The Adverse Effects of Heavy Metals with and without Noise Exposure on the Human Peripheral and Central Auditory System: A Literature Review
Abstract
:1. Introduction
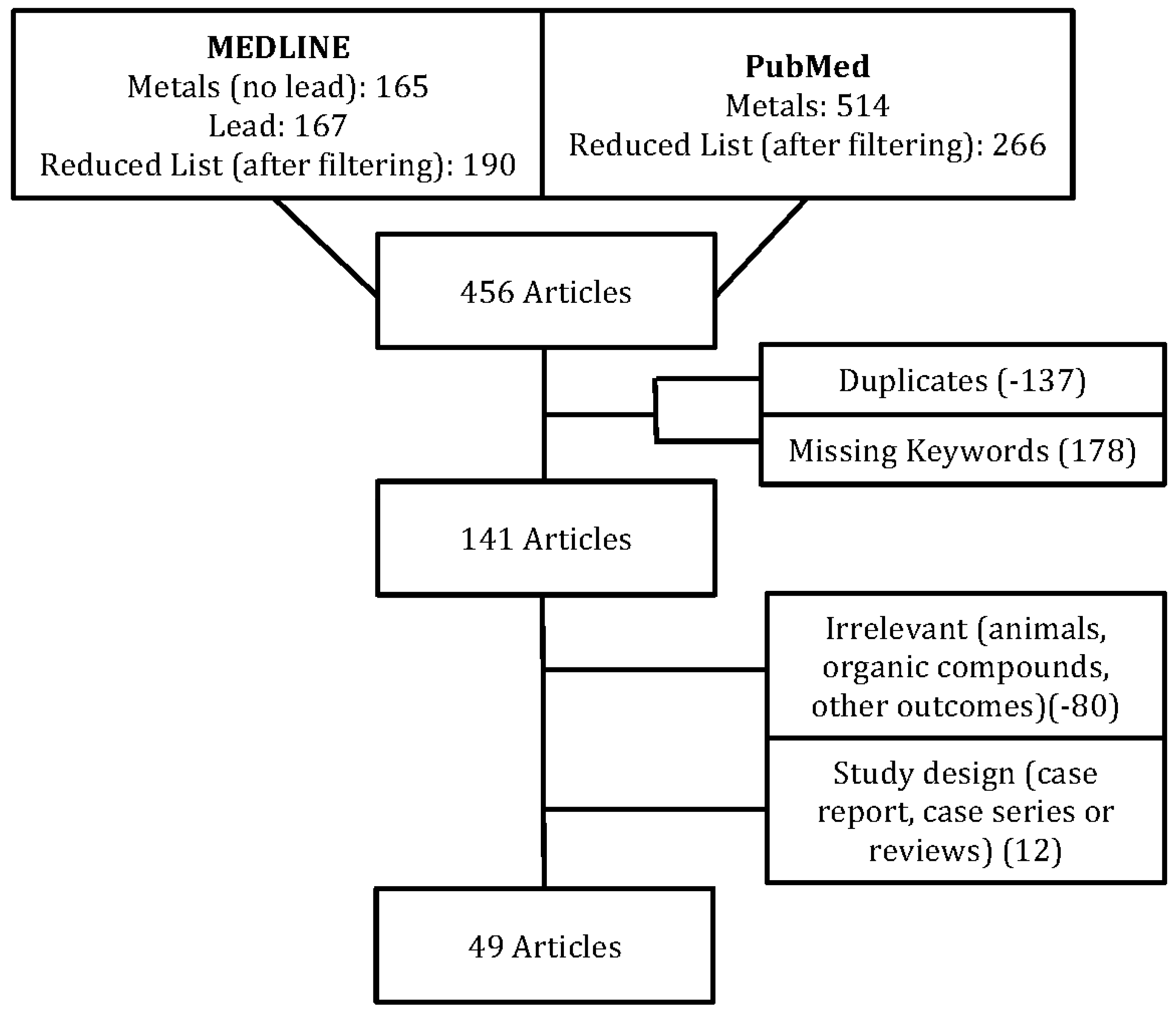
2. Methodology
3. Effects of Heavy Metals on the Human Auditory System
3.1. Arsenic
3.2. Cadmium
3.3. Lead
3.3.1. Hearing Thresholds and Occupational Lead Exposure
3.3.2. Hearing Thresholds and Non-Occupational Lead Exposure in Adulthood
3.3.3. ABR and Occupational Lead Exposure
3.3.4. ABR and Non-Occupational Lead Exposure in Adulthood
3.3.5. Lead-Induced Auditory Dysfunction during Childhood
3.4. Manganese
3.5. Mercury
3.6. Mixture of Heavy Metals
3.7. Heavy Metals and Noise
4. Discussion
5. Clinical Implications and Need for Further Research
6. Conclusions
Author Contributions
Conflicts of Interest
Abbreviations
| ABR | Auditory brainstem response |
| AEP | Auditory evoked potential |
| CI | Confidence interval |
| DPOAE | Distortion product otoacoustic emission |
| IPL | Inter-peak latency (for ABR) |
| OAE | Otoacoustic emission |
| OR | Odds ratio |
| PTA | Pure-tone average |
| TEOAE | Transient evoked otoacoustic emission |
References
- Mielke, H.W.; Laidlaw, M.A.; Gonzales, C. Lead (Pb) legacy from vehicle traffic in eight California urbanized areas: Continuing influence of lead dust on children’s health. Sci. Total Environ. 2010, 408, 3965–3975. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, L.H.; Counter, S.A.; Ortega, F. Environmental lead exposure and otoacoustic emissions in Andean children. J. Toxicol. Environ. Health Part A 2011, 74, 1280–1293. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, D.E.; Clickner, R.P.; Zhou, J.Y.; Viet, S.M.; Marker, D.A.; Rogers, J.W.; Zeldin, D.C.; Broene, P.; Friedman, W. The prevalence of lead-based paint hazards in U.S. housing. Environ. Health Perspect. 2002, 110, A599. [Google Scholar] [CrossRef] [PubMed]
- Dewailly, E.; Ayotte, P.; Bruneau, S.; Lebel, G.; Levallois, P.; Weber, J.P. Exposure of the Inuit population of Nunavik (Arctic Quebec) to lead and mercury. Arch. Environ. Health Int. J. 2001, 56, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Osman, K.; Pawlas, K.; Schutz, A.; Gazdzik, M.; Sokal, J.A.; Vahter, M. Lead exposure and hearing effects in children in Katowice, Poland. Environ. Res. 1999, 80, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tchounwou, P.B.; Yedjou, C.G.; Patlolla, A.K.; Sutton, D.J. Heavy Metal Toxicity and the Environment. In Molecular, Clinical and Environmental Toxicology; Springer: Basel, Switzerland, 2012; pp. 133–164. [Google Scholar]
- Hu, H. Human Health and Heavy Metals. In Life Support: The Environment and Human Health; MIT Press: Cambridge, MA, USA, 2002; p. 65. [Google Scholar]
- Agarwal, S.; Zaman, T.; Tuzcu, E.M.; Kapadia, S.R. Heavy metals and cardiovascular disease: Results from the National Health and Nutrition Examination Survey (NHANES) 1999–2006. Angiology 2011, 62, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Apostoli, P.; Catalani, S.; Zaghini, A.; Mariotti, A.; Poliani, P.L.; Vielmi, V.; Semeraro, F.; Duse, S.; Porzionato, A.; Macchi, V. High doses of cobalt induce optic and auditory neuropathy. Exp. Toxicol. Pathol. 2013, 65, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Lilienthal, H.; Winneke, G. Lead effects on the brain stem auditory evoked potential in monkeys during and after the treatment phase. Neurotoxicol. Teratol. 1996, 18, 17–32. [Google Scholar] [CrossRef]
- Wu, X.-W.; Ding, D.-L.; Sun, H.; Liu, H.; Jiang, H.-Y.; Salvi, R. Lead neurotoxicity in rat cochlear organotypic cultures. J. Otol. 2011, 6, 43–50. [Google Scholar]
- Lasky, R.E.; Maier, M.M.; Snodgrass, E.B.; Hecox, K.E.; Laughlin, N.K. The effects of lead on otoacoustic emissions and auditory evoked potentials in monkeys. Neurotoxicol. Teratol. 1995, 17, 633–644. [Google Scholar] [CrossRef]
- Ozcaglar, H.U.; Agirdir, B.; Dinc, O.; Turhan, M.; Kilinçarslan, S.; Oner, G. Effects of cadmium on the hearing system. Act. Otolaryngol. 2001, 121, 393–397. [Google Scholar]
