High-Intensity Interval Training for Overweight Adolescents: Program Acceptance of a Media Supported Intervention and Changes in Body Composition
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Intervention
2.4. Measurements and Study Endpoints
2.5. Questionnaires
2.6. Statistical Analyses
3. Results
3.1. Recruitment
3.2. Leisure Time Habits and Physical Activity Enjoyment
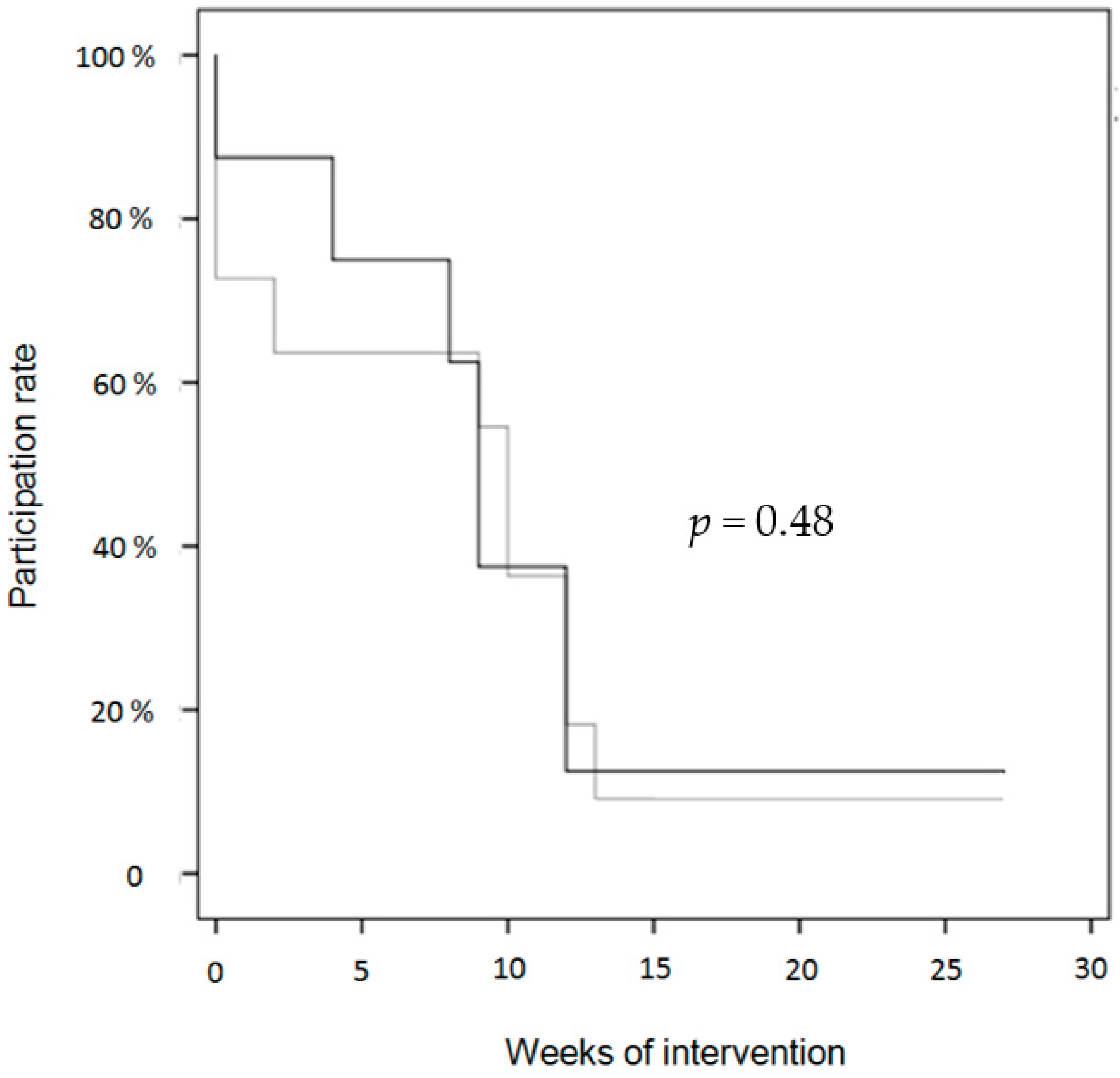
3.3. Program Attendance
3.4. Program Acceptance/Evaluation
3.5. Anthropometric Parameters
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| HIIT | High-intensity interval raining |
| WHtR | Waist-to-height ratio |
References
- Kohl, H.W., 3rd; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S. The pandemic of physical inactivity: Global action for public health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef]
- WHO Global Recommendation on Physical Activity for Health 5–17 Year Olds. Available online: http://www.who.int/dietphysicalactivity/publications/physical-activity-recommendations-5-17years.pdf?ua=1 (accessed on 30 September 2016).
