Nanofiber Scaffolds as Drug Delivery Systems to Bridge Spinal Cord Injury
Abstract
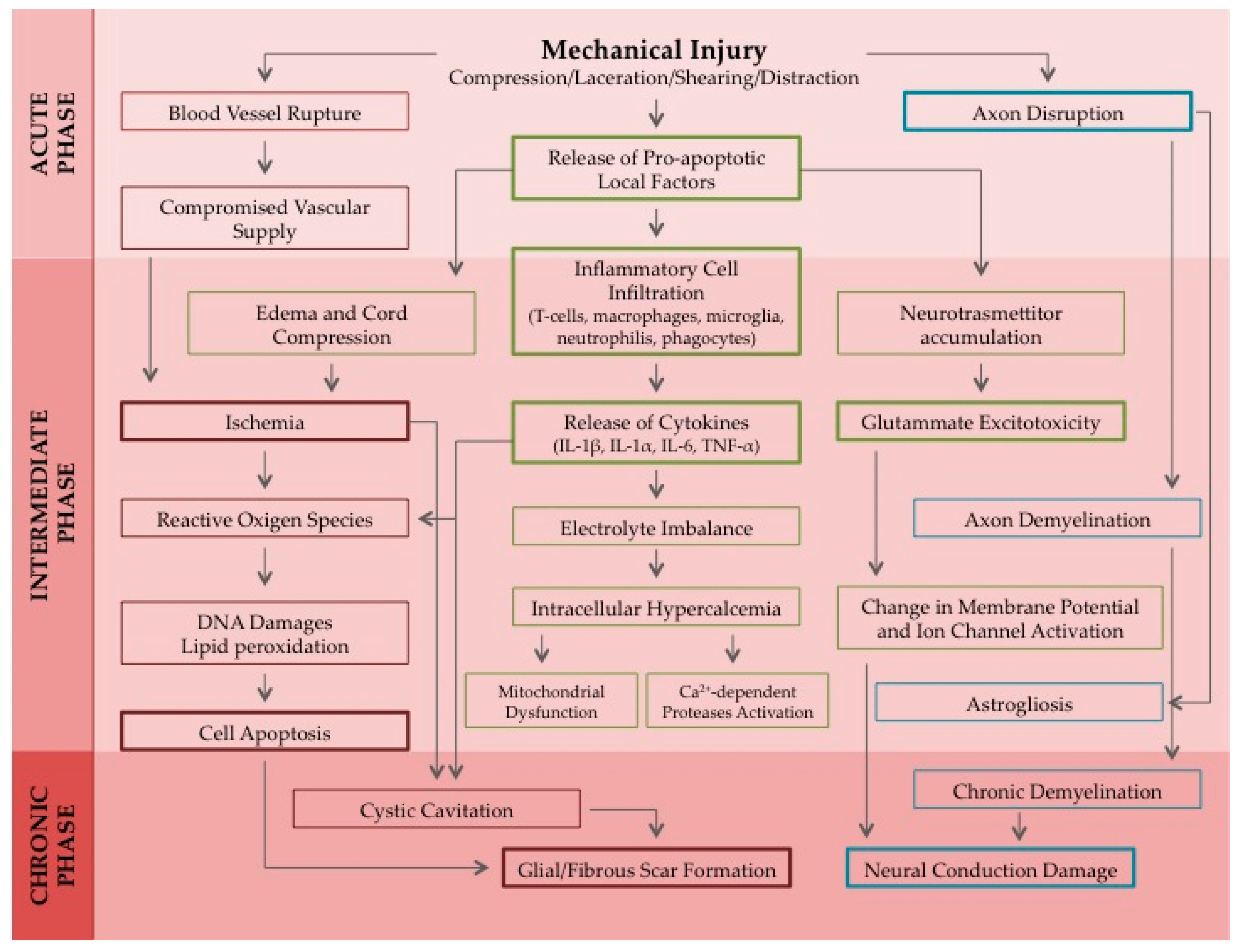
:1. Introduction
2. Overview of Current Pharmacological Approaches for the Treatment of SCI
3. Overview of Promising Nanotechnology Approaches for the Treatment of SCI
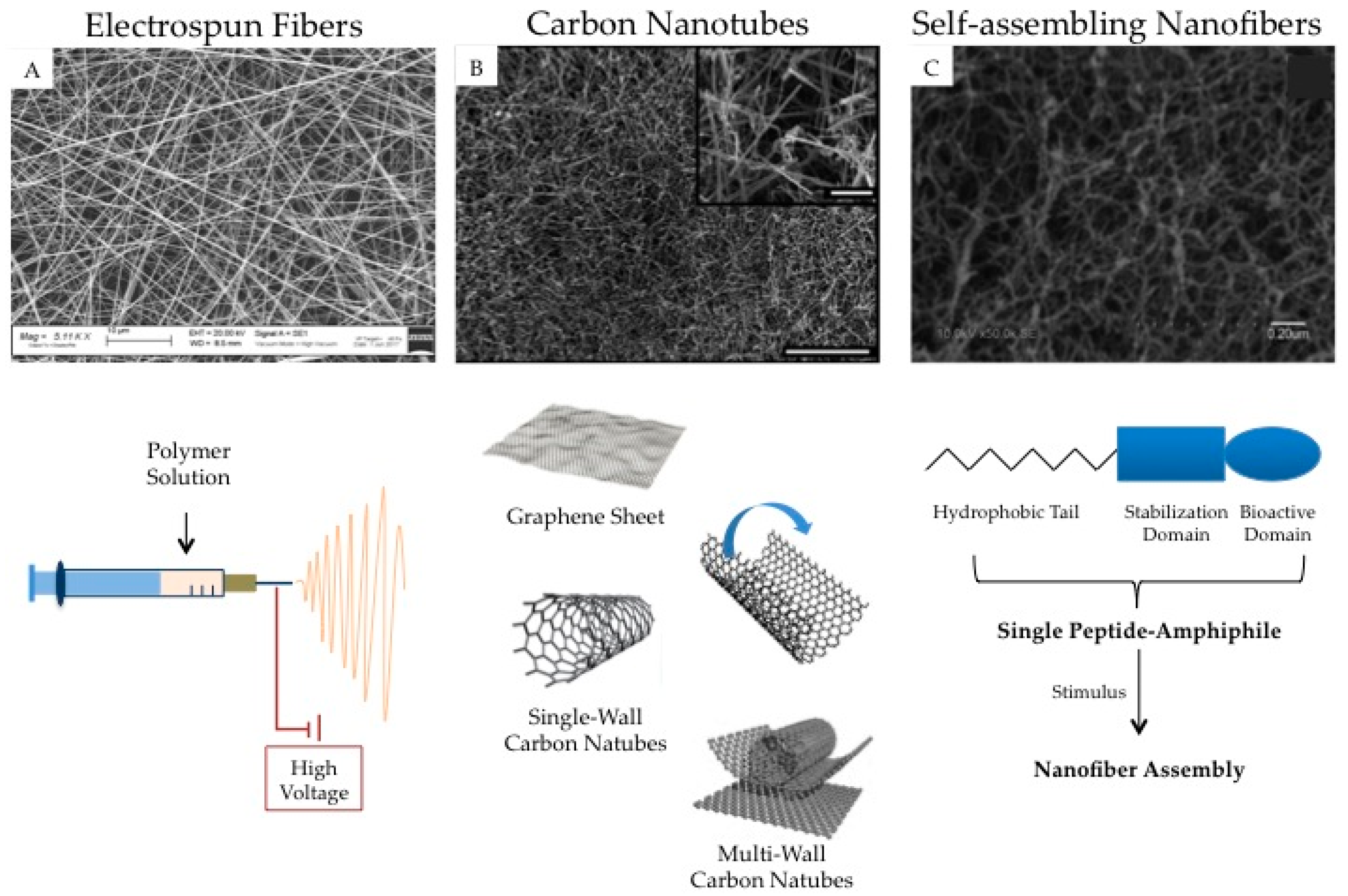
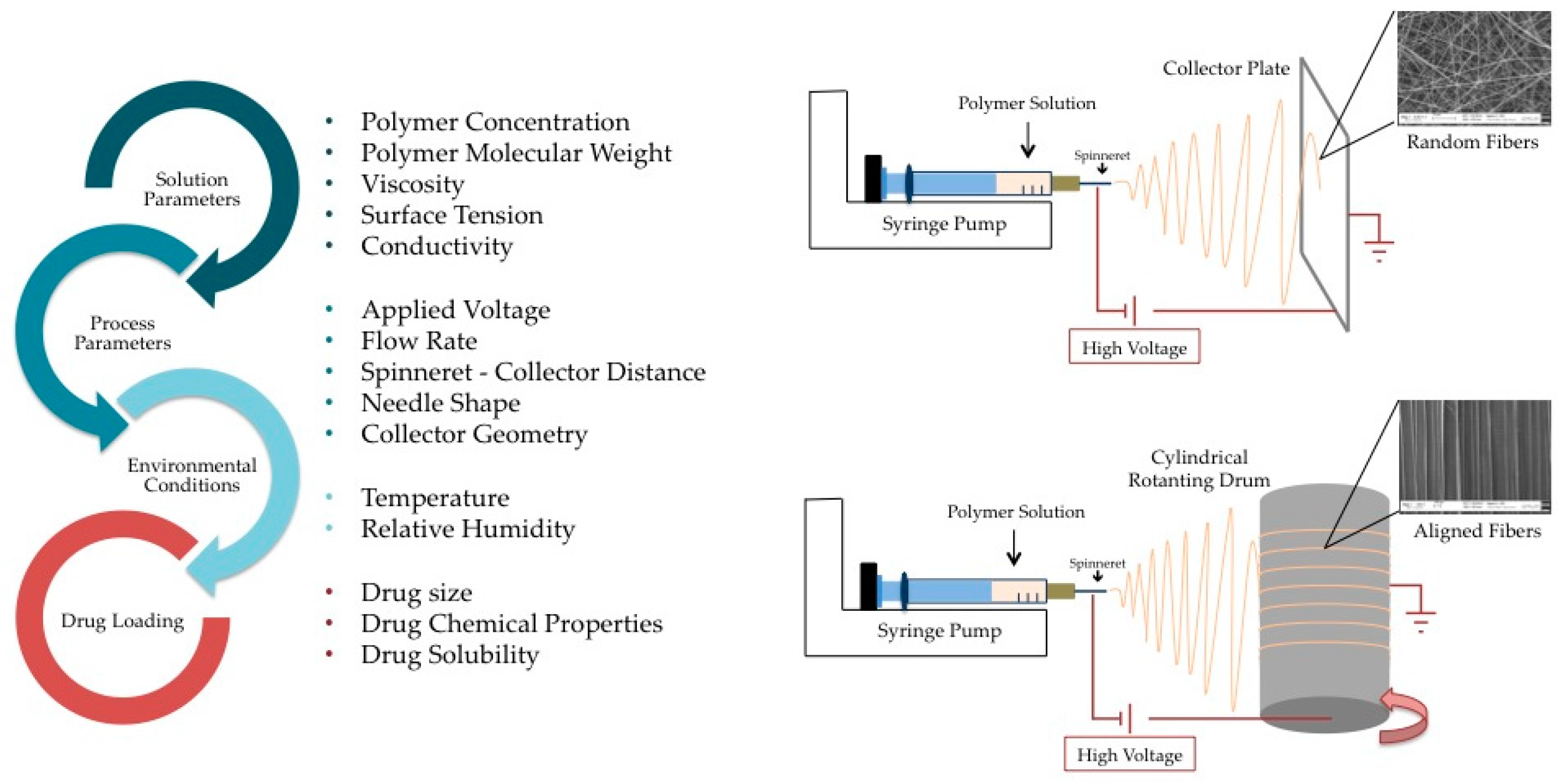
3.1. Electrospun Nanofibers
3.1.1. Solution Electrospinning
3.1.2. Emulsion Electrospinning
3.1.3. Coaxial Electrospinning
3.1.4. Drug Loading
3.1.5. Drug Release
3.2. Carbon Nanotubes
3.3. Self-Assembling Nanofibers
3.4. Nanofibers as Cell Carriers
4. Conclusions
Author Contributions
Conflicts of Interest
References
- Kabu, S.; Gao, Y.; Kwon, B.K.; Labhasetwar, V. Drug delivery, cell-based therapies, and tissue engineering approaches for spinal cord injury. J. Control. Release 2015, 219, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.D.; D’Amato, A.R.; Gilbert, R.J. Electrospun fibers for drug delivery after spinal cord injury and the effects of drug incorporation on fiber properties. Cells Tissues Organs 2016, 202, 116–135. [Google Scholar] [CrossRef] [PubMed]
- Oyinbo, C.A. Secondary injury mechanisms in traumatic spinal cord injury: A nugget of this multiply cascade. Acta Neurobiol. Exp. Wars 2011, 71, 281–299. [Google Scholar] [PubMed]
- Russell, C.M.; Choo, A.M.; Tetzlaff, W.; Chung, T.E.; Oxland, T.R. Maximum principal strain correlates with spinal cord tissue damage in contusion and dislocation injuries in the rat cervical spine. J. Neurotrauma 2012, 29, 1574–1585. [Google Scholar] [CrossRef] [PubMed]
- Choo, A.M.; Liu, J.; Dvorak, M.; Tetzlaff, W.; Oxland, T.R. Secondary pathology following contusion, dislocation, and distraction spinal cord injuries. Exp. Neurol. 2008, 212, 490–506. [Google Scholar] [CrossRef] [PubMed]
- Sofroniew, M.V. Molecular dissection of reactive astrogliosis and glial scar formation. Trends Neurosci. 2009, 32, 638–647. [Google Scholar] [CrossRef] [PubMed]
- Ahuja, C.S.; Wilson, J.R.; Nori, S.; Kotter, M.R.N.; Druschel, C.; Curt, A.; Fehlings, M.G. Traumatic spinal cord injury. Nat. Rev. Dis. Primers 2017, 3, 17018. [Google Scholar] [CrossRef] [PubMed]
- Norenberg, M.D.; Smith, J.; Marcillo, A. The pathology of human spinal cord injury: Defining the problems. J. Neurotrauma 2004, 21, 429–440. [Google Scholar] [CrossRef] [PubMed]
- Kwon, B.K.; Tetzlaff, W.; Grauer, J.N.; Beiner, J.; Vaccaro, A.R. Pathophysiology and pharmacologic treatment of acute spinal cord injury. Spine J. 2004, 4, 451–464. [Google Scholar] [CrossRef] [PubMed]
- Hamid, S.; Hayek, R. Role of electrical stimulation for rehabilitation and regeneration after spinal cord injury: An overview. Eur. Spine J. 2008, 17, 1256–1269. [Google Scholar] [CrossRef] [PubMed]
- Fleming, J.C.; Norenberg, M.D.; Ramsay, D.A.; Dekaban, G.A.; Marcillo, A.E.; Saenz, A.D.; Pasquale-Styles, M.; Dietrich, W.D.; Weaver, L.C. The cellular inflammatory response in human spinal cords after injury. Brain 2006, 129, 3249–3269. [Google Scholar] [CrossRef] [PubMed]
- Bracken, M.B.; Shepard, M.J.; Collins, W.F.; Holford, T.R.; Young, W.; Baskin, D.S.; Eisenberg, H.M.; Flamm, E.; Leo-Summers, L.; Maroon, J.; et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury: Results of the Second National Acute Spinal Cord Injury Study. N. Engl. J. Med. 1990, 322, 1405–1411. [Google Scholar] [CrossRef] [PubMed]
- Bydon, M.; Lin, J.; Macki, M.; Gokaslan, Z.L.; Bydon, A. The current role of steroids in acute spinal cord injury. World Neurosurg. 2014, 82, 848–854. [Google Scholar] [CrossRef] [PubMed]
- Pannu, R.; Christie, D.K.; Barbosa, E.; Singh, I.; Singh, A.K. Post-trauma Lipitor treatment prevents endothelial dysfunction, facilitates neuroprotection, and promotes locomotor recovery following spinal cord injury. J. Neurochem. 2007, 101, 182–200. [Google Scholar] [CrossRef] [PubMed]
- Das, A.; Sribnick, E.A.; Wingrave, J.M.; Del Re, A.M.; Woodward, J.J.; Appel, S.H.; Banik, N.L.; Ray, S.K. Calpain activation in apoptosis of ventral spinal cord 4.1 (VSC4.1) motoneurons exposed to glutamate: Calpain inhibition provides functional neuroprotection. J. Neurosci. Res. 2005, 81, 551–562. [Google Scholar] [CrossRef] [PubMed]
- Saxena, T.; Loomis, K.H.; Pai, S.B.; Karumbaiah, L.; Gaupp, E.; Patil, K.; Patkar, R.; Bellamkonda, R.V. Nanocarrier-mediated inhibition of macrophage migration inhibitory factor attenuates secondary injury after spinal cord injury. ACS Nano 2015, 9, 1492–1505. [Google Scholar] [CrossRef] [PubMed]
- Matis, G.K.; Birbilis, T.A. Erythropoietin in spinal cord injury. Eur. Spine J. 2009, 18, 314–323. [Google Scholar] [CrossRef] [PubMed]
- Kaptanoglu, E.; Solaroglu, I.; Okutan, O.; Surucu, H.S.; Akbiyik, F.; Beskonakli, E. Erythropoietin exerts neuroprotection after acute spinal cord injury in rats: Effect on lipid peroxidation and early ultrastructural findings. Neurosurg. Rev. 2004, 27, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Kwon, B.K.; Okon, E.; Hillyer, J.; Mann, C.; Baptiste, D.; Weaver, L.C.; Fehlings, M.G.; Tetzlaff, W. A systematic review of non-invasive pharmacologic neuroprotective treatments for acute spinal cord injury. J. Neurotrauma 2011, 28, 1545–1588. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Lee, S.Y.; Wu, X.; Tyler, J.Y.; Wang, H.; Ouyang, Z.; Park, K.; Xu, X.M.; Cheng, J.X. Neuroprotective ferulic acid (FA)-glycol chitosan (GC) nanoparticles for functional restoration of traumatically injured spinal cord. Biomaterials 2014, 35, 2355–2364. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.D.; Chow, W.N.; Sato-Bigbee, C.; Graf, M.R.; Graham, R.S.; Colello, R.J.; Young, H.F.; Mathern, B.E. FTY720 reduces inflammation and promotes functional recovery after spinal cord injury. J. Neurotrauma 2009, 26, 2335–2344. [Google Scholar] [CrossRef] [PubMed]
- Hamann, K.; Shi, R. Acrolein scavenging: A potential novel mechanism of attenuating oxidative stress following spinal cord injury. J. Neurochem. 2009, 111, 1348–1356. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Zheng, L.; Marquis, A.; Walls, M.; Duerstock, B.; Pond, A.; Vega-Alvarez, S.; Wang, H.; Ouyang, Z.; Shi, R. Neuroprotective role of hydralazine in rat spinal cord injury-attenuation of acrolein-mediated damage. J. Neurochem. 2014, 129, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Abrams, M.B.; Nilsson, I.; Lewandowski, S.A.; Kjell, J.; Codeluppi, S.; Olson, L.; Eriksson, U. Imatinib enhances functional outcome after spinal cord injury. PLoS ONE 2012, 7, e38760. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Jing, Y.; Yuan, X.; Zhang, X.; Li, B.; Liu, M.; Wang, B.; Li, H.; Liu, S.; Xiu, R. Melatonin treatment protects against acute spinal cord injury-induced disruption of blood spinal cord barrier in mice. J. Mol. Neurosci. 2014, 54, 714–722. [Google Scholar] [CrossRef] [PubMed]
- Paterniti, I.; Mazzon, E.; Emanuela, E.; Paola, R.D.; Galuppo, M.; Bramanti, P.; Cuzzocrea, S. Modulation of inflammatory response after spinal cord trauma with deferoxamine, an iron chelator. Free Radic. Res. 2010, 44, 694–709. [Google Scholar] [CrossRef] [PubMed]
- Rathore, K.I.; Kerr, B.J.; Redensek, A.; López-Vales, R.; Jeong, S.Y.; Ponka, P.; David, S. Ceruloplasmin protects injured spinal cord from iron-mediated oxidative damage. J. Neurosci. 2008, 28, 12736–12747. [Google Scholar] [CrossRef] [PubMed]
- Schültke, E.; Griebel, R.W.; Juurlink, B.H. Quercetin attenuates inflammatory processes after spinal cord injury in an animal model. Spinal Cord 2010, 48, 857–861. [Google Scholar] [CrossRef] [PubMed]
- Fehlings, M.G.; Wilson, J.R.; Frankowski, R.F.; Toups, E.G.; Aarabi, B.; Harrop, J.S.; Shaffrey, C.I.; Harkema, S.J.; Guest, J.D.; Tator, C.H.; et al. Riluzole for the treatment of acute traumatic spinal cord injury: Rationale for and design of the NACTN Phase I clinical trial. J. Neurosurg. Spine 2012, 17, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Schaal, S.M.; Garg, M.S.; Ghosh, M.; Lovera, L.; Lopez, M.; Patel, M.; Louro, J.; Patel, S.; Tuesta, L.; Chan, W.M.; et al. The therapeutic profile of rolipram, PDE target and mechanism of action as a neuroprotectant following spinal cord injury. PLoS ONE 2012, 7, e43634. [Google Scholar] [CrossRef] [PubMed]