- Stevens, M.H.; Jacobsen, T.; Crofts, A.K. Lead and the deafness of Ludwig van Beethoven. Laryngoscope 2013, 123, 2854–2858. [Google Scholar] [CrossRef] [PubMed]
- Agency for Toxic Substances and Disease Registry (ATSDR). Division of Toxicology and Human Health Sciences Atlanta, GA 30333, Support Document to the 2015 Priority List of Hazardous Substances that Will Be Candidates for Toxicological Profiles; Agency for Toxic Substances and Disease Registry (ATSDR): Atlanta, GA, USA, 2015.
- Simeonov, L.I.; Kochubovski, M.V.; Simeonova, B.G. Environmental Heavy Metal Pollution and Effects on Child Mental Development: Risk Assessment and Prevention Strategies; Springer: Dordrecht, The Netherlands, 2010. [Google Scholar]
- Carrizales, L.; Razo, I.; Téllez-Hernández, J.I.; Torres-Nerio, R.; Torres, A.; Batres, L.E.; Cubillas, A.-C.; Diaz-Barriga, F. Exposure to arsenic and lead of children living near a copper-smelter in San Luis Potosi, Mexico: Importance of soil contamination for exposure of children. Environ. Res. 2006, 101, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.X.; Hu, L.; Yand, P.Z.; Tanabe, K.; Miyatalre, M.; Chen, Y. Chronic arsenic poisoning in drinking water in Inner Mongolia and its associated health effects. J. Environ. Sci. Health Part A Toxic/Hazard. Subst. Environ. Eng. 2007, 42, 1853–1858. [Google Scholar] [CrossRef] [PubMed]
- Berg, M.; Tran, H.C.; Nguyen, T.C.; Pham, H.V.; Schertenleib, R.; Giger, W. Arsenic contamination of groundwater and drinking water in Vietnam: A human health threat. Environ. Sci. Technol. 2001, 35, 2621–2626. [Google Scholar] [CrossRef] [PubMed]
- Saunders, J.E.; Jastrzembski, B.G.; Buckey, J.C.; Enriquez, D.; MacKenzie, T.A.; Karagas, M.R. Hearing loss and heavy metal toxicity in a Nicaraguan mining community: Audiological results and case reports. Audiol. Neurotol. 2013, 18, 101–113. [Google Scholar] [CrossRef] [PubMed]
- Eisler, R. Arsenic Hazards to Humans, Plants, and Animals from Gold Mining. In Reviews of Environmental Contamination and Toxicology; Springer: Cham, Switzerland, 2004; pp. 133–165. [Google Scholar]
- Bencko, V.; Symon, K. Test of environmental exposure to arsenic and hearing changes in exposed children. Environ. Health Perspect. 1977, 19, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Milham, S., Jr. Studies of morbidity near a copper smelter. Environ. Health Perspect. 1977, 19, 131–132. [Google Scholar] [CrossRef] [PubMed]
- Supapong, S.; Sriratanabun, J. Brainstem auditory evoked potentials (BAEPs) study in chronic arsenic poisoning patients. J. Med. Assoc. Thail. 2005, 88, S226–S230. [Google Scholar]
- Shargorodsky, J.; Curhan, S.G.; Henderson, E.; Eavey, R.; Curhan, G.C. Heavy metals exposure and hearing loss in US adolescents. Arch. Otolaryngol. Head Neck Surg. 2011, 137, 1183–1189. [Google Scholar] [CrossRef] [PubMed]
- Järup, L.; Berglund, M.; Elinder, C.G.; Nordberg, G.; Vanter, M. Health effects of cadmium exposure—A review of the literature and a risk estimate. Scand. J. Work Environ. Health 1998, 24, 1–51. [Google Scholar] [PubMed]
- Dabeka, R.W.; McKenzie, A.D. Survey of lead, cadmium, fluoride, nickel, and cobalt in food composites and estimation of dietary intakes of these elements by Canadians in 1986–1988. J. AOAC Int. 1994, 78, 897–909. [Google Scholar]
- Elinder, C.G.; Kjellström, T.; Lind, B.; Linnman, L.; Piscator, M.; Sundstedt, K. Cadmium exposure from smoking cigarettes: Variations with time and country where purchased. Environ. Res. 1983, 32, 220–227. [Google Scholar] [CrossRef]
- Bustueva, K.A.; Revich, B.A.; Bezpalko, L.E. Cadmium in the environment of three Russian cities and in human hair and urine. Arch. Environ. Health Int. J. 1994, 49, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Thatcher, R.W.; McAlaster, R.; Lester, M.L. Evoked potentials related to hair cadmium and lead in children. Ann. N. Y. Acad. Sci. 1984, 425, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.-H.; Hu, H.; Mukherjee, B.; Miller, J.; Park, S.K. Environmental cadmium and lead exposures and hearing loss in U.S. adults: The National Health and Nutrition Examination Survey, 1999 to 2004. Environ. Health Perspect. 2012, 120, 1544–1550. [Google Scholar] [CrossRef] [PubMed]
