Facilitators and Barriers of Smokers’ Compliance with Smoking Bans in Public Places: A Systematic Review of Quantitative and Qualitative Literature
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Data Synthesis
2.5. Quality Assessment
3. Results
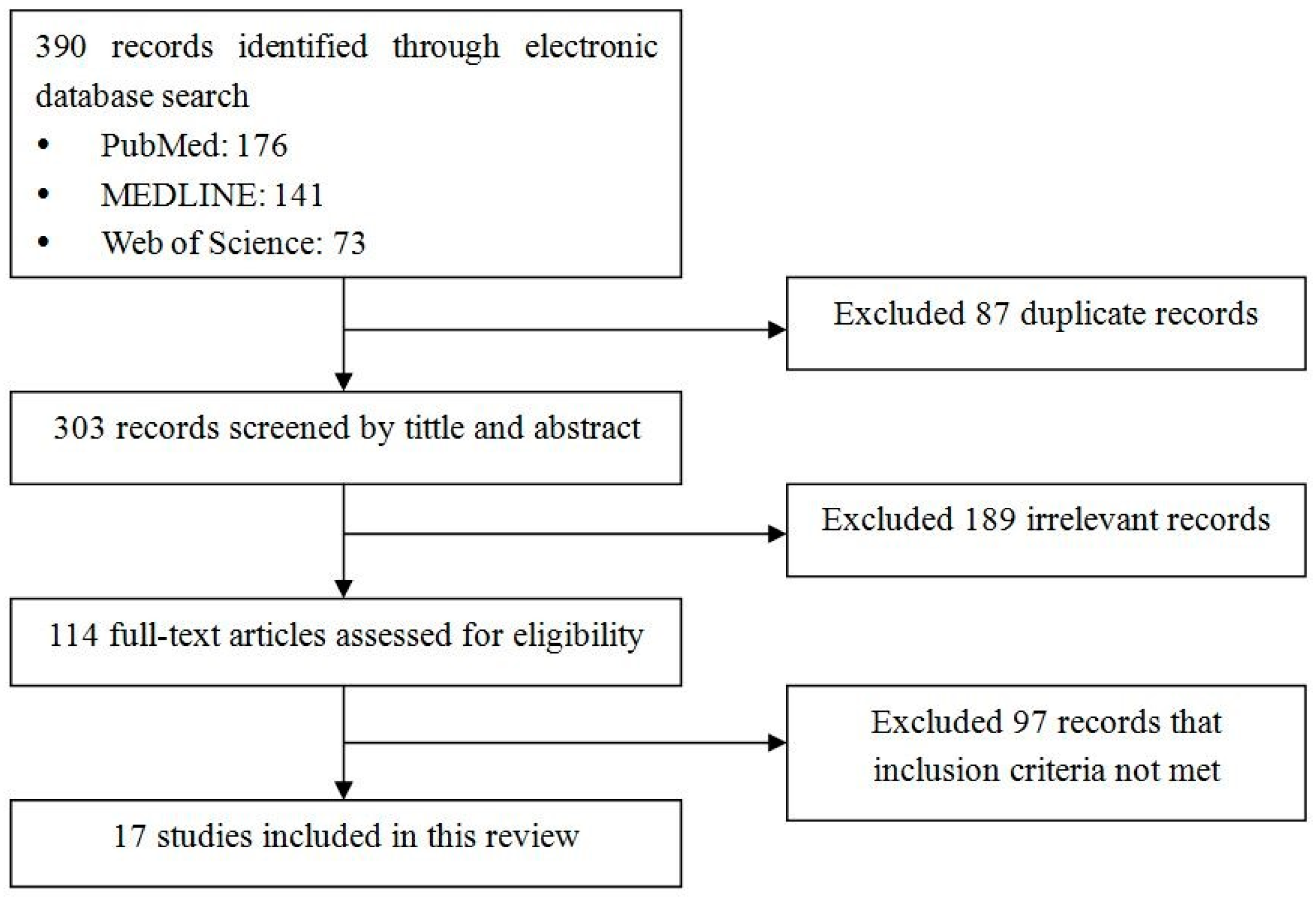
3.1. Search Results
3.2. Characteristics of the Study
3.3. Risk of Bias
3.4. Barriers and Facilitators
3.4.1. Individual Level
3.4.2. Interpersonal Level
3.4.3. Organizational Level
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Wang, Y.; Yang, M.; Tian, L.; Huang, Z.; Chen, F.; Hu, J.; Wang, F.; Chen, G.; Xiao, S. Relationship between caregivers’ smoking at home and urinary levels of cotinine in children. Int. J. Environ. Res. Public Health 2014, 11, 12499–12513. [Google Scholar] [CrossRef] [PubMed]
- Öberg, M.; Jaakkola, M.S.; Woodward, A.; Peruga, A.; Prüss-Ustün, A. Worldwide burden of disease from exposure to second-hand smoke: A retrospective analysis of data from 192 countries. Lancet 2011, 377, 139–146. [Google Scholar] [CrossRef]
- Atlanta, G. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Available online: https://stacks.cdc.gov/view/cdc/13252/ (accessed on 20 June 2015).
