Effectiveness of the Gold Standard Programmes (GSP) for Smoking Cessation in Pregnant and Non-Pregnant Women
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Setting
2.3. Intervention
2.4. Participants
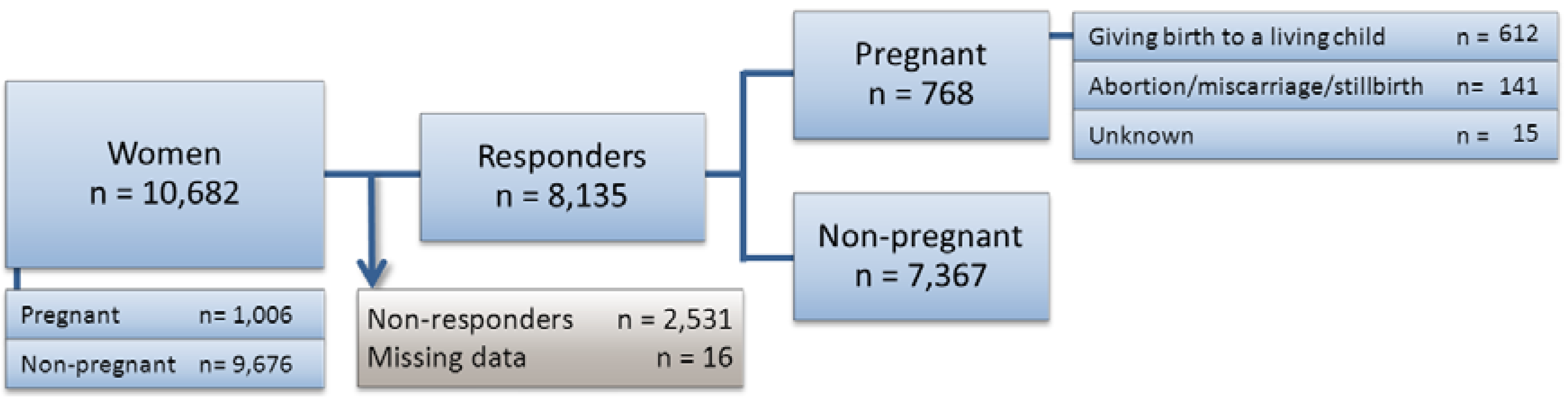
2.5. Data
2.6. Outcomes
2.6.1. Other Variables
| Women in GSP | Pregnant | Non-pregnant | |||
|---|---|---|---|---|---|
| Characteristics n (%) | Characteristics n (%) | ||||
| All | 1,006 | (100) | 9,676 | (100) | |
| Setting | |||||
| Midwife/Hospital | 438 | (43.5) | 622 | (6.4) | |
| Other | 568 | (56.5) | 9,054 | (93.6) | |
| Programme format | |||||
| Individual | 240 | (23.9) | 994 | (10.3) | |
| Group | 766 | (76.1) | 8,682 | (89.7) | |
| Medication for free | |||||
| No free medication | 511 | (50.8) | 5,296 | (54.7) | |
| Free for <1 week | 472 | (46.9) | 4,014 | (41.5) | |
| Free for <5 weeks | 3 | (0.3) | 75 | (0.8) | |
| Free for ≥5 weeks | 17 | (1.7) | 279 | (2.9) | |
| Free for unknown period of time | 3 | (0.3) | 12 | (0.1) | |
| Age (years) | |||||
| 15–24 | 240 | (23.9) | 704 | (7.3) | |
| 25–34 | 549 | (54.6) | 1,522 | (15.7) | |
| 35–44 | 213 | (21.2) | 3,083 | (31.9) | |
| 45–54 | 4 | (0.4) | 4,367 | (45.1) | |
| Smoking | |||||
| <20 pack-years | 885 | (88.0) | 4,549 | (47.0) | |
| ≥20 pack-years | 121 | (12.0) | 5,127 | (53.0) | |
| Fagerström 1–4 points | 451 | (44.8) | 3,658 | (37.8) | |
| Fagerström 5–10 points | 555 | (55.2) | 6,018 | (62.2) | |
| <20 cigarettes per day | 691 | (68.7) | 4,739 | (49.0) | |
| ≥20 cigarettes per day | 315 | (31.3) | 4,937 | (51.0) | |
| Heavy smokers a | |||||
| Yes | 370 | (36.8) | 6,350 | (65.6) | |
| No | 636 | (63.2) | 3,326 | (34.4) | |
| Compliance with programme b | |||||
| Compliant | 476 | (47.3) | 5,377 | (55.6) | |
| Not compliant | 507 | (50.4) | 4,121 | (42.6) | |
| Unknown | 23 | (2.3) | 178 | (1.8) | |
| Living with a smoker | |||||
| Yes | 523 | (52.0) | 3,615 | (37.4) | |
| No | 479 | (47.6) | 5,981 | (61.8) | |
| Unknown | 4 | (0.4) | 80 | (0.8) | |
| Attempts to quit | |||||
| No previous attempts | 421 | (41.8) | 3,616 | (37.4) | |
| Previous attempts | 573 | (57.9) | 5,896 | (60.9) | |
| Unknown | 12 | (1.2) | 176 | (1.8) | |
| Professional recommendation | |||||
| Yes from midwife or medical doctor | 711 | (70.7) | 3,995 | (41.3) | |
| Yes from others | 42 | (4.2) | 977 | (10.1) | |
| No | 213 | (21.2) | 4,265 | (44.1) | |
| Unknown | 40 | (4.0) | 239 | (2.5) | |
| Education | |||||
| Low level | 364 | (36.2) | 2,515 | (26.0) | |
| Medium level | 255 | (25.3) | 2,552 | (26.4) | |
| High level | 372 | (37.0) | 4,324 | (44.7) | |
| Unknown | 15 | (1.5) | 285 | (2.9) | |
| Employment | |||||
| Employed | 578 | (57.5) | 6,900 | (71.3) | |
| Unemployed | 277 | (27.5) | 1,771 | (18.3) | |
| Enrolled in education | 132 | (13.1) | 671 | (6.9) | |
| Unknown | 19 | (1.9) | 334 | (3.5) | |
| Disadvantaged smokers c | |||||
| Yes | 493 | (49.0) | 3,541 | (35.6) | |
| No | 495 | (49.2) | 5,757 | (59.5) | |
| Unknown | 18 | (1.8) | 378 | (3.9) | |
2.6.2. Sub-Analyses
2.7. Statistical Analysis
3. Results
| Women in GSP | ||
|---|---|---|
| Non-adjusted ORs (95% CI) | Adjusted ORs (95% CI) | |
| Pregnancy | ||
| Non-pregnant | 1 | |
| Pregnant | 1.02 (0.87–1.21) | 1.16 (0.95–1.42) |
| Setting | ||
| Midwife/Hospital | 1 | |