- Needleman, H. Lead poisoning. Annu. Rev. Med. 2004, 55, 209–222. [Google Scholar] [CrossRef] [PubMed]
- Pervez, S.; Pandey, G. Toxic metals status in kidneys and gallstones of workers in a steel plant environment. Environ. Monit. Assess. 1994, 32, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Horng, C.-J. Simultaneous determination of urinary zinc, cadmium, lead and copper concentrations in steel production workers by differential-pulse anodic stripping voltammetry. Analyst 1996, 121, 1511–1514. [Google Scholar] [CrossRef] [PubMed]
- Hwang, Y.-H.; Chiang, H.-Y.; Yen-Jean, M.-C.; Wang, J.-D. The association between low levels of lead in blood and occupational noise-induced hearing loss in steel workers. Sci. Total Environ. 2009, 408, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Maizlish, N.A.; Parra, G.; Feo, O. Neurobehavioural evaluation of Venezuelan workers exposed to inorganic lead. Occup. Environ. Med. 1995, 52, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Murata, K.; Araki, S.; Yokoyama, K.; Nomiyama, K.; Nomiyama, H.; Tao, Y.X.; Liu, S.J. Autonomic and central nervous system effects of lead in female glass workers in China. Am. J. Ind. Med. 1995, 28, 233–244. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, K.; Araki, S.; Yamashita, K.; Murata, K.; Nomiyama, K.; Nomiyama, H.; Tao, Y.-X.; Liu, S.-J. Subclinical cerebellar anterior lobe, vestibulocerebellar and spinocerebellar afferent effects in young female lead workers in China: Computerized posturography with sway frequency analysis and brainstem auditory evoked potentials. Ind. Health 2002, 40, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.N.; Shen, C.Y.; Lai, J.S.; Goo, C.F.; Ko, K.N.; Chi, H.Y.; Chang, P.Y.; Liou, S.H. Effects of lead and noise exposures on hearing ability. Arch. Environ. Health 2000, 55, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Abdollahi, M.; Sadeghi Mojarad, A.; Jalali, N. Lead toxicity in employees of a paint factory. Med. J. Islam. Repub. Iran 1996, 10, 203–206. [Google Scholar]
- Chen, J.; Tan, M.; Li, Y.; Zhang, Y.; Lu, W.; Tong, Y.; Zhang, G.; Li, Y. A lead isotope record of Shanghai atmospheric lead emissions in total suspended particles during the period of phasing out of leaded gasoline. Atmos. Environ. 2005, 39, 1245–1253. [Google Scholar] [CrossRef]
- Sun, Y.; Zhuang, G.; Zhang, W.; Wang, Y.; Zhuang, Y. Characteristics and sources of lead pollution after phasing out leaded gasoline in Beijing. Atmos. Environ. 2006, 40, 2973–2985. [Google Scholar] [CrossRef]
- Geagea, M.L.; Stille, P.; Millet, M.; Perrone, T. REE characteristics and Pb, Sr and Nd isotopic compositions of steel plant emissions. Sci. Total Environ. 2007, 373, 404–419. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.; Wu, S.; Deng, W.; Yu, X.; Luo, Q.; Leung, A.; Wong, C.; Luksemburg, W.; Wong, A. Export of toxic chemicals—A review of the case of uncontrolled electronic-waste recycling. Environ. Pollut. 2007, 149, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.; Rampal, K.; Thuppil, V.; Chen, C.; Clark, R.; Roda, S. The lead content of currently available new residential paint in several Asian countries. Environ. Res. 2006, 102, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Romieu, I.; Palazuelos, E.; Avila, M.H.; Rios, C.; Muñoz, I.; Jimenez, C.; Cahero, G. Sources of lead exposure in Mexico City. Environ. Health Perspect. 1994, 102, 384. [Google Scholar] [CrossRef] [PubMed]
