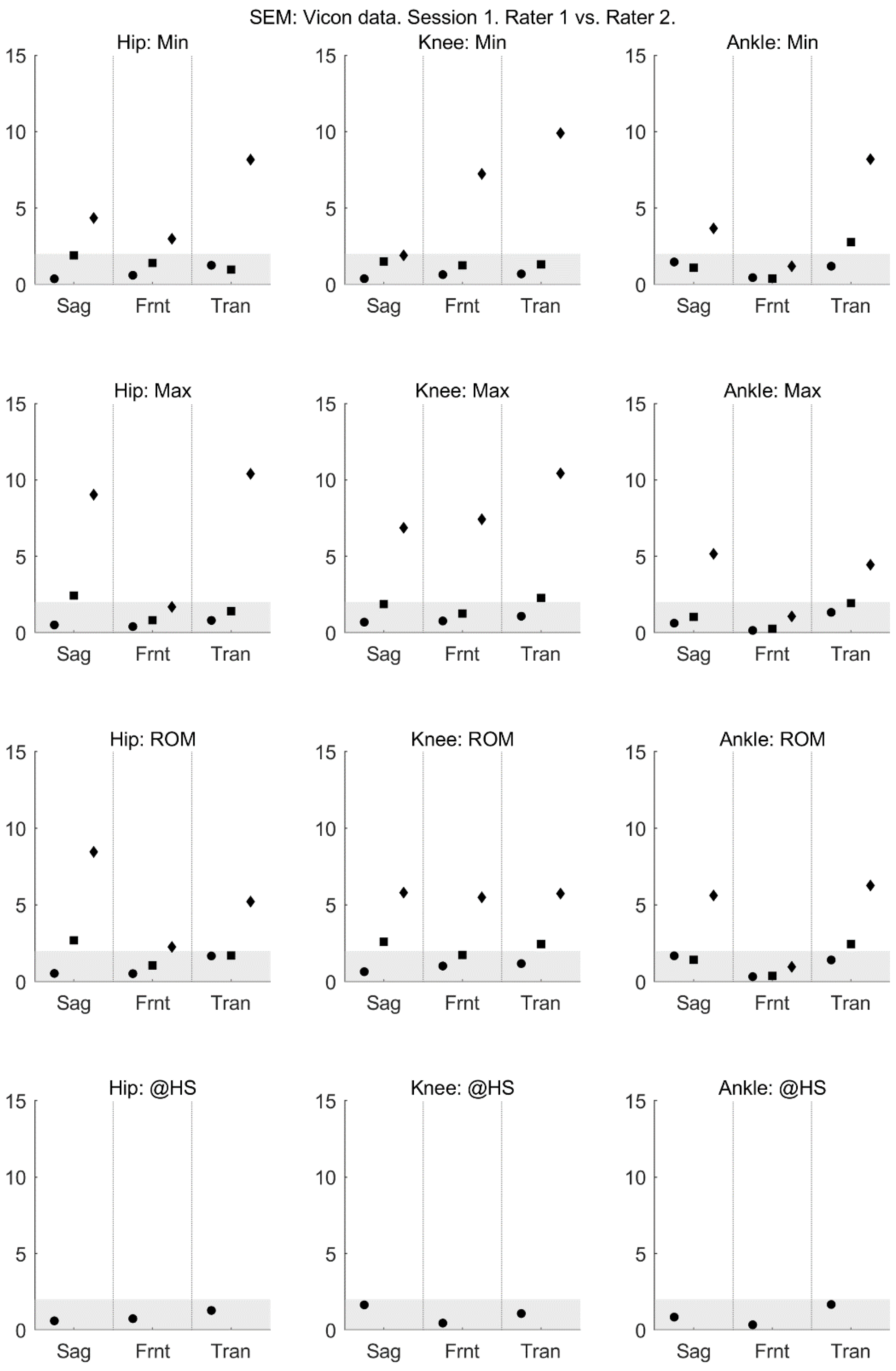
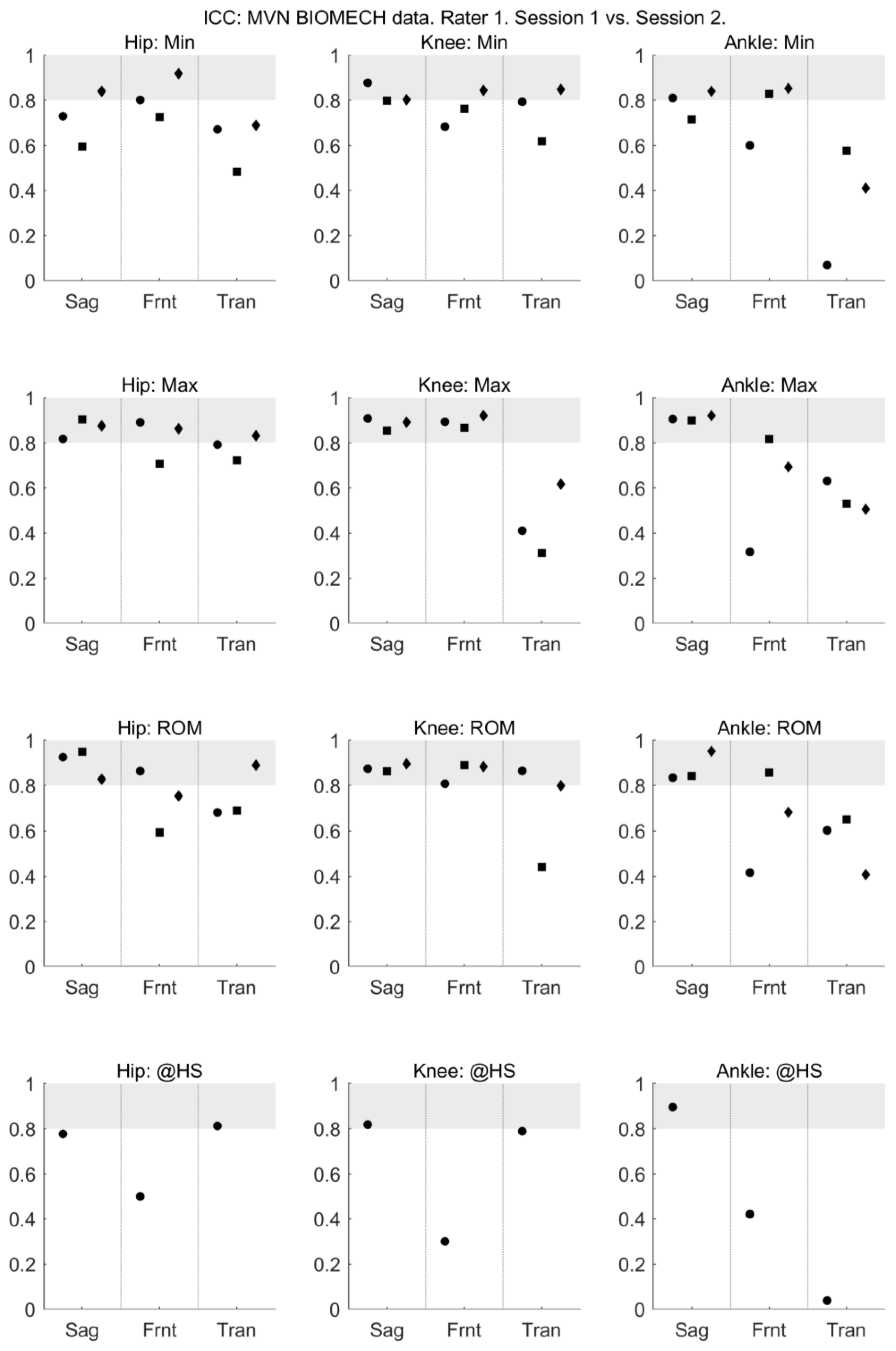
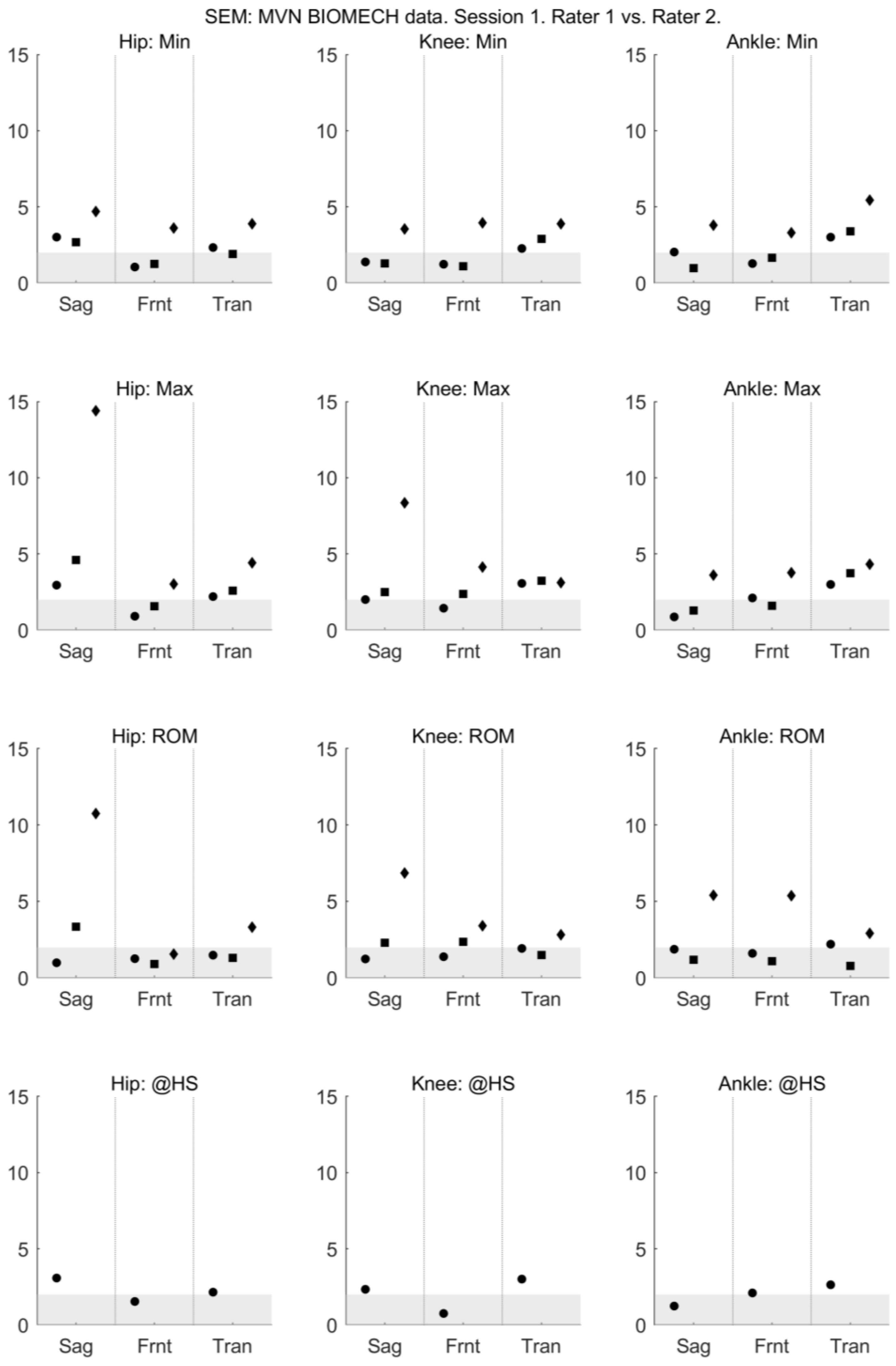
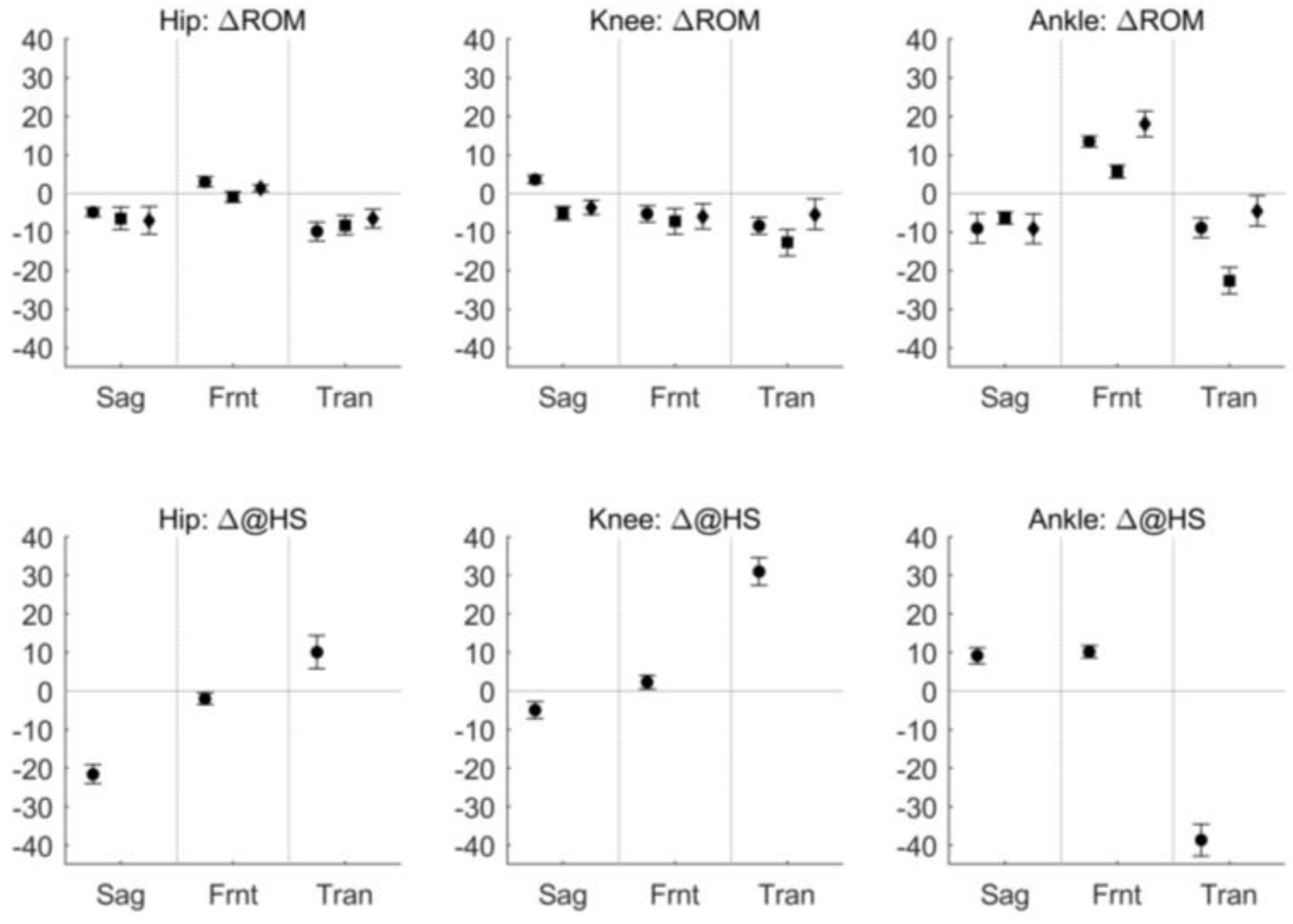
3.2. Reliability
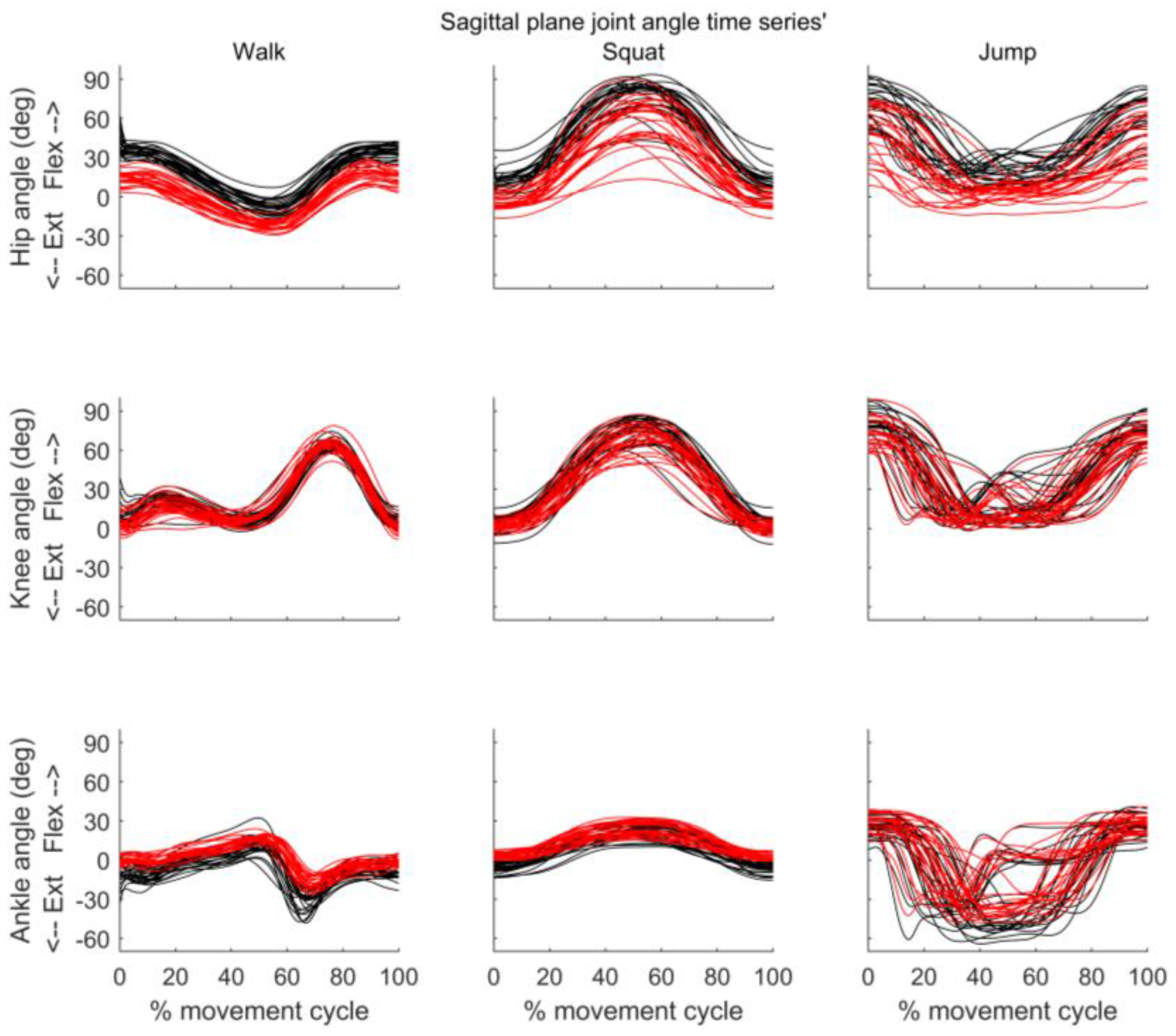
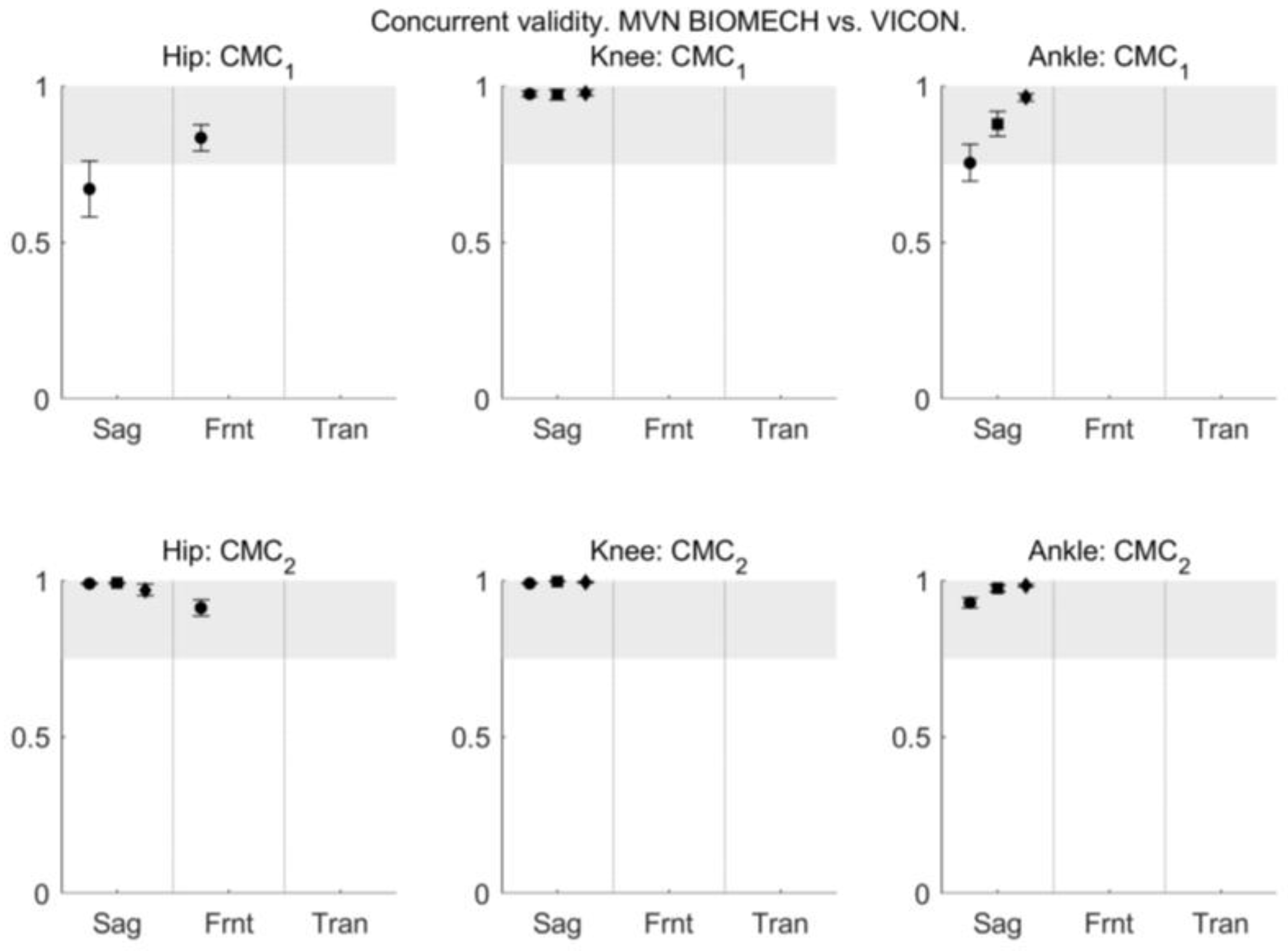
3.3. Concurrent Validity
4. Discussion
4.1. Reliability
4.2. Concurrent Validity
4.3. Limitations
4.4. Clinical Implications and Future Research Directions
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Walk | Squat | Jump | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | ||
| Vicon Hip | Min | −8.8 (6.2) | −9.4 (5.3) | 0.6 [−1.0, 2.2] | 9.1 (7.3) | 8.3 (5.9) | 0.8 [−1.0, 2.6] | 13.8 (5.6) | 14.3 (6.2) | −0.4 [−2.1, 1.2] |
| Max | 36.6 (4.4) | 36.0 (4.1) | 0.6 [−0.8, 2.0] | 79.9 (11.5) | 83.2 (10.8) | −3.3 [−5.7, −0.9] | 71.9 (12.7) | 74.7 (10.1) | −2.7 [−6.7, 1.3] | |
| ROM | 45.4 (4.5) | 45.4 (3.8) | 0.0 [−0.9, 0.9] | 70.8 (13.7) | 74.9 (11.9) | −4.1 [−6.7, −1.5] | 58.1 (11.4) | 60.4 (9.8) | −2.3 [−6.4, 1.8] | |
| @HS | 35.6 (4.4) | 35.0 (4.5) | 0.6 [−0.8, 2.1] | - | - | - | - | - | - | |
| Vicon Knee | Min | 4.2 (3.4) | 2.8 (3.6) | 1.4 [−0.0, 2.8] | 2.2 (5.3) | 0.1 (3.8) | 2.1 [0.6, 3.6] | 5.8 (4.1) | 4.7 (3.9) | 1.2 [−0.7, 3.1] |
| Max | 64.5 (4.0) | 62.9 (4.4) | 1.6 [−0.3, 3.6] | 77.7 (7.7) | 79.2 (9.0) | −1.5 [−4.3, 1.3] | 80.5 (8.1) | 80.8 (5.8) | −0.3 [−3.1, 2.5] | |
| ROM | 60.4 (3.7) | 60.1 (3.4) | 0.3 [−0.8, 1.3] | 75.6 (9.7) | 79.2 (9.0) | −3.6 [−6.9, −0.4] | 74.7 (7.7) | 76.1 (6.2) | −1.4 [−3.8, 0.9] | |
| @HS | 8.5 (5.8) | 7.2 (6.0) | 1.2 [−1.1, 3.5] | - | - | - | - | - | - | |
| Vicon Ankle | Min | −32.3 (8.7) | −33.3 (13.7) | 1.0 [−4.4, 6.3] | −7.1 (4.0) | −10.4 (7.3) | 3.3 [0.5, 6.1] | −51.9 (8.2) | −52.1 (15.3) | 0.2 [−5.1, 5.4] |
| Max | 12.3 (6.5) | 12.6 (9.9) | −0.3 [−3.2, 2.5] | 21.5 (5.6) | 19.6 (6.7) | 1.8 [−0.3, 3.9] | 27.7 (7.1) | 27.4 (9.1) | 0.3 [−2.0, 2.6] | |
| ROM | 44.7 (12.4) | 45.9 (22.6) | −1.3 [−8.6, 6.0] | 28.6 (6.1) | 30.1 (10.9) | −1.5 [−5.4, 2.5] | 79.6 (12.2) | 79.5 (22.6) | 0.1 [−6.9, 7.2] | |
| @HS | −9.1 (6.4) | −10.4 (8.0) | 1.3 [−1.3, 3.9] | - | - | - | - | - | - | |
| Xsens Hip | Min | −21.9 (3.8) | −21.4 (3.7) | −0.6 [−2.0, 0.9] | −5.1 (5.2) | −2.5 (7.0) | −2.6 [−5.4, 0.2] | −1.9 (6.0) | 1.3 (7.3) | −3.2 [−5.4, −1.1] |
| Max | 18.6 (5.8) | 18.7 (6.1) | −0.2 [−2.2, 1.8] | 58.9 (18.0) | 65.9 (15.6) | −6.9 [−11.2, −2.7] | 49.0 (19.9) | 54.1 (17.0) | −5.1 [−10.4, 0.2] | |
| ROM | 40.5 (4.5) | 40.1 (4.8) | 0.4 [−0.7, 1.4] | 64.0 (16.8) | 68.4 (15.2) | −4.3 [−7.3, −1.4] | 50.9 (15.9) | 52.7 (14.0) | −1.9 [−6.8, 3.1] | |
| @HS | 14.3 (5.0) | 14.9 (5.6) | −0.7 [−2.6, 1.3] | - | - | - | - | - | - | |
| Xsens Knee | Min | 0.9 (4.1) | 1.4 (4.2) | −0.5 [−1.6, 0.7] | 0.4 (3.4) | 0.2 (2.6) | 0.2 [−0.9, 1.2] | 2.6 (3.1) | 3.5 (3.2) | −0.9 [−2.0, 0.2] |
| Max | 64.8 (5.3) | 65.1 (5.6) | −0.3 [−1.6, 1.0] | 70.6 (10.3) | 74.4 (9.3) | −3.8 [−6.7, −0.8] | 73.6 (10.6) | 75.8 (9.6) | −2.2 [−4.9, 0.6] | |
| ROM | 63.9 (2.7) | 63.7 (3.3) | 0.2 [−0.7, 1.0] | 70.3 (10.7) | 74.2 (9.8) | −4.0 [−7.0, −0.9] | 71.0 (9.7) | 72.2 (8.3) | −1.3 [−3.7, 1.1] | |
| @HS | 3.7 (6.1) | 4.2 (5.6) | −0.5 [−2.5, 1.4] | - | - | - | - | - | - | |
| Xsens Ankle | Min | −17.7 (5.0) | −17.1 (4.9) | −0.6 [−2.3, 1.1] | 2.5 (2.2) | 1.9 (2.1) | 0.6 [−0.3, 1.4] | −40.0 (5.4) | −39.1 (5.5) | −1.0 [−2.7, 0.8] |
| Max | 17.8 (2.5) | 18.2 (2.6) | −0.4 [−1.0, 0.2] | 24.5 (5.4) | 24.4 (5.4) | 0.1 [−1.2, 1.5] | 30.2 (6.3) | 30.7 (7.0) | −0.5 [−2.1, 1.1] | |
