Safety of Immunosuppressive Drugs Used as Maintenance Therapy in Kidney Transplantation: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Literature Search
2.1. Eligibility Criteria and Study Selection
2.2. Search Strategy
2.3. Selection of Studies and Data Collection
2.4. Quality Assessment
2.5. Data Synthesis and Data Analysis
3. Results
3.1. Study Characteristics


| Study (year) | Treatment | N (female %) | White % | First Transplant % | Deceased Donor % | Cold Ischemia time (SD) | Mean Donor Age (SD) | Mean Age (SD) | Study design, location, time of follow-up and funding |
|---|---|---|---|---|---|---|---|---|---|
| 1. CNI vs. CNI | |||||||||
| 1.Scantleburry (1991) [22] | CsA + Pred TAC + Pred | 20 14 | NR NR | 100 100 | NR NR | NR NR | NR NR | NR NR | RCT, USA, single center, 12 months |
| 2. Mayer (1997) [23] | CsA + AZA + Pred TAC + AZA + Pred | 145 (36.6) 303 (35.3) | NR NR | 89.7 90.4 | 100 100 | NR NR | 43.0 45.2 | 45.8 46.6 | RCT, England, multicenter (15), open label, 12 months, funded by Fujisawa GMBH |
| 3. Yang (1999) [24] | CsA + MMF + Ster TAC + MMF + Ster | 30 (37) 30 (50) | 87.0 77.0 | NR NR | 57.0 67.0 | 15 (1.6) 14 (1.5) | 37 (2.6) 39 (3.0) | 48.0 (2.2) 45.0 (2.4) | RCT, USA, single center, open label, 12 months |
| 4. Wang (2000) [25] | CsA + MMF + Pred TAC + MMF + Pred | 32 25 | NR NR | NR NR | 100 100 | NR NR | NR NR | 38.1 (18.7) | RCT, China, single center, 12 months results |
| 5. Nichelle (2002) [26] | CsA + AZA + Ster TAC + AZA + Ster | 46 48 | NR NR | NR NR | NR NR | NR NR | NR NR | NR NR | RCT, France, single center, 12 and 36 months |
| 6. Campos (2002) [27] | CsA TAC | 81 (44) 85 (52) | NR NR | 94 96 | 52.0 46.0 | NR NR | 37.5(14.3) 36.5(13.7) | 40.9 (12.3) 40.5 (10.7) | RCT, Brazil, multicenter (15), open label, 12 months |
| 7. Murphy (2003) [28] | CsA + Pred + AZA TAC + Pred + AZA | 50 (30.0) 52 (38.5) | NR NR | 88.0 88.0 | 84.0 82.0 | LD:1.7; CAD:19.0; NHBD:15.5; LD: 2.2; CAD:18.7; NHBD:15.1 | LD:49; CAD:44; NHBD:48; LD:45; CAD:39; NHBD:49 | 45.0 (12.0) 45.0 (14.0) | RCT, England, multicenter (2), open label, 12 months |
| 8. Jurewicz (2003) [66] | CsA + AZA + Ster TAC + AZA + Ster | 117 115 | NR NR | NR NR | NR NR | NR NR | NR NR | NR NR | Cohort, United Kingdom, single center, 72months |
| 9. Hardinger (2005) [29] | CsA + AZA + Ster TAC + AZA + Ster | 66 (39) 134 (36) | 79 79 | 100 100 | 51.0 58.0 | 12 (4) 13 (5) | NR NR | 44,0 (13.0) 46,0 (13.0) | RCT, USA, single center, open label, 12 months |
| 10. Fukuhara (2005) [67] | CsA + Pred TAC + Pred | 137 (36.5) 55 (30.9) | NR NR | NR NR | 100 100 | 11.95 (6.12) 12.13 (6.58) | 47 (18) 46 (16) | 44 (9) 42 (11) | Cohort, Japan, single Center, 10 years |
| 11. Silva (2006) [68] | CsA + AZA/MMF TAC + AZA/MMF | 80 (44) 68 (50) | 50 53 | 91 85 | 100 100 | 21 (8) 18 (7) | 34 (14.0) 34 (12.0) | 42 (12.0) 43 (12.0) | Cohort, Brazil, single center, 12 months |
| 12. Silva, Jr. (2007) [30] | CsA + Pred TAC + Pred TAC XL + Pred | 212 (35.5) 212 (35.8) 214 (38.7) | 76.9 71.7 74.8 | 95.8 96.3 96.3 | 47.6 50.0 51.9 | 18.44 (7.11) 19.41 (7.27) 17.88 (7.73) | NR NR NR | 47.6 (13.0) 48.6 (12.9) 47.8 (13.0) | RCT, Brazil, , multicenter (60), open label, 12 months, funded by AstellasPharma US |
| 13. Cheung (2009) [31] | CsA + Pred TAC + Pred | 38 (34.2) 38 (44.8) | 100a 100a | 100 100 | 100 100 | 8.7 (4.6) 9.1 (5.1) | 48.9 (13.2) 48.9 (13.2) | 40.2 (11.7) 41.8 (7.5) | RCT, China, single center, open label, 60 months |
| 14. Vicenti (1996) [32] | CsA TAC | 28 (21.4) 92 (34.8) | 53.6 51.1 | 100 100 | NR NR | NR NR | NR NR | 46.6 44.1 | RCT, USA, multicenter (5), open label, 12 months |
| 2. CNI vs. CNI + AMETAB | |||||||||
| 1. Moreso (1998) [33] | CsA + Pred CsA + MMF(ld) + Pred CsA + MMF + Pred CsA(ld) + MMF + Pred | 27 (48.2) 27 (44.4) 28 (42.9) 15 (33.3) | NR NR NR NR | 37.0 44.4 46.4 93.4 | 100 100 100 100 | NR NR NR NR | 41 (16) 41 (18) 42 (17) 44 (14) | 47 (15) 45 (14) 43 (15) 47 (7) | RCT, Spain, multicenter (2), double blind in the standard dose CsA groups and open label in the low-dose CsA, 24 months |
| 2. Raofi (1999) [34] | CsA + AZA TAC + Pred | 21 (27.7) 14 (22.9) | 100b 100b | 100 100 | 100 100 | 26 (10) 25 (8) | NR NR | 46.0 (11.0) 44.0 (14.0) | RCT, USA, single center, 12 months |
| 3. Sandrini (2000) [35] | CsA + Pred CsA + AZA + Pred | 58 (45.0) 58 (38.0) | NR NR | 100 100 | 100 100 | NR NR | 35 (14) 35 (16) | 42 (11) 44 (10) | RCT, Italy, single center, 60 months |