- Azcona-Cruz, M.I.; Rothenberg, S.J.; Schnaas, L.; Zamora-Muñoz, J.S.; Romero-Placeres, M. Lead-glazed ceramic ware and blood lead levels of children in the city of Oaxaca, Mexico. Arch. Environ. Health Int. J. 2000, 55, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Isidra, H.-S.M.; Rosalba, R.-M.; Carlos, G.-G.; Hulme, J.M.; Gustavo, O.-F. Factors associated with lead exposure in Oaxaca, Mexico. J. Expo. Sci. Environ. Epidemiol. 2003, 13, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Huo, X.; Li, Y.; Wu, K.; Liu, J.; Huang, J.; Zheng, G.; Xiao, Q.; Yang, H.; Wang, Y. Monitoring of lead, cadmium, chromium and nickel in placenta from an e-waste recycling town in China. Sci. Total Environ. 2010, 408, 3113–3117. [Google Scholar] [CrossRef] [PubMed]
- Al-Khashman, O.A.; Shawabkeh, R.A. Metals distribution in soils around the cement factory in southern Jordan. Environ. Pollut. 2006, 140, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Edwards, M.; Triantafyllidou, S.; Best, D. Elevated blood lead in young children due to lead-contaminated drinking water: Washington, DC, 2001–2004. Environ. Sci. Technol. 2009, 43, 1618–1623. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Pervez, S. Toxic metals status in human blood and breast milk samples in an integrated steel plant environment in Central India. Environ. Geochem. Health 2005, 27, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Swarup, D.; Patra, R.; Naresh, R.; Kumar, P.; Shekhar, P. Blood lead levels in lactating cows reared around polluted localities; transfer of lead into milk. Sci. Total Environ. 2005, 349, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Baloh, R.W.; Spivey, G.H.; Brown, C.P.; Morgan, D.; Campion, D.S.; Browdy, B.L.; Valentine, J.L.; Gonick, H.C.; Massey, F.J., Jr.; Culver, B.D. Subclinical effects of chronic increased lead absorption—A prospective study. II. Results of baseline neurologic testing. J. Occup. Med. 1979, 21, 490–496. [Google Scholar] [PubMed]
- Farahat, T.M.; Abdel-Rasoul, G.M.; El-Assy, A.R.; Kandil, S.H.; Kabil, M.K. Hearing thresholds of workers in a printing facility. Environ. Res. 1997, 73, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Forst, L.S.; Freels, S.; Persky, V. Occupational lead exposure and hearing loss. J. Occup. Environ. Med. 1997, 39, 658–660. [Google Scholar] [CrossRef] [PubMed]
- Counter, S.A.; Buchanan, L.H. Neuro-ototoxicity in Andean adults with chronic lead and noise exposure. J. Occup. Environ. Med. 2002, 44, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Park, S.K.; Elmarsafawy, S.; Mukherjee, B.; Spiro, A., 3rd; Vokonas, P.S.; Nie, H.; Weisskopf, M.G.; Schwartz, J.; Hu, H. Cumulative lead exposure and age-related hearing loss: The VA Normative Aging Study. Hear. Res. 2010, 269, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Discalzi, G.L.; Capellaro, F.; Bottalo, L.; Fabbro, D.; Mocellini, A. Auditory brainstem evoked potentials (BAEPs) in lead-exposed workers. Neurotoxicology 1992, 13, 207–209. [Google Scholar] [PubMed]
- Bleecker, M.L.; Ford, D.P.; Lindgren, K.N.; Scheetz, K.; Tiburzi, M.J. Association of chronic and current measures of lead exposure with different components of brainstem auditory evoked potentials. Neurotoxicology 2003, 24, 625–631. [Google Scholar] [CrossRef]
- Discalzi, G.; Fabbro, D.; Meliga, F.; Mocellini, A.; Capellaro, F. Effects of occupational exposure to mercury and lead on brainstem auditory evoked potentials. Int. J. Psychophysiol. 1993, 14, 21–25. [Google Scholar] [CrossRef]
- Lille, F.; Hazemann, P.; Garnier, R.; Dally, S. Effects of lead and mercury intoxications on evoked potentials. J. Toxicol. Clin. Toxicol. 1988, 26, 103–116. [Google Scholar] [CrossRef] [PubMed]
- Holdstein, Y.; Pratt, H.; Goldsher, M.; Rosen, G.; Shenhav, R.; Linn, S.; Mor, A.; Barkai, A. Auditory brainstem evoked potentials in asymptomatic lead-exposed subjects. J. Laryngol. Otol. 1986, 100, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Otto, D.; Robinson, G.; Baumann, S.; Schroeder, S.; Mushak, P.; Kleinbaum, D.; Boone, L. 5-year follow-up study of children with low-to-moderate lead absorption: Electrophysiological evaluation. Environ. Res. 1985, 38, 168–186. [Google Scholar] [CrossRef]