| Other | 0.94 (0.79–1.12) | 0.96 (0.79–1.17) |
| Programme format | ||
| Individual | 1 | |
| Group | 0.72 (0.62–0.84) | 0.79 (0.67–0.93) * |
| Medication for free | ||
| No free medication | 1 | |
| Free for <1 week | 0.87 (0.78–0.96) | 0.93 (0.83–1.04) |
| Free for <5 weeks | 1.17 (0.69–2.02) | 1.07 (0.61–1.88) |
| Free for ≥5 weeks | 1.31 (0.98–1.75) | 1.22 (0.89–1.66) |
| Age (years) | ||
| 25–54 | 1 | |
| 15–24 | 0.56 (0.46–0.70) | 0.65 (0.51–0.82) * |
| Heavy smokers a | ||
| Yes | 1 | |
| No | 1.50 (1.35–1.66) | 1.42 (1.27–1.58) * |
| Compliance with programme b | ||
| Compliant | 1 | |
| Not compliant | 0.27 (0.24–0.31) | 0.29 (0.26–0.32) * |
| Living with a smoker | ||
| Yes | 1 | |
| No | 1.16 (1.05–1.29) | 1.11 (1.00–1.24) |
| Attempts to quit | ||
| No previous attempts | 1 | |
| Previous attempts | 1.13 (1.02–1.25) | 1.03 (0.92–1.15) |
| Professional recommendation | ||
| Yes from midwife or medical doctor | 1 | |
| Yes from others | 1.24 (1.04–1.47) | 1.19 (0.99–1.43) |
| No | 1.25 (1.13–1.40) | 1.18 (1.06–1.33) * |
| Disadvantaged smokers c | ||
| Yes | 1 | |
| No | 1.33 (1.19–1.47) | 1.16 (1.04–1.30) * |
3.1. Secondary Outcomes
| Women in GSP | Pregnant | Non-pregnant | |||||
|---|---|---|---|---|---|---|---|
| Effect (%) | Effect (%) | ||||||
| Characteristics (n) | All | Responders | Characteristics (n) | All | Responders | ||
| Patients | 1,006 | 735 | 9,676 | 7,252 | |||
| Smoke free at end of programme | 419 | 41.7% | 57.0% | 4,729 | 48.9% | 65.2% | |
| OR (95% CI) | 0.98 (0.78–1.21) | 1 | |||||
| Patients | 1,006 | 763 | 9,676 | 7,319 | |||
| Point prevalence (14 days) | 306 | 30.4% | 40.1% | 2,801 | 28.9% | 38.3% | |
| OR (95% CI) | 1.27 (1.05–1.54) * | 1 | |||||
| Patients | 1,006 | 742 | 9,676 | 7,170 | |||
| Satisfied with the programme | 600 | 59.6% | 80.9% | 5,853 | 60.5% | 81.6% | |
| OR (95% CI) | 1.00 (0.79–1.26) | 1 | |||||
3.2. Sub-Analyses
3.3. Non-Responder Analysis
4. Discussion
5. Conclusions
Acknowledgments
Conflicts of Interest
References
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Amann, M.; Anderson, H.R.; Andrews, K.G.; Aryee, M.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013, 380, 2224–2260. [Google Scholar]
- Cnattingius, S. The epidemiology of smoking during pregnancy: Smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob. Res. 2004, 6 (Suppl 2), S125–S140. [Google Scholar] [CrossRef]
- Schneider, S.; Huy, C.; Schütz, J.; Diehl, K. Smoking cessation during pregnancy: A systematic literature review. Drug Alcohol Rev. 2010, 29, 81–90. [Google Scholar] [CrossRef]
- Wisborg, K.; Henriksen, T.B. Tobak og graviditet. Er der behov for forebyggelse? Findes der effektive metoder? (Tobacco and Pregnancy. Is There a Need for Prevention? Are There Effective Methods?), 1st ed.; The Danish Health and Medicines Authority: Copenhagen, Denmark, 2003. [Google Scholar]
- Wisborg, K.; Kesmodel, U.; Henriksen, T.B.; Olsen, S.F.; Secher, N.J. Exposure to tobacco smoke in utero and the risk of stillbirth and death in the first year of life. Am. J. Epidemiol. 2001, 154, 322–327. [Google Scholar] [CrossRef]
- McDonnell-Naughton, M.; McGarvey, C.; O’Regan, M.; Matthews, T. Maternal smoking and alcohol consumption during pregnancy as risk factors for sudden infant death. Irish Med. J. 2012, 105, 105–108. [Google Scholar]