- Cristante, A.F.; Barros Filho, T.E.; Oliveira, R.P.; Marcon, R.M.; Rocha, I.D.; Hanania, F.R.; Daci, K. Antioxidative therapy in contusion spinal cord injury. Spinal Cord 2009, 47, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Lv, R.; Mao, N.; Wu, J.; Lu, C.; Ding, M.; Gu, X.; Wu, Y.; Shi, Z. Neuroprotective effect of allicin in a rat model of acute spinal cord injury. Life Sci. 2015, 143, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Yuksel, Y.; Guven, M.; Kaymaz, B.; Sehitoglu, M.H.; Aras, A.B.; Akman, T.; Tosun, M.; Cosar, M. Effects of Aloe vera on spinal cord ischemia-reperfusion injury of rats. J. Investig. Surg. 2016, 29, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Fu, C.; Wang, Z.; Zhang, Z.; Wang, H.; Liu, Y. Asiaticoside attenuates the effects of spinal cord injury through antioxidant and anti-inflammatory effects, and inhibition of the p38-MAPK mechanism. Mol. Med. Rep. 2015, 12, 8294–8300. [Google Scholar] [CrossRef] [PubMed]
- Xian-Hui, D.; Xiao-Ping, H.; Wei-Juan, G. Neuroprotective effects of the Buyang Huanwu decoction on functional recovery in rats following spinal cord injury. J. Spinal Cord Med. 2016, 39, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Aydin, H.E.; Ozkara, E.; Ozbek, Z.; Vural, M.; Burukoglu, D.; Arslantas, A.; Atasoy, M.A. Histopathological evaluation of the effects of CAPE in experimental spinal cord injury. Turk. Neurosurg 2016, 26, 437–444. [Google Scholar] [PubMed]
- Wang, Z.H.; Xie, Y.X.; Zhang, J.W.; Qiu, X.H.; Cheng, A.B.; Tian, L.; Ma, B.Y.; Hou, Y.B. Carnosol protects against spinal cord injury through Nrf-2 upregulation. J. Recept. Signal Transduct. Res. 2016, 36, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Terraf, P.; Kouhsari, S.M.; Ai, J.; Babaloo, H. Tissue-engineered regeneration of hemisected spinal cord using human endometrial stem cells, poly ε-caprolactone scaffolds, and crocin as a neuroprotective agent. Mol. Neurobiol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Gokce, E.C.; Kahveci, R.; Gokce, A.; Sargon, M.F.; Kisa, U.; Aksoy, N.; Cemil, B.; Erdogan, B. Curcumin attenuates inflammation, oxidative stress, and ultrastructural damage induced by spinal cord ischemia-reperfusion injury in rats. J. Stroke Cerebrovasc. Dis. 2016, 25, 1196–1207. [Google Scholar] [CrossRef] [PubMed]
- Hussain, Z.; Thu, H.E.; Ng, S.F.; Khan, S.; Katas, H. Nanoencapsulation, an efficient and promising approach to maximize wound healing efficacy of curcumin: A review of new trends and state-of-the-art. Colloids Surf. B Biointerfaces 2017, 150, 223–241. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.H.; Yip, P.K.; Adams, L.; Davies, M.; Lee, J.W.; Michael, G.J.; Priestley, J.V.; Michael-Titus, A.T. A single bolus of docosahexaenoic acid promotes neuroplastic changes in the innervation of spinal cord interneurons and motor neurons and improves functional recovery after spinal cord injury. J. Neurosci. 2015, 35, 12733–12752. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Pérez, B.; Homs, J.; Bosch-Mola, M.; Puig, T.; Reina, F.; Verdú, E.; Boadas-Vaello, P. Epigallocatechin-3-gallate treatment reduces thermal hyperalgesia after spinal cord injury by down-regulating RhoA expression in mice. Eur. J. Pain 2016, 20, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Sehitoglu, M.H.; Guven, M.; Yüksel, Y.; Akman, T.; Bozkurt Aras, A.; Farooqi, A.A.; Cosar, M. The effect of glycyrrhizic acid on traumatic spinal cord injury in rats. Cell. Mol. Biol. (Noisy-le-Grand) 2016, 62, 2–8. [Google Scholar]
- Gokce, E.C.; Kahveci, R.; Atanur, O.M.; Gürer, B.; Aksoy, N.; Gokce, A.; Sargon, M.F.; Cemil, B.; Erdogan, B.; Kahveci, O. Neuroprotective effects of Ganoderma lucidum polysaccharides against traumatic spinal cord injury in rats. Injury 2015, 46, 2146–2155. [Google Scholar] [CrossRef] [PubMed]
- Yan, M.; Liu, Y.W.; Shao, W.; Mao, X.G.; Yang, M.; Ye, Z.X.; Liang, W.; Luo, Z.J. EGb761 improves histological and functional recovery in rats with acute spinal cord contusion injury. Spinal Cord 2016, 54, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, M.; Nakae, A.; Kishida, Y.; Baba, K.; Sakashita, N.; Shibata, M.; Yoshikawa, H.; Hagihara, K. Go-sha-jinki-Gan (GJG) ameliorates allodynia in chronic constriction injury-model mice via suppression of TNF-α expression in the spinal cord. Mol. Pain 2016, 12. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.G.; Yang, J.; Lv, Z.P.; Wang, T.H.; Li, X.S.; Liu, J.H.; Zhao, N.; Xiyang, Y.B. Effect of Herba Lycopodii alcohol extracted granule combined methylprednisolone on expression levels of BDNF and NMDA and behavior of traumatic spinal cord injury rats. Zhongguo Zhong Xi Yi Jie He Za Zhi 2015, 35, 1004–1010. [Google Scholar] [PubMed]
- Luo, Y.; Fu, C.; Wang, Z.; Zhang, Z.; Wang, H.; Liu, Y. Mangiferin attenuates contusive spinal cord injury in rats through the regulation of oxidative stress, inflammation and the Bcl-2 and Bax pathway. Mol. Med. Rep. 2015, 12, 7132–7138. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Ma, X. Effect of rutin on spinal cord injury through inhibition of the expression of MIP-2 and activation of MMP-9, and downregulation of Akt phosphorylation. Mol. Med. Rep. 2015, 12, 7554–7560. [Google Scholar] [CrossRef] [PubMed]
- Gökce, E.C.; Kahveci, R.; Gökce, A.; Cemil, B.; Aksoy, N.; Sargon, M.F.; Kısa, Ü.; Erdoğan, B.; Güvenç, Y.; Alagöz, F.; et al. Neuroprotective effects of thymoquinone against spinal cord ischemia-reperfusion injury by attenuation of inflammation, oxidative stress, and apoptosis. J. Neurosurg. Spine 2016, 24, 949–959. [Google Scholar] [CrossRef] [PubMed]
- Ewan, E.E.; Hagg, T. Intrathecal acetyl-l-carnitine protects tissue and improves function after a mild contusive spinal cord injury in rats. J. Neurotrauma 2016, 33, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Celik, H.; Karatay, M.; Erdem, Y.; Yildirim, A.E.; Sertbas, I.; Karatay, E.; Kul, H.; Guvenc, Y.; Koksal, I.; Menekse, G.; et al. The biochemical, histopathological and clinical comparison of the neuroprotective effects of subcutaneous adalimumab and intravenous methylprednisolone in an experimental compressive spinalcord trauma model. Turk. Neurosurg 2016, 26, 622–631. [Google Scholar] [CrossRef] [PubMed]
- Gurcay, A.G.; Gurcan, O.; Kazanci, A.; Bozkurt, I.; Senturk, S.; Bodur, E.; Turkoglu, O.F.; Bavbek, M. Comparative biochemical and motor function analysis of alpha lipoic acid and n-acetyl cysteine treatment on rats with experimental spinal cord injury. Turk. Neurosurg 2016, 26, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Kermani, H.R.; Nakhaee, N.; Fatahian, R.; Najar, A.G. Effect of aspirin on spinal cord injury: An experimental study. Iran. J. Med. Sci. 2016, 41, 217–222. [Google Scholar] [PubMed]
- Zhang, B.; Bailey, W.M.; Kopper, T.J.; Orr, M.B.; Feola, D.J.; Gensel, J.C. Azithromycin drives alternative macrophage activation and improves recovery and tissue sparing in contusion spinal cord injury. J. Neuroinflamm. 2015, 12, 218. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Li, M.; He, F.; Bian, Z.; Liu, J.; He, Q.; Wang, X.; Sun, T.; Zhu, L. Dopamine D1 receptor agonist A-68930 inhibits NLRP3 inflammasome activation and protects rats from spinal cord injury-induced acute lung injury. Spinal Cord 2016, 54, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Han, J.; Zhao, Y.; Ding, W.; Wei, J.; Li, J.; Han, S.; Shang, X.; Wang, B.; Chen, B.; et al. Functionalized collagen scaffold implantation and cAMP administration collectively facilitate spinal cord regeneration. Acta Biomater. 2016, 30, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Karatas, Y.; Cengiz, S.L.; Esen, H.; Toker, A.; Savas, C. Effect of carvedilol on secondary damage in experimental spinal cord injury in rats. Turk. Neurosurg 2015, 25, 930–935. [Google Scholar] [CrossRef] [PubMed]