| ROM | 35.6 (5.7) | 35.4 (5.4) | 0.2 [−1.6, 2.0] | 22.0 (5.5) | 22.5 (5.5) | −0.4 [−2.1, 1.3] | 70.2 (9.3) | 69.7 (9.8) | 0.5 [−1.3, 2.3] | |
| @HS | 0.1 (3.2) | 0.1 (3.8) | 0.0 [−0.9, 0.9] | - | - | - | - | - | - | |
| Walk | Squat | Jump | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | ||
| Vicon Hip | Min | −8.2 (3.3) | −8.4 (3.4) | 0.2 [−1.1, 1.5] | −8.0 (4.8) | −8.7 (4.6) | 0.7 [−1.1, 2.5] | −9.2 (4.8) | −9.1 (4.8) | −0.1 [−1.8, 1.6] |
| Max | 7.4 (4.6) | 7.3 (3.6) | 0.0 [−1.3, 1.4] | −1.6 (3.6) | −1.9 (2.8) | 0.3 [−1.1, 1.7] | −2.2 (4.4) | −2.4 (3.6) | 0.3 [−1.3, 1.8] | |
| ROM | 15.6 (3.9) | 15.7 (3.7) | −0.2 [−0.7, 0.4] | 6.4 (3.5) | 6.8 (3.7) | −0.4 [−1.5, 0.8] | 7.0 (3.3) | 6.6 (3.3) | 0.4 [−0.6, 1.3] | |
| @HS | −0.4 (3.8) | −0.6 (3.0) | 0.2 [−1.4, 1.7] | - | - | - | - | |||
| Vicon Knee | Min | −6.5 (5.7) | −5.8 (7.8) | −0.7 [−3.3, 2.0] | −8.7 (8.3) | −6.2 (8.0) | −2.4 [−5.6, 0.7] | −8.3 (9.5) | −6.3 (9.8) | −2.1 [−5.7, 1.6] |
| Max | 8.9 (8.4) | 11.0 (12.0) | −2.1 [−6.4, 2.2] | 7.0 (9.3) | 9.4 (13.1) | −2.4 [−6.7, 1.8] | 6.7 (9.2) | 9.9 (13.7) | −3.1 [−7.4, 1.1] | |
| ROM | 15.4 (5.1) | 16.8 (7.9) | −1.4 [−4.3, 1.5] | 15.6 (6.4) | 15.6 (9.8) | 0.0 [−4.0, 4.1] | 15.1 (6.5) | 16.2 (9.2) | −1.1 [−5.0, 2.8] | |
| @HS | −3.1 (4.0) | −2.0 (4.4) | −1.1 [−2.4, 0.2] | - | - | - | - | |||
| Vicon Ankle | Min | −3.6 (2.3) | −3.9 (3.8) | 0.3 [−1.2, 1.8] | −3.2 (1.9) | −3.4 (3.2) | 0.2 [−1.2, 1.5] | −2.4 (1.5) | −2.5 (2.7) | 0.1 [−1.0, 1.2] |
| Max | −0.9 (1.3) | −0.7 (1.6) | −0.3 [−1.0, 0.4] | −0.8 (1.3) | −0.6 (1.5) | −0.3 [−0.9, 0.3] | −0.6 (1.1) | −0.2 (1.4) | −0.4 [−1.0, 0.2] | |
| ROM | 2.6 (1.4) | 3.2 (2.6) | −0.6 [−1.6, 0.4] | 2.4 (1.4) | 2.9 (2.3) | −0.4 [−1.4, 0.6] | 1.8 (1.2) | 2.3 (2.0) | −0.5 [−1.4, 0.4] | |
| @HS | −2.8 (2.1) | −3.0 (2.9) | 0.2 [−1.0, 1.4] | - | - | - | - | |||
| Xsens Hip | Min | −9.3 (3.0) | −9.7 (2.6) | 0.3 [−0.6, 1.3] | −5.5 (3.5) | −6.3 (3.9) | 0.8 [−0.6, 2.3] | −8.7 (4.1) | −9.6 (4.4) | 0.9 [−0.1, 1.9] |
| Max | 9.2 (2.7) | 9.1 (2.4) | 0.1 [−0.5, 0.8] | 0.0 (3.6) | −0.5 (3.0) | 0.6 [−0.8, 1.9] | −0.3 (4.1) | −1.0 (4.0) | 0.7 [−0.5, 1.9] | |
| ROM | 18.6 (3.8) | 18.8 (3.0) | −0.2 [−1.2, 0.8] | 5.5 (2.3) | 5.7 (2.3) | −0.3 [−1.3, 0.8] | 8.5 (2.7) | 8.6 (2.6) | −0.2 [−1.2, 0.9] | |
| @HS | −2.3 (3.5) | −2.9 (3.5) | 0.6 [−1.1, 2.3] | - | - | - | - | |||
| Xsens Knee | Min | −4.6 (3.2) | −4.2 (3.5) | −0.3 [−1.7, 1.1] | −2.9 (2.8) | −3.5 (2.8) | 0.6 [−0.5, 1.6] | −4.8 (4.7) | −4.6 (4.2) | −0.1 [−1.6, 1.3] |
| Max | 5.2 (5.6) | 5.8 (5.0) | −0.6 [−1.9, 0.8] | 5.3 (5.9) | 4.8 (5.6) | 0.5 [−1.2, 2.2] | 4.3 (5.6) | 4.6 (5.5) | −0.3 [−1.6, 1.0] | |
| ROM | 9.8 (4.1) | 10.0 (3.8) | −0.2 [−1.6, 1.1] | 8.2 (4.5) | 8.2 (4.4) | −0.1 [−1.2, 1.1] | 9.0 (3.8) | 9.2 (4.6) | −0.2 [−1.3, 1.0] | |
| @HS | −1.0 (1.4) | −0.5 (1.9) | −0.5 [−1.4, 0.4] | - | - | - | - | |||
| Xsens Ankle | Min | −3.6 (2.9) | −3.6 (2.7) | −0.1 [−1.3, 1.2] | −3.6 (5.3) | −2.1 (5.9) | −1.4 [−3.2, 0.4] | −3.7 (5.0) | −4.0 (4.3) | 0.3 [−1.2, 1.7] |
| Max | 12.4 (3.7) | 13.2 (4.7) | −0.8 [−3.1, 1.5] | 4.6 (4.1) | 5.9 (4.2) | −1.3 [−2.7, 0.1] | 15.8 (5.2) | 14.8 (5.0) | 1.1 [−1.1, 3.2] | |
| ROM | 16.0 (3.1) | 16.8 (4.6) | −0.8 [−2.8, 1.3] | 8.1 (3.8) | 8.0 (3.7) | 0.1 [−1.0, 1.3] | 19.5 (7.7) | 18.8 (7.5) | 0.8 [−2.4, 4.0] | |
| @HS | 7.3 (3.3) | 7.1 (3.4) | 0.2 [−1.5, 2.0] | - | - | - | - | |||
