Extreme Heat and Health: Perspectives from Health Service Providers in Rural and Remote Communities in South Australia
Abstract
:1. Introduction
2. Experimental Section
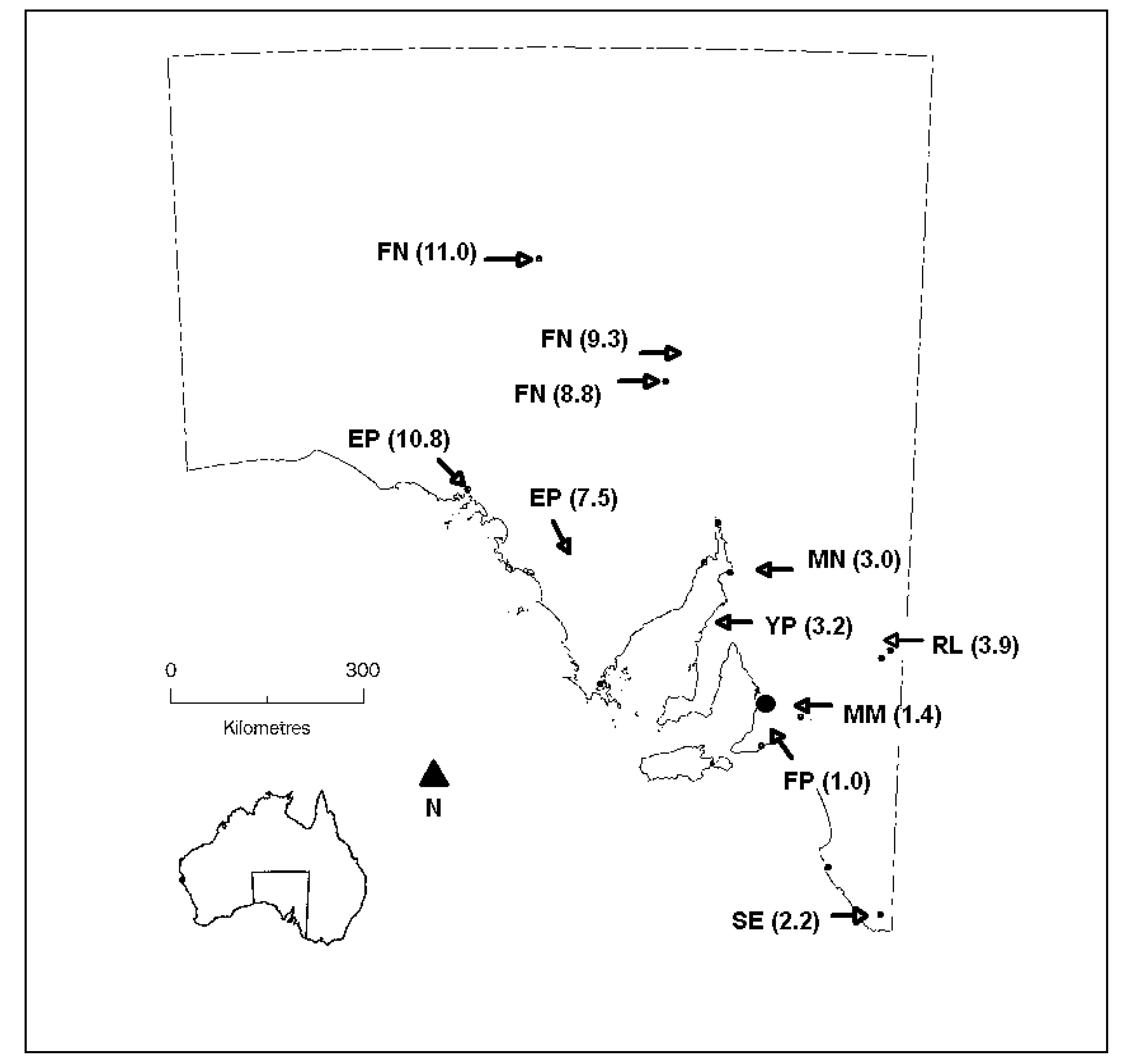
2.1. Sampling
2.2. Data Collection and Analysis
2.3. Ethics Approval
3. Results
| Respondents | Females | Males |
|---|---|---|
| Community Health Service Managers | 1 | |
| Program Managers (including social work, geriatric) | 4 | |
| Community Nurses | 3 | |
| Directors of Nursing | 1 | 1 |
| Remote Area Nurses | 1 | |
| Ambulance Service Regional Team Leaders | 1 | |
| Medical practitioners | 1 | |
| Total | 9 | 4 |
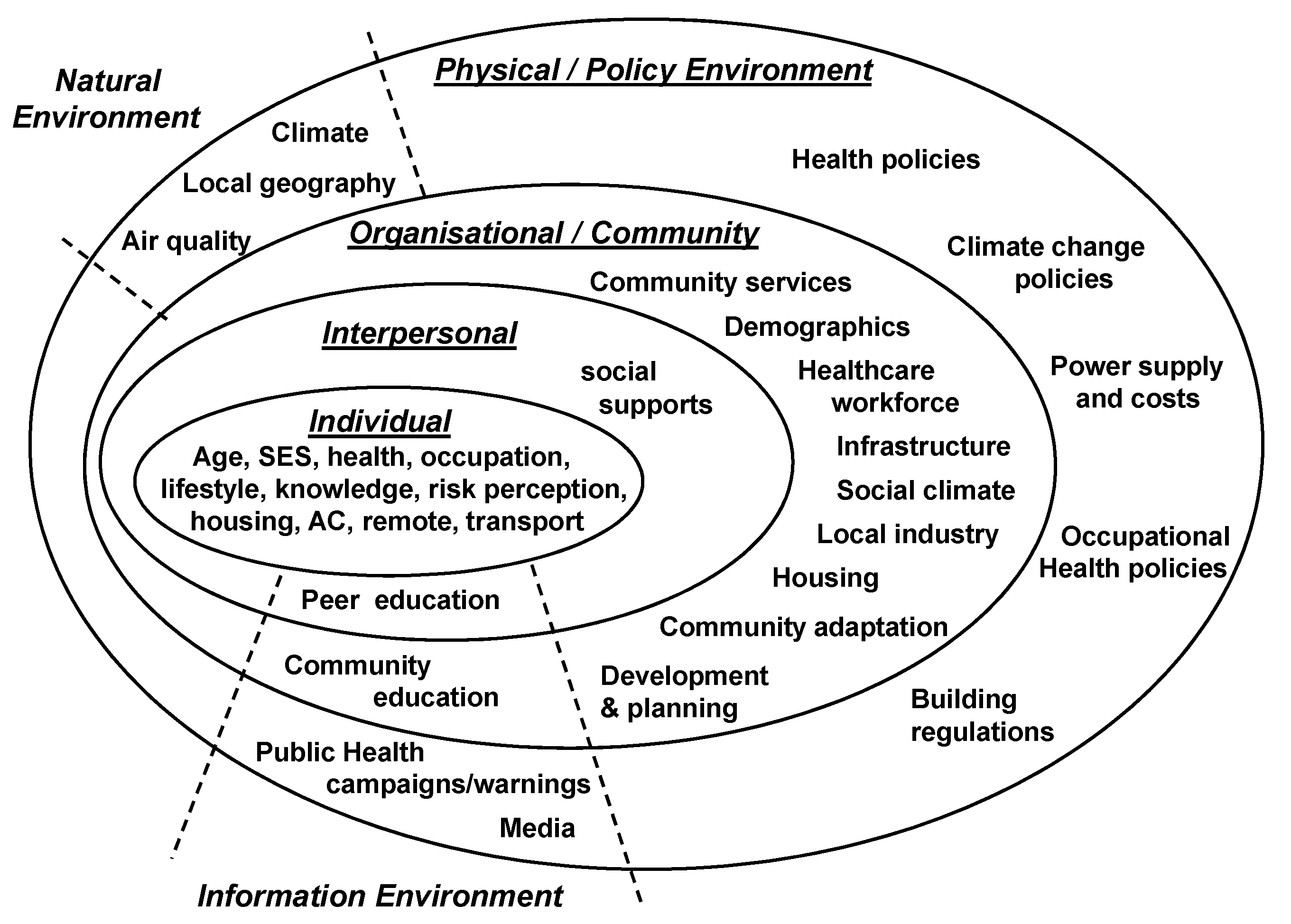
| Socio-Ecological Domains | Impact of Extreme Heat | Factors that Influence Coping and Adaptation to Extreme Heat |
|---|---|---|
| Individual characteristics | Quality of Life | Vulnerabilities (elderly, illness, SE † disadvantage, housing, air-conditioning, occupation, transport, outlying/remote) |
| Independence (experience, behaviours, awareness) | ||
| Interpersonal interactions | Social isolation | Social supports |
| Education | ||
| Community characteristics | Community Life (activities, sport) | Demographics |
| Housing (development) | ||
| Community safety | ||
| Infrastructure (cool places, power and water) | ||
| Public transport | ||
| Local industry (tourism, mining, agriculture) | ||
| Health service (organizational) | Hospital services | Workforce |
| Monitoring (vulnerable clients, education, extra checks, advocacy) | ||
| Occupational risk | ||
| Natural environment | Climate | |
| Local geography (sea breeze, lake, river, water supply) |
3.1. The Impact of Extreme Heat on Health Services
3.1.1. Hospital Services
….at the moment traditionally we get a lot of people come up here for tourism and a lot of the people who clog the A&E (accident and emergency) department are tourists, you know ‘cause they’ve come from out of town they’re not used to the warmer conditions (#1; YP)
3.1.2. Monitoring
The input into them may increase though. May be required to go back to somebody, which we wouldn’t normally do, or follow up on different processes, equipment, procedures, or whatever to ensure the client’s still safe at home. It might include going in and checking out that their air-conditioner is actually on cool and not heat, which we have had happen. That can happen. Just things like that, and that might take extra time to do those things. (#10; RL)
3.1.3. Occupational Risk