| 4. Segoloni (2000) [36] [Pascual (2003)] [37] | TAC + Pred TAC + AZA + Pred | 236 (35.2) 239 (35.6) | NR NR | NR NR | 100 100 | 18.0 17.6 | NR NR | 46.0 45.0 | RCT, Italy and Spain, multicenter (36), open label, 12 and 36 months |
| 5. Chang (2001) [38] | TAC + Ster TAC + AZA + Ster | 124 (37.9) 121 (32.2) | 77,4 76,0 | NR NR | NR NR | 20.4 21.3 | NR NR | 48.0 45.0 | RCT, United Kingdom, multicenter (08), open label, 12 months |
| 6. Squiflet (2001) [39] | TAC + Pred TAC + MMF(ld) + Pred TAC + MMF + Pred | 82 (46.3) 79 (32.9) 71 (36.6) | 93.9 97.5 95.8 | 86.6 87.3 90.1 | 100 100 100 | NR NR NR | 45.6 (18.1) 45.6 (16.0) 45.4 (16.9) | 46.6 (14.5) 46.5 (13.3) 48.0 (13.3) | RCT, Belgium, multicenter (16), 12 months, funded by Fujisawa |
| 3. CNI vs. AMETAB | |||||||||
| 1. Hall (1988) [40] | CsA AZA + Pred | 138 (42.8) 138 (45.0) | NR NR | 100 100 | 100 100 | 22.0 22.7 | NR NR | NR NR | RCT, Australia, multicenter (7), 36 months, funded by Sandoz |
| 2. Schnuelle (2001) [41] | CsA + Ster MMF + Ster | 44 (27.3) 40 (45.0) | NR NR | 95,5 97,5 | NR NR | 21.7 (9.0) 21.0 (7.5) | 40.7 (15.3) 47.7 (15.4) | 44.7 (13.3) 51.3 (11.5) | RCT, Germany, multicenter (3), open label,12 months |
| 3. Hamdy (2008) [42] | TAC + SRL + Pred MMF + SRL + Pred | 65 (20.0) 67 (29.8) | NR NR | 100 100 | 0 0 | NR NR | 35.6 (10.3) 36.2 (10.2) | 32.3 (10.3) 31.8 (8.6) | RCT, Egypt, single center, 63 months |
| 4. CNI vs. TOR-I | |||||||||
| 1. Groth (1998) [43] | CsA + AZA + Pred SRL + AZA + Pred | 42 (40.0) 41 (29.0) | 88.0 98.0 | 100 100 | 100 100 | 17.4 (7.2) 18.9 (7.4) | 37.7 (15.9) 44.6 (13.4) | 41.6 (11.8) 47.5 (10.8) | RCT, Sweden, multicenter (11), open label, 12 months |
| 2. Büchler (2007)[44]Lebranchu (2012) [45] | CsA + MMF + Ster SRL + MMF + Ster | 74 (39.2) 71 (38.0) | 95.9 94.4 | 89.2 95.8 | 100 100 | 20.17 (5.46) 19.30 (5.24) | 41.3 (14.0) 38.7 (14.4) | 45.1 (12.4) 45.6 (10.3) | RCT, France, multicenter (13), 12 months, funded by Wyeth |
| 3. Guba (2010) [46] | CsA + MMF + Ster SRL + MMF + Ster | 71 70 | 98.6 98.6 | 89.9 94.4 | 88.4 90.1 | 13.0 (7.0) 12.1 (5.7) | 47.1 (14.3) 46.9 (14.3) | 47.1 (11.1) 47.0 (10.8) | RCT, Germany, multicenter (9), 12 months, funded by Wyeth and Fresenius Biotech |
| 4.Glotz (2010) [47] | TAC + MMF + Ster SRL + MMF + Ster | 70 71 | 91.4 77.5 | 94.3 94.4 | 100 100 | 18 (6) 19 (5) | 45.1 (12.6) 45.2 (13.4) | 46.7 (10.6) 48.5 (9.5) | RCT, France, multicenter (13), 12 months, funded by Wyeth |
| 5. CNI + AMETAB vs. CNI + AMETAB vs. CNI + AMETAB | |||||||||
| 1. Hernandez (2007) [48] | CsA + AZA + Ster CsA + MMF + Ster TAC + MMF + Ster | 80 (26.2) 80 (37.5) 80 (45.0) | NR NR NR | 100 100 100 | 42 50 59 | 20.3 (4) 21.0 (4) 21 (4) | 45 (16) 42 (15) 44 (17) | 47 (12) 48 (14) 47 (11) | RCT, Spain, single center, open label, 24 months, funded by Spanish Health Ministry |
| 6. AMETAB vs. AMETAB | |||||||||
| 1. Keown (1995) [49] | AZA + CsA + Pred MMF + CsA + Pred MMF(hd) + CsA + Pred | 173 (46.2) 166 (33.1) 164 (40.2) | NR NR NR | 10.4 14.46 10.98 | NR NR NR | 20 (7) 21 (9) 20 (7) | 38 (16) 39 (16) 37 (16) | 46 (13) 47 (13) 46 (13) | RCT, Canada, multicenter (21), double blind, 24 months |
| 2. Pescovitz (1998) [50] [Pescovitz (2001)] [51] | AZA + CsA + Ster MMF + CsA + Ster | 108 (40.7) 113 (36.3) | 68.5 21.3 | 87 91 | NR NR | NR NR | NR NR | 43.7 (11.7) 43.1 (11.6) | RCT, USA, multi centric (15), double blind, 12 and 36 months |
| 3. Folkmane (2002) [52] | AZA + CsA + Pred MMF + CsA + Pred | 23 23 | NR NR | NR NR | 100 100 | NR NR | NR NR | 43.2 (12.1) 43.2 (12.1) | RCT, Lithonia, 12 months |
| 4. Sadek (2002) [53] | AZA + CsA + Pred MMF + CsA + Pred | 157 (29.0) 162 (40.1) | 91.4 90.4 | 100 100 | 87 86 | NR NR | NR NR | 43.9 (12.8) 43.9 (13.0) | RCT, United Kingdom, multicenter (28), open label, 12 months, funded by Novartis |
| 7. AMETAB vs. TOR-I | |||||||||
| 1. Vitko (2004) [54] [Vitko (2005)] [55] | MMF + CsA EVR(hd) + CsA EVR(ld) + CsA | 194 198 196 | NR NR NR | 100 100 100 | NR NR NR | NR NR NR | RCT, Czech Republic, multicenter (54), double blind, 12 and 36 months, funded by Novartis | ||
