Whole of Systems Trial of Prevention Strategies for Childhood Obesity: WHO STOPS Childhood Obesity
Abstract
:1. Introduction
1.1. A Sustainable Monitoring System
1.2. Whole of Community Systems Measures and Interventions
2. Methods
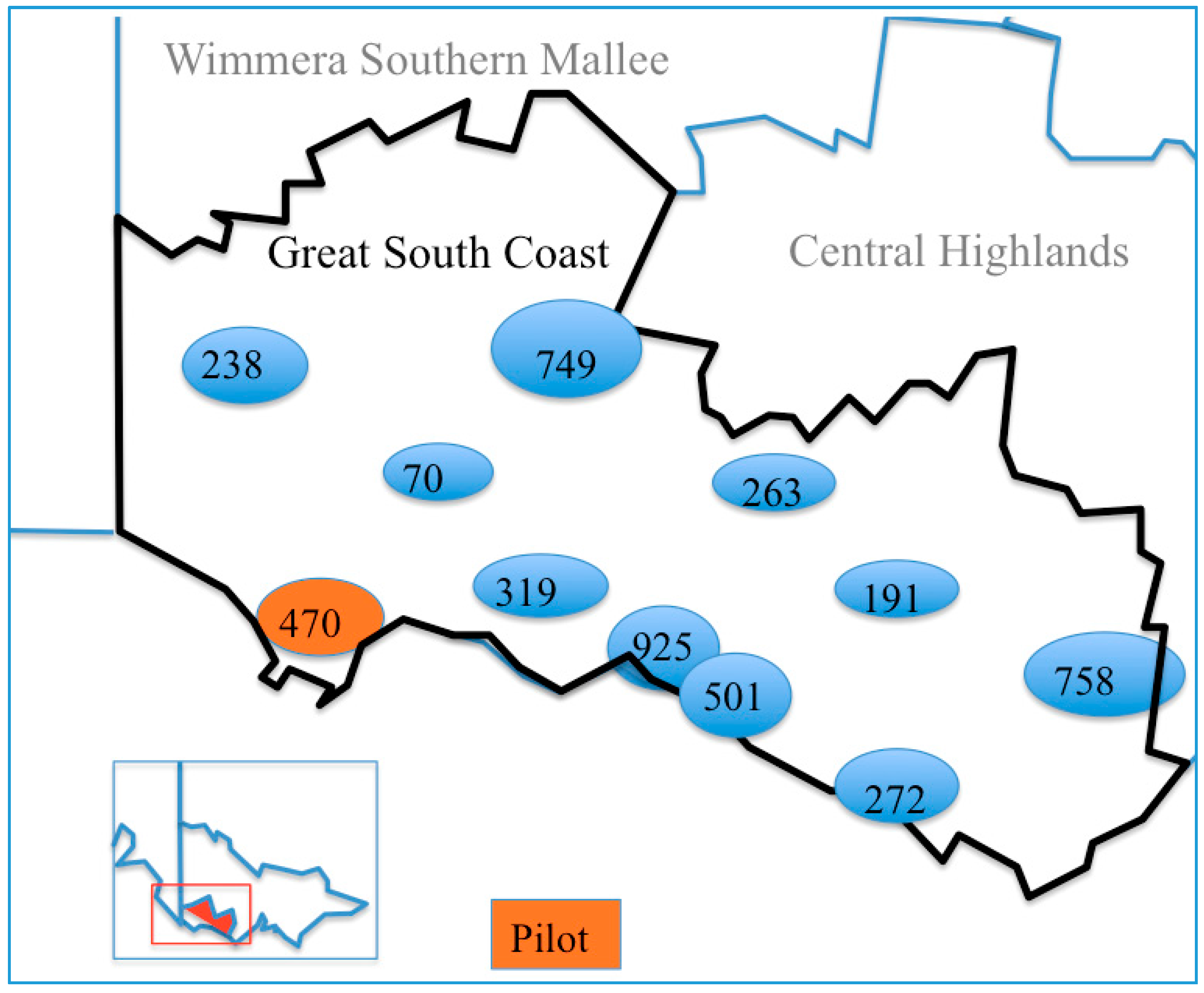
2.1. Study Population
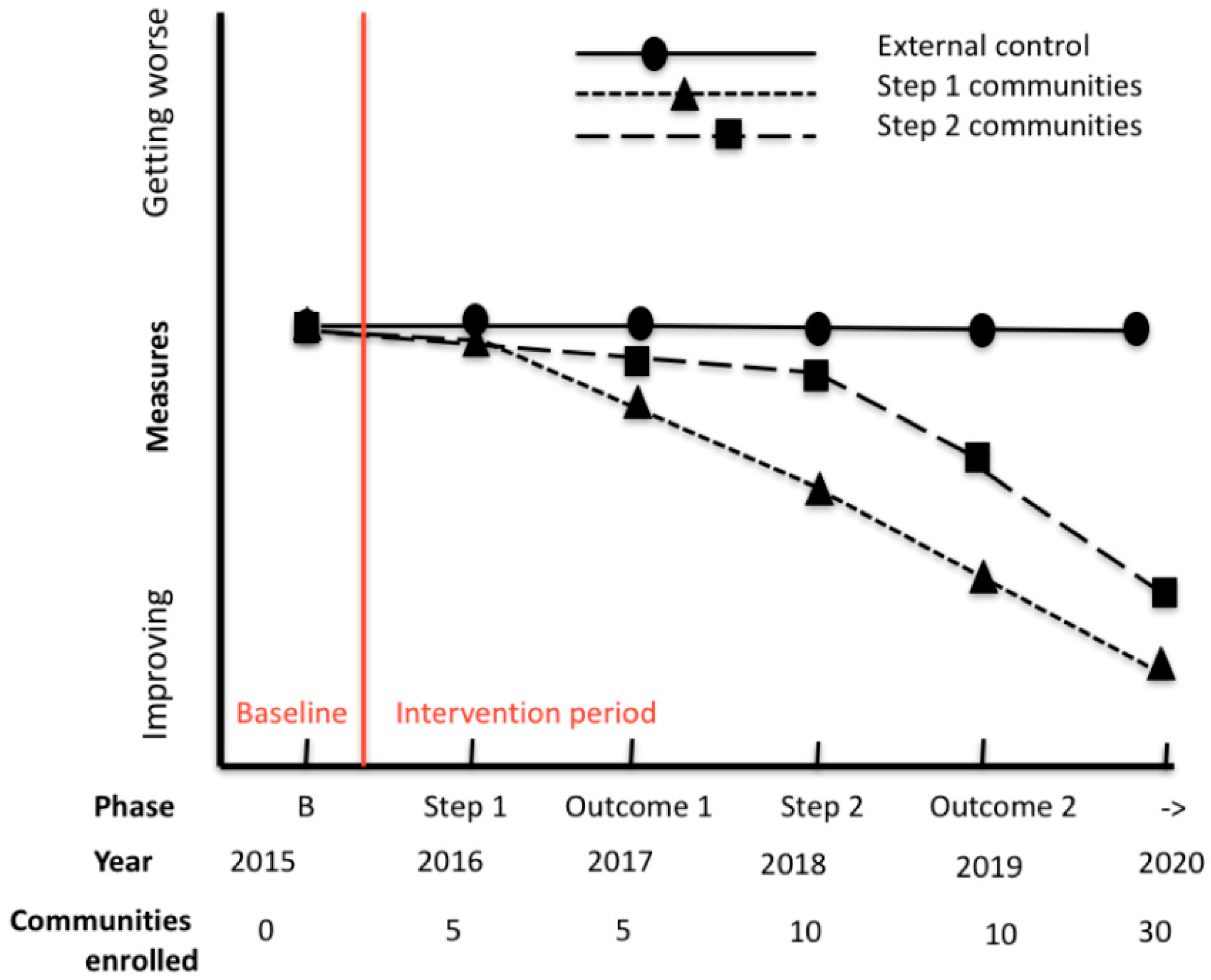
2.2. Intervention
2.3. Characterizing and Intervening in Systems
Systems Maps
2.4. Evaluation
2.4.1. External Control Communities
2.4.2. Primary and Secondary Outcomes
2.4.3. Anthropometry and Behaviours
2.5. Measures/Instruments
2.6. Procedures
2.7. Sample Size
2.8. Environmental Audits
2.9. Ethics Approvals
3. Analysis Plan
Economic Evaluation
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ABM | Agent-Based Model |
| ACTRN | Australian New Zealand Clinical Trials |
| BAEW | Be Active Eat Well |
| BMI | Body Mass Index |
| BMI-z | Body Mass Index z score |
| DES | Discrete Event Simulation |
| DU-HREC | Deakin University’s Human Research Ethics Committee |
| GLOBE | Global Obesity Centre |
| GMB | Group Model Building |
| GSCRV | Great South Coast Region of Victoria |
| HEAG-H | Deakin University’s Human Ethics Advisory Group-Health |
| ISCOLE | International Study of Childhood Obesity, Lifestyle and the Environment |
| SD | System Dynamics |
| SNA | Social Network Snalysis |
| WHO | World Health Organization |
| STOPS | Whole of Systems Trial of Prevention Strategies |
References
- Colagiuri, S.; Lee, C.M.Y.; Colagiuri, R.; Magliano, D.; Shaw, J.E.; Zimmet, P.Z.; Caterson, I.D. The cost of overweight and obesity in Australia. Med. J. Aust. 2010, 192, 260–264. [Google Scholar] [PubMed]
- Australian Bureau of Statistics. Australian Health Survey: First Results, 2014–2015. Available online: http://www.abs.gov.au/ausstats/[email protected]/mf/4364.0.55.001 (accessed on 22 March 2016).