| Walk | Squat | Jump | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | ||
| Vicon Hip | Min | −14.8 (10.2) | −10.4 (12.4) | −4.4 [−9.2, 0.3] | −14.9 (11.2) | −9.2 (13.2) | −5.6 [−10.6, −0.7] | −15.7 (11.1) | −11.2 (14.5) | −4.5 [−9.7, 0.6] |
| Max | 7.4 (12.0) | 9.7 (15.3) | −2.2 [−8.9, 4.4] | 1.5 (13.0) | 5.2 (13.5) | −3.7 [−9.9, 2.5] | 2.1 (12.1) | 5.1 (15.7) | −3.0 [−9.1, 3.1] | |
| ROM | 22.2 (6.6) | 20.0 (7.3) | 2.2 [−1.7, 6.1] | 16.4 (7.7) | 14.5 (4.8) | 1.9 [−0.8, 4.7] | 17.8 (6.9) | 16.2 (6.5) | 1.6 [−0.9, 4.0] | |
| @HS | −12.1 (11.0) | −7.2 (13.7) | −5.0 [−10.2, 0.3] | - | - | - | - | |||
| Vicon Knee | Min | −44.5 (10.5) | −46.8 (11.4) | 2.3 [−2.7, 7.4] | −35.8 (8.9) | −40.0 (9.2) | 4.2 [0.3, 8.2] | −34.2 (12.9) | −35.0 (11.5) | 0.8 [−4.5, 6.1] |
| Max | −22.0 (10.4) | −20.4 (12.9) | −1.6 [−6.1, 2.9] | −15.6 (12.6) | −12.3 (14.4) | −3.3 [−8.3, 1.8] | −16.0 (12.2) | −13.8 (17.0) | −2.2 [−8.2, 3.8] | |
| ROM | 22.5 (5.7) | 26.4 (8.4) | −3.9 [−6.8, −1.0] | 20.2 (7.6) | 27.7 (14.0) | −7.5 [−12.0, −3.0] | 18.3 (9.2) | 21.2 (12.3) | −3.0 [−7.3, 1.4] | |
| @HS | −35.8 (9.8) | −38.8 (9.8) | 3.0 [−0.8, 6.8] | - | - | - | - | |||
| Vicon Ankle | Min | 12.6 (10.5) | 8.1 (15.2) | 4.5 [−0.7, 9.7] | 9.5 (12.9) | 6.6 (16.2) | 2.9 [−2.5, 8.2] | 6.1 (10.5) | 2.0 (14.7) | 4.2 [−0.6, 8.9] |
| Max | 40.9 (10.1) | 39.0 (14.0) | 1.8 [−2.9, 6.6] | 37.2 (9.8) | 35.7 (13.7) | 1.5 [−3.3, 6.3] | 28.9 (9.1) | 26.6 (13.5) | 2.3 [−2.3, 6.8] | |
| ROM | 28.3 (5.1) | 30.9 (6.4) | −2.6 [−5.2, −0.1] | 27.7 (8.5) | 29.1 (10.1) | −1.4 [−4.8, 2.1] | 22.8 (7.9) | 24.7 (9.4) | −1.9 [−4.3, 0.5] | |
| @HS | 35.3 (9.3) | 33.1 (14.2) | 2.2 [−2.2, 6.7] | - | - | - | - | |||
| Xsens Hip | Min | −6.7 (3.9) | −6.8 (4.2) | 0.2 [−1.5, 1.9] | −2.9 (3.7) | −5.0 (4.8) | 2.1 [−0.0, 4.2] | −9.8 (4.4) | −10.5 (4.3) | 0.7 [−1.1, 2.6] |
| Max | 5.7 (4.5) | 5.4 (4.5) | 0.3 [−1.2, 1.9] | 5.0 (4.6) | 3.5 (5.3) | 1.5 [−0.4, 3.5] | 1.3 (5.2) | 0.9 (4.8) | 0.4 [−1.3, 2.0] | |
| ROM | 12.4 (2.7) | 12.2 (3.6) | 0.2 [−1.2, 1.5] | 7.9 (3.3) | 8.5 (3.0) | −0.6 [−1.9, 0.7] | 11.0 (3.6) | 11.4 (4.0) | −0.4 [−1.4, 0.7] | |
| @HS | −2.7 (4.6) | −2.0 (5.2) | −0.7 [−2.4, 0.9] | - | - | - | - | |||
| Xsens Knee | Min | −11.1 (4.8) | −12.1 (3.8) | 1.0 [−0.6, 2.5] | −2.3 (3.8) | −3.1 (2.8) | 0.8 [−0.7, 2.3] | −7.4 (4.7) | −8.2 (4.7) | 0.7 [−0.8, 2.2] |
| Max | 3.0 (4.0) | 1.9 (2.7) | 1.1 [−0.7, 2.8] | 4.8 (4.8) | 4.4 (3.4) | 0.4 [−1.8, 2.7] | 5.0 (4.2) | 4.8 (4.3) | 0.2 [−1.7, 2.1] | |
| ROM | 14.2 (3.8) | 14.0 (3.4) | 0.1 [−0.9, 1.2] | 7.1 (2.6) | 7.5 (2.4) | −0.4 [−1.6, 0.9] | 12.5 (3.2) | 13.0 (4.1) | −0.5 [−1.8, 0.8] | |
| @HS | −4.7 (5.8) | −6.0 (5.1) | 1.3 [−0.6, 3.2] | - | - | - | - | |||
| Xsens Ankle | Min | −6.4 (5.0) | −6.7 (3.7) | 0.3 [−2.2, 2.9] | −4.9 (5.7) | −5.4 (5.5) | 0.5 [−2.1, 3.1] | −5.1 (4.1) | −4.2 (6.2) | −0.9 [−3.6, 1.9] |
| Max | 13.1 (5.4) | 14.1 (5.4) | −0.9 [−3.3, 1.5] | 0.4 (5.7) | −0.0 (5.2) | 0.4 [−2.2, 3.0] | 13.3 (4.2) | 13.2 (6.2) | 0.2 [−2.5, 2.8] | |
| ROM | 19.5 (4.0) | 20.8 (4.5) | −1.2 [−3.2, 0.7] | 5.3 (1.6) | 5.4 (2.1) | −0.1 [−0.9, 0.7] | 18.4 (3.6) | 17.4 (3.8) | 1.0 [−0.9, 3.0] | |
| @HS | −3.0 (4.3) | −3.0 (2.8) | −0.0 [−2.2, 2.1] | - | - | - | - | |||
| Walk | Squat | Jump | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | ||
| Vicon Hip | Min | −8.7 (6.1) | −8.5 (6.3) | −0.2 [−0.5, 0.1] | 9.4 (7.4) | 8.9 (6.9) | 0.5 [−0.9, 2.0] | 13.8 (5.5) | 13.8 (5.7) | −0.0 [−0.9, 0.8] |
