The Role of Community Centre-based Arts, Leisure and Social Activities in Promoting Adult Well-being and Healthy Lifestyles
Abstract
:1. Introduction
2. South West Well-Being Programme
- A focus on individuals’ experiencing low level mental ill health, long term health conditions, low levels of physical activity and/or diet related ill-health. These criteria were combined with low income and/or social isolation.
- The provision of a holistic service that focuses on the social aspects of health and well-being: being inclusive, fun, non-judgemental and non-threatening; people-centred and self-directed lifestyle change-depending on their needs and wishes.
- A focus on reducing stress and anxiety, increasing physical activity and healthy eating, through confidence building and encouraging the development of friends, social networks and local community participation.
- A focus on local collaboration with other agencies and stakeholders with an interest in health promotion and building community capacity.
3. Methods
3.1. Procedure
3.2. Ethical issues
3.3. Questionnaire Tool (SWWBQ)
| General health: How would you describe your health generally over the last week? (5 point scale, widely used measure) | |
| Social Well-Being scale (6 items, 5 point scales, SWB-6; adapted from European Social Survey Round 3) | |
| Below are some statements about feelings and thoughts. What best describes your experience of each over the past four weeks?(paraphrased) | |
| I feel like I belong to something I call community | |
| There are people in my life who really care about me | |
| People in my local area help one another | |
| I regularly meet socially with friends and relatives | |
| I find it easy to meet people who share my hobbies or interests | |
| I often help with or attend activities organised in my local area | |
| Center for Epidemiological Studies Depression scale (7 items, 5 point scales, CES-D-7 [22]) | |
| Below are a number of things people might say that they feel. How often during the past week would each description have applied to you? (paraphrased) | |
| You felt happy or contented | |
| You felt depressed | |
| You felt engaged or focused in what you were doing | |
| You felt energised or lively | |
| You felt lonely | |
| You felt everything you did was an effort | |
| Your sleep was restless | |
| Warwick Edinburgh Mental Well-being Scale (7 items, 5 point scales, WEMWBS-7 [23]) | |
| Below are some statements about feelings and thoughts. What best describes your experience of each over the past four weeks?(paraphrased) | |
| I’ve been feeling optimistic about the future | |
| I’ve been feeling useful | |
| I’ve been feeling relaxed | |
| I’ve been dealing with problems well | |
| I’ve been thinking clearly | |
| I’ve been feeling close to other people | |