- Geneva. WHO Report on the Global Tobacco Epidemic, 2008—The Mpower Package. Available online: http://www.who.int/tobacco/mpower/2008/en/ (accessed on 20 June 2015).
- Nagelhout, G.E.; Mons, U.; Allwright, S.; Guignard, R.; Beck, F.; Fong, G.T.; de Vries, H.; Willemsen, M.C. Prevalence and predictors of smoking in “smoke-free” bars. Findings from the international tobacco control (ITC) Europe surveys. Soc. Sci. Med. 2011, 72, 1643–1651. [Google Scholar] [CrossRef] [PubMed]
- Eadie, D.; Heim, D.; Macaskill, S.; Ross, A.; Hastings, G.; Davies, J. A qualitative analysis of compliance with smoke-free legislation in community bars in Scotland: Implications for public health. Addiction 2008, 103, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Verdonk-Kleinjan, W.M.; Rijswijk, P.C.; de Vries, H.; Knibbe, R.A. Compliance with the workplace-smoking ban in the Netherlands. Health Policy 2013, 109, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Frazer, K.; McHugh, J.; Callinan, J.E.; Kelleher, C. Impact of institutional smoking bans on reducing harms and secondhand smoke exposure. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef]
- Li, X.; Li, Q.; Dong, L.; Sun, B.; Chen, J.; Jiang, Y.; Yang, Y.; Zhou, B.; Fong, G.T. Risk factors associated with smoking behaviour in recreational venues: Findings from the international tobacco control (ITC) China survey. Tob. Control 2010, 19, i30–i39. [Google Scholar] [CrossRef] [PubMed]
- Rivero, L.R.; Persson, J.L.; Romine, D.C.; Taylor, J.T.; Toole, T.C.; Trollman, C.J.; Au, W.W. Towards the world-wide ban of indoor cigarette smoking in public places. Int. J. Hyg. Environ. Health 2006, 209, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Tanni, S.E.; Iritsu, N.I.; Tani, M.; de Camargo, P.A.B.; Sampaio, M.G.E.; Godoy, I.; Godoy, I. Evaluation of hospitalized patients in terms of their knowledge related to smoking. J. Bras. Pneumol. 2010, 36, 218–223. [Google Scholar] [PubMed]
- Frazer, K.; Callinan, J.E.; McHugh, J.; van Baarsel, S.; Clarke, A.; Doherty, K.; Kelleher, C. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst. Rev. 2016, 2, CD005992. [Google Scholar] [PubMed]
- Chapman, S.; Freeman, B. Markers of the denormalisation of smoking and the tobacco industry. Tob. Control 2008, 17, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Xiao, S.; Kohrman, M. Anthropology in China’s health promotion and tobacco. Lancet 2008, 372, 1617–1618. [Google Scholar] [CrossRef]
- Rzeznicki, A.; Stelmach, I.; Kowalska, A.; Krakowiak, J.; Zebrowski, M.; Stelmach, W. Complying with the smoking ban by students before and after introducing legislative intervention. Int. J. Occup. Med. Environ. Health 2015, 28, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Lazuras, L.; Eiser, J.R.; Rodafinos, A. Predicting smokers’ non-compliance with smoking restrictions in public places. Tob. Control 2009, 18, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Sabido, M.; Sunyer, J.; Masuet, C.; Masip, J. Hospitalized smokers: Compliance with a nonsmoking policy and its predictors. Prev. Med. 2006, 43, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Rigotti, N.A.; Arnsten, J.H.; McKool, K.M.; Wood-Reid, K.M.; Pasternak, R.C.; Singer, D.E. Smoking by patients in a smoke-free hospital: Prevalence, predictors, and implications. Prev. Med. 2000, 31, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Goel, S.; Ravindra, K.; Singh, R.J.; Sharma, D. Effective smoke-free policies in achieving a high level of compliance with smoke-free law: Experiences from a district of north India. Tob. Control 2014, 23, 291–294. [Google Scholar] [CrossRef] [PubMed]
- Glanz, K.; Rimer, B.K.; Viswanath, K. Health Behavior and Health Education: Theory, Research, and Practice; John Wiley & Sons: Hoboken, NJ, USA, 2008; pp. 465–482. [Google Scholar]
