The Current Situation of Hypertension among Rural Minimal Assurance Family Participants in Liaoning (China): A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection and Measurements
2.3. Definitions
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef]
- Ranasinghe, P.; Cooray, D.N.; Jayawardena, R.; Katulanda, P. The influence of family history of hypertension on disease prevalence and associated metabolic risk factors among Sri Lankan adults. BioMed Cent. Public Health 2015, 15, 576. [Google Scholar] [CrossRef] [PubMed]
- Qi, S.F.; Zhang, B.; Wang, H.J.; Yan, J.; Mi, Y.J.; Liu, D.W.; Tian, Q.B. Prevalence of hypertension subtypes in 2011 and the trends from 1991 to 2011 among Chinese adults. J. Epidemiol. Community Health 2016, 70, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Gu, H.; Teo, K.K.; Bo, J.; Wang, Y.; Yang, J.; Wang, X.; Zhang, H.; Sun, Y.; Jia, X.; et al. Hypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47,000 people from China. J. Hypertens. 2016, 34, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Xu, Z.; Xu, X.; Cai, Q.; Xu, Y. Prevalence, awareness, treatment, and control of hypertension among residents in Guangdong Province, China, 2004 to 2007. Circ. Card. Qual. Outcomes 2013, 6, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Dong, G.; Wang, D.; Liu, M.M.; Lin, Q.; Tian, S.; Xu, L.; Hou, H.; Ren, Y. Prevalence, awareness, treatment, control, and risk factors associated with hypertension in urban adults from 33 communities of China: The CHPSNE study. J. Hypertens. 2011, 29, 1303–1310. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Li, L.; Zhou, T.; Li, Z. Prevalence of hypertension in rural areas of china: A meta-analysis of published studies. PLoS ONE 2014, 9, e115462. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Zheng, L.; Wei, Y.; Li, J.; Zhang, X.; Zhang, X.; Liu, S.; Xu, C.; Li, J.; Zhao, F.; et al. The prevalence of prehypertension and hypertension among rural adults in Liaoning province of China. Clin. Card. 2007, 30, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Guo, X.; Zheng, L.; Yang, H.; Sun, Y. Grim status of hypertension in rural China: Results from Northeast China Rural Cardiovascular Health Study 2013. J. Am. Soc. Hypertens. 2015, 9, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Xia, J. The changes track and cluster analysis on the security of the rural minimum living guarantee standard: An empirical analysis based on 31 provincial regions. Chin. Public Adm. 2015, 11, 98–104. [Google Scholar]
- O’Brien, E.; Petrie, J.; Littler, W.; de Swiet, M.; Padfield, P.L.; Altman, D.G.; Bland, M.; Coats, A.; Atkins, N. An outline of the revised British Hypertension Society protocol for the evaluation of blood pressure measuring devices. J. Hypertens. 1993, 11, 677–679. [Google Scholar] [CrossRef] [PubMed]