| 2. Lorber (2005) [56] | MMF + CsA + Pred EVR(hd) + Csa + Pred EVR(ld) + CsA + Pred | 196 (32.7) 194 (36.6) 193 (29.5) | 65.8 63.4 70.5 | 100 100 100 | 45.9 51.5 52.3 | CAD:18.6 (6.42); LD:1.3 (1.16); CAD:18.8 (6.43); LD:1.2 (1.14) CAD:19.5 (7.18); LD: 1.4 (3.4) | 36.7 (13.81) 38.4 (13.66) 37.4 (13.55) | 43.4 43.7 43.3 | RCT, Switzerland, multicenter (44), 36 months, funded by Novartis |
| 3. Mendez (2005) [57] | MMF + TAC + Pred SRL + TAC + Pred | 176 (30.1) 185 (33.5) | 54.0 50.8 | NR NR | 64.2 63.2 | 19.8 19.1 | NR NR | 47.8 (12.3) 45.3 (12.4) | RCT, USA, multicenter (27),open label, 12 months, funded by Fujisawa |
| 4. Sampaio (2007) [58] | MMF + TAC + Pred SRL+TAC+Pred | 50 (24.0) 50 (38.0) | 54.0 42.0 | 100 100 | 24.0 24.0 | NR NR | 41.9 (10.5) 41.6 (10.0) | 42.6 (14.2) 37.4 (10.3) | RCT, Brazil, single center, open label, 12 months, funded by Janssen-Cilag |
| 5. Tedesco-Silva (2010) [59]; Cibrik (2013) [60] | MMF EVR EVR(ld) | 277 (31.8) 279 (31.5) 277 (36.5) | 68.6 64.5 69.7 | 100 100 100 | 46.2 45.9 46.6 | NR NR NR | 41.8 (13.6) 41.1 (13.0) 41.4 (13.9) | 47.2 (12.7) 45.3 (13.4) 45.7 (12.7) | RCT, Brazil, multicenter, open label, 12 and 24 months, funded by Novartis |
| 8. CNI vs. CNI vs. TOR-I | |||||||||
| 1. Ekberg (2007) [61]; Ekberg (2009) [62] | CsA(sd) + MMF + Ster CsA(ld) + MMF + Ster TAC(ld) + MMF + Ster SRL(ld) + MMF + Ster | 384 (37.7) 408 (33.6) 403 (34.2) 380 (33.3) | 92.1 92.2 94.0 94.2 | NR NR NR NR | 65.6 64.2 62.8 64.2 | 16.6 (5.5) 16.8 (5.2) 16.5 (5.7) 16.0 (5.8) | 44.6 (15.9) 46.2 (15.1) 45.2 (15.5) 46.0 (14.8) | 45.9 (13.8) 47.2 (13.5) 45.4 (14.7) 44.9 (14.5) | RCT (12 months) and Cohort (36 months), Sweden, multicenter (15), open label, 12 and 36 months, funded by Hoffman-La Roche |
| 9. CNI+AMETAB vs. CNI+TOR-I | |||||||||
| 1.Kumar † (2005) [63] | CsA + MMF CsA + SRL TAC + MMF TAC + SRL | 58 52 50 40 | AA = 0 N − AA = 89 | AA = NR Non – AA = NR | AA = 93 n − AA= 83 | AA = 15.5 (6.8) n − AA = 15.9 (12.1) | AA = 42.0 (16.5) N − AA = 42.3 (19.2) | AA = 52.9 (12.0) n − AA = 53.0 (15.6) | RCT, USA, single center, 12 months |
| 10. TOR-I vs. CNI+TOR-I | |||||||||
| 1. Tedesco-Silva (2010) [64] | SRL SRL+CsA | 102 (36.3) 105 (36.2) | 72.6 62.9 | 98.0 98.1 | 31.4 30.5 | 7.36 (0.99) 7.64 (1.03) | NR NR | 41.5 40.9 | RCT, Brazil, multicenter (9), open label, 12 months, funded by Wyeth |
| 11. CNI+AMETAB vs. CNI vs. AMETAB | |||||||||
| 1. Gheith (2008) [69] | CsA + AZA + Pred CsA + Pred AZA + Pred | 239 (26.36) 75 (42.67) 130 (26.92) | NR NR NR | NR NR NR | 0 0 0 | NR NR NR | 34.0 (9.2) 34.6 (10.3) 33.3 (10.1) | 30.7 (10.1) 28.1 (10.3) 29.8 (7.9) | Cohort, Egypt, single Center, 20 years |
| 12. TOR-I + CNI-Elim vs. TOR-I vs. CNI | |||||||||
| 1. Flechner (2011) [65] | SRL + TAC-Elim SRL + MMF TAC + MMF | 152 (28.3) 152 (27.6) 139 (41.7) | 75.0 77.0 73.4 | 92.8 91.5 92.1 | 60.5 63.2 64.0 | 17.7 (6.7) 17.3 (5.7) 17.4 (6.3) | 43.2 (13.6) 45.5 (14.9) 44.4 (13.9) | 47.9 (13.3) 50.4 (13.0) 48.4 (13.2) | RCT, USA, multicenter (65), open-label, 24 months, funded by Wyeth |
3.2. Outcomes
3.2.1. CNI vs. CNI
| Outcome | Study Design (N) | Time in months | Relative Risk b (95% CI) | Statistics c | |
|---|---|---|---|---|---|
| p | I2 | ||||
| CMV | RCT [23,24,29,61] (1519) | 12 | 0.85 (0.64, 1.15) | 0.30 | 0 |
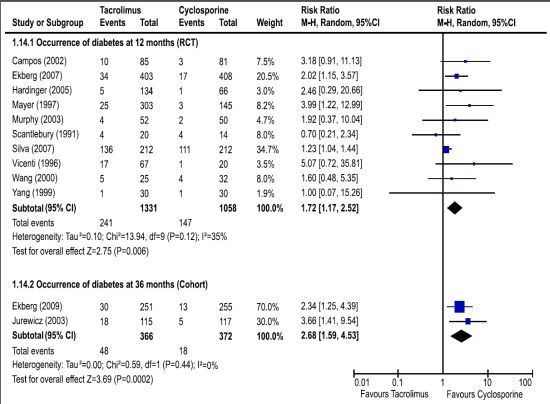
| Diabetes | RCT [22,23,24,25,27,28,29,30,32,61] (2389) | 12 | 1.72 (1.17, 2.52) | 0.006 | 35 |
| Cohort [62,66] (738) | 36 | 2.71 (1.61, 4.57) | 0.0002 | 0 | |
| Dyslipidemia | RCT [29,30,61] (1435) | 12 | 0.75 (0.60, 0.94) | 0.01 | 0 |
| Hypertension | RCT [23,26,27,29,61] (1714) | 12 | 0.97 (0.82, 1.16) | 0.76 | 25 |
| Total Infections | RCT [23,24,25,61] (1376) | 12 | 1.03 (0.93, 1.14) | 0.55 | 12 |
| Lymphoceles | RCT [30,61] (1235) | 12 | 0.61 (0.34, 1.07) | 0.09 | 10 |
| Malignancies | RCT [23,29,61] (1459) | 12 | 1.16 (0.40, 3.38) | 0.79 | 0 |
| Withdraw | RCT [23,24,27,28,29,30,32,61] (2384) | 12 | 0.98 (0.34, 2.81) | 0.97 | 82 * |

3.2.2. AMETAB vs. AMETAB
| Outcome | Study Design (N) | Time in months | Relative Risk b | Statistics c | |
|---|---|---|---|---|---|
| (95% CI) | p | I2 | |||
| Total Infections | RCT [49,51,52,53] (919) | 12 | 1.17 (1.03, 1.33) | 0.01 | 0 |
| CMV | RCT [49,51,52,53] (919) | 12 | 0.94 (0.82, 1.03) | 0.17 | 41 |
| Abdominal pain | RCT [49,50,53] (873) | 12 | 1.40 (1.06, 1.83) | 0.02 | 14 |
| Diarrhea | RCT [49,50,53] (873) | 12 | 1.49 (1.17, 1.90) | 0.001 | 10 |
| Nausea | RCT [49,50,53] (873) | 12 | 0.98 (0.69, 1.39) | 0.91 | 41 |