- Abdel Rasoul, G.M.; Al-Batanony, M.A.; Mahrous, O.A.; Abo-Salem, M.E.; Gabr, H.M. Environmental lead exposure among primary school children in Shebin El-Kom District, Menoufiya Governorate, Egypt. Int. J. Occup. Environ. Med. 2012, 3, 186–194. [Google Scholar] [PubMed]
- Schwartz, J.; Otto, D. Blood lead, hearing thresholds, and neurobehavioral development in children and youth. Arch. Environ. Health 1987, 42, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.; Otto, D. Lead and minor hearing impairment. Arch. Environ. Health 1991, 46, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Kamel, N.M.; Ramadan, A.M.; Kamel, M.I.; Mostafa, Y.A.; Abo, E.N.R.; Ali, A.M. Impact of lead exposure on health status and scholastic achievement of school pupils in Alexandria. J. Egypt. Public Health Assoc. 2003, 78, 1–28. [Google Scholar] [PubMed]
- Baumann, S.; Otto, D.; Robinson, G.; Schroeder, S.; Barton, C. The relationship of late positive ERPs, age, intelligence and lead absorption in socioeconomically disadvantaged children. Electroencephalogr. Clin. Neuropsychol. Suppl. 1987, 40, 617–623. [Google Scholar]
- Zou, C.; Zhao, Z.; Tang, L.; Chen, Z.; Du, L. The effect of lead on brainstem auditory evoked potentials in children. Chin. Med. J. 2003, 116, 565–568. [Google Scholar] [PubMed]
- Counter, S.A.E.A. Normal auditory brainstem and cochlear function in extreme pediatric plumbism. J. Neurol. Sci. 1997, 152, 85–92. [Google Scholar] [CrossRef]
- Counter, S.A.; Vahter, M.; Laurell, G.; Buchanan, L.H.; Ortega, F.; Skerfving, S. High lead exposure and auditory sensory-neural function in Andean children. Environ. Health Perspect. 1997, 105, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Counter, S.A. Brainstem neural conduction biomarkers in lead-exposed children of Andean lead-glaze workers. J. Occup. Environ. Med. 2002, 44, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Counter, S.A.; Buchanan, L.H.; Ortega, F. Association of hemoglobin levels and brainstem auditory evoked responses in lead-exposed children. Clin. Biochem. 2012, 45, 1197–1201. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, L.H.; Counter, S.A.; Ortega, F.; Laurell, G. Distortion product oto-acoustic emissions in Andean children and adults with chronic lead intoxication. Acta Oto-Laryngol. 1999, 119, 652–658. [Google Scholar] [CrossRef]
- Alvarenga Kde, F.; Morata, T.C.; Lopes, A.C.; Feniman, M.R.; Corteletti, L.C. Brainstem auditory evoked potentials in children with lead exposure. Braz. J. Otorhinolaryngol. 2015, 81, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Counter, S.A.; Buchanan, L.H.; Ortega, F.; van der Velde, J.; Borg, E. Assessment of auditory brainstem function in lead-exposed children using stapedius muscle reflexes. J. Neurol. Sci. 2011, 306, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Rothenberg, S.J.; Cansino, S.; Sepkoski, C.; Torres, L.M.; Medina, S.; Schnaas, L.; Poblano, A.; Karchmer, S. Prenatal and perinatal lead exposures alter acoustic cry parameters of neonate. Neurotoxicol. Teratol. 1995, 17, 151–160. [Google Scholar] [CrossRef]
- Rothenber, S.J.; Poblano, A.; Garza-Morales, S. Prenatal and perinatal low level lead exposure alters brainstem auditory evoked responses in infants. Neurotoxicology 1994, 15, 695–700. [Google Scholar]
- Rothenberg, S.J.; Poblano, A.; Schnaas, L. Brainstem auditory evoked response at five years and prenatal and postnatal blood lead. Neurotoxicol. Teratol. 2000, 22, 503–510. [Google Scholar] [CrossRef]
- Geng, F.; Mai, X.; Zhan, J.; Xu, L.; Shao, J.; Meeker, J.; Lozoff, B. Low-level prenatal lead exposure alters auditory recognition memory in 2-month-old infants: An event-related potentials (ERPs) study. Dev. Neuropsychol. 2014, 39, 516–528. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.; Todd, G.D.; Roney, N.; Crawford, J.; Coles, C.; McClure, P.R.; Garey, J.D.; Zaccaria, K.; Citra, M. Toxicological Profile for Manganese; Agency for Toxic Substances and Disease Registry (U.S.): Atlanta, GA, USA, 2012.