- Kwiecien, J.M.; Jarosz, B.; Oakden, W.; Klapec, M.; Stanisz, G.J.; Delaney, K.H.; Kotlinska-Hasiec, E.; Janik, R.; Rola, R.; Dabrowski, W. An in vivo model of anti-inflammatory activity of subdural dexamethasone following the spinal cord injury. Neurol. Neurochir. Polska 2016, 50, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Xia, T.; Ni, S.; Li, X.; Yao, J.; Qi, H.; Fan, X.; Wang, J. Sustained delivery of dbcAMP by poly(propylene carbonate) micron fibers promotes axonal regenerative sprouting and functional recovery after spinal cord hemisection. Brain Res. 2013, 1538, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.W.; Chen, B.; Huang, K.L.; Dai, Y.S.; Teng, H.L. Inhibition of autophagy by estradiol promotes locomotor recovery after spinal cord injury in rats. Neurosci. Bull. 2016, 32, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Amini Pishva, A.; Akbari, M.; Farahabadi, A.; Arabkheradmand, A.; Beyer, C.; Dashti, N.; Moradi, F.; Hassanzadeh, G. Effect of estrogen therapy on TNF-α and iNOS gene expression in spinal cord injury model. Acta Med. Iran. 2016, 54, 296–301. [Google Scholar] [PubMed]
- Ahmad, M.; Zakaria, A.; Almutairi, K.M. Effectiveness of minocycline and FK506 alone and in combination on enhanced behavioral and biochemical recovery from spinal cord injury in rats. Pharmacol. Biochem. Behav. 2016, 145, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Khayrullina, G.; Bermudez, S.; Byrnes, K.R. Inhibition of NOX2 reduces locomotor impairment, inflammation, and oxidative stress after spinal cord injury. J. Neuroinflamm. 2015, 12, 172. [Google Scholar] [CrossRef] [PubMed]
- Sanna, M.D.; Lucarini, L.; Durante, M.; Ghelardini, C.; Masini, E.; Galeotti, N. Histamine H4 receptor agonist-induced relief from painful peripheral neuropathy is mediated by inhibition of spinal neuroinflammation and oxidative stress. Br. J. Pharmacol. 2017, 174, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.K.; Kang, M.W.; Rhee, Y.J.; Kim, C.S.; Jeon, B.H.; Han, S.J.; Cho, H.J.; Na, M.H.; Yu, J.H. In vivo neuroprotective effect of histidine-tryptophan-ketoglutarate solution in an ischemia/reperfusion spinal cord injury animal model. Korean J. Thorac. Cardiovasc. Surg. 2016, 49, 232–241. [Google Scholar] [CrossRef] [PubMed]
- Martini, A.C.; Berta, T.; Forner, S.; Chen, G.; Bento, A.F.; Ji, R.R.; Rae, G.A. Lipoxin A4 inhibits microglial activation and reduces neuroinflammation and neuropathic pain after spinal cord hemisection. J. Neuroinflamm. 2016, 13, 75. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Bai, C.; Zheng, D.; Li, C.; Zhang, W.; Li, M.; Guan, W.; Ma, Y. Combination of melatonin and Wnt-4 promotes neural cell differentiation in bovine amniotic epithelial cells and recovery from spinal cord injury. J. Pineal Res. 2016, 60, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Liu, C.; Gao, K.; Zhao, H.; Zhou, Z.; Shen, Z.; Guo, Y.; Li, Z.; Yao, T.; Mei, X. Metformin preconditioning provide neuroprotection through enhancement of autophagy and suppression of inflammation and apoptosis after spinal cord injury. Biochem. Biophys. Res. Commun. 2016, 477, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Norouzi-Javidan, A.; Javanbakht, J.; Barati, F.; Fakhraei, N.; Mohammadi, F.; Dehpour, A.R. Serotonin 5-HT7 receptor agonist, LP-211, exacerbates Na+, K+-ATPase/Mg2+-ATPase imbalances in spinal cord-injured male rats. Diagn. Pathol. 2015, 10, 157. [Google Scholar] [CrossRef] [PubMed]
- Aceves, M.; Bancroft, E.A.; Aceves, A.R.; Hook, M.A. Nor-binaltorphimine blocks the adverse effects of morphine after spinal cord injury. J. Neurotrauma 2017, 34, 1164–1174. [Google Scholar] [CrossRef] [PubMed]
- Dong, Q.; Sun, L.; Peng, L.; Yan, B.; Lv, J.; Wang, G.; Gong, S. PMX53 protects spinal cord from ischemia-reperfusion injury in rats in the short term. Spinal Cord 2016, 54, 254–258. [Google Scholar] [CrossRef] [PubMed]
- Coronel, M.F.; Raggio, M.C.; Adler, N.S.; De Nicola, A.F.; Labombarda, F.; González, S.L. Progesterone modulates pro-inflammatory cytokine expression profile after spinal cord injury: Implications for neuropathic pain. J. Neuroimmunol. 2016, 292, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q.J.; Yang, Y. Function of SOD1, SOD2, and PI3K/AKT signalling pathways in the protection of propofol on spinal cord ischemic reperfusion injury in a rabbit model. Life Sci. 2016, 148, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Gao, K.; Wang, Y.S.; Yuan, Y.J.; Wan, Z.H.; Yao, T.C.; Li, H.H.; Tang, P.F.; Mei, X.F. Neuroprotective effect of rapamycin on spinal cord injury via activation of the WNT/β-catenin signalling pathway. Neural Regen. Res. 2015, 10, 951–957. [Google Scholar] [PubMed]
- Zhou, Y.; Zheng, B.; Ye, L.; Zhang, H.; Zhu, S.; Zheng, X.; Xia, Q.; He, Z.; Wang, Q.; Xiao, J.; Xu, H. Retinoic acid prevents disruption of blood-spinal cord barrier by inducing autophagic flux after spinal cord injury. Neurochem. Res. 2016, 41, 813–825. [Google Scholar] [CrossRef] [PubMed]
- Li, X.G.; Lin, X.J.; Du, J.H.; Xu, S.Z.; Lou, X.F.; Chen, Z. Combination of methylprednisolone and rosiglitazone promotes recovery of neurological function after spinal cord injury. Neural Regen. Res. 2016, 11, 1678–1684. [Google Scholar] [PubMed]
- Chen, X.B.; Yuan, H.; Wang, F.J.; Tan, Z.X.; Liu, H.; Chen, N. Protective role of selenium-enriched supplement on spinal cord injury through the up-regulation of CNTF and CNTF-Ralpha. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 4434–4442. [Google Scholar] [PubMed]
- Gao, K.; Wang, G.; Wang, Y.; Han, D.; Bi, J.; Yuan, Y.; Yao, T.; Wan, Z.; Li, H.; Mei, X. Neuroprotective effect of simvastatin via inducing the autophagy on spinal cord injury in the rat model. Biomed. Res. Int. 2015, 2015, 260161. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.X.; Gao, C.Z.; Fan, K.L.; Yang, L.M.; Mei, X.F. STAT1 inhibitor alleviates spinal cord injury by decreasing apoptosis. Genet. Mol. Res. 2016, 15. [Google Scholar] [CrossRef] [PubMed]
- Colón, J.M.; Miranda, J.D. Tamoxifen: An FDA approved drug with neuroprotective effects for spinal cord injury recovery. Neural Regen. Res. 2016, 11, 1208–1211. [Google Scholar] [PubMed]
- Wang, C.; Wang, P.; Zeng, W.; Li, W. Tetramethylpyrazine improves the recovery of spinal cord injury via Akt/Nrf2/HO-1 pathway. Bioorg. Med. Chem. Lett. 2016, 26, 1287–1291. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishna, M.; Steuer, I.; Prince, F.; Roberts, M.; Mongeon, D.; Kia, M.; Dyck, S.; Matte, G.; Vaillancourt, M.; Guertin, P.A. Double-blind, placebo-controlled, randomized phase I/IIa study (safety and efficacy) with buspirone/levodopa/carbidopa (SpinalonTM) in subjects with complete AIS A or motor-complete AIS B spinal cord injury. Curr. Pharm. Des. 2017, 23, 1789–1804. [Google Scholar] [CrossRef]
- Park, J.; Zheng, L.; Acosta, G.; Vega-Alvarez, S.; Chen, Z.; Muratori, B.; Cao, P.; Shi, R. Acrolein contributes to TRPA1 up-regulation in peripheral and central sensory hypersensitivity following spinal cord injury. J. Neurochem. 2015, 135, 987–997. [Google Scholar] [CrossRef] [PubMed]
- Han, Z.A.; Song, D.H.; Oh, H.M.; Chung, M.E. Botulinum toxin type A for neuropathic pain in patients with spinal cord injury. Ann. Neurol. 2016, 79, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Wilsey, B.; Marcotte, T.D.; Deutsch, R.; Zhao, H.; Prasad, H.; Phan, A. An exploratory human laboratory experiment evaluating vaporized cannabis in the treatment of neuropathic pain from spinal cord injury and disease. J. Pain 2016, 17, 982–1000. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.C.; Lee, Y.J.; Cho, C.B.; Park, Y.S. Suppressed GABAergic signalling in the zona incerta causes neuropathic pain in a thoracic hemisection spinal cord injury rat model. Neurosci. Lett. 2016, 632, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Pawasauskas, J. Opioid rotation: A case example using methadone in spinal cord injury. J. Opioid Manag. 2015, 11, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Ellis, A.; Grace, P.M.; Wieseler, J.; Favret, J.; Springer, K.; Skarda, B.; Ayala, M.; Hutchinson, M.R.; Falci, S.; Rice, K.C.; et al. Morphine amplifies mechanical allodynia via TLR4 in a rat model of spinal cord injury. Brain Behav. Immun. 2016, 58, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Sang, C.N.; Barnabe, K.J.; Kern, S.E. Phase IA clinical trial evaluating the tolerability, pharmacokinetics, and analgesic efficacy of an intrathecally administered neurotensin an analogue in central neuropathic pain following spinal cord injury. Clin. Pharmacol. Drug Dev. 2016, 5, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Huang, M.; Chen, H.; Jiang, C.; Xie, K.; Tang, P.; Ou, R.; Zeng, J.; Liu, Q.; Li, Q.; Huang, J.; et al. Effects of botulinum toxin A injections in spinal cord injury patients with detrusor overactivity and detrusor sphincter dyssynergia. J. Rehabil. Med. 2016, 48, 683–687. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, H.; Uemura, O.; Mori, T.; Okisio, N.; Unai, K.; Liu, M. Effect of imidafenacin on the urodynamic parameters of patients with indwelling bladder catheters due to spinal cord injury. Spinal Cord 2017, 55, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Chung, Y.G.; Seth, A.; Doyle, C.; Franck, D.; Kim, D.; Cristofaro, V.; Benowitz, L.I.; Tu, D.D.; Estrada, C.R.; Mauney, J.R.; et al. Inosine improves neurogenic detrusor overactivity following spinal cord injury. PLoS ONE 2015, 10, e0141492. [Google Scholar] [CrossRef] [PubMed]