| Vomiting | RCT [49,50,53] (873) | 12 | 1.54 (1.10, 2.15) | 0.01 | 0 |
| Malignancies | RCT [49,53] (652) | 12 | 1.52 (0.81, 2.82) | 0.19 | 0 |
| Withdraw | RCT [49,50,53] (873) | 12 | 1.21 (0.77, 1.92) | 0.40 | 66* |
3.2.3. TOR-I vs. CNI
| SRL vs. CsA | SRL vs. TAC | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Study Design (N) | Time (mo.) | Relative Risk b (95% CI) | Statistics c | Study Design (N) | Time (mo.) | Relative Risk b (95% CI) | Statistics c | ||
| p | I2% | p | I2% | |||||||
| Total Infections | RCT [46,61] (927) | 12 | 0.98 (0.82, 1.18) | 0.86 | 33 | − | − | − | − | − |
| CMV | RCT [43,44,46,61] (1,155) | 12 | 0.46 (0.25, 0.85) | 0.01 | 53 d | RCT [47,61] (924) | 12 | 0.26 (0.03,2.30) | 0.23 | 79 |
| UTI | RCT [43,44,46,61] (1,155) | 12 | 1.04 (0.79, 1.37) | 0.79 | 35 | − | − | − | − | − |
| Anemia | RCT [43,46,61] (1,010) | 12 | 1.48 (1.16, 1.90) | <0.01 | 0 | RCT [47,61] (924) | 12 | 1.56 (1.26,1.93) | <0.01 | 0 |
| Leukopenia | RCT [43,46,61] (1,010) | 12 | 1.32 (0.70, 2.47) | 0.39 | 57 e | RCT [47,61] (924) | 12 | 0.82 (0.59,1.14) | 0.24 | 0 |
| Dyslipidemia | RCT [43,46,61] (1,010) | 12 | 2.02 (1.03, 3.97) | 0.04 | 65 f | RCT [47,61] (924) | 12 | 1.58 (1.10,2.26) | 0.01 | 0 |
| Diabetes | RCT [43,44,46,61] (1,155) | 12 | 1.82 (1.14, 2.89) | 0.05 | 0 | RCT [47,61] (924) | 12 | 0.78 (0.52,1.17) | 0.23 | 0 |
| Hypertension | RCT [43,46,61] (1,010) | 12 | 0.94 (0.66, 1.33) | 0.71 | 28 | RCT [47,61] (924) | 12 | 1.53 (0.55,4.23) | 0.41 | 93 |
| Lymphoceles | RCT [44,46,61] (1,072) | 12 | 1.65 (1.10, 2.46) | 0.01 | 18 | RCT [47,61] (924) | 12 | 2.92 (1.73,4.93) | <0.01 | 0 |
| Malignancies | RCT [43,61] (871) | 12 | 1.09 (0.09,13.46) | 0.95 | 60 | − | − | − | − | − |
| Withdraw | RCT [43,44,46,61] (1,155) | 12 | 3.68 (2.22, 6.11) | <0.01 | 0 | RCT [47,61] (924) | 12 | 4.31 (2.32,7.99) | <0.01 | 0 |
3.2.4. CNI + AMETAB vs. CNI
| Outcome | Study Design (N) | Time in months | Relative Risk b (95% CI) | Statistics c | |
|---|---|---|---|---|---|
| p | I2 | ||||
| Total Infections | RCT [36,38] (720) | 12 | 0.99 (0.82, 1.20) | 0.94 | 0 |
| Leukopenia | RCT [36,38] (720) | 12 | 8.41 (3.36, 21.02) | <0.01 | 0 |
| Diabetes mellitus | RCT [36,38] (720) | 12 | 0.85 (0.41, 1.76) | 0.67 | 0 |
| Hypertension | RCT [36,38] (720) | 12 | 0.83 (0.65, 1.06) | 0.13 | 0 |
| Tremor | RCT [36,38] (720) | 12 | 0.96 (0.68, 1.35) | 0.82 | 0 |
| Withdraw | RCT [36,38] (720) | 12 | 10.39 (4.40, 24.56) | <0.01 | 0 |
3.2.5. TOR-I vs. AMETAB
3.2.6. AMETAB vs. CNI
4. Conclusions
| Outcome | EVL (ld) vs. MMF | EVL (hd) vs. MMF | SRL vs. MMF | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study Design (N) | Time (mo.) | Relative Risk b (95% CI) | Statistics c | Study Design (N) | Time (mo.) | Relative Risk b (95% CI) | Statistics c | Study Design (N) | Time (mo.) | Relative Risk b (95% CI) | Statistics c | ||||
| p | I2 | p | I2 | p | I2 | ||||||||||
| Total Infections | RCT [54,59] (946) | 12 | 0.62 (0.26, 1.48) | 0.28 | 92 | RCT [54,59] (946) | 12 | 0.83 (0.58, 1.18) | 0.29 | 70 | − | − | − | − | − |
| CMV infections | RCT [54,59] (946) | 12 | 0.23 (0.12, 0.42) | <0.01 | 0 | RCT [54,59] (946) | 12 | 0.15 (0.01, 2.17) | 0.16 | 73 | − | − | − | − | − |
| RCT [55,56] (781) | 36 | 0.47 (0.16, 1.41) | 0.18 | 78 | RCT [55,56] (780) | 36 | 0.47 (0.29, 0.74) | <0.01 | 0 | ||||||
| Anemia | RCT [54,59] (946) | 12 | 0.97 (0.79, 1.20) | 0.80 | 0 | RCT [54,59] (946) | 12 | 1.15 (0.95, 1.40) | 0.15 | 0 | − | − | − | − | − |
| RCT [55,56] (781) | 36 | 1.17 (0.73, 1.88) | 0.50 | 76 | RCT [55,56] (780) | 36 | 1.47 (0.97, 2.23) | 0.07 | 74 | ||||||
| Leukopenia | RCT [55,56] (781) | 36 | 0.50 (0.24, 1.06) | 0.07 | 42 | − | − | − | − | − | − | − | − | − | − |
| Dyslipidemia | RCT [54,59] (946) | 12 | 1.68 (1.01, 2.79) | 0.05 | 68 | RCT [54,59] (946) | 12 | 1.63 (1.08, 2.46) | 0.02 | 52 | − | − | − | − | − |
| Hypertension | RCT [54,59] (946) | 12 | 0.98 (0.73, 1.32) | 0.87 | 0 | RCT [54,59] (946) | 12 | 0.97 (0.80, 1.18) | 0.78 | 0 | − | − | − | − | − |
| Lymphoceles | RCT [55,56] (781) | 36 | 1.54 (0.96, 2.45) | 0.07 | 14 | RCT [55,56] (780) | 36 | 2.08 (1.00, 4.32) | 0.05 | 63 | − | − | − | − | − |
| Withdraw | RCT [55,56] (781) | 36 | 1.23 (1.07, 1.43) | 0.005 | 0 | RCT [55,56] (780) | 36 | 1.41 (1.23, 1.62) | <0.01 | 0 | RCT [57,58] (459) | 12 | 1.81 (1.20, 2.72) | 0.004 | 0 |
Acknowledgments