- Lampert, T.; Mensink, G.B.; Romahn, N.; Woll, A. Physical activity among children and adolescents in Germany. Results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2007, 50, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Finne, E.; Bucksch, J.; Lampert, T.; Kolip, P. Age, puberty, body dissatisfaction, and physical activity decline in adolescents. Results of the German Health Interview and Examination Survey (KiGGS). Int. J. Behav. Nutr. Phys. Act. 2011, 8, 119. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S.J.; Petrolini, I.; Pearson, N. Interventions designed to reduce sedentary behaviours in young people: A review of reviews. Br. J. Sports Med. 2014, 48, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.L.; Wilkosz, M.E. Efficacy of technology-based interventions for obesity prevention in adolescents: A systematic review. Adolesc. Health Med. Ther. 2014, 5, 159–170. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.K.; Costigan, S.A.; Morgan, P.J.; Lubans, D.R.; Stodden, D.F.; Salmon, J.; Barnett, L.M. Do school-based interventions focusing on physical activity, fitness, or fundamental movement skill competency produce a sustained impact in these outcomes in children and adolescents? A systematic review of follow-up studies. Sports Med. 2014, 44, 67–79. [Google Scholar] [CrossRef] [PubMed]
- Bond, B.; Cockcroft, E.J.; Williams, C.A.; Harris, S.; Gates, P.E.; Jackman, S.R.; Armstrong, N.; Barker, A.R. Two weeks of high-intensity interval training improves novel but not traditional cardiovascular disease risk factors in adolescents. Am. J. Physiol. Heart Circ. Physiol. 2015, 309, H1039–H1047. [Google Scholar] [CrossRef] [PubMed]
- Taylor, K.L.; Weston, M.; Batterham, A.M. Evaluating intervention fidelity: An example from a high-intensity interval training study. PLoS ONE 2015, 10, e0125166. [Google Scholar] [CrossRef] [PubMed]
- Costigan, S.A.; Eather, N.; Plotnikoff, R.C.; Taaffe, D.R.; Lubans, D.R. High-intensity interval training for improving health-related fitness in adolescents: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 1253–1261. [Google Scholar] [CrossRef] [PubMed]
- Logan, G.R.; Harris, N.; Duncan, S.; Schofield, G. A review of adolescent high-intensity interval training. Sports Med. 2014, 44, 1071–1085. [Google Scholar] [CrossRef] [PubMed]
- Buchan, D.S.; Ollis, S.; Young, J.D.; Thomas, N.E.; Cooper, S.M.; Tong, T.K.; Nie, J.; Malina, R.M.; Baker, J.S. The effects of time and intensity of exercise on novel and established markers of CVD in adolescent youth. Am. J. Hum. Biol. 2011, 23, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Daussin, F.N.; Zoll, J.; Ponsot, E.; Dufour, S.P.; Doutreleau, S.; Lonsdorfer, E.; Ventura-Clapier, R.; Mettauer, B.; Piquard, F.; Geny, B.; et al. Training at high exercise intensity promotes qualitative adaptations of mitochondrial function in human skeletal muscle. J. Appl. Physiol. (1985) 2008, 104, 1436–1441. [Google Scholar] [CrossRef] [PubMed]
- Racil, G.; Ben Ounis, O.; Hammouda, O.; Kallel, A.; Zouhal, H.; Chamari, K.; Amri, M. Effects of high vs. moderate exercise intensity during interval training on lipids and adiponectin levels in obese young females. Eur. J. Appl. Physiol. 2013, 113, 2531–2540. [Google Scholar] [CrossRef] [PubMed]