- Li, G.J.; Zhang, L.-L.; Lu, L.; Wu, P.; Zheng, W. Occupational exposure to welding fume among welders: Alterations of manganese, iron, zinc, copper, and lead in body fluids and the oxidative stress status. J. Occup. Environ. Med. 2004, 46, 241. [Google Scholar] [CrossRef] [PubMed]
- Chandra, S.V.; Shukla, G.S.; Srivastava, R.; Singh, H.; Gupta, V. An exploratory study of manganese exposure to welders. Clin. Toxicol. 2008, 18, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Wennberg, A.; Iregren, A.; Struwe, G.; Cizinsky, G.; Hagman, M.; Johansson, L. Manganese exposure in steel smelters a health hazard to the nervous system. Scand. J. Work Environ. Health 1991, 17, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Duan, N.; Fan, W.; Changbo, Z.; Chunlei, Z.; Hongbing, Y. Analysis of pollution materials generated from electrolytic manganese industries in China. Resour. Conserv. Recycl. 2010, 54, 506–511. [Google Scholar] [CrossRef]
- Loranger, S.; Zayed, J.; Forget, E. Manganese contamination in Montreal in relation with traffic density. Water Air Soil Pollut. 1994, 74, 385–396. [Google Scholar]
- Santos-Burgoa, C.; Rios, C.; Mercado, L.A.; Arechiga-Serrano, R.; Cano-Valle, F.; Eden-Wynter, R.A.; Texcalac-Sangrador, J.L.; Villa-Barragan, J.P.; Rodriguez-Agudelo, Y.; Montes, S. Exposure to manganese: Health effects on the general population, a pilot study in central Mexico. Environ. Res. 2001, 85, 90–104. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-D.; Zheng, W. Human exposure and health effects of inorganic and elemental mercury. J. Prev. Med. Public Health 2012, 45, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Lodenius, M.; Malm, O. Mercury in the Amazon. In Reviews of Environmental Contamination and Toxicology; Springer: Cham, Switzerland, 1998; pp. 25–52. [Google Scholar]
- Al-Batanony, M.A.; Abdel-Rasul, G.M.; Abu-Salem, M.A.; Al-Dalatony, M.M.; Allam, H.K. Occupational exposure to mercury among workers in a fluorescent lamp factory, Quisna Industrial Zone, Egypt. Int. J. Occup. Environ. Med. 2013, 4, 149–156. [Google Scholar] [PubMed]
- Björkman, L.; Lundekvam, B.F.; Lægreid, T.; Bertelsen, B.I.; Morild, I.; Lilleng, P.; Lind, B.; Palm, B.; Vahter, M. Mercury in human brain, blood, muscle and toenails in relation to exposure: An autopsy study. Environ. Health 2007, 6, 17931423. [Google Scholar] [CrossRef] [PubMed]
- Rothwell, J.A.; Boyd, P.J. Amalgam dental fillings and hearing loss. Int. J. Audiol. 2008, 47, 770–776. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.; Papadopoulos, P.; Watfa, N.; Takala, J.; Goelzer, B.; Hansen, C.; Sehrndt, G. Exposure Criteria, Occupational Exposure Levels. In Occupational Exposure to Noise: Evaluation, Prevention and Control; Goelzer, B., Hansen, C.H., Sehrndt, G.A., Eds.; World Health Organization: Dortmund/Berlin, Germany, 2001; pp. 79–102. [Google Scholar]
- Dutra, M.D.S.; Monteiro, M.C.; Câmara, V.D.M. Evaluation of central auditory processing in adolescents exposed to metallic mercury. Pro Fono 2010, 22, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Counter, S.A.; Buchanan, L.H.; Laurell, G.; Ortega, F. Blood mercury and auditory-sensory responses in children and adults in the Nambija gold mining area of Ecuador. Neurotoxicology 1998, 19, 185–196. [Google Scholar] [PubMed]
- Nriagu, J.O. Mercury pollution from the past mining of gold and silver in the Americas. Sci. Total Environ. 1994, 149, 167–181. [Google Scholar] [CrossRef]
- Araki, S.; Murata, K.; Yokoyama, K.; Uchida, E. Auditory event-related potential (P300) in relation to peripheral nerve conduction in workers exposed to lead, zinc, and copper: Effects of lead on cognitive function and central nervous system. Am. J. Ind. Med. 1992, 21, 539–547. [Google Scholar] [CrossRef] [PubMed]
- Chuang, H.-Y.; Kuo, C.-H.; Chiu, Y.-W.; Ho, C.-K.; Chen, C.-J.; Wu, T.-N. A case-control study on the relationship of hearing function and blood concentrations of lead, manganese, arsenic, and selenium. Sci. Total Environ. 2007, 387, 79–85. [Google Scholar] [CrossRef] [PubMed]
| Reference | Heavy Metal(s) | Study Design | Population | Procedures | Results |
|---|---|---|---|---|---|
| Guo et al. (2007) [18] | As | Cross-sectional with a control group | Adults | Hearing loss prevalence | Higher prevalence of hearing loss |
| Bencko and Symon (1977) [22] | As | Cross-sectional with a control group | Children | Pure-tone audiometry | Arsenic-exposed children presented with significantly higher (worse) pure-tone thresholds than non-exposed children for 125, 250 and 8000 Hz |
| Milham (1977) [23] | As | Descriptive | Children | Hearing screening | No higher prevalence of failed hearing screening |
| Supapong and Sriratanabun (2005) [24] | As | Cross-sectional with a control group | Adults | Auditory brainstem response (ABR) | No significant differences between groups found |
| Shargorodsky et al. (2011) [25] | As | Cross-sectional without a control group | Adults | Pure-tone audiometry | No association found |
| Shargorodsky et al. (2011) [25] | Cd | Cross-sectional without a control group | Adults | Pure-tone audiometry | Highest cadmium urinary levels quartile had higher odds of an increased low-frequency pure tone average (500, 1000 and 2000 Hz) |
| Thatcher et al. (1984) [30] | Cd | Cross-sectional without a control group | Children | Long latency AEP | Association between cadmium level in hair and amplitude of one of the components of the AEP |
| Choi et al. (2012) [31] | Cd | Cross-sectional without a control group | Adults | Pure-tone audiometry | Increase in PTA by 13.8% between highest and lowest quintile levels of cadmium, adjusted for noise and other major risk factors for hearing loss. |
| Wennberg et al. (1991) [85] | Mn | Cross-sectional with a control group | Adults | ABR and P300 | No significant differences found |