Conflicts of Interest
References
- Levey, A.S.; Coresh, J.; Balk, E.; Kausz, A.T.; Levin, A.; Steffes, M.W.; Hogg, R.J.; Perrone, R.D.; Lau, J.; Eknoyean, G. National Kidney Foundation practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Ann. Intern. Med. 2003, 139, 137–147. [Google Scholar] [CrossRef]
- Coresh, J.; Selvin, E.; Stevens, L.A.; Manzi, J.; Kusek, J.W.; Eggers, P.; van Lente, F.; Levey, A.S. Prevalence of chronic kidney disease in the United States. JAMA 2007, 298, 2038–2046. [Google Scholar] [CrossRef]
- Zhang, Q.L.; Rothenbacher, D. Prevalence of chronic disease in population-based studies: Systematic review. BMC Public Health 2008, 8, 117. [Google Scholar] [CrossRef]
- Nagata, M.; Ninomiya, T.; Doi, Y.; Yonemoto, K.; Kubo, M.; Hata, J.; Tsuruya, K.; Iida, M.; Kiyohara, Y. Trends in the prevalence of chronic kidney disease and its risk factors in a general Japanese population: The Hisayama study. Nephrol. Dial. Transplant. 2010, 25, 2557–2564. [Google Scholar] [CrossRef]
- Van Pottelbergh, G.; Bartholomeeusen, S.; Buntinx, F.; Degryse, J. The prevalence of chronic kidney disease in a Flemish primary care morbidity register. Age Ageing 2011, 41, 231–233. [Google Scholar]
- Muntner, P.; Newsome, B.; Kramer, H.; Peralta, C.A.; Kim, Y.; Jacobs, D.R., Jr.; Kiefe, C.I.; Lewis, C.E. Racial Differences in the Incidence of Chronic Kidney Disease. Clin J. Am. Soc. Nephrol. 2011, 7, 101–107. [Google Scholar]
- McCullough, K.; Sharma, P.; Ali, T.; Khan, I.; Smith, W.C.S.; MacLeod, A.; Black, C. Measuring the population burden of chronic kidney disease: A systematic literature review of the estimated prevalence of impaired kidney function. Nephrol. Dial. Transplant. 2012, 27, 1812–1821. [Google Scholar] [CrossRef]
- Levey, A.S.; Atkins, R.; Coresh, J.; Cohen, E.P.; Collins, A.J.; Eckardt, K.U.; Nahas, M.E.; Jaber, B.L.; Jadoul, M.; Levin, A.; et al. Chronic kidney disease as a global public health problem: Approaches and initiatives—A position statement from Kidney Disease Improving Global Outcomes. Kidney Int. 2007, 72, 247–259. [Google Scholar] [CrossRef]
- Cusumano, A.M.; Gonza´lez Bedat, M.C. Chronic Kidney Disease in Latin America: Time to improve screening and detection. Clin. J. Am. Soc. Nephrol. 2008, 3, 594–600. [Google Scholar] [CrossRef]
- Port, F.K.; Wolfe, R.A.; Mauger, E.A.; Berling, D.P.; Jiang, K. Comparison of survival probabilities for dialysis patients vs. cadaveric renal transplantation recipients. JAMA 1993, 270, 1339–1343. [Google Scholar] [CrossRef]
- Evans, R.W.; Manninen, D.L.; Garrison, L.P.; Hart, L.G; Blagg, C.R.; Gutman, R.A.; Hull, A.R.; Lowrie, E.G. The quality of life of patients with end-stage renal disease. N. Engl. J. Med. 1985, 312, 553–559. [Google Scholar] [CrossRef]
- Eggers, P.W. Effect of transplantation on the Medicare End-Stage Renal Disease Program. N. Engl. J. Med. 1988, 318, 223–229. [Google Scholar] [CrossRef]
- National Kidney and Urologic Diseases Information Clearinghouse. Kidney and Urologic Diseases Statistics for the United States. Available online: http://kidney.niddk.nih.gov/kudiseases/pubs/kustats/ (accessed on 1 May 2012).
- Kidney Disease: Improving Global Outcomes (KDIGO). Clinical practice guideline for the care of kidney transplant recipients. Am. J. Transplant. 2009, 9, S1–S155.
- Sprangers, B.; Kuypers, D.R.; Vanrenterghem, Y. Immunosuppression: Does on regimen fit all? Transplantation 2011, 92, 251–261. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Loannidis, J.P.A.; Clarke, M.; Devereaux, J.K.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, 7:1–7:28. [Google Scholar]
- Woodroffe, R.; Yao, G.L.; Meads, C.; Bayliss, S.; Ready, A.; Raftery, J.; Taylor, R.S. Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: A systematic review and modelling study. Health Technol. Assess. 2005, 9, 21:1–21:179. [Google Scholar]
- Webster, A.C.; Woodroffe , R.C.; Taylor, R.S.; Chapman, J.R.; Craig, J.C. Tacrolimo versus ciclosporin as primary immunosuppression for kidney transplant recipients: Meta-analysis and meta-regression of randomised trial data. BMJ 2005, 331, 810:1–810:11. [Google Scholar]
- Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. Available online: www.cochrane-handbook.org/ (accessed on 24 June 2013).
- Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm/ (accessed on 6 August 2010).