- Sallis, J.F.; Owen, N.; Fisher, E.B. Twenty: Ecological Models of Health Behavior; Jossey-Bass: San Francisco, CA, USA, 2008. [Google Scholar]
- Kmet, L.M.; Lee, R.C. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields; Institute of Health Economics: Edmonton, AB, Canada, 2004. [Google Scholar]
- Emmons, K.M.; Cargill, B.R.; Hecht, J.; Goldstein, M.; Milman, R.; Abrams, D.B. Characteristics of patients adhering to a a hospital’s no-smoking policy. Prev. Med. 1998, 27, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Moore, R.S.; Lee, J.P.; Martin, S.E.; Todd, M.; Chu, B.C. Correlates of persistent smoking in bars subject to smokefree workplace policy. Int. J. Environ. Res. Public Health 2009, 6, 1341–1357. [Google Scholar] [CrossRef] [PubMed]
- Parks, T.; Wilson, C.V.; Turner, K.; Chin, J.W. Failure of hospital employees to comply with smoke-free policy is associated with nicotine dependence and motives for smoking: A descriptive cross-sectional study at a teaching hospital in the United Kingdom. BMC Public Health 2009, 9, 238. [Google Scholar] [CrossRef] [PubMed]
- Lacchetti, C.; Cohen, J.; Ashley, M.J.; Ferrence, R.; Bull, S.; de Groh, M.; Pederson, L. Is nicotine dependence related to smokers’ support for restrictions on smoking? Nicotine Tob. Res. 2001, 3, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Borland, R.; Yong, H.H.; Siahpush, M.; Hyland, A.; Campbell, S.; Hastings, G.; Cummings, K.M.; Fong, G.T. Support for and reported compliance with smoke-free restaurants and bars by smokers in four countries: Findings from the international tobacco control (ITC) four country survey. Tob. Control 2006, 15, iii34–iii41. [Google Scholar] [CrossRef] [PubMed]
- Moore, R.S.; Lee, J.P.; Antin, T.M.J.; Martin, S.E. Tobacco free workplace policies and low socioeconomic status female bartenders in San Francisco. J. Epidemiol. Community Health 2006, 60, ii51–ii56. [Google Scholar] [CrossRef]
- Irvin, V.L.; Hofstetter, C.R.; Nichols, J.F.; Chambers, C.D.; Usita, P.M.; Norman, G.J.; Kang, S.; Hovell, M.F. Compliance with smoke-free policies in Korean bars and restaurants: A descriptive analysis in California. Asian Pac. J. Cancer Prev. 2015, 16, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Shopik, N.A.; Schultz, A.S.; Nykiforuk, C.I.; Finegan, B.A.; Kvern, M.A. Impact of smoke-free hospital grounds policies: Patient experiences and perceptions. Health Policy 2012, 108, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Galan, I.; Diez-Ganan, L.; Mata, N.; Gandarillas, A.; Cantero, J.L.; Durban, M. Individual and contextual factors associated to smoking on school premises. Nicotine Tob. Res. 2012, 14, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Jancey, J.; Bowser, N.; Burns, S.; Crawford, G.; Portsmouth, L.; Smith, J. No smoking here: Examining reasons for noncompliance with a smoke-free policy in a large university. Nicotine Tob. Res. 2014, 16, 976–983. [Google Scholar] [CrossRef] [PubMed]
- Russette, H.C.; Harris, K.J.; Schuldberg, D.; Green, L. Policy compliance of smokers on a tobacco-free university campus. J. Am. Coll. Health 2014, 62, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Lazuras, L.; Zlatev, M.; Rodafinos, A.; Eiser, J.R. Smokers’ compliance with smoke-free policies, and non-smokers’ assertiveness for smoke-free air in the workplace: A study from the Balkans. Int. J. Public Health 2012, 57, 769–775. [Google Scholar] [CrossRef] [PubMed]
- Hovell, M.F.; Hughes, S.C. The behavioral ecology of secondhand smoke exposure: A pathway to complete tobacco control. Nicotine Tob. Res. 2009, 11, 1254–1264. [Google Scholar] [CrossRef] [PubMed]