- WHO Expert Committee on Hypertension Control; World Health Organization. Hypertension Control: Report of a WHO Expert Committee, 1st ed.; World Health Organization: Geneva, Switzerland, 1996; pp. 1–83. [Google Scholar]
- Egan, B.M.; Li, J.; Qanungo, S.; Wolfman, T.E. Blood pressure and cholesterol control in hypertensive hypercholesterolemic patients: National health and nutrition examination surveys 1988–2010. Circulation 2013, 128, 29–41. [Google Scholar] [CrossRef] [PubMed]
- Skevington, S.M.; Lotfy, M.; O’Connell, K.A. The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual. Life Res. 2004, 13, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Xia, P.; Li, N.; Hau, K.T.; Liu, C.; Lu, Y. Quality of life of Chinese urban community residents: A psychometric study of the mainland Chinese version of the WHOQOL-BREF. BioMed Cent. 2012, 12, 37. [Google Scholar] [CrossRef] [PubMed]
- Harper, A.; Power, M. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar]
- Zhang, W.; Doherty, M.; Bardin, T.; Pascual, E.; Barskova, V.; Conaghan, P.; Gerster, J.; Jacobs, J.; Leeb, B.; Liote, F. EULAR evidence based recommendations for gout. Part II: Management. Report of a task force of the EULAR standing committee for international clinical studies including therapeutics (ESCISIT). Ann. Rheum. Dis. 2006, 65, 1312–1324. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; International Diabetes Federation. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/IDF Consultation, 1st ed.; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Sarki, A.M.; Nduka, C.U.; Stranges, S.; Kandala, N.B.; Uthman, O.A. Prevalence of hypertension in low- and middle-income countries: A systematic review and meta-analysis. Medicine 2015, 94, e1959. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Bots, M.L.; Yang, F.; Hoes, A.W.; Vaartjes, I. Prevalence of hypertension in China: A systematic review and meta-regression analysis of trends and regional differences. J. Hypertens. 2014, 32, 1919–1927. [Google Scholar] [CrossRef] [PubMed]
- Chow, C.K.; Teo, K.K.; Rangarajan, S.; Islam, S.; Gupta, R.; Avezum, A.; Bahonar, A.; Chifamba, J.; Dagenais, G.; Diaz, R. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. J. Am. Med. Assoc. 2013, 310, 959–968. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhang, L.; Wang, F.; Liu, L.; Wang, H. Prevalence, awareness, treatment, and control of hypertension in China: Results from a national survey. Am. J. Hypertens. 2014, 27, 1355–1361. [Google Scholar] [CrossRef] [PubMed]