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Scantleburry, V.; Shapiro, R.; Fung, J.; Tzakis, A.; McCauley, J.; Jordan, M.; Jensen, C.; Hakala, T.; Simmons, R.; Starzi, T.E. New onset of diabetes in FK 506 vs. cyclosporine-treated kidney transplant recipients. Transplant. Proc. 1991, 23, 3169–3170. [Google Scholar]
- Mayer, A.D.; Dmitrewski, J.; Squifflet, J.P.; Bese, T.; Grabensee, B.; Klein, B; Eigler, F.W.; Heemann, U.; Pichlmayr, R.; Behrend, M. Multicenter randomized trial comparing tacrolimus (FK506) and cyclosporine in the prevention of renal allograft rejection: A report of the European Tacrolimus Multicenter Renal Study Group. Transplantation 1997, 64, 436–443. [Google Scholar] [CrossRef]
- Yang, H.C.; Holman, M.J.; Langhoff, E.; Ulsh, P.J.; Dellock, C.A.; Gupta, M.; Ahsan, N. Tacrolimus/“low-dose” mycophenolate mofetil versus microemulsion cyclosporine/“low-dose” mycophenolate mofetil after kidney transplantation: 1-year follow-up of a prospective, randomized, clinical trial. Transplant. Proc. 1999, 31, 1121–1124. [Google Scholar] [CrossRef]
- Wang, X.H.; Tang, X. D.; Xu, D. Tacrolimus vs. Cya Neoral in Combination with MMF and steroid after cadaveric renal transplantation. Transplant. Proc. 2000, 32, 1702–1703. [Google Scholar] [CrossRef]
- Nichelle, L.; Canet, S.; Garrigue, V.; Chong, G.; Mourad, G. Arterial hypertension in renal transplant recipients treated with tacrolimus or cyclosporine-Neoral. Transplant. Proc. 2002, 34, 2824–2825. [Google Scholar] [CrossRef]
- Campos, H.H.; Abbud, M.F. One-year follow-up of a brazilian randomized multicenter study comparing tacrolimus versus cyclosporine in kidney transplantation. Transplant. Proc. 2002, 34, 1656–1658. [Google Scholar] [CrossRef]
- Murphy, G.J.; Waller, J.R.; Sandford, R.S.; Furness, P.N.; Nicholson, M.L. Randomized clinical trial of the effect of microemulsion cyclosporine and tacrolimus on renal allograft fibrosis. Br. J. Surg. 2003, 90, 680–686. [Google Scholar] [CrossRef]
- Hardinger, K.L.; Bohl, D.L.; Schnitzler, M.A.; Lockwood, M.; Storch, G.A.; Brennan, D.C. A randomized, prospective, pharcoeconomic trial of tacrolimus versus cyclosporine in combination with thymoglobulin in renal transplant recipients. Transplantation 2005, 80, 41–46. [Google Scholar] [CrossRef]
- Silva, H.T., Jr.; Yang, H.C.; Abouljoud, M.; Kuo, P.C.; Wisemandle, K.; Bhattacharya, P.; Dhadda, S.; Holman, J.; Fitzsimmoms, W.; First, M.R. One-year results with extended-release tacrolimus/MMF, tacrolimus/MMF and cyclosporine/MMF in de novo kidney transplant recipients. Am. J. Transplant. 2007, 7, 595–608. [Google Scholar] [CrossRef]
- Cheung, C.Y.; Chan, H.W.; Liu, Y.L.; Chau, K.F.; Li, C.S. Long-term graft function with tacrolimus and cyclosporine in renal transplantation: Paired kidney analysis. Nephrology 2009, 14, 758–763. [Google Scholar] [CrossRef]
- Vicenti, F.; Laskow, D.A.; Neylan, J.F.; Mendez, R.; Matas, A.J. One-year follow-up of an open-label trial of Fk506 for primary kidney transplantation: A report of the U.S. multicenter fk506 kidney transplant group. Transplantation 1996, 61, 1576–1581. [Google Scholar] [CrossRef]
- Moreso, F.; Serón, D.; Morales, J.M.; Cruzado, J.M.; Gil-Vernet, S.; Pérez, J.L.; Fulladosa, X.; Andrés, A.; Grinyó, J.M. Incidence of leucopenia and citomegalovirus disease in kidney transplants treated with mycophenolate mofetil combined with low cyclosporine and steroid doses. Clin. Transplant. 1998, 12, 198–205. [Google Scholar]
- Raofi, V.; Holman, D.M.; Coady, N.; Vazquez, E.; Dunn, T.B.; Bartholomew, A.M.; Pollak, R.; Benedetti, E. A prospective randomized trial comparing the efficacy of tacrolimus versus cyclosporine in black recipients of primary cadaveric renal transplants. Am. J. Surg. 1999, 177, 299–302. [Google Scholar] [CrossRef]
- Sandrini, S.; Maiorca, R.; Scolari, F.; Cancarini, G.; Setti, G.; Gaggia, P.; Cristinelli, L.; Zubani, R.; Bonardelli, S.; Maffeis, R.; et al. A prospective randomized trial on azathioprine addition to cyclosporine versus cyclosporine monotherapy at steroid withdrawal, 6 months after renal transplantation. Transplantation 2000, 69, 1861–1867. [Google Scholar] [CrossRef]
- Segoloni, G.; Bonomini, V.; Maresca, M.C.; Arisi, L.; Gonzales-Molina, M.; Tarantino, A.; del Castillo, D.; Ortuño, J.; Carmellini, M.; Capdevila, L.; et al. Tacrolimus is highly effective in bith dual and triple therapy regimens following renal transplantation. Transpl. Int. 2000, 13, S336–S340. [Google Scholar]
- Pascual, J.; Segoloni, G.; Gonzales-Molina, G.; del Castillo, D.; Capdevila, L.; Arias, M.; Garcia, J.; Ortuño, J. Comparison between a two-drug regimen with tacrolimus and steroids and a triple one with azathioprine in kidney tansplantation: Results of a European Trial with 3-year follow up. Transplant. Proc. 2003, 35, 1701–1703. [Google Scholar] [CrossRef]
- Chang, R.W.S.; Snowden, S.; Palmer, A.; Kwan, J.T.C.; Nocholson, M.; Kashi, S.H.; Fernando, O.N.; Perner, F.; Neild, G.H. European randomized trial of dual versus triple tacrolimus-based regimens for controlof acute rejection in renal allograft recipients. Transpl. Int. 2001, 14, 384–390. [Google Scholar] [CrossRef]
- Squifflet, J.P.; Bäckman, L.; Claesson, K.; Dieth, K.H.; Ekberg, H.; Dorsythe, J.L.R.; Kunsendorf, U.; Heemann, U.; Land, W.; Morales, J.M.; et al. Dose Optimization of a Micophenolate Mofetil when administered with a low dose of tacrolimus in cadaveric renal transplant recipients. Transplantation 2001, 72, 63–69. [Google Scholar] [CrossRef]
- Hall, B.M.; Tiller, D.J.; Hardie, I.; Mahony, J.; Mathew, T.; Thatcher, G.; Miach, P.; Thomson, N.; Sheil, A.G. Comparison of three immunosuppressive regimens in cadaver renal transplantation: Long-term cyclosporine, short-term cyclosposrine followed by azathioprine and prednisolone, and azathioprine and prednisolone without cyclosporine. N. Engl. J. Med. 1988, 318, 1499–1507. [Google Scholar] [CrossRef]
- Schnuelle, P.; van der Heide, J.H.; Tegzess, A.; Verburgh, C.A.; Paul, L.C.; van der Woude, F.J.; de Fijter, J.W. Open randomized trial comparing early withdrawal of either cyclosporine or micophenolate mofetil in stable renal transplant recipients initially treated with a triple drug regimen. J. Am. Soc. Nephrol. 2002, 13, 536–543. [Google Scholar]