But certainly from a staff perspective, really hard work going out and about on a day like that, especially with a north wind blowing as well, and expected to visit 9 or 10 clients a day, getting in and out of the car. The car often can’t be parked in a shaded area, so the car’s very hot to get in and out of. You have to ensure that staff have got policy and procedure to follow to ensure they’re hydrated, to ensure that they rest if they need to, get out of the heat if they must, all those sorts of things. (#10; RL)
So when we get the, you know, the days that are catastrophic days and stuff, we actually don’t go outside the confines of the actual town because some of our girls travel, you know, say forty kilometres out to people in isolated places to give them services. …..Yes basically some services have to get cut then. (#5; MN)
3.2. The Impact of Extreme Heat on Individuals and Communities
Quality of Life, Social isolation and Community life
It will definitely have an impact, because even now over the heat of the summer there’s less social stuff going on, you know, sport doesn’t get played, that sort of stuff. So it’s already affecting the community in that sort of way. (#14; FN)
3.3. Factors that Influence Coping and Adaptation to Extreme Heat
3.3.1. Local Climate and Geography
3.3.2. Vulnerabilities
I find that a lot of elderly people don’t like having the air-conditioner on. They find that the air is actually too cold and so lots of times they won’t actually put their air-conditioner on, some do, and sometimes it’s a matter of economics as well people really can’t afford to run an air-conditioner all the time so they’ll wait until they’ve got no choice and then they’ll use their air-conditioner (#15; EP)
There is a group of people who suffer from compound disadvantage, and that means that they might have less than favourable living environment, no transport, out in the donga * somewhere, so for a number of reasons they couldn’t come into another place where it’s cooler or get into the lake for a swim or whatever. I think sometimes a group of things that would disadvantage some people would stop them from seeking help somehow. (#10; RL)(* donga is an Australian colloquialism referring to a remote bush area)
.. there have been plenty of innovations in recent times, obviously all the farmers, not all of them, but they’ve got air-conditioned tractors now, they sit up there and they’ve got their stereo and their air-conditioning and away they go and it doesn’t matter what the temperature is outside (#1; YP)
3.3.3. Independence
I think that rural communities in general are used to dealing with heat and or unusual weather conditions. The majority of people have lived on the land or farmed the land or worked in partnership or in industries over time and they’re used to the environment they’re in and with the exception of those people that have lost their, a significant proportion of their independence or cognitive function most people have means and more than a basic understanding of how to and what they can do during extreme heat or prolonged heat, and they put in fair, legitimate and effective strategies to cope with extreme heat, in almost all cases (#1; YP)