- Wisborg, K.; Kesmodel, U.; Henriksen, T.B.; Olsen, S.F.; Secher, N.J. A prospective study of smoking during pregnancy and SIDS. Arch. Dis. Child. 2000, 83, 203–206. [Google Scholar] [CrossRef]
- Wisborg, K.; Henriksen, T.B.; Obel, C.; Skajaa, E.; Ostergaard, J.R. Smoking during pregnancy and hospitalization of the child. Pediatrics 1999, 104, e46:1–e46:4. [Google Scholar]
- Andres, R.L.; Day, M.C. Perinatal complications associated with maternal tobacco use. Sem. Neonatol. 2000, 5, 231–241. [Google Scholar] [CrossRef]
- Yang, Q.; Wen, S.W.; Phillips, K.; Oppenheimer, L.; Black, D.; Walker, M.C. Comparison of maternal risk factors between placental abruption and placenta previa. Am. J. Perinatol. 2009, 26, 279–286. [Google Scholar] [CrossRef]
- Benowitz, N.L.; Dempsey, D.A. Pharmacotherapy for smoking cessation during pregnancy. Nicotine Tob. Res. 2004, 6, 189–202. [Google Scholar] [CrossRef]
- Shi, Y.; De Groh, M.; Morrison, H. Perinatal and early childhood factors for overweight and obesity in young Canadian children. Canad. J. Public Health 2013, 104, e69–e74. [Google Scholar]
- Egebjerg Jensen, K.; Jensen, A.; Nøhr, B.; Krüger Kjaer, S. Do pregnant women still smoke? A study of smoking patterns among 261,029 primiparous women in Denmark 1997–2005. Acta Obstetricia et Gynecologica Scandinavica 2008, 87, 760–767. [Google Scholar] [CrossRef]
- Hiscock, R.; Judge, K.; Bauld, L. Social inequalities in quitting smoking: What factors mediate the relationship between socioeconomic position and smoking cessation? J. Public Health 2011, 33, 39–47. [Google Scholar] [CrossRef]
- Ferguson, J.; Bauld, L.; Chesterman, J.; Judge, K. The English smoking treatment services: One-year outcomes. Addiction 2005, 100 (Suppl), 59–69. [Google Scholar] [CrossRef]
- Rasmussen, M.; Ammari, A.B.H.; Pedersen, B.; Tønnesen, H. Smoking cessation intervention activities and outcome before, during and after the national Healthcare Reform in Denmark. Clin. Health Promot. 2012, 2, 26–35. [Google Scholar]
- Ghith, N.; Ammari, A.B.; Rasmussen, M.; Frølich, A.; Cooper, K.; Tønnesen, H. Impact of compliance on quit rates in a smoking cessation intervention: Population study in Denmark. Clin. Health Promot. 2012, 2, 111–119. [Google Scholar]
- Neumann, T.; Rasmussen, M.; Ghith, N.; Heitmann, B.L.; Tønnesen, H. The Gold Standard Programme: Smoking cessation interventions for disadvantaged smokers are effective in a real-life setting. Tob. Contr. 2012. [Google Scholar] [CrossRef] [Green Version]
- Neumann, T.; Rasmussen, M.; Heitmann, B.L.; Tønnesen, H. Smoking cessation among heavy smokers in a real life setting. Int. J. Environ. Res. Public Health 2013. under review. [Google Scholar]
- Lind, M.; Jaspers, K. Manual til rygeafvænning i grupper (Manual for smoking cessation in groups), 2nd ed.; Danish Cancer Association: Copenhagen, Denmark, 2008. [Google Scholar]
- Lind, M.; Jaspers, K.; Kjaer, N.T. Rygeafvænning—Teori og praksis for professionelle rådgivere (Smoking Cessation—Theory and Practice of Professional Counsellors), 1st ed.; Danish Cancer Association: Copenhagen, Denmark, 2009. [Google Scholar]