| I’ve been able to make up my own mind about things | |
| Mental well-being: life satisfaction. All things considered, how satisfied are you with your life as a whole nowadays? (10 point scale, widely used measure) | |
| Healthy eating (5 point scales) | |
| Fruit & vegetable intake: portions per day (widely used measure) | |
| Enjoyment: I enjoy eating healthy food (study specific question) | |
| Importance: I value putting effort and care into the food I eat (study specific question) | |
| Physical activity | |
| GP Physical Activity Questionnaire (5 point scales, GPPAQ [24]) | |
| Enjoyment: I enjoy taking part in regular physical activity (5 point scale, study specific question) | |
| Importance: Regular physical activity is important for my health (5 point scale, study specific question) | |
- Belonging (community) I feel like I belong to something I call community
- Support (intimate) There are people in my life who really care about me
- Support (community) People in my local area help one another
- Engagement (social) I regularly meet socially with friends and relatives
- Engagement (intimate) I find it easy to meet people who share my hobbies or interests
- Participation (community) I often help with or attend activities organised in my local area
- CES-D-7 baseline Cronbach’s α 0.853; follow-up Cronbach’s α 0.715
- WEMWBS-7 baseline Cronbach’s α 0.885; follow up Cronbach’s α 0.849
- SWB-6 baseline Cronbach’s α of 0.714; follow-up Cronbach’s α of 0.708
3.4. Data Analysis
4. Results
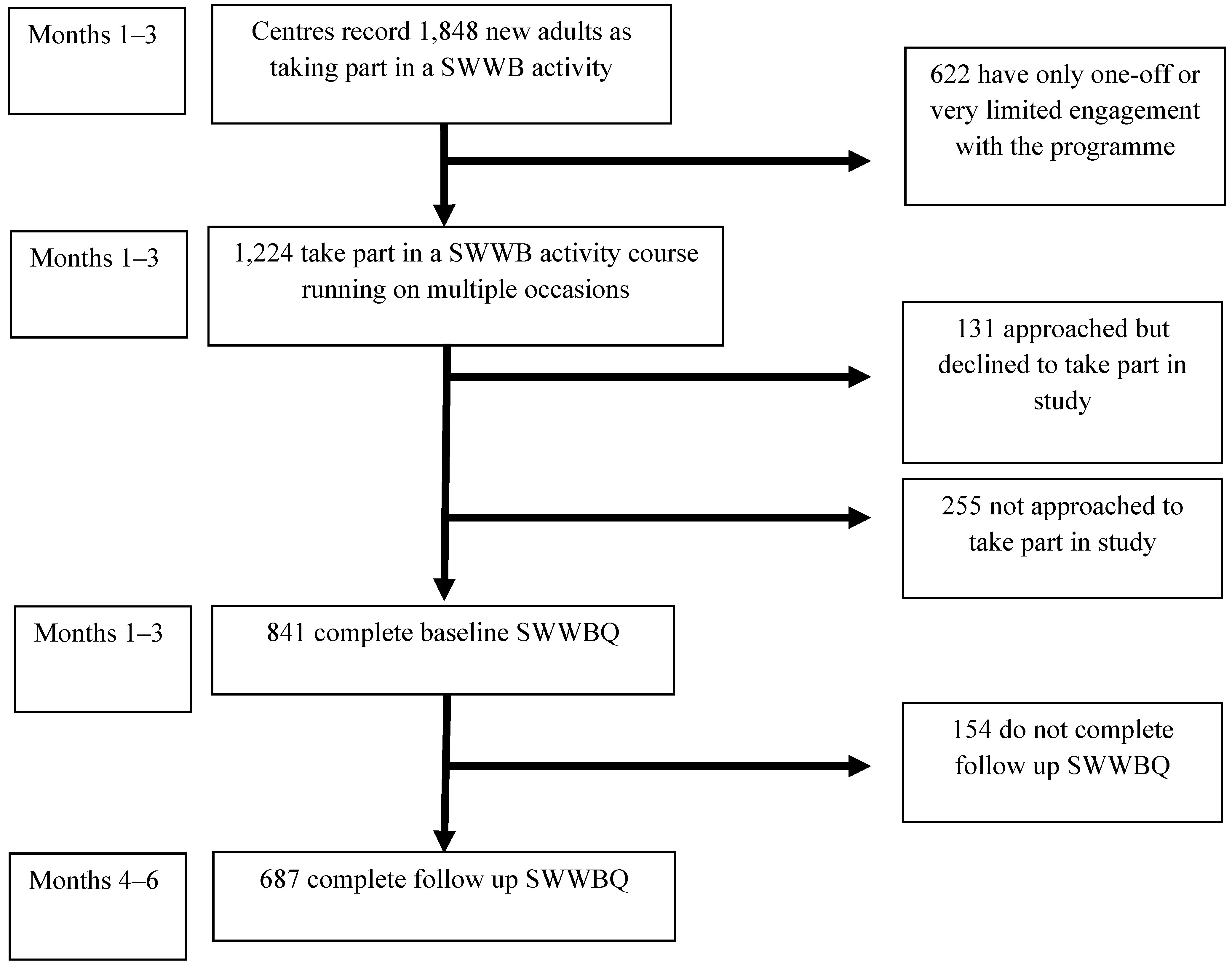
4.1. Recruitment of Study Participants
4.2. Participant Profile
| Variable | N | (%) | |
|---|---|---|---|
| Gender | |||
| Male | 179 | (26) | |
| Gender | 536 | (78) | |
| Age band | |||
| 18–30 | 102 | (14.8) | |
| 31–40 | 138 | (20.2) | |
| 41–50 | 159 | (23.1) | |
| 51–60 | 91 | (13.2) | |
| 61–70 | 128 | (18.6) | |
| 70+ | 61 | (8.9) | |
| Not known | 8 | (1.2) | |
| Race/ethnicity | |||
| White (British & Other) | 623 | (90.7) | |
| Black or Minority Ethnic Group | 38 | (5.5) | |
| Not known | 26 | (3.8) | |
| Employment status | |||
| Training, education | 42 | (6.1) | |
| Retired | 209 | (30.4) | |
| Seeking work | 136 | (19.8) | |
| Full time family carer | 88 | (12.8) | |
| In employment | 129 | (18.8) | |
| Incapacity for work (illness, disability) | 62 | (9) | |
| Not known | 21 | (3.1) | |
| Domestic circumstances | |||
| Living alone | 228 | (33.2) | |
| Living with partner & children | 132 | (19.2) | |
| Living with partner only | 136 | (19.7) | |
| Living with other relative | 54 | (7.9) | |
| Living children only | 44 | (6.4) | |
| Not known/Other | 93 | (13.6) | |
| Main focus of initial project activity | |||
| Physical activity | 144 | (21.0) | |
| Mental wellbeing | 101 | (14.7) | |