- Baker, F.; Ainsworth, S.R.; Dye, J.T.; Crammer, C.; Thun, M.J.; Hoffmann, D.; Repace, J.L.; Henningfield, J.E.; Slade, J.; Pinney, J.; et al. Health risks associated with cigar smoking. JAMA 2000, 284, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Cokkinides, V.; Bandi, P.; Ward, E.; Jemal, A.; Thun, M. Progress and opportunities in tobacco control. CA Cancer J. Clin. 2006, 56, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.J.; Wang, J.F.; Mei, C.Z.; Xu, X.F.; Yang, G.H. Passive smoking in China: Contributing factors and areas for future interventions. Biomed. Environ. Sci. 2007, 20, 420–425. [Google Scholar] [PubMed]
- Hu, M.; Rich, Z.C.; Luo, D.; Xiao, S. Cigarette sharing and gifting in rural China: A focus group study. Nicotine Tob. Res. 2012, 14, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Ceraso, M.; McElroy, J.A.; Kuang, X.; Vila, P.M.; Du, X.; Lu, L.; Ren, H.; Qian, N.; Jorenby, D.E.; Fiore, M.C. Smoking, barriers to quitting, and smoking-related knowledge, attitudes, and patient practices among male physicians in China. Prev. Chronic Dis. 2009, 6, A06. [Google Scholar] [PubMed]
| First Author and Year | Risk of Bias | Setting/Country | Study Design | Sampling Methods | Sample Characteristics (Sample Size, Gender, Age) | Measurement/Definition of Compliance or Non-Compliance |
|---|---|---|---|---|---|---|
| Quantitative study | ||||||
| Rigotti, 2000 [18] | 0.86 | Hospital/U.S. | Cohort | Random | 650 inpatient smokers; 55% male; age: 49.2 ± 16.2 years | Patients who did not smoke while hospitalized or smoked outdoors only were classified as compliant; those who reported smoking indoors were noncompliant. |
| Sabidó, 2006 [17] | 0.91 | Hospital/Spain | Cross-sectional | Convenient | 229 inpatient smokers; 77% male; age: 50 ± 16.9 years | Compliant: those who did not smoke indoors or who only smoked outdoors; noncompliant: those who smoked indoors. |
| Parks, 2009 [25] | 0.77 | Hospital/UK | Cross-sectional | Convenient | 101 smoking staff; 22.8% male | Those who are compliant with smoke-free policy and only ever smoke off the site; those who are non-compliant and continue to smoke on site. |
| Lazuras, 2009 [16] | 0.73 | University/Greek | Cross-sectional | Convenient | 182 undergraduate smokers | Whether they had ever smoked in a smoke-free sector in public settings. |
| Lazuras, 2012 [34] | 0.73 | Companies/Greece and Bulgaria | Cross-sectional | Random | 170 daily or weekly smokers | Compliance with smoking restrictions in smoker-free sectors at work |
| Galán, 2012 [31] | 0.91 | Schools/Spain | Cross-sectional | Cluster | 1116 student smokers; 42.0% male | Having smoked sometime in the last thirty days on school premises in open or closed spaces. |
| Emmons, 1998 [23] | 0.77 | Hospitals/U.S. | Cross-sectional | Convenient | 358 hospitalized smokers; 45% male; mean age: 46 years | Adherence was defined as self-reporting of abstaining from cigarettes during the hospital stay. |
| Lacchetti, 2001 [26] | 0.86 | restaurants,workplaces, bingo halls, and hockey arenas/Canada | Cross-sectional | Random | 423 adult smokers | Compliance with more restrictions. |
| Li, 2010 [9] | 0.86 | Recreational venues/China | Cross-sectional | Stratified multistage cluster sampling | 2403 smokers who reported patronizing recreational venues; 84.0% males; age: 47.36 ± 8.53 | Smoking vs not smoking in recreational settings. |
| Nagelhout, 2011 [5] | 0.91 | Bars/Ireland, France, Netherlands, Germany | Cohort | Probability sampling | 4634 smokers; | Smoking in smoke-free bars. |
| Irvin, 2015 [29] | 0.91 | Korean bars and restaurants/U.S. | Cohort | Probability sampling | 224 current smokers of Korean descent who visited a Korean bar or restaurant bars and restaurants; 84.4% male; | Smoked inside Korean bars or restaurants. |
| Borland, 2006 [27] | 0.95 | recreational venues/U.S., Canada, UK, and Australia | Cross-sectional | Stratified random sampling | 9046 adult smokers; female (52.7%–56.6%) | Smoking inside recreational venues. |
| Qualitative study | ||||||
| Shopik, 2012 [30] | 0.85 | Hospital/Canada | Semi-structured interview | Convenient | 82 current smokers | Smoking in the hospital during hospitalization. |