| Araki et al. (1992) [98] | Cu, Pb and Zn | Cross-sectional with a control group | Adults | AEP- N100 and P300 | P300 latency in the exposed group was significantly correlated with blood and urinary levels of lead |
| Chuang et al. (2007) [99] | Pb (Se, As, Mn) | Cross-sectional with a control group | Adults | Pure-tone audiometry | A dose–response association was found between blood lead levels and average hearing thresholds |
| Saunders et al. (2013) [20] | Al | Cross-sectional without a control group | Adults | Pure-tone audiometry and DPOAE | Correlation with decreased DPOAE amplitudes at 3000 Hz in subjects with low noise exposure levels. No correlation with pure-tone thresholds |
| As | Correlation with decreased DPOAE amplitudes at 2000 Hz in subjects with low noise exposure levels. No correlation with pure-tone thresholds | ||||
| Hg | No correlation found | ||||
| Mn | Correlation with decreased DPOAEs amplitude at 3000 Hz in subjects with low noise exposure levels. No association with pure-tone thresholds | ||||
| Pb | Correlation with DPOAE amplitude at 3000 Hz, 4000 Hz, and the mean DPOAE amplitude in subjects with low noise exposure levels. No correlation with pure-tone thresholds |
| Reference | Study Design | Procedures | Results |
|---|---|---|---|
| Hearing thresholds and occupational lead exposure | |||
| Choi et al. (2012) [31] | Cross-sectional without a control group | Pure-tone audiometry | The highest quintiles of lead blood levels were associated with increases in PTA compared to the lowest quintiles (after adjusting for sociodemographic and clinical risk factors and exposure to occupational and non-occupational noise). |
| Hwang et al. (2009) [35] | Cross-sectional without a control group | Pure-tone audiometry | Association between lead in blood and hearing thresholds at most of the audiometric frequencies. A logistic regression model, adjusted for age and noise exposure level, showed that blood levels above 7 µg/dL were significantly associated with hearing loss at 3000 and 8000 Hz. |
| Wu et al. (2000) [39] | Cross-sectional without a control group | Pure-tone audiometry | Association between long-term lead exposure and higher pure-tone threshold at 4000 Hz in the worse ear. No association for short-term lead exposure. No interaction with noise and exposure level was found. |
| Baloh et al. (1979) [54] | Cross-sectional with a control group | Hearing loss prevalence | No significant association found. |
| Farahat et al. (1997) [55] | Cross-sectional with a control group | Pure-tone audiometry | Lead-exposed workers presented with higher (worse) hearing thresholds for the 1000–8000 Hz range than non-exposed workers. Hearing threshold at 8000 Hz was the frequency most significantly affected by lead exposure. Hearing thresholds were found to correlate significantly to blood lead levels and years of lead exposure. |
| Forst et al. (1997) [56] | Cross-sectional without a control group | Pure-tone audiometry | Significant correlation between blood lead level and hearing threshold only at 4000 Hz. |
| Counter and Buchanan (2002) [57] | Cross-sectional without a control group | Pure-tone audiometry and ABR | Mean pure-tone thresholds from 2000 to 8000 Hz showed sensorineural hearing loss among exposed male subjects. Bilateral ABR on workers with elevated blood lead levels showed delayed wave latencies. |
| Hearing thresholds and non-occupational lead exposure in adulthood | |||
| Shargorodsky et al. (2011) [25] | Cross-sectional without a control group | Pure-tone audiometry | Significant association between the quartile with the highest level of lead exposure and a higher high-frequency PTA. |
| Park et al. (2010) [58] | Cross-sectional without a control group | Pure-tone audiometry | Trabecular bone lead levels were significantly associated with poorer hearing thresholds (at 2000, 3000, 4000, 6000 and 8000 Hz), PTA (mean of 500, 1000, 2000 and 4000 Hz) and odds of hearing loss. Significant positive longitudinal association between cortical bone lead levels and the rate of change in hearing thresholds at 1000, 2000 and 8000 Hz, as well as with PTA. |
| Auditory brainstem response and occupational lead exposure | |||
| Murata et al. (1995) [37] | Cross-sectional with a control group | ABR | No significant differences between groups found. |
| Yokoyama et al. (2002) [38] | Cross-sectional with a control group | ABR | No significant differences between groups found. |
| Discalzi et al. (1992) [59] | Cross-sectional without a control group | ABR | Lead exposed workers had significantly longer I–V IPL than non-exposed subjects. |
| Bleecker et al. (2003) [60] | Cross-sectional without a control group | ABR | Significant correlation between ABR wave I latency and blood lead levels. Significant association between working-lifetime weighted average blood lead and ABR wave III latency. Association between abnormal ABR waves I absolute latency and I–V IPL and lead exposure levels. |
| Discalzi et al . (1993) [61] | Cross-sectional with a control group | ABR | Lead-exposed subjects presented significantly longer I–V IPL than an age- and gender-matched control group. |
| Auditory brainstem response and non-occupational lead exposure in adulthood | |||
| Holdstein et al. (1986) [63] | Cross-sectional without a control group | ABR | Significant association between higher blood lead levels and longer I–III IPL. Significant correlations between blood lead levels and III–V IPL. |
| Reference | Study Design | Procedures | Results |
|---|---|---|---|
| Buchanan et al. (2011) [2] | Cross-sectional cohort without a control group | Pure-tone audiometry and DPOAE | No association found. |
| Osman et al. (1999) [5] | Cross-sectional without a control group | Pure-tone audiometry | Association between blood lead levels and hearing thresholds. Children with the highest blood lead levels presented with a significantly increased latency of ABR wave I (adjusted for age) when compared to children with lowest blood lead levels. |