| Max | 36.7 (4.3) | 36.6 (4.7) | 0.1 [−0.3, 0.5] | 80.2 (11.4) | 80.6 (10.8) | −0.3 [−2.2, 1.6] | 72.8 (13.2) | 72.2 (12.9) | 0.7 [−1.6, 2.9] | |
| ROM | 45.4 (4.4) | 45.1 (4.5) | 0.3 [−0.1, 0.8] | 70.8 (13.4) | 71.7 (13.1) | −0.9 [−3.0, 1.3] | 59.0 (12.0) | 58.3 (12.4) | 0.7 [−1.4, 2.9] | |
| @HS | 35.7 (4.4) | 35.9 (4.8) | −0.2 [−0.7, 0.4] | - | - | - | - | |||
| Vicon Knee | Min | 4.1 (3.3) | 3.9 (3.5) | 0.2 [−0.1, 0.5] | 2.3 (5.3) | 1.7 (4.2) | 0.6 [−0.5, 1.7] | 5.6 (4.1) | 6.0 (4.8) | −0.4 [−1.7, 0.9] |
| Max | 64.6 (3.9) | 64.3 (4.0) | 0.3 [−0.3, 0.8] | 78.0 (7.7) | 77.6 (7.8) | 0.4 [−1.1, 1.8] | 81.3 (8.9) | 80.0 (8.3) | 1.3 [−0.6, 3.3] | |
| ROM | 60.4 (3.6) | 60.4 (3.7) | 0.1 [−0.5, 0.6] | 75.7 (9.5) | 75.9 (8.6) | −0.3 [−2.2, 1.7] | 75.7 (8.9) | 73.9 (8.0) | 1.7 [−0.1, 3.6] | |
| @HS | 8.3 (5.7) | 8.3 (5.8) | 0.1 [−1.2, 1.4] | - | - | - | - | |||
| Vicon Ankle | Min | −32.3 (8.5) | −32.0 (8.6) | −0.3 [−1.5, 0.9] | −7.1 (3.9) | −7.6 (4.3) | 0.5 [−0.4, 1.4] | −51.9 (8.0) | −50.6 (9.4) | −1.4 [−3.6, 0.9] |
| Max | 12.2 (6.5) | 12.2 (6.3) | −0.1 [−0.6, 0.5] | 21.3 (5.6) | 21.1 (5.9) | 0.3 [−0.6, 1.1] | 27.3 (7.2) | 28.0 (7.1) | −0.7 [−1.6, 0.1] | |
| ROM | 44.4 (12.2) | 44.2 (11.7) | 0.2 [−1.1, 1.5] | 28.5 (6.0) | 28.7 (6.3) | −0.2 [−1.4, 1.0] | 79.2 (12.1) | 78.6 (13.3) | 0.6 [−1.2, 2.5] | |
| @HS | −9.2 (6.3) | −9.4 (6.7) | 0.2 [−0.5, 1.0] | - | - | - | - | |||
| Xsens Hip | Min | −22.1 (3.8) | −20.8 (3.4) | −1.2 [−3.1, 0.6] | −5.0 (5.1) | −4.6 (5.1) | −0.4 [−2.3, 1.6] | −2.0 (5.9) | −0.8 (6.0) | −1.2 [−3.2, 0.8] |
| Max | 18.5 (5.7) | 19.3 (4.7) | −0.8 [−2.8, 1.1] | 59.3 (17.8) | 61.5 (14.5) | −2.2 [−5.6, 1.1] | 50.0 (20.1) | 51.3 (17.5) | −1.3 [−5.5, 3.0] | |
| ROM | 40.5 (4.5) | 40.1 (5.2) | 0.4 [−0.4, 1.3] | 64.3 (16.5) | 66.2 (16.3) | −1.8 [−4.5, 0.8] | 52.1 (16.6) | 52.1 (15.7) | −0.1 [−3.1, 2.9] | |
| @HS | 14.1 (5.0) | 15.1 (3.9) | −0.9 [−2.8, 1.0] | - | - | - | - | |||
| Xsens Knee | Min | 0.6 (4.2) | 0.9 (3.7) | −0.3 [−1.3, 0.7] | 0.4 (3.3) | 0.5 (3.7) | −0.1 [−1.2, 0.9] | 2.3 (3.5) | 2.8 (3.9) | −0.5 [−1.9, 0.8] |
| Max | 64.7 (5.2) | 64.6 (5.1) | 0.1 [−1.4, 1.6] | 70.9 (10.1) | 71.3 (9.9) | −0.4 [−2.4, 1.7] | 74.3 (10.9) | 72.8 (10.1) | 1.5 [−1.4, 4.3] | |
| ROM | 64.0 (2.8) | 63.7 (3.6) | 0.3 [−0.8, 1.4] | 70.5 (10.5) | 70.7 (10.5) | −0.2 [−2.1, 1.6] | 72.0 (10.8) | 70.0 (10.0) | 2.0 [−0.8, 4.8] | |
| @HS | 3.4 (6.2) | 3.6 (5.2) | −0.2 [−1.8, 1.4] | - | - | - | - | |||
| Xsens Ankle | Min | −17.8 (4.9) | −20.3 (5.2) | 2.5 [0.9, 4.1] | 2.3 (2.3) | 1.7 (2.8) | 0.6 [−0.3, 1.4] | −40.3 (5.5) | −41.6 (6.6) | 1.3 [−0.6, 3.1] |
| Max | 17.6 (2.6) | 17.3 (3.0) | 0.4 [−0.4, 1.1] | 24.4 (5.3) | 22.7 (5.9) | 1.7 [0.6, 2.7] | 29.8 (6.4) | 29.3 (6.7) | 0.5 [−0.7, 1.7] | |
| ROM | 35.4 (5.6) | 37.6 (5.5) | −2.2 [−3.6, −0.7] | 22.1 (5.4) | 21.0 (5.5) | 1.1 [0.1, 2.1] | 70.1 (9.1) | 70.9 (10.8) | −0.8 [−2.9, 1.3] | |
| @HS | 0.0 (3.2) | −2.4 (3.5) | 2.4 [1.4, 3.5] | - | - | - | - | |||
| Walk | Squat | Jump | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | ||
| Vicon Hip | Min | −8.1 (3.3) | −8.0 (3.4) | −0.0 [−0.5, 0.5] | −8.1 (4.7) | −9.2 (5.3) | 1.1 [−0.1, 2.2] | −9.4 (4.7) | −10.0 (4.3) | 0.6 [−0.1, 1.3] |
| Max | 7.4 (4.5) | 7.5 (4.4) | −0.1 [−0.4, 0.2] | −1.6 (3.6) | −1.9 (3.4) | 0.3 [−0.3, 1.0] | −2.1 (4.3) | −2.0 (4.0) | −0.1 [−0.7, 0.6] | |