| Jancey, 2014 [32] | 0.80 | University/Australian | An environmental audit; direct observation; intercept interview. | Convenient | 37 smokers (27% staff and 73% students); 83.8% male; 59.4% aged between 18 and 29 years | Smoking behavior on campus. |
| Mixed-method study | ||||||
| Moore, 2006 [28] | 0.72 | Bars/U.S. | Structure observations, semi-structure interviewers | Study 1: random Study 2: opportunistic sampling | Study 1: 479 observations study 2: 35 bar staff and patrons | Non-compliance: patron smoking. |
| Moore, 2009 [24] | 0.78 | Bars/U.S. | High-structure naturalistic observations, semi-structured interviews | Random | 121 stand-alone bars | Indoor smoking by bar patrons and staff. |
| Russette, 2014 [33] | 0.72 | School/U.S. | Semi-structure interview with 22-item survey and two open-ended questions | Convenient | 60 student and non-student smokers; 52% male; mean age: 28 years | Smoking on campus property or off campus property. |
| Level | Facilitators | Studies | Barriers | Studies |
|---|---|---|---|---|
| Individual level | Demographic factors | |||
| Male | 1 [17] | Low education level | 1 [31] | |
| Being older | 2 [18,23] | Being older | 1 [34] | |
| Smoking behaviors | ||||
| Lighter smokers | 1 [23] | Heavier smokers | 6 [9,16,18,25,29,31] | |
| Heavier nicotine dependence | 4 [17,18,26,30] | |||
| Nicotine withdrawal symptoms | 2[17,18] | |||
| Quiting smoking | ||||
| Having confidence toquit smoking | 1 [23] | No confidence to quit smoking | 1 [17] | |
| No quit smoking attempts | 1 [18] | |||
| Earlier stage of quit smoking | 1 [17] | |||
| Without substance abuse | 1 [23] | Illicit drug consumption | 1 [31] | |
| Higher level of knowledge about smoking and passive smoking | 3 [5,9,34] | Less awareness of harms of smoking | 1 [16] | |
| Negative attitudes towards smoking | 1 [5] | Supportive attitudes towards smoking | 3 [9,32,34] | |
| Supportive attitudes towards the bans | 3 [5,27,33] | Negative attitude towards smoking | 3 [9,32,33] | |
| Unawareness of policy boundaries | 2 [32,33] | |||
| History of chronic dieases (e.g., dyspnea, heartdisease) | 1 [18] | Limited physical mobility | 1 [30] | |
| Interpersonal level | No parental permission | 1 [31] | Smoking behaviors of people around in the same setting | 3 [24,28,29] |
| Smoking status of the peers | 2 [9,16] | |||
| Peers’dissuasion | 1 [33] | Close relatives and friends’ approval | 1 [16] | |
| Organizational level | Efficient implementation | 3 [27,30,33] | Lack of surveillance | 3 [24,28,30] |
| Convenience of the designative smoking area | 2 [30,33] | Inconvenience of the designative smoking area | 3 [30,32,33] | |
| Private schools (e.g., religious schools) | 1 [31] | Only female bartenders were on duty | 1 [24] | |
| Bars serving predominantly Asian or Irish patrons | 2 [24,28] |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, L.; Niu, L.; Jiang, H.; Jiang, C.; Xiao, S. Facilitators and Barriers of Smokers’ Compliance with Smoking Bans in Public Places: A Systematic Review of Quantitative and Qualitative Literature. Int. J. Environ. Res. Public Health 2016, 13, 1228. https://doi.org/10.3390/ijerph13121228
Zhou L, Niu L, Jiang H, Jiang C, Xiao S. Facilitators and Barriers of Smokers’ Compliance with Smoking Bans in Public Places: A Systematic Review of Quantitative and Qualitative Literature. International Journal of Environmental Research and Public Health. 2016; 13(12):1228. https://doi.org/10.3390/ijerph13121228
Chicago/Turabian StyleZhou, Li, Lu Niu, Hui Jiang, Caixiao Jiang, and Shuiyuan Xiao. 2016. "Facilitators and Barriers of Smokers’ Compliance with Smoking Bans in Public Places: A Systematic Review of Quantitative and Qualitative Literature" International Journal of Environmental Research and Public Health 13, no. 12: 1228. https://doi.org/10.3390/ijerph13121228