3.3.4. Social Support
You know there is not always family – sometimes it is the neighbours who go and checks on them, you know, twice a day or whatever when it’s has got past a certain temperature. We have a lot of that kind of, you know, buddy-ing sort of thing happens. (#5; MN)
3.3.5. Education
3.3.6. Community Demographics
3.3.7. Housing
3.3.8. Community Safety
I mean I guess we’re a little bit safer. I know personally that my partner and I sleep with the house wide open in the middle of summer to let the cool evening air in and so on, but I’m fairly certain that there would be an older contingent or any contingent that are afraid that wouldn’t do that – remain in the closed house and not let cool air in, because they are frightened and frightened at night because they’re on their own or their closest neighbours aren’t close. (#10; RL)
3.3.9. Limited Cool Public Spaces
3.3.10. Power and Water Supply
3.4. Concerns and Strategies for Future Adaptation
I think most of the remote communities will cope because they do. That’s how they’ve grown up and there’s no whingeing to anyone because you’re miles from anywhere. (#14; FN)
I’ve seen just in the 10 years I’ve been in this area, the average age of my clients has gone from being perhaps early 80 s and I’ve now got clients well up into their 90 s and some in their 100 s, and they’re frailer, they’re more at risk and I suppose for me that’s going to be the concern, is that we’re going to have much higher numbers of the really frail elderly. And often out there on their own at home. They are going to be a huge risk, because they also as they age they are often starting to become dehydrated before they experience thirst. So, huge risk for dehydration because they’re often so frail and the really high ages they often haven’t got friends around to check on them. So I think that’s going to be a much bigger burden on community services. (#13; SE)
| Topic | Quotes |
|---|---|
| Infrastructure/facilities |
|
| Power subsidies/ Electricity costs |
|
| Rescheduling work and activities |
|
| Education |
|
| Organisational |
|
| Building regulations |
|
| Resources/Support |
|
| More of the same |
|
4. Discussion
5. Conclusions
Acknowledgments
Conflicts of Interest
References
- Kovats, R.S.; Hajat, S. Heat stress and public health: A critical review. Annu. Rev. Public Health 2008, 29, 41–55. [Google Scholar] [CrossRef]