| ROM | 15.5 (3.8) | 15.5 (3.7) | −0.1 [−0.5, 0.4] | 6.5 (3.4) | 7.2 (3.7) | −0.7 [−1.6, 0.1] | 7.3 (3.5) | 8.0 (3.7) | −0.7 [−1.6, 0.2] | |
| @HS | −0.4 (3.7) | −0.7 (3.6) | 0.3 [−0.3, 0.9] | - | - | - | - | |||
| Vicon Knee | Min | −6.7 (5.6) | −6.5 (5.4) | −0.2 [−0.7, 0.3] | −8.9 (8.2) | −8.6 (8.6) | −0.3 [−1.4, 0.7] | −8.6 (9.4) | −8.3 (8.8) | −0.3 [−1.4, 0.7] |
| Max | 8.4 (8.6) | 7.7 (8.7) | 0.6 [0.0, 1.3] | 6.4 (9.5) | 6.3 (9.8) | 0.1 [−1.0, 1.1] | 6.3 (9.3) | 6.3 (9.3) | 0.0 [−1.0, 1.0] | |
| ROM | 15.1 (5.2) | 14.2 (5.1) | 0.8 [−0.0, 1.6] | 15.3 (6.5) | 14.9 (7.4) | 0.4 [−1.1, 1.9] | 14.9 (6.4) | 14.6 (6.3) | 0.3 [−0.7, 1.4] | |
| @HS | −3.3 (3.9) | −3.0 (3.8) | −0.3 [−0.7, 0.1] | - | - | - | - | |||
| Vicon Ankle | Min | −3.6 (2.3) | −3.6 (2.5) | 0.1 [−0.3, 0.5] | −3.2 (1.9) | −3.3 (2.0) | 0.1 [−0.2, 0.4] | −2.4 (1.5) | −2.6 (1.8) | 0.2 [−0.2, 0.7] |
| Max | −0.9 (1.3) | −1.0 (1.4) | 0.0 [−0.1, 0.2] | −0.8 (1.3) | −1.0 (1.4) | 0.2 [−0.1, 0.4] | −0.6 (1.1) | −0.9 (1.1) | 0.3 [−0.2, 0.9] | |
| ROM | 2.6 (1.4) | 2.7 (1.5) | −0.0 [−0.3, 0.2] | 2.4 (1.4) | 2.3 (1.2) | 0.1 [−0.2, 0.4] | 1.8 (1.2) | 1.7 (1.0) | 0.1 [−0.2, 0.4] | |
| @HS | −2.8 (2.0) | −2.9 (2.0) | 0.0 [−0.2, 0.3] | - | - | - | - | |||
| Xsens Hip | Min | −9.2 (3.0) | −9.6 (3.6) | 0.4 [−0.5, 1.3] | −5.7 (3.6) | −7.0 (4.6) | 1.2 [0.1, 2.4] | −9.0 (4.3) | −9.7 (4.3) | 0.6 [−0.4, 1.6] |
| Max | 9.2 (2.7) | 9.0 (3.0) | 0.2 [−0.5, 1.0] | −0.2 (3.6) | −0.7 (4.1) | 0.6 [−0.7, 1.8] | −0.3 (4.0) | −0.8 (4.1) | 0.5 [−0.7, 1.7] | |
| ROM | 18.4 (3.8) | 18.6 (3.5) | −0.1 [−1.1, 0.8] | 5.6 (2.3) | 6.3 (2.5) | −0.7 [−1.5, 0.1] | 8.7 (2.9) | 8.8 (2.8) | −0.1 [−0.8, 0.5] | |
| @HS | −2.4 (3.4) | −3.8 (3.7) | 1.4 [0.2, 2.6] | - | - | - | - | |||
| Xsens Knee | Min | −4.5 (3.2) | −3.0 (2.6) | −1.4 [−2.3, −0.6] | −2.8 (2.8) | −1.9 (2.1) | −0.9 [−1.7, −0.1] | −4.6 (4.7) | −3.3 (3.5) | −1.3 [−2.4, −0.2] |
| Max | 5.3 (5.5) | 7.3 (5.4) | −1.9 [−3.0, −0.8] | 5.3 (5.8) | 5.8 (4.3) | −0.5 [−2.1, 1.0] | 4.4 (5.5) | 5.3 (3.9) | −0.9 [−2.2, 0.4] | |
| ROM | 9.8 (4.1) | 10.3 (4.4) | −0.5 [−1.6, 0.6] | 8.1 (4.4) | 7.7 (3.6) | 0.3 [−1.2, 1.9] | 9.0 (3.7) | 8.6 (2.3) | 0.4 [−0.9, 1.7] | |
| @HS | −0.9 (1.4) | 0.3 (1.4) | −1.2 [−1.8, −0.6] | - | - | - | - | |||
| Xsens Ankle | Min | −3.6 (2.9) | −5.0 (3.1) | 1.4 [0.4, 2.4] | −3.6 (5.2) | −3.5 (5.6) | −0.0 [−1.4, 1.3] | −3.6 (4.9) | −4.2 (4.9) | 0.6 [−0.8, 2.1] |
| Max | 12.5 (3.7) | 12.5 (4.1) | −0.0 [−1.6, 1.5] | 4.6 (4.0) | 4.6 (4.2) | −0.0 [−1.3, 1.3] | 16.2 (5.4) | 16.2 (5.8) | 0.0 [−2.2, 2.2] | |
| ROM | 16.0 (3.0) | 17.4 (3.8) | −1.4 [−2.7, −0.1] | 8.1 (3.7) | 8.1 (3.4) | 0.0 [−0.8, 0.9] | 19.8 (7.6) | 20.4 (6.8) | −0.6 [−3.5, 2.3] | |
| @HS | 7.3 (3.3) | 7.1 (3.3) | 0.2 [−1.2, 1.7] | - | - | - | - | |||
| Walk | Squat | Jump | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | Session 1 | Session 2 | Difference | ||
| Vicon Hip | Min | −15.2 (10.2) | −14.9 (10.2) | −0.3 [−1.4, 0.7] | −15.2 (11.1) | −15.4 (10.8) | 0.2 [−0.6, 1.0] | −16.1 (11.0) | −17.2 (10.7) | 1.2 [−0.4, 2.7] |
| Max | 7.0 (12.0) | 5.9 (12.0) | 1.0 [0.3, 1.7] | 1.0 (13.0) | 0.7 (13.4) | 0.3 [−0.9, 1.4] | 1.6 (12.0) | 1.2 (11.9) | 0.5 [−0.7, 1.6] | |
| ROM | 22.1 (6.4) | 20.8 (5.9) | 1.3 [0.1, 2.6] | 16.1 (7.6) | 16.0 (8.3) | 0.1 [−1.3, 1.5] | 17.7 (6.8) | 18.4 (9.1) | −0.7 [−2.4, 1.0] | |
| @HS | −12.6 (11.0) | −12.5 (11.0) | −0.1 [−1.1, 1.0] | - | - | - | - | |||