- Hamdy, A.F.; Bakr, M.A.; Ghoneim, M.A. Long-term efficacy and safety of a calcineurin inhibitor-free regimen in live-donor renal transplant recipients. J. Am. Soc. Nephrol. 2008, 19, 1225–1232. [Google Scholar] [CrossRef]
- Groth, C.G.; Bäckman, L.; Morales, J.M.; Kreis, H.; Lang, P.; Touraine, J.L.; Claesson, K.; Campistol, J.M.; Durand, D.; Wramner, L.; et al. Sirolimus (rapamycin)-based therapy in human renal transplantation: Similar efficacy and different toxicity compared with cyclosporine. Transplantation 1999, 67, 1036–1042. [Google Scholar] [CrossRef]
- Büchler, M.; Caillard, S.; Barbier, S.; Thervet, E.; Toupance, O.; Mazouz, H.; de Ligny, D.H.; Le Meur, Y.; Thierry, A.; Villemain, F.; et al. Sirolimus versus cyclosporine in kidney recipients receiving thymoglobulin, mycophenolate mofetil and a 6-month course of steroids. Am. J. Transplant. 2007, 7, 2522–2531. [Google Scholar] [CrossRef]
- Lebranchu, Y.; Snanoudj, R.; Toupance, O.; Weestel, P.F.; Hurault de Ligny, B.; Buchler, M.; Rerolle, J.P.; Thierry, A.; Moulin, B.; Subra, J.F.; et al. Five-year results of a randomized trial comparing de novo sirolimus and cyclosporine in renal transplantation: The SPIESSER study. Am. J. Transplant. 2012, 12, 1801–1810. [Google Scholar] [CrossRef]
- Guba, M.; Pratschke, J.; Hugo, C.; Krämer, B.K.; Nohr-Westphal, C.; Brockman, J.; Andrassy, J.; Reinke, P.; Pressmar, K.; Hakenberg, O.; et al. Renal function, efficacy, and safety of sirolimus ans mycophenolate mofetil after short-term calcineurin inhibitor-based quadruple therapy in de novo renal transplant patients: One-year analysis of a randomized multicenter trial. Tansplantation 2010, 90, 175–183. [Google Scholar]
- Glotz, D.; Charpentier, B.; Abramovicz, D.; Lang, P.; Rostaing, L.; Rifle, G.; Vanrenterghem, Y.; Bethous, F.; Bourbigot, B.; Delahousse, M.; et al. Thymoglobulin induction and sirolimus versus tacrolimus in kidney transplant recipients receiving mycophenolate mofetil and steroids. Transplantation 2010, 89, 1511–1517. [Google Scholar] [CrossRef]
- Hernández, D.; Miquel, R.; Porrini, E.; Fernández, A.; González-Posada, J.; Hortal, L.; Checa, M.D.; Rodríguez, A.; García, J.J.; Rufino, M.; et al. Randomized controlled study comparing reduced calcineurin inhibitors exposure versus standard cyclosporine-based immunosuppression. Transplantation 2007, 84, 706–714. [Google Scholar] [CrossRef]
- Keown, P.; Häyry, P.; Mathew, T.; Morris, P.; Stiller, C.; Barker, C.; Carr, L. A blinded, randomized clinical trial of mycophenolate mofetil for the prevention of acute rejection in cadaveric renal transplantation. The tricontinental mycophenolate mofetil renal transplantation study group. Transplantation 1996, 61, 1029–1037. [Google Scholar] [CrossRef]
- Pescovitz, M.; Conti, D.; Greenstein, S.M.; Inokuchi, S.; Rosenthal, J.; Cohen, D.; Stiller, C.; Pirsch, J.; Tomlanovich, S.; Cho, S.; et al. Mycophenolate Mofetil for The Treatment of a first acute renal allograft rejection. The tricontinental mycophenolate mofetil renal transplantation study group. Transplantation 1998, 65, 235–241. [Google Scholar]
- Pescovitz, M.; Conti, D.; Greenstein, S.M.; Inokuchi, S.; Rosenthal, J.; Cohen, D.; Stiller, C.; Pirsch, J.; Tomlanovich, S.; Cho, S.; et al. Mycophenolate mofetil for the treatment of a first acute renal allograft rejection: Three-year follow-up. The mycophenolate mofetil acute renal rejection study group. Transplantation 2001, 71, 1091–1097. [Google Scholar] [CrossRef]
- Folkmane, I.; Bicans, J.; Chapenko, S.; Murovska, M.; Rosentals, R. Results of renal transplantation with different immunosuppressive regimens. Transplant. Proc. 2002, 34, 558–559. [Google Scholar] [CrossRef]
- Sadek, S.; Medina, J.; Arias, M.; Sennesael, J.; Squifflet, J.P.; Vogt, B. Short-term combination of mycophenolate mofetil with cyclosporine as a therapeutic option for renal transplant recipients. Transplantation 2002, 74, 511–517. [Google Scholar] [CrossRef]
- Vítko, S.; Margreiter, R.; Weimar, W.; Dantal, J.; Viljoen, H.G.; Li, Y.; Jappe, A.; Cretin, N. Everolimus (Certican) 12-month safety efficacy versus mycophenolate mofetil in de novo renal transplant recipients. Transplantation 2004, 78, 1532–1540. [Google Scholar] [CrossRef]
- Vítko, S.; Margreiter, R.; Weimar, W.; Dantal, J.; Kuypers, D.; Winkler, M.; Oyen, O.; Viljoen, H.G.; Filiptsev, P.; Sadek, S.; et al. Three-year efficacy and safety results form a study of everolimus versus mycophenolate mofetil in de novo renal transplant patients. Am. J. Transplant. 2005, 5, 2521–2530. [Google Scholar] [CrossRef]
- Lorber, M.I.; Mulgaonkar, S.; Butt, K.M.H.; Elkhammas, E.; Mendez, R.; Rajagopalan, P.R.; Kahan, B.; Solinger, H.; Li, Y.; Cretin, N.; et al. Everolimus versus mycophenolate mofetil in the prevention of rejection in de novo renal transplant recipients: A 3-year randomized, multicenter phase III study. Transplantation 2005, 80, 244–252. [Google Scholar] [CrossRef]
- Mendez, R.; Gonwa, T.; Yang, H.C.; Weinstein, S.; Jensik, S.; Steinberg, S. A prospective, randomized trial of tacrolimus in combination with sirolimus or mycophenolate mofetil in kidney transplantation: Results at 1 year. Transplantation 2005, 80, 303–309. [Google Scholar] [CrossRef]
- Sampaio, E.L.; Pinheiro-Machado, P.G.; Garcia, R.; Felipe, C.R.; Park, S.I.; Casarini, D.E.; Moreira, S.; Franco, M.F.; Tedesco-Silva, H., Jr.; Medina-Pestana, J.O. Mycophenolate mofetil vs. sirolimus in kidney transplant recipients receiving tacrolimus-based immunosuppressive regimen. Clin. Transplant. 2008, 22, 141–149. [Google Scholar]
- Tedesco-Silva, H., Jr.; Cibrik, D.; Johnston, T.; Lackova, E.; Mange, K.; Pamos, C.; Walker, R.; Wang, Z.; Zibari, G.; Kim, Y.S. Everolimus plus reduced-exposure CsA versus mycophenolic acid plus standard exposure CsA in renal-transplant patients. Am. J. Transplant. 2010, 10, 1401–1413. [Google Scholar] [CrossRef]