- Basu, R.; Samet, J.M. Relation between elevated ambient temperature and mortality: A review of the epidemiologic evidence. Epidemiol. Rev. 2002, 24, 190–202. [Google Scholar] [CrossRef]
- Smoyer, K.E. Putting risk in its place: Methodological considerations for investigating extreme event health risk. Soc. Sci. Med. 1998, 47, 1809–1824. [Google Scholar] [CrossRef]
- Johnson, D.P.; Stanforth, A.; Lulla, V.; Luber, G. Developing an applied extreme heat vulnerability index utilizing socioeconomic and environmental data. Appl. Geogr. 2012, 35, 23–31. [Google Scholar] [CrossRef]
- Harlan, S.L.; Brazel, A.J.; Prashad, L.; Stefanov, W.L.; Larsen, L. Neighborhood microclimates and vulnerability to heat stress. Soc. Sci. Med. 2006, 63, 2847–2863. [Google Scholar] [CrossRef]
- Vaneckova, P.; Beggs, P.; Jacobson, C. Spatial analysis of heat-related mortality among the elderly between 1993 and 2004 in Sydney, Australia. Soc. Sci. Med. 2009, 70, 293–304. [Google Scholar] [CrossRef]
- O’Neill, M.S.; Ebi, K.L. Climate Change. In Macrosocial Determinants of Population Health; Galea, S., Ed.; Springer: New York, NY, USA, 2007; pp. 139–157. [Google Scholar]
- Yardley, J.; Sigal, R.J.; Kenny, G.P. Heat health planning: The importance of social and community factors. Glob. Environ. Chang. 2011, 21, 670–679. [Google Scholar] [CrossRef]
- Ebi, K.L.; Semenza, J.C. Community-based adaptation to the health impacts of climate change. Am. J. Prev. Med. 2008, 35, 501–507. [Google Scholar] [CrossRef]
- McGeehin, M.A.; Mirabelli, M.C. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environ. Health Perspect. 2001, 109, 185–189. [Google Scholar] [CrossRef]
- Smoyer, K.E.; Rainham, D.G.C.; Hewko, J.N. Heat-stress-related mortality in five cities in Southern Ontario: 1980–1996. Int. J. Biometeorol. 2000, 44, 190–197. [Google Scholar] [CrossRef]
- Hajat, S.; Kovats, R.S.; Lachowycz, K. Heat-related and cold-related deaths in England and Wales: Who is at risk? Occup. Environ. Med. 2007, 64, 93–100. [Google Scholar]
- Gabriel, K.M.A.; Endlicher, W.R. Urban and rural mortality rates during heat waves in Berlin and Brandenburg, Germany. Environ. Pollut. 2011, 159, 2044–2050. [Google Scholar] [CrossRef]
- Burkart, K.; Schneider, A.; Breitner, S.; Khan, M.H.; Krämer, A.; Endlicher, W. The effect of atmospheric thermal conditions and urban thermal pollution on all-cause and cardiovascular mortality in Bangladesh. Environ. Pollut. 2011, 159, 2035–2043. [Google Scholar] [CrossRef]
- Sheridan, S.C.; Dolney, T.J. Heat, mortality, and level of urbanization:measuring vulnerability across Ohio, USA. Climate Res. 2003, 24, 255–265. [Google Scholar] [CrossRef]