| Vicon Knee | Min | −44.2 (10.3) | −43.9 (10.1) | −0.3 [−0.9, 0.3] | −35.5 (8.8) | −36.5 (8.6) | 1.0 [−0.0, 2.1] | −33.9 (12.8) | −32.0 (15.1) | −1.9 [−6.5, 2.8] |
| Max | −21.7 (10.3) | −22.0 (10.7) | 0.3 [−0.6, 1.2] | −15.6 (12.3) | −16.2 (11.6) | 0.7 [−1.1, 2.4] | −15.8 (12.0) | −14.7 (14.3) | −1.1 [−3.3, 1.2] | |
| ROM | 22.5 (5.5) | 21.9 (6.2) | 0.6 [−0.4, 1.6] | 20.0 (7.5) | 20.3 (8.9) | −0.4 [−2.4, 1.7] | 18.1 (9.1) | 17.3 (6.7) | 0.8 [−1.7, 3.4] | |
| @HS | −35.5 (9.8) | −35.9 (9.4) | 0.4 [−0.4, 1.3] | - | - | - | - | |||
| Vicon Ankle | Min | 12.6 (10.3) | 13.2 (10.4) | −0.6 [−1.6, 0.4] | 9.5 (12.6) | 10.9 (12.8) | −1.4 [−3.6, 0.8] | 6.2 (10.3) | 5.3 (13.9) | 0.8 [−1.6, 3.3] |
| Max | 41.1 (9.9) | 41.1 (10.0) | −0.0 [−1.1, 1.0] | 37.3 (9.7) | 37.8 (10.0) | −0.5 [−2.1, 1.1] | 29.2 (9.0) | 27.2 (15.3) | 2.0 [−3.1, 7.0] | |
| ROM | 28.5 (5.0) | 27.9 (4.9) | 0.6 [−0.5, 1.7] | 27.8 (8.3) | 27.0 (8.3) | 0.9 [−1.1, 2.8] | 23.0 (7.8) | 21.8 (6.0) | 1.1 [−1.9, 4.2] | |
| @HS | 35.8 (9.3) | 35.5 (9.4) | 0.2 [−1.1, 1.6] | - | - | - | - | |||
| Xsens Hip | Min | −6.4 (4.1) | −3.7 (3.8) | −2.7 [−4.3, −1.2] | −2.8 (3.6) | −2.5 (3.4) | −0.4 [−1.8, 1.0] | −9.6 (4.4) | −8.6 (4.2) | −1.0 [−2.7, 0.6] |
| Max | 5.9 (4.5) | 7.0 (4.3) | −1.1 [−2.7, 0.4] | 5.0 (4.5) | 5.2 (3.3) | −0.2 [−1.8, 1.5] | 1.5 (5.3) | 2.9 (3.3) | −1.4 [−3.3, 0.6] | |
| ROM | 12.3 (2.7) | 10.7 (2.8) | 1.6 [0.5, 2.7] | 7.9 (3.2) | 7.6 (2.9) | 0.2 [−0.7, 1.2] | 11.1 (3.6) | 11.4 (3.8) | −0.3 [−1.4, 0.7] | |
| @HS | −2.5 (4.6) | 1.7 (4.6) | −4.2 [−5.8, −2.6] | - | - | - | - | |||
| Xsens Knee | Min | −10.9 (4.9) | −13.4 (4.8) | 2.5 [0.9, 4.2] | −2.1 (3.9) | −2.9 (3.5) | 0.8 [−0.9, 2.5] | −7.3 (4.6) | −8.6 (4.9) | 1.2 [−0.6, 3.0] |
| Max | 3.2 (4.0) | 1.4 (3.8) | 1.8 [−0.2, 3.7] | 5.1 (5.0) | 5.3 (4.9) | −0.1 [−2.3, 2.0] | 5.4 (4.4) | 5.3 (4.8) | 0.1 [−1.8, 1.9] | |
| ROM | 14.1 (3.8) | 14.8 (4.2) | −0.8 [−2.2, 0.7] | 7.2 (2.6) | 8.1 (3.2) | −0.9 [−2.1, 0.2] | 12.7 (3.3) | 13.8 (3.9) | −1.1 [−2.3, 0.0] | |
| @HS | −4.5 (5.8) | −8.9 (5.7) | 4.4 [2.2, 6.6] | - | - | - | - | |||
| Xsens Ankle | Min | −6.2 (5.0) | −8.6 (6.0) | 2.5 [0.1, 4.8] | −4.7 (5.6) | −6.2 (6.1) | 1.5 [−1.0, 3.9] | −4.9 (4.1) | −7.0 (6.0) | 2.1 [0.0, 4.2] |
| Max | 13.4 (5.4) | 11.5 (7.4) | 1.9 [−0.6, 4.5] | 0.5 (5.6) | −0.8 (6.2) | 1.3 [−1.3, 4.0] | 13.5 (4.2) | 12.0 (6.9) | 1.5 [−1.2, 4.3] | |
| ROM | 19.5 (4.0) | 20.1 (4.9) | −0.5 [−2.3, 1.2] | 5.2 (1.6) | 5.3 (1.8) | −0.1 [−0.7, 0.5] | 18.4 (3.6) | 19.0 (3.3) | −0.6 [−2.4, 1.2] | |
| @HS | −2.9 (4.3) | −4.3 (5.0) | 1.4 [−0.6, 3.4] | - | - | - | - | |||
Appendix B
References
- Whatman, C.; Hing, W.; Hume, P. Physiotherapist agreement when visually rating movement quality during lower extremity functional screening tests. Phys. Ther. Sport 2012, 13, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Baker, R. Gait analysis methods in rehabilitation. J. Neuroeng. Rehabil. 2006, 3, 4. [Google Scholar] [CrossRef] [PubMed]
- Sabatini, A.M. Variable-state-dimension Kalman-based filter for orientation determination using inertial and magnetic sensors. Sensors 2012, 12, 8491–8506. [Google Scholar] [CrossRef] [PubMed]
- Sabatini, A.M. Kalman-filter-based orientation determination using inertial/magnetic sensors: Observability analysis and performance evaluation. Sensors 2011, 11, 9182–9206. [Google Scholar] [CrossRef] [PubMed]