- Wöllner, J.; Pannek, J. Initial experience with the treatment of neurogenic detrusor overactivity with a new β-3 agonist (mirabegron) in patients with spinal cord injury. Spinal Cord 2016, 54, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Ishida, H.; Yamauchi, H.; Ito, H.; Akino, H.; Yokoyama, O. α1D-Adrenoceptor blockade increases voiding efficiency by improving external urethral sphincter activity in rats with spinal cord injury. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2016, 311, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Sakakibara, F.; Takahama, K.; Nanri, M.; Sasaki, E. Pharmacological properties of propiverine contribute to improving lower urinary tract dysfunctions in rats with spinal cord injuries. Drug Res. (Stuttg) 2016, 66, 464–469. [Google Scholar] [CrossRef] [PubMed]
- Rossi, F.; Perale, S.; Papa, S.; Forloni, G.; Veglianese, P. Current options for drug delivery to the spinal cord. Expert Opin. Drug Deliv. 2013, 10, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Zamani, F.; Amani-Tehran, M.; Latifi, M.; Shokrgozar, M.A.; Zaminy, A. Promotion of spinal cord axon regeneration by 3D nanofibrous core-sheath scaffolds. J. Biomed. Mater Res. A 2014, 102, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Cheethamb, A.G.; Cui, H. Building nanostructures with drugs. Nano Today 2016, 11, 13–30. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, A.; Matsushita, A.; Sankai, Y. A 3D nanofibrous hydrogel and collagen sponge scaffold promotes locomotor functional recovery, spinal repair, and neuronal regeneration after complete transection of the spinal cord in adult rats. Biomed. Mater 2015, 10, 015008. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.S.; Quian, C.H.; Ling, E.A.; Zeng, Y.S. Nanofiber scaffolds for treatment of spinal cord injury. Curr. Med. Chem. 2014, 21, 4282–4289. [Google Scholar] [CrossRef] [PubMed]
- Asghari, F.; Samiei, M.; Adibkia, K.; Akbarzadeh, A.; Davaran, S. Biodegradable and biocompatible polymers for tissue engineering application: A review. Artif. Cells Nanomed. Biotechnol. 2017, 45, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Goyal, R.; Macri, L.K.; Kaplan, H.M.; Kohn, J. Nanoparticles and nanofibers for topical drug delivery. J. Control Release 2016, 28, 77–92. [Google Scholar] [CrossRef] [PubMed]
- Owen, S.C.; Shoichet, M.S. Design of three-dimensional biomimetic scaffolds. J. Biomed. Mater Res. A 2010, 94, 1321–1331. [Google Scholar] [CrossRef] [PubMed]
- Hurtado, A.; Cregg, J.M.; Wang, H.B.; Wendell, D.F.; Oudega, M.; Gilbert, R.J.; McDonald, J.W. Robust CNS regeneration after complete spinal cord transection using aligned poly-l-lactic acid microfibers. Biomaterials 2011, 32, 6068–6079. [Google Scholar] [CrossRef] [PubMed]
- Prabhakaran, M.P.; Vatankhah, E.; Ramakrishna, S. Electrospun aligned PHBV/collagen nanofibers as substrates for nerve tissue engineering. Biotechnol. Bioeng. 2013, 110, 2775–2784. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Lee, Y.J.; Cho, H.J.; Shin, H. Guidance of in vitro migration of human mesenchymal stem cells and in vivo guided bone regeneration using aligned electrospun fibers. Tissue Eng. Part A 2014, 20, 2031–2042. [Google Scholar] [CrossRef] [PubMed]
- Zuidema, J.M.; Hyzinski-García, M.C.; Van Vlasselaer, K.; Zaccor, N.W.; Plopper, G.E.; Mongin, A.A.; Gilbert, R.J. Enhanced GLT-1 mediated glutamate uptake and migration of primary astrocytes directed by fibronectin-coated electrospun poly-L-lactic acid fibers. Biomaterials 2014, 35, 1439–1449. [Google Scholar] [CrossRef] [PubMed]
- Lanza, R.P.; Langer, R.; Chick, W.L.; Peppas, N.A. Principles of tissue engineering. Nature 1997, 389, 453. [Google Scholar]
- Raspa, A.; Marchini, A.; Pugliese, R.; Mauri, M.; Maleki, M.; Vasita, R.; Gelain, F. A biocompatibility study of new nanofibrous scaffolds for nervous system regeneration. Nanoscale 2016, 8, 253–265. [Google Scholar] [CrossRef] [PubMed]
- Qu, J.; Wang, D.; Wang, H.; Dong, Y.; Zhang, F.; Zuo, B.; Zhang, H. Electrospun silk fibroin nanofibers in different diameters support neurite outgrowth and promote astrocyte migration. J. Biomed. Mater Res. A 2013, 101, 2667–2678. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.C.; Kim, Y.H.; Kim, J.W.; Ha, K.Y. Transplantation of mesenchymal stem cells for acute spinal cord injury in rats: Comparative study between intralesional injection and scaffold based Transplantation. J. Korean Med. Sci. 2016, 31, 1373–1382. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Houle, J.D.; Xu, J.; Chan, B.P.; Chew, S.Y. Nanofibrous collagen nerve conduits for spinal cord repair. Tissue Eng. Part A 2012, 18, 1057–1066. [Google Scholar] [CrossRef] [PubMed]
- Altinova, H.; Möllers, S.; Führmann, T.; Deumens, R.; Bozkurt, A.; Heschel, I.; Damink, L.H.; Schügner, F.; Weis, J.; Brook, G.A. Functional improvement following implantation of a microstructured, type-I collagen scaffold into experimental injuries of the adult rat spinal cord. Brain Res. 2014, 1585, 37–50. [Google Scholar] [CrossRef] [PubMed]
- Palejwala, A.H.; Fridley, J.S.; Mata, J.A.; Samuel, E.L.; Luerssen, T.G.; Perlaky, L.; Kent, T.A.; Tour, J.M.; Jea, A. Biocompatibility of reduced graphene oxide nanoscaffolds following acute spinal cord injury in rats. Surg. Neurol. Int. 2016, 7, 75. [Google Scholar] [CrossRef] [PubMed]
- Jeffries, E.M.; Wang, Y. Biomimetic micropatterned multi-channel nerve guides by templated electrospinning. Biotechnol. Bioeng. 2012, 109, 1571–1582. [Google Scholar] [CrossRef] [PubMed]
- Ranjbar-Mohammadi, M.; Prabhakaran, M.P.; Bahrami, S.H.; Ramakrishna, S. Gum tragacanth/poly(l-lactic acid) nanofibrous scaffolds for application in regeneration of peripheral nerve damage. Carbohydr. Polym. 2016, 140, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Webber, M.J.; Matson, J.B.; Tamboli, V.K.; Stupp, S.I. Controlled release of dexamethasone from peptide nanofiber gels to modulate inflammatory response. Biomaterials 2012, 33, 6823–6832. [Google Scholar] [CrossRef] [PubMed]
- Hsu, K.H.; Fang, S.P.; Lin, C.L.; Liao, Y.S.; Yoon, Y.K.; Chauhan, A. Hybrid electrospun polycaprolactone mats consisting of nanofibers and microbeads for extended release of dexamethasone. Pharm. Res. 2016, 33, 1509–1516. [Google Scholar] [CrossRef] [PubMed]
- Saadai, P.; Nout, Y.S.; Encinas, J.; Wang, A.; Downing, T.L.; Beattie, M.S.; Bresnahan, J.C.; Li, S.; Farmer, D.L. Prenatal repair of myelomeningocele with aligned nanofibrous scaffolds-a pilot study in sheep. J. Pediatr. Surg. 2011, 46, 2279–2283. [Google Scholar] [CrossRef] [PubMed]
- Gelain, F.; Panseri, S.; Antonini, S.; Cunha, C.; Donega, M.; Lowery, J.; Taraballi, F.; Cerri, G.; Montagna, M.; Baldissera, F.; et al. Transplantation of nanostructured composite scaffolds results in the regeneration of chronically injured spinal cords. ACS Nano 2011, 5, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Pires, L.R.; Guarino, V.; Oliveira, M.J.; Ribeiro, C.C.; Barbosa, M.A.; Ambrosio, L.; Pêgo, A.P. Ibuprofen-loaded poly(trimethylene carbonate-co-ε-caprolactone) electrospun fibres for nerve regeneration. J. Tissue Eng. Regen. Med. 2016, 10, 154–166. [Google Scholar] [CrossRef] [PubMed]