- Weston, M.; Taylor, K.L.; Batterham, A.M.; Hopkins, W.G. Effects of low-volume high-intensity interval training (HIT) on fitness in adults: A meta-analysis of controlled and non-controlled trials. Sports Med. 2014, 44, 1005–1017. [Google Scholar] [CrossRef] [PubMed]
- Blüher, S.; Käpplinger, J.; Herget, S.; Reichhardt, S.; Böttcher, Y.; Grimm, A.; Kratzsch, J.; Petroff, D. Adipocyte fatty acid binding protein (aFABP) is related to cardiometabolic risk markers in obese adolescents—A study involving high-intensity interval training (HIIT). Metabolism 2016, in press. [Google Scholar]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. J. Pharmacol. Pharmacother. 2010, 1, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Kromeyer-Hauschild, K.; Wabitsch, M.; Kunze, D.; Geller, F.; Geiß, H.C.; Hesse, V.; von Hippel, A.; Jäger, U.; Johnsen, D.; Korte, W.; et al. Perzentile für den Body-mass-Index für das Kindes- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Percentiles of body mass index in children and adolescents evaluated from different regional German cohorts. Monatsschr. Kinderheilkd. 2001, 149, 807–818. [Google Scholar] [CrossRef]
- Boucoul, R.; Fernandes, M.; Oliveira Carvalho, V. Six-minute walking test in children. Disabil. Rehabil. 2013, 35, 1586–1587. [Google Scholar] [CrossRef] [PubMed]
- Vanhelst, J.; Fardy, P.S.; Salleron, J.; Béghin, L. The six-minute walk test in obese youth: Reproducibility, validity, and prediction equation to assess aerobic power. Disabil. Rehabil. 2013, 35, 479–482. [Google Scholar] [CrossRef] [PubMed]
- Emberts, T.; Porcari, J.; Dobers-Tein, S.; Steffen, J.; Foster, C. Exercise intensity and energy expenditure of a tabata workout. J. Sports Sci. Med. 2013, 12, 612–613. [Google Scholar] [PubMed]
- Little, J.P.; Safdar, A.; Wilkin, G.P.; Tarnopolsky, M.A.; Gibala, M.J. A practical model of low-volume high-intensity interval training induces mitochondrial biogenesis in human skeletal muscle: Potential mechanisms. J. Physiol. 2010, 588, 1011–1022. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef] [PubMed]
- Bluher, S.; Petroff, D.; Wagner, A.; Warich, K.; Gausche, R.; Klemm, T.; Wagner, M.; Keller, A. The one year exercise and lifestyle intervention program KLAKS: Effects on anthropometric parameters, cardiometabolic risk factors and glycemic control in childhood obesity. Metabolism 2014, 63, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Green, P.J. Smoothing reference centile curves: The LMS method and penalized likelihood. Stat. Med. 1992, 11, 1305–1319. [Google Scholar] [CrossRef] [PubMed]
- Kromeyer-Hauschild, K.; Neuhauser, H.; Schaffrath Rosario, A.; Schienkiewitz, A. Abdominal obesity in German adolescents defined by waist-to-height ratio and its association to elevated blood pressure: The KiGGS study. Obes. Facts 2013, 6, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Slaughter, M.H.; Lohman, T.G.; Boileau, R.A.; Horswill, C.A.; Stillman, R.J.; van Loan, M.D.; Bemben, D.A. Skinfold equations for estimation of body fatness in children and youth. Hum. Biol. 1998, 60, 709–723. [Google Scholar]
- Ardelt-Gattinger, E.; Moorehead, M. (Eds.) Skala zum Körperbild (SKB). In AD-EVA Interdisziplinäres Testsystem zur Diagnostik und Evaluation bei Adipositas und Anderen Durch Ess-und Bewegungsverhalten Beeinflussbaren Krankheiten (AD-EVA) (Modul1) Manual zum Theretischen Hintergrund und zur Testentwicklung; Verlag Hans Huber-Hogrefe: Bern, Switzerland, 2010; pp. 208–222.