- Busingye, D.; Arabshahi, S.; Subasinghe, A.K.; Evans, R.G.; Riddell, M.A.; Thrift, A.G. Do the socioeconomic and hypertension gradients in rural populations of low- and middle-income countries differ by geographical region? A systematic review and meta-analysis. Int. J. Epidemiol. 2014, 43, 1563–1577. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Yue, X.; Wang, H.; Bao, C.; Xu, W.; Chen, L.; Qi, X. Relation of socioeconomic status to hypertension occurrence. Int. J. Card. 2014, 173, 544–545. [Google Scholar] [CrossRef] [PubMed]
- Fikadu, G.; Lemma, S. Socioeconomic status and hypertension among teachers and bankers in Addis Ababa, Ethiopia. Int. J. Hypertens. 2016, 2016, 4143962. [Google Scholar] [CrossRef] [PubMed]
- Cois, A.; Ehrlich, R. Analysing the socioeconomic determinants of hypertension in South Africa: A structural equation modelling approach. BioMed Cent. 2014, 14, 414. [Google Scholar] [CrossRef] [PubMed]
- Adedoyin, R.A.; Mbada, C.E.; Awofolu, O.O.; Oyebami, O.M. The influence of socio-economic status on casual blood pressures of the adult Nigerians. Eur. J. Card. Prev. Rehabil. 2005, 12, 271–273. [Google Scholar] [CrossRef]
- Reddy, K.S.; Naik, N.; Prabhakaran, D. Hypertension in the developing world: A consequence of progress. Curr. Card. Rep. 2006, 8, 399–404. [Google Scholar] [CrossRef]
- Zhang, Y.; Ou, F.; Gao, S.; Gao, Q.; Hu, L.; Liu, Y. Effect of low income on health-related quality of life: A cross-sectional study in northeast China. Asia Pac. J. Public Health 2015, 27. [Google Scholar] [CrossRef] [PubMed]
- Baumstarck, K.; Boyer, L.; Auquier, P. The role of stable housing as a determinant of poverty-related quality of life in vulnerable individuals. Int. J. Qual. Health Care 2015, 27, 356–360. [Google Scholar] [CrossRef] [PubMed]
- Cushman, W.C.; Ford, C.E.; Cutler, J.A.; Margolis, K.L.; Davis, B.R.; Grimm, R.H.; Black, H.R.; Hamilton, B.P.; Holland, J.; Nwachuku, C.; et al. Success and predictors of blood pressure control in diverse North American settings: The antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). J. Clin. Hypertens. 2002, 4, 393–404. [Google Scholar] [CrossRef]
- Perkovic, V.; Huxley, R.; Wu, Y.; Prabhakaran, D.; MacMahon, S. The burden of blood pressure-related disease: A neglected priority for global health. Hypertension 2007, 50, 991–997. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Gu, D.; Wu, X.; Reynolds, K.; Duan, X.; Yao, C.; Wang, J.; Chen, C.S.; Chen, J.; Wildman, R.P.; et al. Major causes of death among men and women in China. N. Engl. J. Med. 2005, 353, 1124–1134. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Ordinary Family | Minimal Assurance Family | p Value |
|---|---|---|---|
| Age, years | 53.3 ± 10.3 | 57.8 ± 11.4 | <0.001 |
| Gender | 0.008 | ||