- Hakim, J.S.; Esmaeili Rad, M.; Grahn, P.J.; Chen, B.K.; Knight, A.M.; Schmeichel, A.M.; Isaq, N.A.; Dadsetan, M.; Yaszemski, M.J.; Windebank, A.J. Positively charged oligo[poly(ethylene glycol) fumarate] scaffold implantation results in a permissive lesion environment after spinal cord injury in rat. Tissue Eng. Part A 2015, 21, 2099–2114. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Bashur, C.A.; Goldstein, A.S.; Schmidt, C.E. Polypyrrole-Coated Electrospun PLGA Nanofibers for Neural Tissue Applications. Biomaterials 2009, 30, 4325–4335. [Google Scholar] [CrossRef] [PubMed]
- Schnell, E.; Klinkhammeer, K.; Balzer, S.; Brook, G.; Klee, D.; Dalton, P.; Mey, J. Guidance of glial cell migration and axonal growth on electrospun nanofibers of poly-ε-caprolactone and a collagen/poly-ε-caprolactone blend. Biomaterials 2007, 28, 3012–3025. [Google Scholar] [CrossRef] [PubMed]
- Kubinová, Š.; Horák, D.; Hejčl, A.; Plichta, Z.; Kotek, J.; Proks, V.; Forostyak, S.; Syková, E. SIKVAV-modified highly superporous PHEMA scaffolds with oriented pores for spinal cord injury repair. J. Tissue Eng. Regen. Med. 2015, 9, 1298–1309. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Kai, D.; Ye, H.; Tian, L.; Ding, X.; Ramakrishna, S.; Loh, X.J. Electrospinning of poly(glycerol sebacate)-based nanofibers for nerve tissue engineering. Mater. Sci. Eng. C Mater. Biol. Appl. 2017, 70, 1089–1094. [Google Scholar] [CrossRef] [PubMed]
- Entekhabi, E.; Haghbin Nazarpak, M.; Moztarzadeh, F.; Sadeghi, A. Design and manufacture of neural tissue engineering scaffolds using hyaluronic acid and polycaprolactone nanofibers with controlled porosity. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 69, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.V.; Chen, W.S.; Keratithamkul, K.; Stoick, M.; Kapala, B.; Johnson, E.; Huang, A.C.; Chin, T.Y.; Chen-Yang, Y.W.; Yang, M.L. Degradation of the electrospun silica nanofiber in a biological medium for primary hippocampal neuron-effect of surface modification. Int. J. Nanomed. 2016, 11, 729–741. [Google Scholar]
- Fan, Z.; Shen, Y.; Zhang, F.; Zuo, B.; Lu, Q.; Wu, P.; Xie, Z.; Dong, Q.; Zhang, H. Control of olfactory ensheathing cell behaviors by electrospun silk fibroin fibers. Cell Transplant. 2013, 22, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Gnavi, S.; Fornasari, B.E.; Tonda-Turo, C.; Laurano, R.; Zanetti, M.; Ciardelli, G.; Geuna, S. The Effect of Electrospun Gelatin Fibers Alignment on Schwann Cell and Axon Behavior and Organization in the Perspective of Artificial Nerve Design. Int. J. Mol. Sci. 2015, 16, 12925–12942. [Google Scholar] [CrossRef] [PubMed]
- Junka, R.; Valmikinathan, C.M.; Kalyon, D.M.; Yu, X. Laminin Functionalized Biomimetic Nanofibers for Nerve Tissue Engineering. J. Biomater. Tissue Eng. 2013, 3, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Dwivedi, C.; Pandey, H.; Pandey, A.C.; Ramteke, P.W. Repair and regenerations. Curr. Pharm. Des. 2016, 22, 1460–1471. [Google Scholar] [CrossRef] [PubMed]
- Ranjbar-Mohammadi, M.; Bahrami, S.H. Electrospun curcumin loaded poly(ε-caprolactone)/gum tragacanth nanofibers for biomedical application. Int. J. Biol. Macromol. 2016, 84, 448–456. [Google Scholar] [CrossRef] [PubMed]
- Kubinová, Š.; Syková, E. Nanotechnology for trearment of stroke spinal cord injury. Nanomedicine 2010, 5, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Schaub, N.J.; Johnson, C.D.; Cooper, B.; Gilbert, R.J. Electrospun fibers for spinal cord injury research and regeneration. J. Neurotrauma 2016, 33, 1405–1415. [Google Scholar] [CrossRef] [PubMed]
- Rochkind, S.; Shahar, A.; Fliss, D.; El-Ani, D.; Astachov, L.; Hayon, T.; Alon, M.; Zamostiano, R.; Ayalon, O.; Biton, I.E.; et al. Development of a tissue-engineered composite implant for treating traumatic paraplegia in rats. Eur. Spine J. 2006, 15, 234–245. [Google Scholar] [CrossRef] [PubMed]
- Usmani, S.; Aurand, E.R.; Medelin, M.; Fabbro, A.; Scaini, D.; Laishram, J.; Rosselli, F.B.; Ansuini, A.; Zoccolan, D.; Scarselli, M.; et al. 3D meshes of carbon nanotubes guide functional reconnection of segregated spinal explants. Sci. Adv. 2016, 2, e1600087. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ye, H.; Satkunendrarajah, K.; Yao, G.S.; Bayon, Y.; Fehlings, M.G. A self-assembling peptide reduces glial scarring, attenuates post-traumatic inflammation and promotes neurological recovery following spinal cord injury. Acta Biomater. 2013, 9, 8075–8088. [Google Scholar] [CrossRef] [PubMed]
- Rogina, A. Electrospinning process: Versatile preparation method for biodegradable and natural polymers and biocomposite systems applied in tissue engineering and drug. Appl. Surf. Sci. 2014, 296, 221–230. [Google Scholar] [CrossRef]
- Pelipenko, J.; Kristl, J.; Janković, B.; Baumgartner, S.; Kocbek, P. The impact of relative humidity during electrospinning on the morphology and mechanical properties of nanofibers. Int. J. Pharm. 2013, 456, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Luu, Y.K.; Chang, C.; Fang, D.; Hsiao, B.S.; Chu, B.; Hadjiargyrou, M. Incorporation and controlled release of a hydrophilic antibiotic using poly(lactide-co-glycolide)-based electrospun nanofibrous scaffolds. J. Control Release 2004, 98, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Jannesari, M.; Varshosaz, J.; Morshed, M.; Zamani, M. Composite poly (vinyl alcohol)/poly (vinyl acetate) electrospun nanofibrous mats as a novel wound dressing matrix for controlled release of drugs. Int. J. Nanomed. 2011, 6, 993–1003. [Google Scholar]
- Meng, Z.; Xu, X.X.; Zheng, W.; Zhou, H.M.; Li, L.; Zheng, Y.F.; Lou, X. Preparation and characterization of electrospun PLGA/gelatin nanofibers as a potential drug delivery system. Colloids Surf. B Biointerfaces 2011, 84, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Bhattarai, N.; Cha, D.I.; Bhattarai, S.R.; Khil, M.S.; Kim, H.Y. Biodegradable electrospun mat: Novel block copolymer of poly (p-dioxanone-co-l-lactide)-block-poly(ethylene glycol). J. Polym. Sci. B Polym. Phys. 2003, 41, 1955–1964. [Google Scholar] [CrossRef]
- Lu, Y.; Huang, J.; Yu, G.; Cardenas, R.; Wei, S.; Wujcik, E.K.; Guo, Z. Coaxial electrospun fibers: Applications in drug delivery and tissue engineering. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2016, 8, 654–677. [Google Scholar] [CrossRef] [PubMed]
- Siafaka, P.I.; Barmbalexis, P.; Bikiaris, D.N. Novel electrospun nanofibrous matrices prepared from poly(lactic acid)/poly(butylene adipate) blends for controlled release formulations of an anti-rheumatoid agent. Eur. J. Pharm. Sci. 2016, 88, 12–25. [Google Scholar] [CrossRef] [PubMed]
- Mohammadian, F.; Eatemadi, A. Drug loading and delivery using nanofibers scaffolds. Artif. Cells Nanomed. Biotechnol. 2016, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Yarin, A.L. Coaxial electrospinning and emulsion electrospinning of core-shell fibers. Polym. Adv. Technol. 2011, 22, 310–317. [Google Scholar] [CrossRef]
- McClellan, P.; Landis, W.J. Recent applications of coaxial and emulsion electrospinning methods in the field of tissue engineering. BioRes. Open Access 2016, 5, 212–227. [Google Scholar] [CrossRef] [PubMed]
- Sperling, L.E.; Reis, K.P.; Pranke, P.; Wendorff, J.H. Advantages and challenges offered by biofunctional core-shell fiber systems for tissue engineering and drug delivery. Drug Discov. Today 2016, 21, 1243–1256. [Google Scholar] [CrossRef] [PubMed]
- Schaub, N.J.; Le Beux, C.; Miao, J.; Linhardt, R.J.; Alauzun, J.G.; Laurencin, D.; Gilbert, R.J. The effect of surface modification of aligned poly-l-lactic acid electrospun fibers on fiber degradation and neurite extension. PLoS ONE 2015, 10, e0136780. [Google Scholar] [CrossRef] [PubMed]
- Schaub, N.J.; Gilbert, R.J. Controlled release of 6-aminonicotinamide from aligned, electrospun fibers alters astrocyte metabolism and dorsal root ganglia neurite outgrowth. J. Neural Eng. 2011, 8, 046026. [Google Scholar] [CrossRef] [PubMed]
- Pires, L.R.; Rocha, D.N.; Ambrosio, L.; Pêgo, A.P. The role of the surface on microglia function: Implications for central nervous system tissue engineering. J. R. Soc. Interface 2015, 12. [Google Scholar] [CrossRef] [PubMed]