- Dewar, D.L.; Lubans, D.R.; Morgan, P.J.; Plotnikoff, R.C. Development and evaluation of social cognitive measures related to adolescent physical activity. J. Phys. Act. Health 2013, 10, 544–555. [Google Scholar] [CrossRef] [PubMed]
- Durso, L.E.; Latner, J.D. Understanding self-directed stigma: Development of the weight bias internalization scale. Obesity 2008, 16 (Suppl. 2), S80–S86. [Google Scholar] [CrossRef] [PubMed]
- Jekauc, D.; Voelkle, M.; Wagner, M.O.; Mewes, N.; Woll, A. Reliability, validity, and measurement invariance of the German version of the physical activity enjoyment scale. J. Pediatr. Psychol. 2013, 38, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Jekauc, D.; Wagner, M.; Kahlert, D.; Woll, A. Reliabilität und Validität des MoMo-Aktivitätsfragebogens für Jugendliche (MoMo-AFB). Diagnostica 2013, 59, 100–111. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Auquier, P.; Erhart, M.; Gosch, A.; Rajmil, L.; Bruil, J.; Power, M.; Duer, W.; Cloetta, B.; Czemy, L.; et al. The KIDSCREEN-27 quality of life measure for children and adolescents: Psychometric results from a cross-cultural survey in 13 European countries. Qual. Life Res. 2007, 16, 1347–1356. [Google Scholar] [CrossRef] [PubMed]
- Fay, M.P.; Proschan, M.A. Wilcoxon-Mann-Whitney or t-test? On assumptions for hypothesis tests and multiple interpretations of decision rules. Stat. Surv. 2010, 4, 1–39. [Google Scholar] [CrossRef] [PubMed]
- Sawilowsky, S.S.; Blair, R.C. A more realistic look at the robustness and Type II error properties of the t test to departures from population normality. Psychol. Bull. 1992, 111, 352–360. [Google Scholar] [CrossRef]
- The R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2010. [Google Scholar]
- Graf, C. Preventing and treating obesity in pediatrics through physical activity. EPMA J. 2011, 2, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Graf, C.; Beneke, R.; Bloch, W.; Bucksch, J.; Dordel, S.; Eiser, S.; Ferrari, N.; Koch, B.; Krug, S.; Lawrenz, W.; et al. Recommendations for promoting physical activity for children and adolescents in Germany. A consensus statement. Obes. Facts 2014, 7, 178–190. [Google Scholar] [PubMed]
- Jung, M.E.; Bourne, J.E.; Little, J.P. Where does HIT fit? An examination of the affective response to high-intensity intervals in comparison to continuous moderate- and continuous vigorous-intensity exercise in the exercise intensity-affect continuum. PLoS ONE 2014, 9, e114541. [Google Scholar] [CrossRef] [PubMed]
- Keteyian, S.J.; Hibner, B.A.; Bronsteen, K.; Kerrigan, D.; Aldred, H.A.; Reasons, L.M.; Saval, M.A.; Brawner, C.A.; Schairer, J.R.; Thompson, T.M.; et al. Greater improvement in cardiorespiratory fitness using higher-intensity interval training in the standard cardiac rehabilitation setting. J. Cardiopulm. Rehabil. Prev. 2014, 34, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Little, J.P.; Jung, M.E.; Wright, A.E.; Wright, W.; Manders, R.J. Effects of high-intensity interval exercise versus continuous moderate-intensity exercise on postprandial glycemic control assessed by continuous glucose monitoring in obese adults. Appl. Physiol. Nutr. Metab. 2014, 39, 835–841. [Google Scholar] [CrossRef] [PubMed]
- Shaban, N.; Kenno, K.A.; Milne, K.J. The effects of a 2 week modified high intensity interval training program on the homeostatic model of insulin resistance (HOMA-IR) in adults with type 2 diabetes. J. Sports Med. Phys. Fit. 2014, 54, 203–209. [Google Scholar]