- Luinge, H.J.; Veltink, P.H. Measuring orientation of human body segments using miniature gyroscopes and accelerometers. Med. Biol. Eng. Comput. 2005, 43, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Favre, J.; Aissaoui, R.; Jolles, B.M.; de Guise, J.A.; Aminian, K. Functional calibration procedure for 3D knee joint angle description using inertial sensors. J. Biomech. 2009, 42, 2330–2335. [Google Scholar] [CrossRef] [PubMed]
- Favre, J.; Jolles, B.M.; Aissaoui, R.; Aminian, K. Ambulatory measurement of 3D knee joint angle. J. Biomech. 2008, 41, 1029–1035. [Google Scholar] [CrossRef] [PubMed]
- Picerno, P.; Cereatti, A.; Cappozzo, A. Joint kinematics estimate using wearable inertial and magnetic sensing modules. Gait Posture 2008, 28, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Inoue, Y.; Shibata, K. Development of a wearable sensor system for quantitative gait analysis. Measurement 2009, 42, 978–988. [Google Scholar] [CrossRef]
- Ferrari, A.; Cutti, A.G.; Garofalo, P.; Raggi, M.; Heijboer, M.; Cappello, A.; Davalli, A. First in vivo assessment of “outwalk”: A novel protocol for clinical gait analysis based on inertial and magnetic sensors. Med. Biol. Eng. Comput. 2010, 48, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Seel, T.; Raisch, J.; Schauer, T. IMU-based joint angle measurement for gait analysis. Sensors 2014, 14, 6891–6909. [Google Scholar] [CrossRef] [PubMed]
- Picerno, P. 25 years of lower limb joint kinematics by using inertial and magnetic sensors: A review of methodological approaches. Gait Posture 2017, 51, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Van Den Noort, J.C.; Ferrari, A.; Cutti, A.G.; Becher, J.G.; Harlaar, J. Gait analysis in children with cerebral palsy via inertial and magnetic sensors. Med. Biol. Eng. Comput. 2013, 51, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Roetenberg, D.; Luinge, H.; Slycke, P. Xsens MVN: Full 6DOF human motion tracking using miniature inertial sensors. Xsens Technol. 2009, 8, 1–7. [Google Scholar]
- Godwin, A.; Agnew, M.; Stevenson, J. Accuracy of Inertial Motion Sensors in Static, Quasistatic, and Complex Dynamic Motion. J. Biomech. Eng. 2009, 131, 114501. [Google Scholar] [CrossRef] [PubMed]
- Lebel, K.; Boissy, P.; Hamel, M.; Duval, C. Inertial measures of motion for clinical biomechanics: Comparative assessment of accuracy under controlled conditions—Changes in accuracy over time. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [PubMed]
- Lebel, K.; Boissy, P.; Hamel, M.; Duval, C. Inertial measures of motion for clinical biomechanics: Comparative assessment of accuracy under controlled conditions—Effect of velocity. PLoS ONE 2013, 8. [Google Scholar] [CrossRef] [PubMed]
- Robert-Lachaine, X.; Mecheri, H.; Larue, C.; Plamondon, A. Validation of inertial measurement units with an optoelectronic system for whole-body motion analysis. Med. Biol. Eng. Comput. 2017, 55, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.T.; Novak, A.C.; Brouwer, B.; Li, Q. Concurrent validation of Xsens MVN measurement of lower limb joint angular kinematics. Physiol. Meas. 2013, 34. [Google Scholar] [CrossRef] [PubMed]
- Walter, S.D.; Eliasziw, M.; Donner, A. Sample size and optimal designs for reliability studies. Stat. Med. 1998, 17, 101–110. [Google Scholar] [CrossRef]
- Xsens Technologies B.V. MVN User Manual: User Guide MVN, MVN BIOMECH MVN Link, MVN Awinda. Available online: https://fccid.io/QILMTW2-3A7G6/User-Manual/Users-Manual-2695756 (accessed on 28 June 2017).