- Seif, S.; Franzen, L.; Windbergs, M. Overcoming drug crystallization in electrospun fibers—Elucidating key parameters and developing strategies for drug delivery. Int. J. Pharm. 2015, 478, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Downing, T.L.; Wang, A.; Yan, Z.Q.; Nout, Y.; Lee, A.L.; Beattie, M.S.; Bresnahan, J.C.; Farmer, D.L.; Li, S. Drug-eluting microfibrous patches for the local delivery of rolipram in spinal cord repair. J. Control Release 2012, 161, 910–917. [Google Scholar] [CrossRef] [PubMed]
- Stout, D.A. Recent advancements in carbon nanofiber and carbon nanotube applications in drug delivery and tissue engineering. Curr. Pharm. Des. 2015, 21, 2037–2044. [Google Scholar] [CrossRef] [PubMed]
- Su, W.T.; Shih, Y.A. Nanofiber containing carbon nanotubes enhanced PC12 cell proliferation and neuritogenesis by electrical stimulation. Bio. Med. Mater. Eng. 2015, 26, 189–195. [Google Scholar] [CrossRef] [PubMed]
- López-Dolado, E.; González-Mayorga, A.; Gutiérrez, M.C.; Serrano, M.C. Immunomodulatory and angiogenic responses induced by graphene oxide scaffolds in chronic spinal hemisected rats. Biomaterials 2016, 99, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Raspa, A.; Pugliese, R.; Maleki, M.; Gelain, F. Recent Therapeutic Approaches for Spinal Cord Injury. Biotechnol. Bioeng. 2016, 113, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Gelain, F.; Zhao, X. Designer self assembling peptide nanofiber scaffold for 3D tissue cell cultures. Semin Cancer Biol. 2005, 15, 410–420. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Su, H.; Zeng, Y.; Liang, Y.X.; Wong, W.M.; Ellis-Behnke, R.G.; So, K.F.; Wu, W. Reknitting the injured spinal cord by self-assembling peptide nanofiber scaffold. Nanomedicine 2007, 3, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Tysseling-Mattiace, V.M.; Sahni, V.; Niece, K.L.; Birch, D.; Czeisler, C.; Fehlings, M.G.; Stupp, S.I.; Kessler, J.A. Self-assembling nanofibers inhibit glial scar formation and promote axon elongation after spinal cord injury. J. Neurosci. 2008, 28, 3814–3823. [Google Scholar] [CrossRef] [PubMed]
- Gelain, F.; Cigognioni, D.; Caprini, A.; Silva, D.; Colleoni, B.; Donegà, M.; Antonini, S.; Choen, B.E.; Vescovi, A. New bioactive motif and their use in functionalized self-assembling peptides for NSC differentiation and neural tissue engineering. Nanoscale 2012, 4, 2946–2957. [Google Scholar] [CrossRef] [PubMed]
- Tetzlaff, W.; Okon, E.B.; Karimi-Abdolrezaee, S.; Hill, C.E.; Sparling, J.S.; Plemel, J.R.; Plunet, W.T.; Tsai, E.C.; Baptiste, D.; Smithson, L.J.; et al. A systematic review of cellular transplantation therapies for spinal cord injury. J. Neurotrauma 2011, 28, 1611–1682. [Google Scholar] [CrossRef] [PubMed]
- Cigognini, D.; Silva, D.; Paloppi, S.; Gelain, F. Evaluation of mechanical properties and therapeutic effect of injectable self-assembling hydrogels for spinal cord injury. J. Biomed. Nanotechnol. 2014, 10, 309–323. [Google Scholar] [CrossRef] [PubMed]
- Tavakol, S.; Saber, R.; Hoveizi, E.; Tavakol, B.; Aligholi, H.; Ai, J.; Rezayat, S.M. Motif of Laminin Induces Neural Differentiation, Tubulin Polymerization, and Neurogenesis: In Vitro, Ex Vivo, and In Vivo Studies. Mol. Neurobiol. 2016, 53, 5288–5299. [Google Scholar] [CrossRef] [PubMed]
- Gerth, D.J.; Tashiro, J.; Thaller, S.R. Clinical outcomes for conduits and scaffolds in peripheral nerve repair. World J. Clin. Cases 2015, 3, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Goswami, D.; Vitorino, H.A.; Machini, M.T.; Espòsito, B.P. Self-Assembled Penetratin-Deferasirox Micelles as Potential Carriers for Hydrophobic Drug Delivery. Pept. Sci. 2015, 104, 712–719. [Google Scholar] [CrossRef] [PubMed]
- Ninomiya, K.; Iwatsuki, K.; Ohnishi, Y.; Ohkawa, T.; Yoshimine, T. Intranasal delivery of bone marrow stromal cells to spinal cord lesions. J. Neurosurg. Spine 2015, 23, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Lee, H.L.; Yun, Y.; Kim, J.S.; Ha, Y.; Yoon, D.H.; Lee, S.H.; Shin, D.A. Human adipose stem cells improve mechanical allodynia and enhance functional recovery in a rat model of neuropathic pain. Tissue Eng. A 2015, 21, 2044–2052. [Google Scholar] [CrossRef] [PubMed]
- Mehta, T.; Feroz, A.; Thakkar, U.; Vanikar, A.; Shah, V.; Trivedi, H. Subarachnoid placement of stem cells in neurological disorders. Transplant Proc. 2008, 40, 1145–1147. [Google Scholar] [CrossRef] [PubMed]
- Mei, L.; Wang, Y.; Tong, A.; Guo, G. Facile electrospinning of an efficient drug delivery system. Expert Opin. Drug Deliv. 2016, 13, 741–753. [Google Scholar] [CrossRef] [PubMed]
| Name | Mechanism of Action | Effect on SCI |
|---|---|---|
| Atorvastatin (Lipitor) [14] | Reduction of cholesterol levels | Anti-inflammatory effect, anti-apoptosis, tissue sparing and locomotion recovery |
| Calpain inhibitors [15] | Inhibition of cytoskeletal protein degradation and apoptosis | Tissue preservation, locomotion recovery, anti-apoptosis |
| Chicago sky blue [16] | Macrophage migration inhibition | White matter increase and blood vessel integrity recovery |
| Erythropoietin (EPO) [17,18] | Activation of EPO receptor | Anti-inflammatory effect, anti-apoptosis, cytoprotection, vascular integrity recovery, lipid peroxidation inhibition |
| Estrogen [19] | Hormone replacement | Anti-apoptosis, myeloperoxidase activity reduction, microglial/macrophage accumulation |
| C3-exoenzyme, Fasudil, Y27532, Ibuprofen [1] | Rho antagonists | Locomotion recovery |
| Ferulic acid from Ferula species [20] | Antioxidant activity | Anti-inflammatory effect, locomotion recovery, axonal/myelin protection and excitotoxicity prevention |
| FTY720 [21] | Modulation of sphingosine receptor | Anti-inflammatory effect, anti-apoptosis, tissue sparing and locomotion recovery |
| Hydralazine [22,23] | Acrolein scavenger | Neuropathic pain reduction and locomotion recovery |
| Imatinib [24] | Protein-tyrosine kinase inhibitor (clinically used for leukemias and gastrointestinal stromal tumors) | Anti-inflammatory effect, anti-apoptosis, tissue sparing and locomotion recovery |
| Melatonin [25] | Antioxidant activity | Lipid peroxidation reduction, neuro-axonal and blood-spinal cord barrier (BSCB) protection, locomotion recovery |
| Minocycline [19] | Antioxidant activity | Immunomodulation of microglia, excitotoxicity, mitochondrial stabilization, anti-apoptosis |
| NSAIDs [19] | Selective cycloxygenase (COX−2) inhibitors | Anti-inflammatory effect |
| Quercitin, Deferoxamine and Ceruloplasmin [26,27,28] | Ca2+ chelation | Locomotion recovery |
| Riluzole [29] | Blockage of the sodium channels | Intracellular [Na+] and [Ca2+] modulation and excitotoxicity reduction |
| Rolipram [30] | Phosphodiesterase type 4 inhibitor | Anti-inflammatory effect, anti-apoptosis, tissue sparing and locomotion recovery |
| Vitamins C and E [31] | Antioxidant activity | Anti-inflammatory effect |
| Name | Mechanism of Action | Effect on SCI | Administration Route in Animal Models |
|---|---|---|---|
| Allicin [32] | Increase in nuclear factor (erythroid-derived 2)-related Factor-2 (Nrf-2) nuclear translocation in neurons and astrocytes | Neuro-protection, locomotion recovery antioxidant, anti-apoptosis and anti-inflammatory effects | Intraperitoneal injection |
| Aloe vera [33] | Reduction of neuronal nitric oxide synthase (nNOS) and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) protein | Anti-inflammatory, antioxidant, anti-apoptosis | Per os |
| Asiaticoside [34] | Inhibition of p38-mitogen-activated protein kinase (p38-MAPK) signaling pathway | Antioxidant and anti-inflammatory effects | Intraperitoneal injection |
| Buyang Huanwu decoction [35] | Reduction in caspase-3 and Bax expression and increase in Bcl-2 expression | Anti-apoptosis effect and hind-limb motor function recovery | Per os |
| Caffeic acid phenethyl ester (CAPE) [36] | Antioxidant activity | Neuro-protection, anti-apoptosis | Intraperitoneal injection |
| Carnosol [37] | Down-regulation of NF-κB and COX-2 levels and up-regulation of phosphorylated Akt and Nrf-2 expression | Neuro-protection, antioxidant and anti-inflammatory effects | Intraperitoneal injection |