- De Feo, P. Is high-intensity exercise better than moderate-intensity exercise for weight loss? Nutr. Metab. Cardiovasc. Dis. 2013, 23, 1037–1042. [Google Scholar] [CrossRef] [PubMed]
- Tate, D.F.; LaRose, J.G.; Griffin, L.P.; Erickson, K.E.; Robichaud, E.F.; Perdue, L.; Espeland, M.A.; Wing, R.R. Recruitment of young adults into a randomized controlled trial of weight gain prevention: Message development, methods, and cost. Trials 2014, 15, 326. [Google Scholar] [CrossRef] [PubMed]
- Hartlieb, K.B.; Jacques-Tiura, A.J.; Naar-King, S.; Ellis, D.A.; Jen, K.L.; Marshall, S. Recruitment strategies and the retention of obese urban racial/ethnic minority adolescents in clinical trials: The FIT families project, Michigan, 2010–2014. Prev. Chronic Dis. 2015, 12, 140409. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.L.; Straker, L.M.; McManus, A.; Fenner, A.A. Barriers and enablers for participation in healthy lifestyle programs by adolescents who are overweight: A qualitative study of the opinions of adolescents, their parents and community stakeholders. BMC Pediatr. 2014, 14, 53. [Google Scholar] [CrossRef] [PubMed]
- Costigan, S.A.; Eather, N.; Plotnikoff, R.C.; Taaffe, D.R.; Pollock, E.; Kennedy, S.G.; Lubans, D.R. Preliminary efficacy and feasibility of embedding high intensity interval training into the school day: A pilot randomized controlled trial. Prev. Med. Rep. 2015, 2, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Weston, K.L.; Azevedo, L.B.; Bock, S.; Weston, M.; George, K.P.; Batterham, A.M. Effect of Novel, School-Based High-Intensity Interval Training (HIT) on Cardiometabolic Health in Adolescents: Project FFAB (Fun Fast Activity Blasts)—An Exploratory Controlled Before-and-After Trial. PLoS ONE 2016, 11, e0159116. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, B.; Shrewsbury, V.A.; O’Connor, J.; Lau, C.; Steinbeck, K.S.; Hill, A.J.; Baur, L.A. A process evaluation of an adolescent weight management intervention: Findings and recommendations. Health Promot. Int. 2015, 30, 201–212. [Google Scholar] [CrossRef] [PubMed]
- Hadziabdic, M.O.; Mucalo, I.; Hrabac, P.; Matic, T.; Rahelic, D.; Bozikov, V. Factors predictive of drop-out and weight loss success in weight management of obese patients. J. Hum. Nutr. Diet. 2015, 28 (Suppl. 2), 24–32. [Google Scholar] [CrossRef] [PubMed]
- Walker, S.E.; Smolkin, M.E.; O’Leary, M.L.; Cluett, S.B.; Norwood, V.F.; Deboer, M.D.; Gurka, M.J. Predictors of retention and BMI loss or stabilization in obese youth enrolled in a weight loss intervention. Obes. Res. Clin. Pract. 2012, 6, e330–e339. [Google Scholar] [CrossRef] [PubMed]
- Donini, L.M.; Cuzzolaro, M.; Gnessi, L.; Lubrano, C.; Migliaccio, S.; Aversa, A.; Pinto, A.; Lenzi, A. Obesity treatment: Results after 4 years of a nutritional and psycho-physical rehabilitation program in an outpatient setting. Eat. Weight Disords 2014, 19, 249–260. [Google Scholar] [CrossRef] [PubMed]
- De Niet, J.; Timman, R.; Jongejan, M.; Passchier, J.; van den Akker, E. Predictors of participant dropout at various stages of a pediatric lifestyle program. Pediatrics 2011, 127, e164–e170. [Google Scholar] [CrossRef] [PubMed]
- McGoey, T.; Root, Z.; Bruner, M.W.; Law, B. Evaluation of physical activity interventions in youth via the Reach, Efficacy/Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework: A systematic review of randomised and non-randomised trials. Prev. Med. 2015, 76, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Markowitz, J.T.; Cousineau, T.; Franko, D.L.; Schultz, A.T.; Trant, M.; Rodgers, R.; Laffel, L.M. Text messaging intervention for teens and young adults with diabetes. J. Diabetes Sci. Technol. 2014, 8, 1029–1034. [Google Scholar] [CrossRef] [PubMed]