| Male | 4659 (45.8) | 626 (49.8) | |
| Female | 5518 (54.2) | 632 (50.2) | |
| Married/cohabiting | 9281 (91.2) | 985 (78.3) | <0.001 |
| Annual income (CNY/year) | <0.001 | ||
| ≤5000 | 1047 (10.3) | 376 (29.9) | |
| 5000–20,000 | 5485 (53.9) | 746 (59.3) | |
| >20,000 | 3645 (35.8) | 136 (10.8) | |
| Educational status | <0.001 | ||
| Primary school or below | 4879 (47.9) | 821 (65.3) | |
| Middle school | 4280 (42.1) | 380 (30.2) | |
| High school or above | 1018 (10.0) | 57 (4.5) | |
| Occupational physical activity | <0.001 | ||
| Low | 3549 (34.9) | 649 (51.6) | |
| Moderate | 1970 (19.4) | 216 (17.2) | |
| Heavy | 4658 (45.8) | 393 (31.2) | |
| Current smoking | 3556 (34.9) | 478 (38.0) | 0.032 |
| Current drinking | 2330 (22.9) | 258 (20.5) | 0.056 |
| Body mass index, kg/m2 | 24.8 ± 3.6 | 24.5 ± 4.0 | 0.007 |
| waist circumference, cm | 82.5 ± 9.8 | 82.1 ± 10.3 | 0.241 |
| LDL-cholesterol, mmol/L | 2.9 ± 0.8 | 3.0 ± 0.8 | 0.002 |
| HDL-cholesterol, mmol/L | 1.4 ± 0.4 | 1.4 ± 0.4 | 0.006 |
| Triglycerides, mmol/L | 1.6 ± 1.5 | 1.7 ± 1.7 | 0.537 |
| Total cholesterol, mmol/L | 5.2 ± 1.1 | 5.3 ± 1.1 | 0.056 |
| Fasting glucose, mmol/L | 5.9 ± 1.6 | 6.0 ± 1.8 | 0.241 |
| Systolic blood pressure, mmHg | 141.0 ± 23.0 | 147.9 ± 25.5 | <0.001 |
| Diastolic blood pressure, mmHg | 81.9 ± 11.7 | 83.1 ± 12.4 | 0.001 |
| Serum uric acid, mmol/L | 291.8 ± 84.4 | 289.9 ± 84.5 | 0.451 |
| Family medical expenses (CNY/year) a | 4411.0 (2000.0) | 7990 (3000.0) | <0.001 |
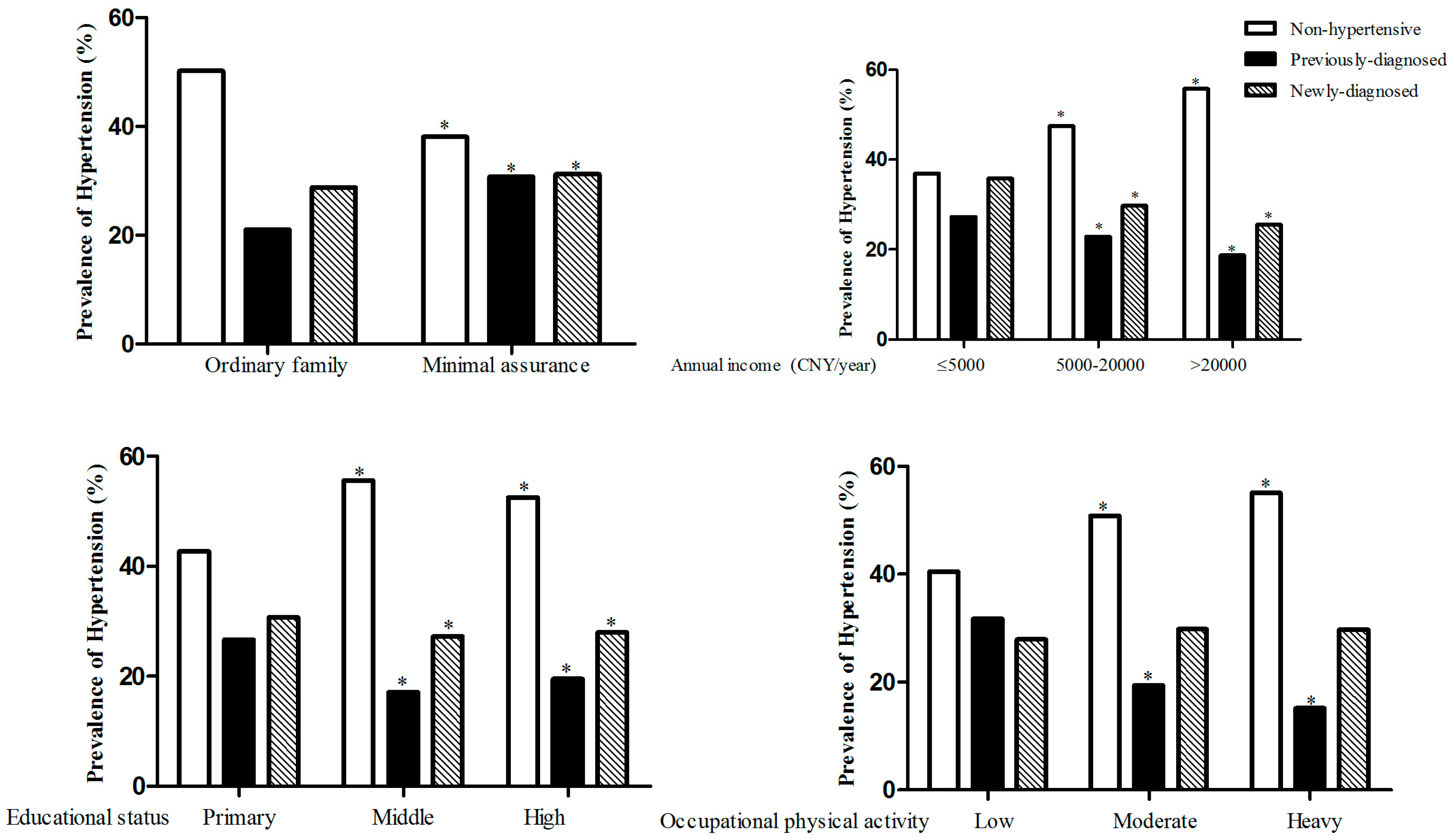
| Characteristic | Prevalence | Awareness | Treatment | Control |
|---|---|---|---|---|
| Ordinary Family | 5066 (49.8) | 2153 (42.5) | 1548 (30.6) | 310 (20.0) |
| Annual income (CNY/year) | ||||
| ≤5000 | 645 (61.6) | 271 (42.0) | 203 (31.5) | 46 (22.7) |
| 5000–20,000 | 2825 (51.5) | 1205 (42.7) | 860 (30.4) | 166 (19.3) |
| >20,000 | 1596 (43.8) | 677 (42.4) | 485 (30.4) | 98 (20.2) |
| p values | <0.001 | 0.954 | 0.863 | 0.557 |
| Educational status | ||||
| Primary school or below | 2726 (55.9) | 1260 (46.2) | 913 (33.5) | 176 (19.3) |
| Middle school | 1870 (43.7) | 700 (37.4) | 495 (26.5) | 107 (21.6) |
| High school or above | 470 (46.2) | 193 (41.1) | 140 (29.8) | 27 (19.3) |
| p values | <0.001 | <0.001 | <0.001 | 0.563 |
| Occupational physical activity | ||||
| Low | 2046 (57.7) | 1084 (53.0) | 836 (40.9) | 158 (18.9) |
| Moderate | 950 (48.2) | 376 (39.6) | 257 (27.1) | 53 (20.6) |
| Heavy | 2070 (44.4) | 693 (33.5) | 455 (22.0) | 99 (21.8) |
| p values | <0.001 | <0.001 | <0.001 | 0.456 |
| Minimal assurance family | 779 (61.9) | 388 (49.8) | 299 (38.4) | 41 (13.7) |
| Annual income (CNY/year) | ||||
| ≤5000 | 253 (67.3) | 119 (47.0) | 91 (36.0) | 16 (17.6) |