- Vicon Motion System. Plug-in Gait Product Guide—Foundation Notes Revision 2.0. Available online: https://www.vicon.com/downloads/documentation/plug-in-gait-product-guide (accessed on 27 February 2018).
- Wu, G.; Cavanagh, P.R. ISB Recommendations in the Reporting for Standardization of Kinematic Data. J. Biomech. 1995, 28, 1257–1261. [Google Scholar] [CrossRef]
- Grood, E.S.; Suntay, W.J. A Joint Coordinate System for the Clinical Description of Three-Dimensional Motions: Application to the Knee. J. Biomech. Eng. 1983, 105, 136. [Google Scholar] [CrossRef] [PubMed]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wooten, M.E.; Gainey, J.; Gorton, G.; Cochran, G.V.B. Repeatability of Kinematic, Kinetic, and EMG Data in Normal Adult Gait.pdf. J. Orthop. Res. 1989, 7, 849–860. [Google Scholar] [CrossRef] [PubMed]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E. Measurement of lower extremity kinematics during level walking. J. Orthop. Res. 1990, 8, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.B.; Ounpuu, S.; Tyburski, D.; Gage, J.R. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Button, K.; Roos, P.E.; Van Deursen, R.W.M. Activity progression for anterior cruciate ligament injured individuals. Clin. Biomech. 2014, 29, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Roos, P.E.; Button, K.; Van Deursen, R.W.M. Motor control strategies during double leg squat following anterior cruciate ligament rupture and reconstruction: An observational study. J. Neuroeng. Rehabil. 2014, 11. [Google Scholar] [CrossRef] [PubMed]
- Roos, P.E.; Button, K.; Sparkes, V.; van Deursen, R.W.M. Altered biomechanical strategies and medio-lateral control of the knee represent incomplete recovery of individuals with injury during single leg hop. J. Biomech. 2014, 47, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Button, K.; van Deursen, R.; Price, P. Recovery in functional non-copers following anterior cruciate ligament rupture as detected by gait kinematics. Phys. Ther. Sport 2008, 9, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Zeni, J.A.; Richards, J.G.; Higginson, J.S. Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait Posture 2008, 27, 710–714. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; Prinsen, C.A.C.; Bouter, L.M.; de Vet, H.C.W.; Terwee, C.B. The COnsensus-based standards for the selection of health measurement INstruments (COSMIN) and how to select an outcome measurement instrument. Braz. J. Phys. Ther. 2016, 20, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; Terwee, C.B.; Knol, D.L.; Stratford, P.W.; Alonso, J.; Patrick, D.L.; Bouter, L.M.; De Vet, H.C.W. Protocol of the COSMIN study: COnsensus-based Standards for the selection of health Measurement INstruments. BMC Med. Res. Methodol. 2006, 6. [Google Scholar] [CrossRef] [PubMed]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Bruton, A.; Conway, J.H.; Holgate, S.T. Reliability: What is it, and how is it measured? Physiotherapy 2000, 86, 94–99. [Google Scholar] [CrossRef]
- Atkinson, G.; Nevill, A.M. Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sport. Med. 1998, 26, 217–238. [Google Scholar] [CrossRef]
- McGinley, J.L.; Baker, R.; Wolfe, R.; Morris, M.E. The reliability of three-dimensional kinematic gait measurements: A systematic review. Gait Posture 2009, 29, 360–369. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, A.; Cutti, A.G.; Cappello, A. A new formulation of the coefficient of multiple correlation to assess the similarity of waveforms measured synchronously by different motion analysis protocols. Gait Posture 2010, 31, 540–542. [Google Scholar] [CrossRef] [PubMed]
- Røislien, J.; Skare, O.; Opheim, A.; Rennie, L. Evaluating the properties of the coefficient of multiple correlation (CMC) for kinematic gait data. J. Biomech. 2012, 45, 2014–2018. [Google Scholar] [CrossRef] [PubMed]
- Iosa, M.; Cereatti, A.; Merlo, A.; Campanini, I.; Paolucci, S.; Cappozzo, A. Assessment of waveform similarity in clinical gait data: The linear fit method. Biomed Res. Int. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Al-Amri, M.; Al Balushi, H.; Mashabi, A. Intra-rater repeatability of gait parameters in healthy adults during self-paced treadmill-based virtual reality walking. Comput. Methods Biomech. Biomed. Eng. 2017, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, K.; Miller, E.; Kingsbury, T.; Russell Esposito, E.; Wolf, E.; Wilken, J.; Wyatt, M. Reliability of 3D gait data across multiple laboratories. Gait Posture 2016, 49, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Wilken, J.M.; Rodriguez, K.M.; Brawner, M.; Darter, B.J. Reliability and minimal detectible change values for gait kinematics and kinetics in healthy adults. Gait Posture 2012, 35, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Charlton, I.W.; Tate, P.; Smyth, P.; Roren, L. Repeatability of an optimised lower body model. Gait Posture 2004, 20, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Meldrum, D.; Shouldice, C.; Conroy, R.; Jones, K.; Forward, M. Test-retest reliability of three dimensional gait analysis: Including a novel approach to visualising agreement of gait cycle waveforms with Bland and Altman plots. Gait Posture 2014, 39, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Krause, D.A.; Boyd, M.S.; Hager, A.N.; Smoyer, E.C.; Thompson, A.T.; Hollman, J.H. Reliability and accuracy of a goniometer mobile device application for video measurement of the functional movement screen deep squat test. Int. J. Sports Phys. Ther. 2015, 10, 37–44. [Google Scholar]
- Ford, K.R.; Myer, G.D.; Hewett, T.E. Reliability of landing 3D motion analysis: Implications for longitudinal analyses. Med. Sci. Sports Exerc. 2007, 39, 2021–2028. [Google Scholar] [CrossRef] [PubMed]
- Mok, K.M.; Petushek, E.; Krosshaug, T. Reliability of knee biomechanics during a vertical drop jump in elite female athletes. Gait Posture 2016, 46, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Chappell, J.D.; Limpisvasti, O. Effect of a neuromuscular training program on the kinetics and kinematics of jumping tasks. Am. J. Sports Med. 2008, 36, 1081–1086. [Google Scholar] [CrossRef] [PubMed]
- Kirtley, C. Sensitivity of the modified helen hayes model to marker placement errors. In Proceedings of the Seventh International Symposium on the 3-D Analysis of Human Movement, Newcastle, UK, 10–12 July 2002. [Google Scholar]
- Leardini, A.; Chiari, A.; Della Croce, U.; Cappozzo, A. Human movement analysis using stereophotogrammetry Part 3. Soft tissue artifact assessment and compensation. Gait Posture 2005, 21, 212–225. [Google Scholar] [CrossRef] [PubMed]
- Piazza, S.J.; Cavanagh, P.R. Measurement of the screw-home motion of the knee is sensitive to errors in axis alignment. J. Biomech. 2000, 33, 1029–1034. [Google Scholar] [CrossRef]
- Ferrari, A.; Benedetti, M.G.; Pavan, E.; Frigo, C.; Bettinelli, D.; Rabuffetti, M.; Crenna, P.; Leardini, A. Quantitative comparison of five current protocols in gait analysis. Gait Posture 2008, 28, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Baker, R. Measuring Walking: A Handbook of Clinical Gait Analysis; Mac Keith Press: London, UK, 2013; ISBN 9780874216561. [Google Scholar]
- Cappozzo, A.; Catani, F.; Della Croce, U.; Leardini, A. Position and orientation in space of bones during movement: Anatomical frame definition and determination. Clin. Biomech. 1995, 10, 171–178. [Google Scholar] [CrossRef]






| Start | End | |
|---|---|---|
| Walk | Heel strike * | Subsequent heel strike * on the same side |
| Jump | Local maxima in left knee flexion angle that preceded each local peak in vertical heel position | Local maxima in left knee flexion angle that succeeded each local peak in vertical heel position |
| Squat | Local minima in left knee flexion angle | Subsequent local minima in left knee flexion angle |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Amri, M.; Nicholas, K.; Button, K.; Sparkes, V.; Sheeran, L.; Davies, J.L. Inertial Measurement Units for Clinical Movement Analysis: Reliability and Concurrent Validity. Sensors 2018, 18, 719. https://doi.org/10.3390/s18030719
Al-Amri M, Nicholas K, Button K, Sparkes V, Sheeran L, Davies JL. Inertial Measurement Units for Clinical Movement Analysis: Reliability and Concurrent Validity. Sensors. 2018; 18(3):719. https://doi.org/10.3390/s18030719
Chicago/Turabian StyleAl-Amri, Mohammad, Kevin Nicholas, Kate Button, Valerie Sparkes, Liba Sheeran, and Jennifer L Davies. 2018. "Inertial Measurement Units for Clinical Movement Analysis: Reliability and Concurrent Validity" Sensors 18, no. 3: 719. https://doi.org/10.3390/s18030719