- Hoad, V.; Somerford, P.; Katzenellenbogen, J. High body mass index overtakes tobacco as the leading independent risk factor contributing to disease burden in Western Australia. Aust. N. Z. J. Public Health 2010, 34, 214–215. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Mulder, C.; Twisk, J.; van Mechelen, W.; Chinapaw, M. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes. Rev. 2008, 9, 474–488. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Waters, E.; de Silva-Sanigorski, A.; Hall, B.J.; Brown, T.; Campbell, K.J.; Gao, Y.; Armstrong, R.; Prosser, L.; Summerbell, C.D. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011. [Google Scholar] [CrossRef]
- De Silva-Sanigorski, A.M.; Bell, A.C.; Kremer, P.; Nichols, M.; Crellin, M.; Smith, M.; Sharp, S.; de Groot, F.; Carpenter, L.; Boak, R.; et al. Reducing obesity in early childhood: Results from Romp & Chomp, an Australian community-wide intervention program. Am. J. Clin. Nutr. 2010, 91, 831–840. [Google Scholar] [PubMed]
- Millar, L.; Kremer, P.; de Silva-Sanigorski, A.; McCabe, M.; Mavoa, H.; Moodie, M.; Utter, J.; Bell, C.; Malakellis, M.; Mathews, L.; et al. Reduction in overweight and obesity from a 3 year community-based intervention in Australia: The “It’s Your Move!” project. Obes. Rev. 2011, 12, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Sanigorski, A.M.; Bell, A.C.; Kremer, P.J.; Cuttler, R.; Swinburn, B.A. Reducing unhealthy weight gain in children through community capacity-building: Results of a quasi-experimental intervention program, Be Active Eat Well. Int. J. Obes. 2008, 32, 1060–1067. [Google Scholar] [CrossRef] [PubMed]
- Millar, L.; Robertson, N.; Allender, S.; Nichols, M.; Bennett, C.; Swinburn, B. Increasing community capacity and decreasing prevalence of overweight and obesity in a community based intervention among Australian adolescents. Prev. Med. 2013, 56, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Swinburn, B.; Dietz, W.; Kleinert, S. A lancet commission on obesity. Lancet 2015, 386, 1716–1717. [Google Scholar] [CrossRef]
- Gortmaker, S.L.; Swinburn, B.A.; Levy, D.; Carter, R.; Mabry, P.L.; Finegood, D.T.; Huang, T.; Marsh, T.; Moodie, M.L. Changing the future of obesity: Science, policy, and action. Lancet 2011, 378, 838–847. [Google Scholar] [CrossRef]
- New Zealand Government. Healthy Families New Zealand. Available online: http://www.healthyfamilies.govt.nz/#home-2 (accessed on 3 November 2015).
- Leeds Beckett University. Whole Systems Approach to Tackle Obesity. Available online: http://www.leedsbeckett.ac.uk/wholesystemsobesity/ (accessed on 12 August 2016).