| Otto et al. (1985) [64] | Cross-sectional without a control group | ABR | Association between blood lead levels and absolute wave latencies for waves III and V. |
| Abdel Rasoul et al. (2012) [65] | Cross-sectional without a control group | Pure-tone audiometry | Blood lead levels were significantly correlated with pure-tone thresholds. |
| Schwartz and Otto (1987) [66] | Cross-sectional study without a control group | Pure-tone audiometry | Blood lead levels were significantly associated with increased right and left hearing thresholds at 500, 1000, 2000 and 4000 Hz. |
| Schwartz and Otto (1991) [67] | Cross-sectional study without a control group | Pure-tone audiometry | Significant association between blood lead levels and pure-tone thresholds at 500 Hz, 1000 Hz, 2000 Hz, and 4000 Hz. |
| Kamel et al. (2003) [68] | Cross-sectional study without a control group | Pure-tone audiometry | Significant correlation between blood lead level and PTA. |
| Baumann et al. (1987) [69] | Cross-sectional study without a control group | Long latency AEP | Significant association between blood lead level and the positive peak of the long latency AEP. |
| Zou et al. (2003) [70] | Cross-sectional without a control group | ABR | Significant association between high blood lead levels and longer peak-latencies for I, III and V. Significant positive correlations between peak-latencies for waves I, III and V in both ears and blood lead levels. |
| Counter et al. (1997) [72] | Cross-sectional with a control group | Pure-tone audiometry and ABR | No association found. |
| Counter (2002) [73] | Pure-tone audiometry and ABR | No association found. | |
| Counter et al. (2012) [74] | Cross-sectional without a control group | ABR | No significant association between blood lead levels and ABR wave latencies. |
| Buchanan et al. (1999) [75] | Cross-sectional without a control group | Pure-tone audiometry and DPOAE | No association found |
| Alvarenga et al. (2015) [76] | Cross-sectional cohort without a control group | pure-tone audiometry, ABR and TEOAE | No association found. |
| Counter et al. (2011) [77] | Cross-sectional without a control group | Acoustic reflex thresholds, amplitude growth and decay | No significant correlations between blood lead levels and various acoustic reflex tests at any of the frequencies tested. |
| Rothenberg et al. (1995) [78] | Repeated measures without a control group | ABR | Association between higher maternal blood lead level at 20 weeks of pregnancy and increased ABR I–V and III–V IPL in 1-month-old babies. |
| Rothenberg et al. (2000) [80] | Cohort without a control group | ABR | Maternal blood lead levels at 20 weeks of pregnancy significantly associated with ABR I–V and III–V IPL in 5 year-old children. |
| Geng et al. (2014) [81] | Cross-sectional with a control group | ABR | Infants with cord-blood lead concentrations above 2 µg/dL did not present differences in amplitudes for event-related potential (P2, P750) and late slow wave when using their mother’s voice versus strangers’ voices as eliciting stimuli as opposed to infants with cord-blood lead concentrations below 2 µg/dL. |
| Reference | Study Design | Population | Procedures | Results |
|---|---|---|---|---|
| Shargorodsky et al. (2011) [25] | Cross-sectional without a control group | Adults | Pure-tone audiometry | No association found. |
| Discalzi et al. (1993) [61] | Cross-sectional with a control group | Adults | ABR | Workers exposed to mercury had significantly increased I–V IPL compared to an age- and gender-matched non-exposed control group. |
| Al-Batanony et al. (2013) [91] | Cross-sectional with a control group | Adults | Pure-tone audiometry | Significant difference in the prevalence of hearing loss between workers exposed to mercury and the non-exposed control group. |
| Rothwell and Boyd (2008) [93] | Cross-sectional without a control group | Adults | Pure-tone audiometry | The number of dental amalgam fillings by surface area had a significant association with hearing thresholds at 8, 11.2, 12.5, 14, and 16 kHz. |
| Dutra et al. (2010) [95] | Cross-sectional with a control group | Adolescents | Central Auditory processing | Significant difference between groups for the results of sequential memory of nonverbal stimuli. Significant difference for temporal frequency, duration pattern, and staggered spondaic word tests. No significant difference between groups for the sequential memory of verbal stimuli and sound localization. No significant difference for speech test with competitive white noise. |
| Counter et al. (1998) [96] | Cross-sectional without a control group | Children and adults | Pure-tone audiometry and ABR | Significant correlation between the hearing threshold at 3 kHz in the right ear and blood lead level in children. No effect on ABR results found. |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castellanos, M.-J.; Fuente, A. The Adverse Effects of Heavy Metals with and without Noise Exposure on the Human Peripheral and Central Auditory System: A Literature Review. Int. J. Environ. Res. Public Health 2016, 13, 1223. https://doi.org/10.3390/ijerph13121223
Castellanos M-J, Fuente A. The Adverse Effects of Heavy Metals with and without Noise Exposure on the Human Peripheral and Central Auditory System: A Literature Review. International Journal of Environmental Research and Public Health. 2016; 13(12):1223. https://doi.org/10.3390/ijerph13121223
Chicago/Turabian StyleCastellanos, Marie-Josée, and Adrian Fuente. 2016. "The Adverse Effects of Heavy Metals with and without Noise Exposure on the Human Peripheral and Central Auditory System: A Literature Review" International Journal of Environmental Research and Public Health 13, no. 12: 1223. https://doi.org/10.3390/ijerph13121223