- Hattis, D.; Ogneva-Himmelberger, Y.; Ratick, S. The spatial variability of heat-related mortality in Massachusetts. Appl. Geogr. 2012, 33, 45–52. [Google Scholar] [CrossRef]
- Henderson, S.B.; Wan, V.; Kosatsky, T. Differences in heat-related mortality across four ecological regions with diverse urban, rural, and remote populations in British Columbia, Canada. Health & Place. 2013. Available online: http://dx.doi.org/10.1016/j.healthplace.2013.1004.1005 (accessed on 3 May 2013).
- Lippmann, S.J.; Fuhrmann, C.M.; Waller, A.E.; Richardson, D.B. Ambient temperature and emergency department visits for heat-related illness in North Carolina, 2007–2008. Environ. Res. 2013. Available online: http://dx.doi.org/10.1016/j.envres.2013.1003.1009i (accessed on 3 May 2013).
- Wu, P.-C.; Lin, C.-Y.; Lung, S.-C.; Guo, H.-R.; Chou, C.-H.; Su, H.-J. Cardiovascular mortality during heat and cold events: Determinants of regional vulnerability in Taiwan. Occup. Environ. Med. 2011, 68, 525–530. [Google Scholar] [CrossRef]
- Loughnan, M.; Nicholls, N.; Tapper, N. Mortality-temperature thresholds for ten major population centres in rural Victoria, Australia. Health Place 2010, 16, 1287–1290. [Google Scholar] [CrossRef]
- Bi, P.; Parton, K. Effect of climate change on Australian rural and remote regions: What do we know and what do we need to know? Aust. J. Rural Health 2008, 16, 2–4. [Google Scholar] [CrossRef]
- Horton, G.; Hanna, L.; Kelly, B. Drought, drying and climate change: Emerging health issues for ageing Australians in rural areas. Australas. J. Ageing 2010, 29, 2–7. [Google Scholar] [CrossRef]
- Griffin, T.; McCaskill, M. Atlas of South Australia. South Australian Government Printing Division, South Australia. 1986. Available online: http://www.atlas.sa.gov.au/resources/atlas-of-south-australia-1986/environment-resources/climate-and-weather (accessed on 7 May 2013).
- Suppiah, R.; Preston, B.; Whetton, P.; McInnes, K.; Jones, R.; Macadam, I.; Bathols, J.; Kirono, D. Climate Change under Enhanced Greenhouse Conditions in South. Australia; CSIRO Marine and Atmospheric Research Group, Commonwealth Science and Industrial Research Organisation: Melbourne, Australia, 2006. [Google Scholar]
- Nitschke, M.; Tucker, G.R.; Hansen, A.L.; Williams, S.; Zhang, Y.; Bi, P. Impact of two recent extreme heat episodes on morbidity and mortality in Adelaide, South Australia: A case-series analysis. Environ. Health 2011, 10. [Google Scholar] [CrossRef]
- Williams, S.; Nitschke, M.; Tucker, G.; Bi, P. Extreme heat arrangements in South Australia: An assessment of trigger temperatures. Health Promot. J. Aust. 2011, 22, S21–S27. [Google Scholar]
- South Australian State Emergency Service, Extreme Heat Arrangements; Government of South Australia: Adelaide, Australia, 2009.