| 5000–20,000 | 452 (60.6) | 233 (51.5) | 180 (39.8) | 23 (12.8) |
| >20,000 | 74 (54.4) | 36 (48.6) | 28 (37.8) | 2 (7.1) |
| p values | 0.015 | 0.505 | 0.598 | 0.316 |
| Educational status | ||||
| Primary school or below | 539 (65.7) | 263 (48.8) | 206 (38.2) | 27 (13.1) |
| Middle school | 199 (52.4) | 106 (53.3) | 78 (39.2) | 13 (16.7) |
| High school or above | 41 (71.9) | 19 (46.3) | 15 (36.6) | 1 (6.7) |
| p values | <0.001 | 0.504 | 0.943 | 0.53 |
| Occupational physical activity | ||||
| Low | 455 (70.1) | 256 (56.3) | 212 (46.6) | 33 (15.6) |
| Moderate | 125 (57.9) | 53 (42.4) | 36 (28.8) | 4 (11.1) |
| Heavy | 199 (50.6) | 79 (39.7) | 51 (25.6) | 4 (7.8) |
| p values | <0.001 | <0.001 | <0.001 | 0.316 |
| Total Sample | Ordinary Family | Minimal Assurance Family | ||||
|---|---|---|---|---|---|---|
| Wald | OR (95 % CI) | Wald | OR (95 % CI) | Wald | OR (95 % CI) | |
| Model 1 | ||||||
| Minimal assurance family a | 65.13 | 1.64 (1.46–1.85) * | - ** | - | - | - |
| Model 2 | ||||||
| Minimal assurance family a | 10.04 | 1.27 (1.10–1.46) * | - | - | - | - |
| Annual income (CNY/year) b | ||||||
| ≤5000 | 5.18 | 1.19 (1.03–1.38) * | 3.32 | 1.17 (0.99–1.38) | 0.81 | 1.24 (0.78–1.98) |
| 5000–20,000 | 11.18 | 1.17 (1.07–1.29) * | 9.30 | 1.16 (1.06–1.28) * | 0.85 | 1.22 (0.80–1.87) |
| Educational status c | ||||||
| Primary school or below | 0.2 | 0.97 (0.83–1.13) | 0.10 | 0.97 (0.83–1.14) | 2.32 | 0.59 (0.30–1.16) |
| Middle school | 0.001 | 1.00 (0.86–1.16) | 0.18 | 1.03 (0.89–1.21) | 4.16 | 0.49 (0.24–0.97) * |
| Occupational physical activity d | ||||||
| Low | 3.4 | 1.10 (1.00–1.22) | 1.51 | 1.07 (0.96–1.19) | 4.17 | 1.38 (1.01–1.87) |
| Moderate | 0.13 | 1.02 (0.91–1.14) | 0.05 | 1.01 (0.90–1.14) | 0.31 | 1.12 (0.76–1.64) |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Y.; Yu, S.; Chen, S.; Guo, X.; Li, Y.; Li, Z.; Sun, Y. The Current Situation of Hypertension among Rural Minimal Assurance Family Participants in Liaoning (China): A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2016, 13, 1199. https://doi.org/10.3390/ijerph13121199
Chen Y, Yu S, Chen S, Guo X, Li Y, Li Z, Sun Y. The Current Situation of Hypertension among Rural Minimal Assurance Family Participants in Liaoning (China): A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2016; 13(12):1199. https://doi.org/10.3390/ijerph13121199
Chicago/Turabian StyleChen, Yintao, Shasha Yu, Shuang Chen, Xiaofan Guo, Yuan Li, Zhao Li, and Yingxian Sun. 2016. "The Current Situation of Hypertension among Rural Minimal Assurance Family Participants in Liaoning (China): A Cross-Sectional Study" International Journal of Environmental Research and Public Health 13, no. 12: 1199. https://doi.org/10.3390/ijerph13121199