- Cibrik, D.; Silva, H.T., Jr; Vathsala, A.; Lackova, E.; Cornu-Artis, C.; Walker, RG.; Wang, Z.; Zibari, G.B.; Shihab, F.; Kim, Y.S. Randomized trial of everolimus-facilitated calcineurin inhibitor minimization over 24 months in renal transplantation. Transplantation 2013, 95, 933–942. [Google Scholar] [CrossRef]
- Ekberg, H.; Tedesco-Silva, H.; Demirbas, A.; Vitko, S.; Nashan, B.; Gürkan, A.; Margreiter, R.; Hugo, C.; Grinyó, J.M.; Frei, U.; et al. Reduced exposure to calcineurin inhibitors in renal transplantation. N. Engl. J. Med. 2007, 357, 2562–2575. [Google Scholar] [CrossRef]
- Ekberg, H.; Bernasconi, C.; Tedesco-Silva, H.; Vitko, S.; Hugo, C.; Demirbas, A.; Acevedo, R.R.; Grinyó, J.; Frei, U.; Vamrenterghem, Y.; et al. Calcineurin inhibitor minimization in the Symphony Study: Observational results 3 years after transplantation. Am. J. Transplant. 2009, 9, 1876–1885. [Google Scholar] [CrossRef]
- Kumar, M.S.A.; Moritz, M.J.; Saaed, M.I.; Heifets, M.; Sustento-Reodica, N.; Fyfe, B.; Kumar, A. Avoidance of chronic steroid therapy in african american kidney transplant recipients monitored by surveilance biopsy: 1-year results. Am. J. Transplant. 2005, 5, 1976–1985. [Google Scholar] [CrossRef]
- Tedesco-Silva, H.; Garcia, V.D.; Contieri, F.L.C.; Carvalho, D.B.M.; Noronha, I.L.; Gonçalves, R.T.; de Paula, F.J.; Abbud-Filho, M.; Manfro, R.C.; David-Neto, R. Comparison of the safety and efficacy of cyclosporine minimization versus cyclosporine elimination in de novo renal allograft patients receiving sirolimus. Transplant. Proc. 2010, 42, 1659–1666. [Google Scholar] [CrossRef]
- Flechner, S.M.; Glyda, M.; Cockfield, S.; Grinyó, J.; Legendre, C.; Russ, G.; Steinberg, S.; Wissing, K.M.; Tai, S.S. The ORION study: Comparison of two sirolimus-based regimens versus tacrolimus and mycophenolate mofetil in renal allograft recipients. Am. J. Transplant. 2011, 11, 1633–1644. [Google Scholar] [CrossRef]
- Jurewicz, W.A. Tacrolimus versus ciclosporin immunosuppression: Long-term outcome in renal transplantation. Nephrol. Dial. Transplant. 2003, 18, i7–i11. [Google Scholar] [CrossRef]
- Fukuhara, N.; Ono, Y.; Hattori, R.; Nishiyama, N.; Yamada, S.; Kamihira, O.; Kinukawa, T.; Ohshima, S. The long-term outcome of tacrolimus in cadaveric kidney transplantation form non-heart beating donors. Clin. Transplant. 2005, 19, 153–157. [Google Scholar] [CrossRef]
- Silva, L.A.; Felipe, C.R.; Park, S.I.; Pinheiro-Machado, P.; Garcia, R.; Franco, M.; Moreira, S.R.; Tedesco-Silva, H., Jr.; Medina-Pestana, J. Impact of initial exposure to calcineurin inhibitors on kidney graft function of patients at high risk to develop delayed graft function. Braz. J. Med. Biol. Res. 2006, 39, 43–52. [Google Scholar] [CrossRef] [Green Version]
- Gheith, O.A.; Bakr, M.A.; Fouda, M.A.; Shokeir, A.A.; Bayoumy, A.; Sobh, M.; Ghoneim, M. Steroid and azathioprine versus steroid, cyclosporine, and azathioprine therapies in primary haplo-identical living donor kidney transplantation: Twenty-year experience. Iran J. Kidney Dis. 2008, 2, 34–39. [Google Scholar]
- Cotovio, P.; Neves, M.; Rodrigues, L.; Alves, R.; Bastos, M.; Baptista, C.; Macário, F.; Mota, A. New-onset diabetes after transplantation: Assessment of risk factors and clinical outcomes. Transplant. Proc. 2013, 45, 1079–1083. [Google Scholar] [CrossRef]
- Knight, S.R.; Russell, N.K.; Barcena, L.; Morris, P.J. Mycophenolate mofetil decreases acute rejection and may improve graft survival in renal transplant recipients when compared with azathioprine: A systematic review. Transplantation 2009, 87, 785–794. [Google Scholar] [CrossRef]
- Van Hooff, J.P.; Squifflet, J.P. A prospective randomized multicenter study of tacrolimus in combination with sirolimus in renal transplant recipients. Transplantation 2003, 75, 1934–1939. [Google Scholar] [CrossRef]
- Webster, A.C.; Lee, V.W.; Chapman, J.R.; Craig, J.C. Target of rapamycin inhibitors (sirolimus and everolimus) for primary immunosuppression of kidney transplant recipients: A systematic review and meta-analysis of randomized trials. Transplantation 2006, 81, 1234–1248. [Google Scholar] [CrossRef]
- Johnston, O.; Rose, C.L.; Webster, A.C.; Gill, J.S. Sirolimus is associated with new-onset diabetes in kidney transplant recipients. J. Am. Soc. Nephrol. 2008, 19, 1411–1418. [Google Scholar] [CrossRef]
- Danovitch, G.M. Immunosuppressive Medications and Protocols for Kidney Transplantation. In Handbook of Kidney Transplantation, 4th ed.; Danovitch, G.M., Ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005; pp. 72–134. [Google Scholar]
- Ribes, D.; Kamar, N. Combined use of tacrolimus and sirolimus in de novo renal transplant patients: Current data. Transplant. Proc. 2005, 37, 2813–2816. [Google Scholar] [CrossRef]
- Gralla, J.; Wiseman, A.C. Tacrolimus/sirolimus versus tacrolimus/mycophenolate in kidney transplantation: Improved 3-year graft and patient survival in recent era. Transplantation 2009, 87, 1712–1719. [Google Scholar] [CrossRef]
- Yabu, J.M.; Vincenti, F. Kidney Transplantation: The ideal immunosuppression regimen. Adv. Chronic Kidney Dis. 2009, 16, 226–233. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Almeida, C.C.; Silveira, M.R.; De Araújo, V.E.; De Lemos, L.L.P.; De Oliveira Costa, J.; Reis, C.A.L.; De Assis Acurcio, F.; Das Gracas Braga Ceccato, M. Safety of Immunosuppressive Drugs Used as Maintenance Therapy in Kidney Transplantation: A Systematic Review and Meta-Analysis. Pharmaceuticals 2013, 6, 1170-1194. https://doi.org/10.3390/ph6101170
Almeida CC, Silveira MR, De Araújo VE, De Lemos LLP, De Oliveira Costa J, Reis CAL, De Assis Acurcio F, Das Gracas Braga Ceccato M. Safety of Immunosuppressive Drugs Used as Maintenance Therapy in Kidney Transplantation: A Systematic Review and Meta-Analysis. Pharmaceuticals. 2013; 6(10):1170-1194. https://doi.org/10.3390/ph6101170
Chicago/Turabian StyleAlmeida, Celline Cardoso, Micheline Rosa Silveira, Vânia Eloisa De Araújo, Livia Lovato Pires De Lemos, Juliana De Oliveira Costa, Carlos Augusto Lins Reis, Francisco De Assis Acurcio, and Maria Das Gracas Braga Ceccato. 2013. "Safety of Immunosuppressive Drugs Used as Maintenance Therapy in Kidney Transplantation: A Systematic Review and Meta-Analysis" Pharmaceuticals 6, no. 10: 1170-1194. https://doi.org/10.3390/ph6101170