| Crocin from Crocus sativus [38] | Down-regulation of tumor necrosis factor- α (TNF-α) and Interleukin 1β (IL-1β) and antioxidant activity | Neuro-protection and functional recovery in animal SCI | Implantation |
| Curcumin [39,40] | Reduction of inflammatory cytokine expression and antioxidant activity | Neuro-protection, anti-apoptosis, oxidative stress and lipid peroxidation reduction, locomotion recovery | Intraperitoneal injection |
| Docosahexaenoic acid (DHA) [41] | miR-21 and phosphorylated Akt up-regulation and phosphatase and tensin homologue (PTEN) down-regulation | Neuroplasticity enhancement | Tail vein injection |
| (−)-epigallocatechin-3-gallate polyphenol [42] | Down-regulation of Ras homolog gene family, member A (RhoA), fatty acid synthase (FASN) and TNF-α expression | Neuro-protection, reduction of thermal hyperalgesia and of astro- and microglia reactivity | Intraperitoneal injection |
| Glycyrrhizic acid [43] | Reduction of NF-κB and S100B expression | Neuro-protection, lipid peroxidation reduction, anti-necrotic and anti-inflammatory effects | Catheter inserted into the extradurally thoracic |
| Ganoderma lucidum polysaccharides from Basidiomycota [44] | Modulation of caspase-3 and myeloperoxidase activities, reduction of transforming growth factor- α (TGF-α), malondialdehyde and nitric oxide levels | Neuro-protection and functional recovery | Per os |
| Ginkgo biloba extract 761 [45] | Antioxidant, antiapoptosis | Neuro-protection, motor recovery | Intraperitoneal injection |
| Go-sha-jinki-Gan [46] | Anti TNF-α | Neuro-protection, analgesic and anti-necrosis effects | Implantation |
| Herba Lycopodii [47] | Increase of brain derived neurotrophic factor (BDNF) expression | Neuro-protection and motor function improvement | Intragastric injection |
| Mangiferin [48] | Reduction of malondialdehyde (MDA), superoxide dismutase (SOD), catalase (CAT) activities and serum levels of glutathione peroxidase (GSH-PX), NF-κB, TNF-α, IL-1β, modulation of Bcl-2 and Bax pathway | Neuro-protection, antioxidant and anti-inflammatory effects and anti-apoptosis, locomotion recovery | Intraperitonesl injection |
| Rutin [49] | Macrophage inflammatory protein-2 (MIP-2) expression inhibition and matrix metalloproteinase-9 (MMP-9) activation, down-regulation of p-Akt expression | Neuro-protection and locomotion recovery | Intraperitoneal injection |
| Thymoquinone from Nigella sativa [50] | Antioxidant activity, modulation of cytokine, activation of antioxidant enzyme | Neuro-protection, antioxidant activity, anti-inflammatory effect, reduction of motor neuron apoptosis | Intraperitoneal injection |
| Name | Mechanism of Action | Effect on SCI | Administration Route in Animal Models |
|---|---|---|---|
| Acetyl-L-carnitine [51] | Improvement of mitochondria respiration for adenosine tri-phosphate (ATP) production | Protection of endothelial cells of microvessels and locomotor function recovery in lumbar injury | Intrathecal (sub-arachnoid) injection in rats |
| Adalimumab [52] | Antioxidant, TNF-α, IL-1β and IL-6 serum levels | Neuro-protection and anti-inflammatory effect | Subcutaneous injection in compressive spinal cord injury |
| Alpha Lipoic Acid + N-Acetyl Cysteine [53] | TNF-α, IL-6 and malondialdehyde (MDA) inhibitor | Motor recovery and anti-inflammatory and antioxidant effects | Intraperitoneal injection |
| Aspirin [54] | Inhibition of phospholipases, nitric oxide synthetases, and cyclooxygenases | Neuro-protection and, anti-inflammatory effects, lipid peroxidation reduction and locomotion recovery | Intraperitoneal injection |
| Azithromicyn (AZM, macrolide antibiotic) [55] | Reduction of pro-inflammatory macrophage activation | Anti-inflammatory effect, tissue sparing and motor recovery | per os |
| A68930 (Dopamine D1 receptor agonist) [56] | Inhibition of NLRP3 inflammasome activation and reduction of pro-inflammatory cytokines levels and MPO activity | Neuro-protection and anti-inflammatory effect | Intraperitoneal injection |
| cAMP combined with functionalized collagen scaffold [57] | Reduction of cavitation volume, axonal and neuronal regeneration | Neuro-regeneration, remyelination, revascularization and locomotion recovery | Implantation |
| Carvedilol [58] | Increase in SOD and glutathione (GSH), reduction of MPO and malondialdehyde (MDA) | Neuro-protection, antioxidant and anti-apoptosis effects, locomotion recovery | |
| Dexamethasone [59] | Macrophages modulation | Neuro-protection and locomotor recovery | Subdural infusion |
| Dibutyryl cyclic adenosine monophosphate (db-cAMP) [60] | Activation of protein kinase A (PKA) signaling by cAMP-related pathways; reduction of apoptosis | Neuro-regeneration, axonal sprouting, functional recovery and modulation of glial scar formation | Implantation |
| 17β-estradiol (E2) [61] | Down-regulation of LC3II and beclin-1 expression and suppression of excessive autophagy | Neuro-protection and locomotion recovery | Intramuscular injection |
| Estrogen hormone [62] | Reduction of TNF-α and iNOS genes expression | Antioxidant, locomotion recovery and anti-inflammatory effect | Intraperitoneal injection |
| FK506 (Tacrolimus) + Minocycline [63] | Reduction of thiobarbituric acid–reactive species (TBARS), total glutathione (GSH) and MPO activity | Neuro-protection, functional recovery and antioxidant effect | Per os |
| Gp91ds-tat (NOX2-specific inhibitor) [64] | Inhibition of NADPH oxidase (NOX) enzyme (NOX 2 isoform) | Antioxidant and anti-inflammatory effects | Intrathecal injection |
| Histamine H4 receptor agonist [65] | Reduction of IL-1β, TNF-α, 8-hydroxy-2′-deoxyguanosine (8-OHdG) and PARP expression and restoration of MnSOD enzymatic activity | Antioxidant, anti-inflammatory and analgesic effects | Per os |
| Histidine-Tryptophan-Ketoglutarate (HTK) solution [66] | Metabolic regulation and blood-flow maintenance agents | Locomotion recovery, neuro-protection and reduction of ischemia | Infusion into the occluded aortic segment |
| Lipoxin A4 (LXA4) [67] | Reduction of spinal expression levels of microglial markers (IBA-1) and pro-inflammatory cytokines (TNF-α) | Neuro-protection, analgesic and anti-inflammatory effects | Intrathecal injection |
| Melatonin with amniotic epithelial cells (AECs) [68] | Melatonin receptor 1 stimulation and promotion of ARC differentiation into neural cells by Wint-4 gene expression | Neuro-regeneration and locomotion recovery | Injection along the midline of spinal cord |
| Metformin [69] | Reduction of NF-κB expression and caspase 3 activation, autophagy activation via mTOR/p70S6K signaling | Neuro-protection, anti-apoptosis and anti-inflammatory effects in preconditioning treatment | Intraperitoneal injection |
| N-(4-cyanophenylmethy)-4-(2-diphenyl)-1-piperazinehexanamide (LP-211) [70] | Serotonin (5-HT7) selective agonism, hyponatremia, hyperkalemia and hypermagnesemia induction | Modulation of imbalances in serum electrolyte concentration, neuro- and renal tissue protection | Intraperitoneal injection |
| Nor-Binaltorphimine (norBNI) [71] | κ-opioid receptor (KOR) antagonism and morphine antagonism | Locomotion recovery | Intraperitoneal injection |
| PMX53 (C5aR antagonist) [72] | Inhibition of neutrophil infiltration and reduction of MPO activity | Neuro-protection from ischemia-reperfusion injury | Femoral vein injection |
| Progesterone [73] | Modulation of pro-inflammatory cytokine expression | Anti-inflammatory, remyelinating action, and analgesic effects | Subcutaneous injection |
| Propofol [74] | Reduction of superoxide dismutase 1 (SOD1) expression related to PI3K/AKT signal pathway | Reduction of spinal cord ischemia/reperfusion injury and antioxidant effect | intraperitoneal injection in rabbit with ischemia/reperfusion (I/R) spinal cord injury by aortic occlusion |
| Rapamycin [75] | Activation of Wnt/β-catenin pathway | Neuro-protection and locomotion recovery | Intraperitoneal injection |
| Retinoic acid (Vitamin A) [76] | Autophagic flux activation after trauma | Neuro-protection, functional recovery and prevention of BSCB disruption | Intraperitoneal injection |
| Rosiglitazone in combination with MP [77] | Peroxisome proliferator-activated receptor-γ (PPAR-γ) activation | Functional recovery, anti-inflammatory antioxidant and anti-apoptosis effects | Intraperitoneal injection |