- Riiser, K.; Londal, K.; Ommundsen, Y.; Smastuen, M.C.; Misvaer, N.; Helseth, S. The outcomes of a 12-week Internet intervention aimed at improving fitness and health-related quality of life in overweight adolescents: The Young & Active controlled trial. PLoS ONE 2014, 9, e114732. [Google Scholar]
- Prestwich, A.; Perugini, M.; Hurling, R. Can the effects of implementation intentions on exercise be enhanced using text messages? Psychol. Health 2009, 24, 677–687. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.; Ferguson, M.; Vandelanotte, C.; Plotnikoff, R.; de Bourdeaudhuij, I.; Thomas, S.; Nelson-Field, K.; Olds, T. A Web-based, social networking physical activity intervention for insufficiently active adults delivered via facebook app: Randomized controlled trial. J. Med. Internet Res. 2015, 17, e174. [Google Scholar] [CrossRef] [PubMed]
- Weston, K.S.; Wisloff, U.; Coombes, J.S. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: A systematic review and meta-analysis. Br. J. Sports Med. 2014, 48, 1227–1234. [Google Scholar] [CrossRef] [PubMed]

| Time | Month 1 | Month 2 | Month 3 | Month 4 | Month 5 | Month 6 |
|---|---|---|---|---|---|---|
| Media support (social cognitive theory) example message (shortened) | General attitude of physical activity “Physical activity is beneficial for your health and well-being. The moveHIT program can help you to improve your fitness!” | Outcome expectations “By attending the moveHIT program twice a week, you can increase your muscle strength and feel more flexible.” | Behavioral strategies to practice HIIT “Write down the dates for the training in your calendar, to remind yourself to come to the moveHIT program.” | Seeking social support for physical activity “Tell your friends and family of the moveHIT program. They can join for a trial session and exercise with you.” | Increasing self-efficacy in HIIT “We have noticed your improvements in the training and you will have noticed that you can perform the exercises more easily now!” | Practicing social cognitive constructs “Think of the last months and keep reminding yourself of the training sessions and include your friends and family in your physical activity regimen.” |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herget, S.; Reichardt, S.; Grimm, A.; Petroff, D.; Käpplinger, J.; Haase, M.; Markert, J.; Blüher, S. High-Intensity Interval Training for Overweight Adolescents: Program Acceptance of a Media Supported Intervention and Changes in Body Composition. Int. J. Environ. Res. Public Health 2016, 13, 1099. https://doi.org/10.3390/ijerph13111099
Herget S, Reichardt S, Grimm A, Petroff D, Käpplinger J, Haase M, Markert J, Blüher S. High-Intensity Interval Training for Overweight Adolescents: Program Acceptance of a Media Supported Intervention and Changes in Body Composition. International Journal of Environmental Research and Public Health. 2016; 13(11):1099. https://doi.org/10.3390/ijerph13111099
Chicago/Turabian StyleHerget, Sabine, Sandra Reichardt, Andrea Grimm, David Petroff, Jakob Käpplinger, Michael Haase, Jana Markert, and Susann Blüher. 2016. "High-Intensity Interval Training for Overweight Adolescents: Program Acceptance of a Media Supported Intervention and Changes in Body Composition" International Journal of Environmental Research and Public Health 13, no. 11: 1099. https://doi.org/10.3390/ijerph13111099