- Australian Bureau of Statistics. ABS Releases Measures of Socio-Economic Advantage and Disadvantage. Available online: http://www.abs.gov.au/AUSSTATS/[email protected]/Previousproducts/2033.0.55.001Media%20Release22006?opendocument&tabname=Summary&prodno=2033.0.55.001&issue=2006&num=&view= (accessed on 6 May 2013).
- Australian Bureau of Statistics. Population by Age and Sex, Regions of Australia. 2011. Available online: http://www.abs.gov.au/ausstats/[email protected]/Latestproducts/3235.0Main%20Features82011?opendocument&tabname=Summary&prodno=3235.0&issue=2011&num=&view= (accessed on 7 May 2013).
- Hanna, E.G.; Kjellstrom, T.; Bennett, C.; Dear, K. Climate change and rising heat: Population health implications for working people in Australia. Asia Pac. J. Public Health 2011, 23, 14S–26S. [Google Scholar] [CrossRef]
- National Rural Health Alliance Inc. Fact Sheet 23: Measuring the metropolitan-rural inequity. 2010. Available online: http://nrha.ruralhealth.org.au/factsheets/?IntContId=14819&IntCatId=41 (accessed on 8 May 2013).
- Onyx, J.; Bullen, P. Measuring social capital in five communities. J. Appl. Behav. Sci. 2000, 36, 23–42. [Google Scholar] [CrossRef]
- Hegney, D.G.; Buikstra, E.; Baker, P.; Rogers-Clark, C.; Pearce, S.; Ross, H.; King, C.; Watson-Luke, A. Individual resilience in rural people: A Queensland study, Australia. Rural Remote Health 2007, 7, 1–13. [Google Scholar]
- Australian Government Bureau of Meteorology. South Australia in Summer 2011–12: Wet and Cool in the North, Warm and Dry in the Elsewhere. Available online: http://www.bom.gov.au/climate/current/season/sa/archive/201202.summary.shtml (accessed on 15 October 2013).
- Sims-Schouten, W.; Riley, S.C.E.; Willig, C. Critical realism in discourse analysis: A presentation of a systematic method of analysis using women’s talk of motherhood, childcare and female employment as an example. Theor. Psychol. 2007, 17, 101–124. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psych. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Sallis, J.F.; Owen, N.; Fisher, E.B. Ecological Models of Health Behaviour. In Health Behavior and Health Education: Theory, Research, and Practice, 4th ed.; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; Jossey-Bass: San Francisco, CA, USA, 2008; pp. 465–482. [Google Scholar]
- Commonwealth Department of Health and Aged Care. Measuring Remoteness: Accessibility/Remoteness Index of Australia (ARIA). Available online: http://www.health.gov.au/internet/main/publishing.nsf/Content/E2EE19FE831F26BFCA257BF0001F3DFA/$File/ocpanew14.pdf (accessed on 5 March 2013).