| Selenium-enriched supplement (SES) [78] | Up-regulation of ciliary neurotrophic factor (CNTF) and CNTF-Rα expression | Neuro-protection | Per os |
| Simvastatin [79] | Autophagy activation by mTOR signaling pathway inhibition | Neuro-protection | |
| Stat 1 Inhibitor (S1491) [80] | Neuro-protection and anti-apoptosis effect | Intraperitoneal injection | |
| Tamoxifen [81] | Estrogen receptor modulator | Anti-apoptotic, antioxidant, anti-inflammatory, anti barrier permeability and antigliotic effects | |
| Tetramethylpyrazine (TMP) [82] | Activation of Akt/Nrf-2/HO-1 signaling pathway | Neuro-protection, locomotion recovery and reduction of BSCB permeability | Intraperitoneal injection |
| Name | Mechanism of Action | Effect in SCI | Administration Route |
|---|---|---|---|
| Acrolein [84] | Activation of transient receptor protein ankyrin 1 (TRPA1) in both central and peripheral systems | Reduction of both acute and chronic neuropathic pain | Injection in spinal cord |
| Botulinum Toxin type A (BTX-A) [85] | Inhibition of the release of substance P, calcitonin and glutamate | Reduction of chronic neuropathic pain | Subcutaneous injection |
| Cannabis [86] | Reduction of neuropathic pain | Vaporization | |
| GABAergic inhibitors [87] | Reduced neuronal activity in the GABAergic ZI (zona incerta) | Reduction of neuropathic pain | Cannula implantation |
| Methadone [88] | Opioid agonist | Reduction of neuropathic pain during opioid rotation for chronic pain | |
| Morphine [89] | Toll like receptor 4 (TLR4) pathway attivation and allodynia increase shortly after trauma | Prevention of amplified allodyna in a long/term administration | Subcutaneous injection |
| Neurothensin A analogue (CGX-1160) [90] | Reduction of neuropathic pain | Intrathecal injection |
| Name | Mechanism of Action | Effect in SCI | Administration Route |
|---|---|---|---|
| Botulinum toxin A [91] | Upper urinary tract protection, modulation of detrusor overactivity and detrusor external sphincter dyssynergia | Injections into detrusor and external urethral sphincter in humans with suprasacral and sacral injuries | |
| Imidafenacin [92] | Anticholinergics selective for the urinary bladder, detrusor pressure reduction and cystometric volume increase | Urodynamic effects with possibly alleviation of bladder complication | Injections in patients with SCI and low cystometric volume and/or detrusor compliance |
| Inosine [93] | antioxidant by peroxynitrite disattivation, anti-inflammatory, axogenic and neurotrophic properties | Modulation of detrusor overactivity, decrease of non-voiding contraction (NVC), decrease TRPV1 in bladder tissue | Intraperitoneal injection in rat with NVC immediately after SCI |
| Mirabegron [94] | β-3 agonist | Urodynamic improvement | Administered in patients with neurogenic detrusor overactivity (NDO) after SCI |
| Naftopidil/BMY7378/Silodosin (α-adrenoceptor blockers) [95] | α-adrenoceptor blockade | Reduction of urethral resistance, voiding efficiency improvement by external urethral sphincter-electromyography(EMG) | Intravenous injection in rat with chronic SCI |
| Propiverine (antimuscarinic agent) [96] | Antagonism against muscarinic receptor, L-type Ca2+ channels and transient receptor potential vanilloid subtype 1 (TRPV1) | Amelioration of urinary tract dysfunctions and reduction of detrusor overactivity | Administered to rats with SCI and non-voiding contraction (NVC) |
| Materials Employed | Drug Loaded | Potential Effect in SCI |
|---|---|---|
| Ac-FAQ with PCL+ PLGA [110] | - | In vivo nerve regeneration |
| Bombyx mori silk fibroin (SF) [111] | - | In vitro neurite outgrowth and astrocyte migration |
| Chitosan scaffold [112] | - | In vivo functional recovery |
| Collagen type I [113] | In vivo neurite outgrowth and astrocyte migration | |
| Collagen type I [114] | - | In vivo motor recovery |
| Graphene nanoscaffold [115] | - | In vivo biocompatibility and nerve outgrow |
| Multi-layer PCL [116] | - | In vitro axonal regeneration |
| PCL + Gum tragacanth (GT) [117] | Curcumin | In vitro biocompatibility, long-lasting release of drug and wound healing properties |
| Peptide anphiphile (PA) [118] | Dexamethasone | Achievement of long-lasting release of drug and In vivo localized anti-inflammatory effect |
| PCL [119] | Dexamethasone | Achievement of long-lasting release of drug |
| PCL + PLGA functionalized with Ac-FAQ [110] | - | In vivo nerve regeneration |
| PLA [120] | - | In vivo biocompatibility and promotion of spinal cord damage repair |
| PLGA + PCL + (RADA16, a ionic self-complementary peptide) [121] | Cytokines | In vivo axonal regeneration and neurological recovery |
| PLGA [98] | - | In vivo axonal regeneration and motor and sensory recovery |
| PLA + gum tragacanth (PLA/GT) [117] | - | In vitro neurite outgrowth and nerve cell elongation on aligned nanofibers |
| PPC [60] | Dibutyryl cyclic adenosine monophosphate (dbcAMP) | In vivo nerve regeneration, functional recovery and glial scar reduction |
| Poly(trimethylene carbonate-co-ε-caprolactone) [122] | Ibuprofen | In vivo nerve conduit and anti-inflammatory |
| Positively charged oligo[poly(ethylene glycol)fumarate] (OPF+) [123] | - | In vivo axonal regeneration and functional recovery |
| PuraMatrix nanofibrous hydrogel + honeycomb collagen sponge [107] | - | In vivo locomotion functional recovery, spinal repair and neuronal regeneration |
| Electrospun PLGA coated with polypyrrole (PPy) [124] | - | Electrical stimulation and topographical guidance In vitro on PC12 cells improved neurite outgrowth |
| PCL/collagen/nonobioglass(NBG) [125] | - | Human Endometrial Stem cells adhesion and proliferation |
| (Ser-Ile-Lys-Val-Ala-Val)-modified poly(2-hydroxethyl methacrylate) (PHEMA) [126] | - | In vivo tissue bridging and aligned axonal ingrowth |
| Poly(glycerol sebacate) (PGS) + poly(methyl methacrylate) (MMA) with and without gelatin [127] | PC12 cells proliferation | |
| Hyaluronic acid (HA) + PCL [128] | Attachment of SH-SY5Y neuroblastoma cells | |
| SNF coated with poly-d-lysine (PDL) or (3-aminopropyl) trimethoxysilane (APTS) [129] | - | Promotion of In vitro neuron growth and neurite density increase |
| Tussah silk fibroin (TSF) [130] | - | In vitro improvement of olfactory ensheathing cell (OECs) neuro-regenerative potential |
| Gelatin (GL) + polyethylene-oxide (PEO) + (3-Glycidoxypropyl) methyldiethoxysilane(GPTMS) [131] | Schwann cells proliferation | |
| PCL-Chitosan [132] | Laminin | Schwann cells grown |
| Self-Assembling Peptides | Animal Model | Potential Effect in SCI |
|---|---|---|
| Biotin B24 (GGGAFASTKT-CONH2) [166] | Murine contusion model | Low infiltration of CD68 + macrophages and iba + microglia |
| Biotin LDLK12 (LDLKLDLKLDLK-CONH2) [166] | Murine contusion model | Low infiltration of CD68 + macrophages and iba + microglia |
| Laminin epitope CQIK (Ac-(RADA)4GGCQAASIKVAV-CONH2) [167] | Motor recovery in SCI model | Higher neural differentiation of hEnSCs (human endometrial-derived stromal cells,) neurite outgrowth and myelination |
| Laminin epitope IKVAV-peptide amphiphile (PA) [163] | Murine spinal cord contusion and compression model | Promotion of functional recovery |
| SAP: K2(QL)6K2 [139] | Murine model clip compression | Improvement of locomotion function attenuation of inflammation |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faccendini, A.; Vigani, B.; Rossi, S.; Sandri, G.; Bonferoni, M.C.; Caramella, C.M.; Ferrari, F. Nanofiber Scaffolds as Drug Delivery Systems to Bridge Spinal Cord Injury. Pharmaceuticals 2017, 10, 63. https://doi.org/10.3390/ph10030063
Faccendini A, Vigani B, Rossi S, Sandri G, Bonferoni MC, Caramella CM, Ferrari F. Nanofiber Scaffolds as Drug Delivery Systems to Bridge Spinal Cord Injury. Pharmaceuticals. 2017; 10(3):63. https://doi.org/10.3390/ph10030063
Chicago/Turabian StyleFaccendini, Angela, Barbara Vigani, Silvia Rossi, Giuseppina Sandri, Maria Cristina Bonferoni, Carla Marcella Caramella, and Franca Ferrari. 2017. "Nanofiber Scaffolds as Drug Delivery Systems to Bridge Spinal Cord Injury" Pharmaceuticals 10, no. 3: 63. https://doi.org/10.3390/ph10030063