| Healthy eating | 230 | (33.5) | |
| Befriending | 147 | (21.4) | |
| Non-specific | 65 | (9.4) | |
| Format of initial project activity | |||
| Group activities plus a structured series of 1-1 practitioner support sessions | 235 | (34.2) | |
| Group activities plus unspecified or ad hoc 1-1 practitioner contact | 452 | (65.8) | |
| Main route for activity enrolment | |||
| Project direct contact (e.g., leaflet, practitioner contact) | 201 | (29.2) | |
| Informal networks (e.g., word of mouth) | 197 | (28.7) | |
| Healthcare agency (e.g., GP, primary care centre) | 176 | (25.6) | |
| Other agency (e.g., social services, children’s centre) | 85 | (12.4) | |
| Not known | 28 | (4.1) | |
| Additional registration notes | |||
| Practitioner referral notes recorded depression, anxiety or another mental health issue | 111 | (16.1) | |
| Practitioner referral notes recorded obesity or overweight, BMI > 25 | 178 | (25.9) | |
| Participants recorded being in receipt of a disability benefit | 106 | (15.5) | |
| Participants recorded being unpaid carer for an adult with illness or disability | 54 | (7.9) | |
4.3. Health and Well-Being Results
| Measure | Baseline Mean (SD a) | Follow up Mean (SD) | Mean Difference (SD) | Standard Error of the Mean (SEM) | t value (df c) | p value |
|---|---|---|---|---|---|---|
| General health | 2.60 b (0.95) | 3.12 b (1.02) | 0.51 (1.07) | 0.41 | 12.34 (675) | <0.001 h |
| Social wellbeing: SWB-6 d | 20.05 (3.16) | 21.82 (4.18) | 1.77 (4.07) | 0.17 | −10.52 (633) | <0.001 h |
| i. Relatedness (community: belonging) | 3.00 (1.16) | 3.32 (1.12) | 0.32 (1.16) | 0.05 | −6.90 (645) | <0.001 h |
| ii. Engagement (community: attending local activities) | 2.99 (1.63) | 3.36 (1.59) | 0.37 (1.55) | 0.06 | −6.07 (648) | <0.001 h |
| iii. Engagement (community: meeting friends & family) | 3.71 (1.08) | 3.91 (0.99) | 0.20 (1.11) | 0.04 | −4.59 (648) | <0.001 h |
| iv. Support (community: local people help) | 3.33 (0.98) | 3.51 (0.99) | 0.02 (1.39) | 0.72 | −4.45 (648) | <0.001 h |
| v. Engagement (intimate: sharing interests & hobbies) | 2.70 (1.13) | 2.72 (1.19) | 0.02 (1.39) | 0.05 | 0.28 (640) | 0.77 j |
| vi. Support (intimate: people care about me) | 4.32 (0.85) | 4.33 (0.89) | 0.01 (1.01) | 0.04 | −0.19 (654) | 0.85 j |
| Mental well-being: life satisfaction | 6.17 (2.40) | 7.01 (2.17) | 0.84 (2.67) | 0.10 | −8.00 (661) | <0.001 h |
| Mental well-being: WEMWBS-7 e | 23.24 (5.24) | 25.52 (4.48) | 2.28 (5.08) | 0.21 | −10.48 (621) | <0.001 h |
| Mental ill health: depression CES-D-7 f | 10.93 (4.83) | 8.94 (2.96) | −1.99 (4.58) | 0.20 | −8.29 (601) | <0.001 i |
| Healthy eating: fruit & vegetable intake | 3.90 (2.18) | 3.54 (2.12) | −0.36 (2.85) | 0.19 | 3.08 (585) | 0.002 i |