- Banwell, C.; Dixon, J.; Bambrick, H.; Edwards, F.; Kjellstrom, T. Socio-cultural reflections on heat in Australia with implications for health and climate change adaptation. Glob. Health Action 2012, 5. [Google Scholar] [CrossRef]
- Tonts, M. Competitive sport and social capital in rural Australia. J. Rural Stud. 2005, 21, 137–149. [Google Scholar] [CrossRef]
- Hansen, A.; Bi, B.; Nitschke, M.; Pisaniello, D.; Newbury, J.; Kitson, A. Perceptions of heat-susceptibility in older persons: Barriers to adaptation. Int. J. Environ. Res. Public. Health 2011, 8, 4714–4728. [Google Scholar] [CrossRef]
- Akompab, D.; Bi, P.; Williams, S.; Saniotis, A.; Walker, I.; Augoustinos, M. Climate change, community understanding and emotional responses to the impacts of heat waves in Adelaide, Australia. Int. J. Clim. Chang. Imp. Responses 2013, 4, 109–126. [Google Scholar]
- Stimson, R.; Baum, S.; O’Connor, K. The social and economic performance of Australia’s large regional cities and towns: Implications for rural and regional policy. Aust. Geogr. Stud. 2003, 41, 131–147. [Google Scholar]
- Loughnan, M.; Carroll, M.; Tapper, N. Learning from our older people: Pilot study findings on responding to heat. Australas. J. Ageing 2013. [Google Scholar] [CrossRef]
- Glazer, J.L. Management of heatstroke and heat exhaustion. Am. Fam. Phys. 2005, 71, 2133–2140. [Google Scholar]
- Wolf, J.; Adger, W.N.; Lorenzoni, I.; Abrahamson, V.; Raine, R. Social capital, individual responses to heat waves and climate change adaptation: An empirical study of two UK cities. Glob. Environ. Chang. 2010, 20, 44–52. [Google Scholar] [CrossRef]
- Semenza, J.C.; Wilson, D.J.; Parra, J.; Bontempo, B.D.; Hart, M.; Sailor, D.J.; George, L.A. Public perception and behavior change in relationship to hot weather and air pollution. Environ. Res. 2008, 107, 401–411. [Google Scholar] [CrossRef]
- Humphreys, J.; Jones, J.; Jones, M.; Hugo, G.; Bamford, E.; Taylor, D. A critical review of rural medical workforce retention in Australia. Aust. Health Rev. 2001, 24, 91–102. [Google Scholar]
- Hennessy, K.; Lucas, C.; Nicholls, N.; Bathols, J.; Suppiah, R.; Ricketts, J. Climate Change Impacts on Fire-Weather in South-East Australia; CSIRO, Commonwealth Science and Industrial Research Organisation: Melbourne, Australia, 2006. [Google Scholar]
- Gao, C.; Kuklane, K.; Wang, F.; Holmer, I. Personal cooling with phase change materials to improve thermal comfort from a heat wave perspective. Indoor Air 2012, 22, 523–530. [Google Scholar] [CrossRef]
- McInnes, J.; Ibrahim, J. Minimising harm to older Victorians from heatwaves: A qualitative study of the role of community-based health profession and carer organisations. Australas. J. Ageing 2010, 29, 104–110. [Google Scholar] [CrossRef]
- Oakman, T.; Byles-Drage, H.; Pope, R.; Pritchard, J. Beat the heat: Don’t forget your drink—A brief public education program. Aust. N. Z. J. Pub. Health 2010, 34, 346–350. [Google Scholar] [CrossRef]
- Green, H.; Gilbert, J.; James, R.; Byard, R.W. An analysis of factors contributing to a series of deaths caused by exposure to high environmental temperatures. Am. J. Forensic Med. Pathol. 2001, 22, 196–199. [Google Scholar] [CrossRef]
- Hansen, A.; Bi, P.; Saniotis, A.; Nitschke, M.; Benson, J.; Tan, Y.; Smyth, V.; Wilson, L.; Han, G.-S. Extreme Heat and Climate Change: Adaptation in Culturally and Linguistically Diverse (CALD) Communities; National Climate Change Adaptation Research Facility: Gold Coast, Australia, 2013; p. 101. [Google Scholar]
- Jones, R.; Tonts, M. Transition and diversity in rural housing provision: The case of Narrogin, Western Australia. Aust. Geogr. 2003, 34, 47–59. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Williams, S.; Bi, P.; Newbury, J.; Robinson, G.; Pisaniello, D.; Saniotis, A.; Hansen, A. Extreme Heat and Health: Perspectives from Health Service Providers in Rural and Remote Communities in South Australia. Int. J. Environ. Res. Public Health 2013, 10, 5565-5583. https://doi.org/10.3390/ijerph10115565
Williams S, Bi P, Newbury J, Robinson G, Pisaniello D, Saniotis A, Hansen A. Extreme Heat and Health: Perspectives from Health Service Providers in Rural and Remote Communities in South Australia. International Journal of Environmental Research and Public Health. 2013; 10(11):5565-5583. https://doi.org/10.3390/ijerph10115565
Chicago/Turabian StyleWilliams, Susan, Peng Bi, Jonathan Newbury, Guy Robinson, Dino Pisaniello, Arthur Saniotis, and Alana Hansen. 2013. "Extreme Heat and Health: Perspectives from Health Service Providers in Rural and Remote Communities in South Australia" International Journal of Environmental Research and Public Health 10, no. 11: 5565-5583. https://doi.org/10.3390/ijerph10115565