- Lind, M.; Jaspers, K. Manual til individuel rygeafvænning (Manual for Individual Smoking Cessation), 5th ed.; Danish Cancer Association: Copenhagen, Denmark, 2011. [Google Scholar]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Fagerström, K.O. The Fagerström test for nicotine dependence: A revision of the Fagerström Tolerance Questionnaire. Br. J. Addict. 1991, 86, 1119–1127. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef]
- West, R.; Hajek, P.; Stead, L.; Stapleton, J. Outcome criteria in smoking cessation trials: Proposal for a common standard. Addiction 2005, 100, 299–303. [Google Scholar] [CrossRef]
- Myung, S.; Ju, W.; Jung, H.; Park, C.; Oh, S.; Seo, H.; Kim, H. Efficacy and safety of pharmacotherapy for smoking cessation among pregnant smokers: A meta-analysis. BJOG 2012, 119, 1029–1039. [Google Scholar] [CrossRef]
- Brose, L.S.; McEwen, A.; West, R. Association between nicotine replacement therapy use in pregnancy and smoking cessation. Drug Alcohol Depend. 2013. [Google Scholar] [CrossRef]
- Fidler, J.; Ferguson, S.G.; Brown, J.; Stapleton, J.; West, R. How does rate of smoking cessation vary by age, gender and social grade? Findings from a population survey in England. Addiction 2013. [Google Scholar] [CrossRef]
- Messer, K.; Trinidad, D.R.; Al-Delaimy, W.K.; Pierce, J.P. Smoking cessation rates in the United States: A comparison of young adult and older smokers. Am. J. Public Health 2008, 98, 317–322. [Google Scholar] [CrossRef]
- Medicinhåndbogen (The Medicine Handbook). Available online: http://pro.medicin.dk/ Laegemiddelgrupper/Grupper/315353#MASTER (accessed on 3 July 2013).
- Poulsen, P.B.; Dollerup, J.; Møller, A.M. Is a percentage a percentage? Systematic review of the effectiveness of Scandinavian behavioural modification smoking cessation programmes. Clin. Respir. J. 2010, 4, 3–12. [Google Scholar] [CrossRef]
- Judge, K.; Bauld, L.; Chesterman, J.; Ferguson, J. The English smoking treatment services: Short-term outcomes. Addiction 2005, 100 (Suppl), 46–58. [Google Scholar]
- Lumley, J.; Chamberlain, C.; Dowswell, T.; Oliver, S.; Oakley, L.; Watson, L. Interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst. Rev. 2009. [Google Scholar] [CrossRef]
- Pisinger, C.; Vestbo, J.; Borch-Johnsen, K.; Thomsen, T.; Jørgensen, T. Acceptance of the smoking cessation intervention in a large population-based study: The Inter99 study. Scand. J. Public Health 2005, 33, 138–145. [Google Scholar] [CrossRef]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Rasmussen, M.; Heitmann, B.L.; Tønnesen, H. Effectiveness of the Gold Standard Programmes (GSP) for Smoking Cessation in Pregnant and Non-Pregnant Women. Int. J. Environ. Res. Public Health 2013, 10, 3653-3666. https://doi.org/10.3390/ijerph10083653
Rasmussen M, Heitmann BL, Tønnesen H. Effectiveness of the Gold Standard Programmes (GSP) for Smoking Cessation in Pregnant and Non-Pregnant Women. International Journal of Environmental Research and Public Health. 2013; 10(8):3653-3666. https://doi.org/10.3390/ijerph10083653
Chicago/Turabian StyleRasmussen, Mette, Berit Lilienthal Heitmann, and Hanne Tønnesen. 2013. "Effectiveness of the Gold Standard Programmes (GSP) for Smoking Cessation in Pregnant and Non-Pregnant Women" International Journal of Environmental Research and Public Health 10, no. 8: 3653-3666. https://doi.org/10.3390/ijerph10083653