| Healthy eating: enjoyment | 3.75 (0.97) | 4.19 (1.01) | 0.44 (1.00) | 0.03 | −9.87 (662) | <0.001 h |
| Healthy eating: importance | 3.76 (0.96) | 4.20 (0.99) | 0.44 (1.20) | 0.05 | −9.233 (668) | <0.001 h |
| Physical activity: GPPAQ g | 1.93 (1.05) | 2.90 (1.12) | 0.97 (1.36) | 0.05 | −18.17 (651) | <0.001 h |
| Physical activity: enjoyment | 3.16 (1.71) | 3.73 (1.15) | 0.56 (1.64) | 0.03 | −8.02 (639) | <0.001 h |
| Physical activity: importance | 3.52 (1.2) | 3.79 (1.18) | 0.27 (1.46) | 0.02 | −2.92 (353) | 0.004 h |
4.4. Further Analyses
4.4.1. Associations between Well-Being, Healthy Eating and Physical Activity
- Enjoy eating healthy food (χ2 52.794, p < 0.001)
- Value putting effort and care into food (χ2 56.507, p < 0.001)
- Enjoy taking part in regular physical activity (χ2 31.640, p = 0.007)
- Believe that physical activity is important for health (χ2 46.185, p < 0.001)
4.4.2. Associations between Outcomes and the Focus of Activity Input
4.4.3. Outcomes Associated with Format of Activity: One-to-One and Group Support
4.4.4. Outcomes Associated with Self vs. Practitioner Referral
5. Discussion
6. Conclusions
Acknowledgments
Conflict of Interest
References
- No Health without Public Mental Health; Royal College of Psychiatrists: London, UK, 2010.
- Marmot, M. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post 2010; UCL: London, UK, 2010. [Google Scholar]
- Health Reform: Meeting the Challenge of Ageing and Multiple Morbidities; OECD Publishing: Paris, France, 2011.
- Health Systems Financing: Paths to Universal Coverage; World Health Organisation: Geneva, Switzerland, 2010.
- The Community and Voluntary Sector in Health; Kings Funds and NCVO: London, UK, 2011.
- Healthy Lives, Healthy People White Paper: Our Strategy for Public Health in England; Department of Health: London, UK, 2010.
- A vision for Adult Social Care: Capable Communities and Active Citizens; Department of Health: London, UK, 2010.
- Aiken, M.; Cairns, B.; Taylor, M.; Moran, R. Community Organisations Controlling Assets: a better understanding; Joseph Rowntree Foundation: York, UK, 2011. [Google Scholar]
- Newbigging, K.; Heginbotham, C. Commissioning Mental Wellbeing: A Leadership Brief for Boards and Senior Managers; University of Central Lancashire: Preston, UK, 2010. [Google Scholar]
- South, J.; Higgins, T.; Woodall, J.; White, S. Can social prescribing provide the missing link? Prim. Health Care Res. Dev. 2008, 9, 310–318. [Google Scholar]
- Rankin, D.; Truman, J.; Backett-Milburn, K.; Platt, S.; Petticrew, M. The contextual development of healthy living centre services: An examination of food-related initiatives. Health Place 2006, 12, 644–655. [Google Scholar]
- Community Engagement and Development; National Institute for Health and Clinical Excellence: London, UK, 2007.