- Sorensen, G.; Emmons, K.; Hunt, M.K.; Johnston, D. Implications of the results of community intervention trials. Ann. Rev. Public Health 1998, 19, 379–416. [Google Scholar] [CrossRef] [PubMed]
- Richardson, G.P. Reflections on the foundations of system dynamics. Sys. Dyn. Rev. 2011, 27, 219–243. [Google Scholar] [CrossRef]
- Crooks, N.; Strugnell, C.; Bell, C.; Allender, S. A sustainable and high participation childhood obesity monitoring system in regional Victoria, Australia. Aust. N. Z. J. Public Health 2016. Accepted. [Google Scholar]
- Brown, C.A.; Lilford, R.J. The stepped wedge trial design: A systematic review. BMC Med. Res. Methodol. 2006, 6, 54–54. [Google Scholar] [CrossRef] [PubMed]
- Hainaut, P. The Gambia hepatitis intervention study (GHIS). Iatreia 2007, 20, S21–S22. [Google Scholar]
- Brimblecombe, J.; Ferguson, M.; Liberato, S.C.; Ball, K.; Moodie, M.L.; Magnus, A.; Miles, E.; Leach, A.J.; Chatfield, M.D.; Mhurchu, C.N.; et al. Stores healthy options project in remote indigenous communities (SHOP@RIC): A protocol of a randomised trial promoting healthy food and beverage purchases through price discounts and in-store nutrition education. BMC Public Health 2013, 13. [Google Scholar] [CrossRef] [PubMed]
- Hemming, K.; Lilford, R.; Girling, A.J. Stepped-wedge cluster randomised controlled trials: A generic framework including parallel and multiple-level designs. Stat. Med. 2015, 34, 181–196. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, N.G.; Sanson-Fisher, R.W.; Shakeshaft, A.; D’Este, C.; Green, L.W. Theme article: The multiple baseline design for evaluating population-based research. Am. J. Prev. Med. 2007, 33, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Mdege, N.D.; Man, M.S.; Taylor Nee Brown, C.A.; Torgerson, D.J. Systematic review of stepped wedge cluster randomized trials shows that design is particularly used to evaluate interventions during routine implementation. J. Clin. Epidemiol. 2011, 64, 936–948. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Everybody Business: Strengthening Health Systems to Improve Health Outcomes: Who’s Framework for Action. Available online: http://www.wpro.who.int/health_services/health_systems_framework/en/ (accessed on 21 July 2016).
- World Health Organization. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. Available online: http://www.who.int/healthinfo/systems/WHO_MBHSS_2010_full_web.pdf (accessed on 28 August 2016).
- Department of Health New South Wales. A Framework for Building Capacity to Improve Health; Department of Health Sydney: Sydney, Australia, 2001.
- Allender, S.; Owen, B.; Whelan, J.; Kuhlberg, J.; Lowe, J.; Nagorcka-Smith, P.; Bell, C. A community based systems diagram of obesity causes. PLoS ONE 2015, 10. [Google Scholar] [CrossRef] [PubMed]
- Simmons, A.; Reynolds, R.C.; Swinburn, B. Review: Defining community capacity building: Is it possible? Prev. Med. 2011, 52, 193–199. [Google Scholar] [PubMed]
- Carr, W.; Kemmis, S. Becoming Critical: Education, Knowledge and Action Research; Deakin University Press: Burwood, Australia, 1986. [Google Scholar]
- Graham, I.D.; Logan, J.; Harrison, M.B.; Straus, S.E.; Tetroe, J.; Caswell, W.; Robinson, N. Lost in knowledge translation: Time for a map? J. Contin. Educ. Health Prof. 2006, 26, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Rose, J.; Riolo, R.; Hovmand, P.S.; Cherng, S.; Ferrer, R.; Katerndahl, D.A. Modeling the paradox of primary care. In Handbook of Systems and Complexity in Health; Sturmberg, J.P., Martin, C.M., Eds.; Springer: Chicago, IL, USA, 2013. [Google Scholar]
- Black, L.J. When visual representations are boundary objects in system dynamics work. Syst. Dynam. Rev. 2013, 29, 70–86. [Google Scholar] [CrossRef]
- Black, L.J.; Andersen, D.F. Using visual representations as boundary objects to resolve conflict in collaborative model-building applications. Syst. Res. Behav. Sci. 2012, 29, 194–208. [Google Scholar] [CrossRef]
- Hovmand, P.S. Community Based System Dynamics; Springer: New York, NY, USA, 2014. [Google Scholar]
- Hovmand, P.S.; Andersen, D.F.; Rouwette, E.; Richardson, G.P.; Rux, K.; Calhoun, A. Group model building “scripts” as a collaborative tool. Syst. Res. Behav. Sci. 2012, 29, 179–193. [Google Scholar] [CrossRef]
- Scriptapedia. Available online: https://en.wikibooks.org/wiki/Scriptapedia (accessed on 15 June 2016).
- Strugnell, C.; Millar, L.; Churchill, A.; Jacka, F.; Bell, C.; Malakellis, M.; Swinburn, B.; Allender, S. Healthy together Victoria and childhood obesity-a methodology for measuring changes in childhood obesity in response to a community-based, whole of system cluster randomized control trial. Arch. Public Health 2016, 74. [Google Scholar] [CrossRef] [PubMed]
- Mathews, L.; Kremer, P.; Sanigorski, A.; Simmons, A.; Nichols, M.; Moodie, M. Nutrition and Physical Activity in Children and Adolescents; Report 1: Methods and Tools; Department of Human Services (Victoria): Victoria, Australia, 2009.
- Card, A.; Manske, S.; Mammen, G.; King, M.; Gleddie, D.; Schwartz Mobo, Y.E. Core Indicators and Measures of Youth Health Physical Activity and Sedentary Behaviour Module: Indicators and Questions to Use with Youth Respondents and/or School Setting Assessments; Memorial University of Newfoundland: St. John’s, NL, Canada, 2012. [Google Scholar]
- Wong, S.L.; Leatherdale, S.T.; Manske, S.R. ReliFability and validity of a school-based physical activity questionnaire. Med. Sci. Sports Exerc. 2006, 38, 1593–1600. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Australia’s Physical Activity and Sedentary Behaviour Guidelines Canberra: Australian Government. Available online: http://www.health.gov.au/internet/main/publishing.nsf/content/health-pubhlth-strateg-phys-act-guidelines#apa512 (accessed on 25 August 2014).
- Parletta, N.; Cooper, P.; Petkov, J.; O’Dea, K. Effects of fish oil supplementation on learning and behaviour of children from Australian Indigenous remote community schools: A randomised control trial. Prostagland Leuk. Essent. Fatty Acid. 2013, 89. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Eat for Health: Australian Dietary Guidelines Summary Canberra: Australian Government. Available online: https://www.eatforhealth.gov.au/sites/default/Ffiles/files/the_guidelines/n55a_australian_dietary_guidelines_summary_book.pdf (accessed on 4 April 2013).
- Varni, J.W.; Limbers, C.A.; Burwinkle, T.M. How young can children reliably and validly self-report their health-related quality of life? An analysis of 8591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health Qual. Life Outcomes 2007, 5. [Google Scholar] [CrossRef]
- Stevens, K.J. Working with children to develop dimensions for a preference-based, generic, pediatric, health-related quality-of-life measure. Qual. Health Res. 2010, 20, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Barreira, T.V.; Broyles, S.T.; Champagne, C.M.; Chaput, J.-P.; Fogelholm, M.; Hu, G.; Johnson, W.D.; Kuriyan, R.; Kurpad, A.; et al. The international study of childhood obesity, lifestyle and the environment (ISCOLE): Design and methods. BMC Public Health 2013, 13, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scholz, J.T.; Kile, B.; Berardo, R. Do networks solve collective action problems? Credibility, search, and collaboration. J. Polit. 2008, 70, 393–406. [Google Scholar] [CrossRef]
- Carrington, P.J.; Scott, J.; Wasserman, S. Models and Methods in Social Network Analysis; Cambridge University Press: Cambridge, UK, 2005. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria.