- Milton, B.; Attree, P.; French, B.; Povall, S.; Whitehead, M.; Popay, J. The impact of community engagement on health and social outcomes: A systematic review. Community Dev. J. 2011. [Google Scholar] [CrossRef]
- Wilkinson, R.; Pickett, K. The Spirit Level: Why More Equal Societies almost always Do Better; Allen Lane: London, UK, 2009. [Google Scholar]
- Hunter, B.; Neiger, B.; West, J. The importance of addressing social determinants of health at the local level: The case for social capital. Health Soc. Care Community 2011, 19, 522–530. [Google Scholar] [CrossRef]
- Renton, A.; Phillips, G.; Daykin, N.; Yu, G.; Taylor, K.; Petticrew, M. Think of your art-eries: Arts participation, behavioural cardiovascular risk factors and mental well-being in deprived communities in London. Public Health 2012, 126, S57–S64. [Google Scholar]
- Thomson, H.; Atkinson, R.; Petticrew, M.; Kearns, A. Do urban regeneration programmes improve public health and reduce health inequalities? A synthesis of the evidence from UK policy and practice (1980–2004). J. Epidemiol. Community Health 2006, 60, 108–115. [Google Scholar] [CrossRef]
- Thomson, H. A dose of realism for healthy urban policy: Lessons from area-based initiatives in the UK. J. Epidemiol. Community Health 2008, 62, 932–936. [Google Scholar] [CrossRef]
- Morrow-Howell, N. Volunteering in later life: Research frontiers. J. Gerontol. B Psychol. Sci. Soc. Sci. 2010, 65, 461–469. [Google Scholar] [CrossRef]
- South West Healthy Living Alliance Strategy; Westbank HLC: Devon, UK, 2008.
- Abdallah, S.; Steuer, N.; Marks, N. Well-Being Evaluation Tools: A Research and Development Project for the Big Lottery Fund; New Economics Foundation: London, UK, 2008. [Google Scholar]
- Radloff, L. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5, 63–75. [Google Scholar] [CrossRef]
- Wareham, N.; Jakes, R.; Renni, K.; Schuit, J.; Mitchell, J.; Hennings, S.; Day, N. Validity and repeatability of a simple index derived from the short physical activity questionnaire used in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr. 2002, 6, 407–413. [Google Scholar]
- Hawthorne, G.; Elliott, P. Imputing cross-sectional missing data: Comparison of common techniques. Aust. NZ J. Psychiat. 2005, 39, 583–590. [Google Scholar] [CrossRef]
- Buck, D.; Frosini, F. The Clustering of Unhealthy Behaviours Over Time; Kings Fund: London, UK, 2012. [Google Scholar]
- The Commissioning Framework for Health and Well-being; Department of Health: London, UK, 2007.
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Jones, M.; Kimberlee, R.; Deave, T.; Evans, S. The Role of Community Centre-based Arts, Leisure and Social Activities in Promoting Adult Well-being and Healthy Lifestyles. Int. J. Environ. Res. Public Health 2013, 10, 1948-1962. https://doi.org/10.3390/ijerph10051948
Jones M, Kimberlee R, Deave T, Evans S. The Role of Community Centre-based Arts, Leisure and Social Activities in Promoting Adult Well-being and Healthy Lifestyles. International Journal of Environmental Research and Public Health. 2013; 10(5):1948-1962. https://doi.org/10.3390/ijerph10051948
Chicago/Turabian StyleJones, Mat, Richard Kimberlee, Toity Deave, and Simon Evans. 2013. "The Role of Community Centre-based Arts, Leisure and Social Activities in Promoting Adult Well-being and Healthy Lifestyles" International Journal of Environmental Research and Public Health 10, no. 5: 1948-1962. https://doi.org/10.3390/ijerph10051948