- Carter, R.; Moodie, M.; Markwick, A.; Magnus, A.; Vos, T.; Swinburn, B.; Haby, M.M. Assessing cost-effectiveness in obesity (ACE-Obesity): An overview of the ACE approach, economic methods and cost results. BMC Public Health 2009, 9. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Carter, R.; Barendregt, J.; Mihalopoulos, C.; Veerman, L.; Magnus, A. Assessing Cost-Effectiveness in Prevention: (ACE-Prevention): Final Report; Centre for Burden of Disease and Cost Effectiveness, School of Population Health, University of Queensland: Brisbane, Australia, 2010. [Google Scholar]
| Community Type | n | Baseline | Step 1 | Step 2 | ||
|---|---|---|---|---|---|---|
| Participant communities | 5 | # * (0) | # (0) | # * (0) | # (1) | # * (2) |
| 5 | # * (0) | # (1) | # * (2) | # (3) | # * (4) | |
| External control | 13 | * (0) | (0) | * (0) | (0) | * (0) |
| Year | 2015 | 2016 | 2017 | 2018 | 2019 | |
| Workshop | Content |
|---|---|
| 3 h Workshop 1 Problem Identification | Background, evidence, plan presentation; fill in community capacity index; develop system logic model for “causes of childhood obesity in their community” (outcomes evidence translation, baseline measurements, base systems model). |
| 3 hour Workshop 2 Problem Refinement | Further evidence presentation; fill in social network analysis questionnaires; validation of system logic model on contextualised caused of childhood obesity constructed from the previous workshop (outcomes-further baseline data and knowledge translation and first validation of model). |
| Half-day Workshop Solution Formulation and Prioritisation | Steering group recruits between 50 and 200 champions from across the community who validate the systems logia model and identify priority actions for each sub-system (e.g., water system, school system, food system) related to them (outcomes; wider community validation of model and action plans). |
| 2 h Workshop 2 Solution Integration | Review the consolidated priority actions (outcomes; translate to institutional action plans). |
| 1–2 h EvaluationSessions Adaptive Solutions | Steering: six monthly sessions to identify subsystem changes and modifications to the systems map (outcomes such as individual child measures, process change; follow up system measures). |
| Item | Outcome(s) of Interest | Instrument/Measure |
|---|---|---|
| Anthropometry | Body Mass Index-z score | Height and weight |
| Overweight and obesity prevalence [37,38] | ||
| Physical activity and sedentary behavior | Minutes per day (min·d−1) spent in moderate-to-vigorous physical activity and sedentary behavior | Modified Core Indicators and Measures of Youth Health [39] and School Health Action, Planning and Evaluation System [40] Accelerometer (sub sample) |
| Proportion of participants meeting the national physical activity guidelines and screen-time recommendations [41] | ||
| Diet Type, frequency | Usual serves of: fruit and vegetable daily | Modified version of the Simple Dietary Questionnaire [42] |
| Usual frequency of non-core foods (e.g., take-away food, chips, lollies, chocolate) | ||
| Usual frequency of sugar-sweetened beverages | ||
| Proportion of participants meeting the Australian Dietary guidelines for fruit and vegetable intakes [43] | ||
| Quality of life | Global summary score | Paediatric Quality of Life Inventory 4.0 (PedsQL)TM [44] CHU-9D Child Health Utility Index [45] |
| Physiological health summary score | ||
| Physical health summary score | ||
| Child Health Utility Index (CHU-9D ) | ||
| Environments | School healthy eating and activity policies and practices | Modified version of the Be Active Eat Well Environment audit [38], the International study of childhood obesity, lifestyle and the environment tool [46] |
| Adherence to physical education and sport education mandate for Victorian primary schools | ||
| Social networks (ecological data) | Characteristics of Community Leader social networks | Validated measures of socio-centric and ego-centric communication and collaboration networks |
| Density, diffusion, change dynamics, key players |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allender, S.; Millar, L.; Hovmand, P.; Bell, C.; Moodie, M.; Carter, R.; Swinburn, B.; Strugnell, C.; Lowe, J.; De la Haye, K.; et al. Whole of Systems Trial of Prevention Strategies for Childhood Obesity: WHO STOPS Childhood Obesity. Int. J. Environ. Res. Public Health 2016, 13, 1143. https://doi.org/10.3390/ijerph13111143
Allender S, Millar L, Hovmand P, Bell C, Moodie M, Carter R, Swinburn B, Strugnell C, Lowe J, De la Haye K, et al. Whole of Systems Trial of Prevention Strategies for Childhood Obesity: WHO STOPS Childhood Obesity. International Journal of Environmental Research and Public Health. 2016; 13(11):1143. https://doi.org/10.3390/ijerph13111143
Chicago/Turabian StyleAllender, Steven, Lynne Millar, Peter Hovmand, Colin Bell, Marj Moodie, Rob Carter, Boyd Swinburn, Claudia Strugnell, Janette Lowe, Kayla De la Haye, and et al. 2016. "Whole of Systems Trial of Prevention Strategies for Childhood Obesity: WHO STOPS Childhood Obesity" International Journal of Environmental Research and Public Health 13, no. 11: 1143. https://doi.org/10.3390/ijerph13111143






