What Contributes to the Regularity of Patients with Hypertension or Diabetes Seeking Health Services? A Pilot Follow-Up, Observational Study in Two Sites in Hubei Province, China
Abstract
:1. Introduction
2. Materials and Methods
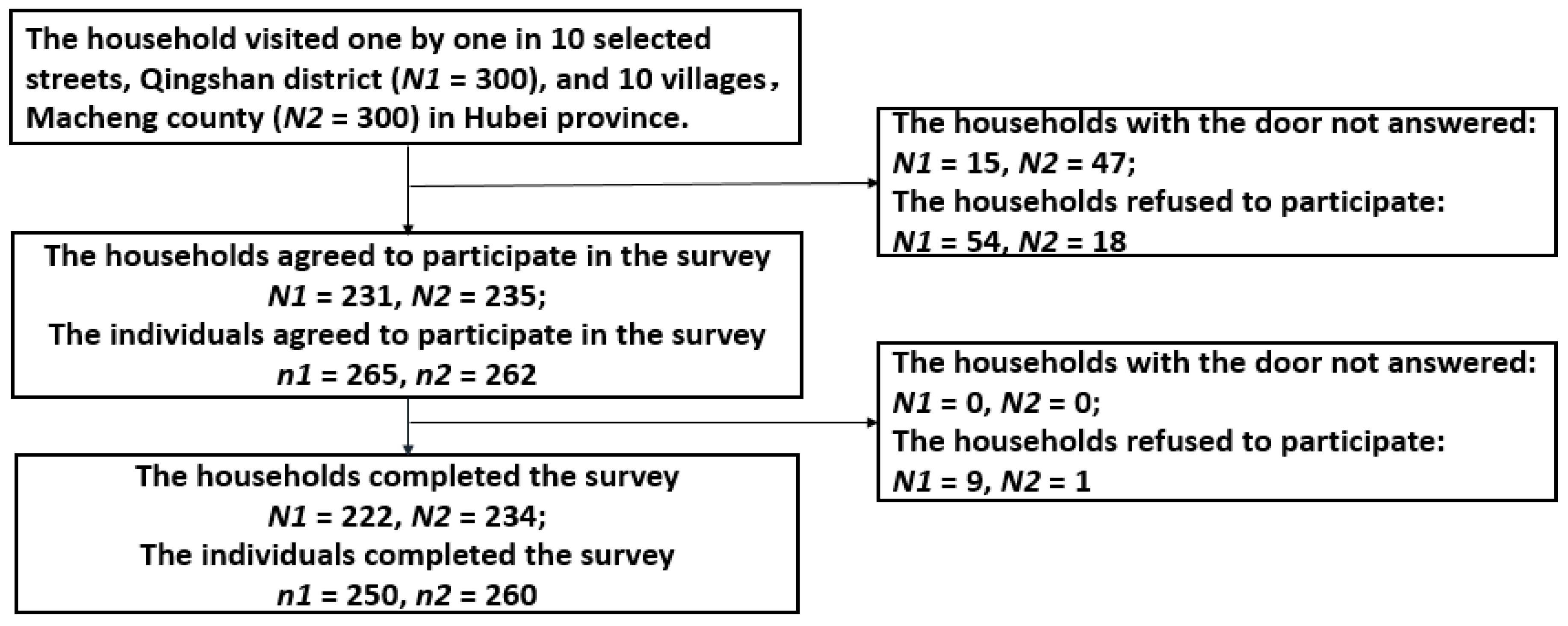
2.1. Study Design
2.2. Measurements
2.3. Statistical Analysis
2.4. Ethical Statement
3. Results
3.1. Socio-Demographic Characteristics of Participants
3.2. Factors Affecting Regularity of Health Seeking Behavior among Patients with Hypertension or Diabetes
3.3. Predictors of Regular Health-Seeking Behavior among Diabetic and Hypertensive Patients
4. Discussion
5. Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization (WHO). Global Status Report on Non-Communicable Diseases; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Xu, L.; Meng, Q. The second part of Fifth National Health Service Survey—Health service need demand and utilization. Chin. J. Health Inform. Manag. 2014, 11, 193–194. (In Chinese) [Google Scholar]
- Finkelstein, E.A.; Chay, J.; Bajpai, S. The Economic Burden of Self-Reported and Undiagnosed Cardiovascular Diseases and Diabetes on Indonesian Households. PLoS ONE 2014, 9, e995726. [Google Scholar]
- Bauer, U.E.; Briss, P.A.; Goodman, R.A.; Bowman, B.A. Prevention of chronic disease in the 21st century: Elimination of the leading preventable causes of premature death and disability in the USA. Lancet 2014, 384, 45–52. [Google Scholar] [CrossRef]
- Yoon, P.W.; Bastian, B.; Anderson, R.N.; Collins, J.L.; Jaffe, H.W. Potentially preventable deaths from the five leading causes of death—United States, 2008–2010. MMWR Morb. Mortal. Wkly Rep. 2014, 63, 369–374. [Google Scholar] [PubMed]
- Samb, B.; Desai, N.; Nishtar, S.; Mendis, S.; Bekedam, H.; Wright, A.; Hsu, J.; Martiniuk, A.; Celletti, F.; Patel, K.; et al. Prevention and management of chronic disease: A litmus test for health-systems strengthening in low-income and middle-income countries. Lancet 2010, 376, 1785–1797. [Google Scholar] [CrossRef]
- Qiu, M.; Shen, W.; Song, X.; Ju, L.; Tong, W.; Wang, H.; Zheng, S.; Jin, Y.; Wu, Y.; Wang, W.; et al. Effects of pre-diabetes mellitus alone or plus hypertension on subsequent occurrence of cardiovascular disease and diabetes mellitus: Longitudinal study. Hypertension 2015, 65, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Gorgui, J.; Gorgui, J.; Gorshkov, M.; Khan, N.; Daskalopoulou, S.S. Hypertension as a risk factor for ischemic stroke in women. Can. J. Cardiol. 2014, 30, 774–782. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Dong, D.; Ji, L.; Fu, H.; Feng, Z.; Bishwajit, G.; He, Z.; Ming, H.; Fu, Q.; Xian, Y. What Contributes to the Activeness of Ethnic Minority Patients with Chronic Illnesses Seeking Allied Health Services? A Cross-Sectional Study in Rural Western China. Int. J. Environ. Res. Public Health 2015, 12, 11579–11593. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Feng, Z.; Zhang, P.; Shen, X.; Wei, L.; Tian, M. Association between Time of Pay-for-Performance for Patients and Community Health Services Use by Chronic Patients. PLoS ONE 2014, 9, e897932. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.J.; Berman, M.D.; Hiratsuka, V.Y.; Frazier, R.R. The Effect of Regular Primary Care Utilization on Long-Term Glycemic and Blood Pressure Control in Adults with Diabetes. J. Am. Board Fam. Med. 2015, 28, 28–37. [Google Scholar] [CrossRef] [PubMed]
- McCusker, J.; Roberge, D.; Lesque, J.F.; Ciampi, A.; Vadeboncoeur, A.; Larouche, D.; Steven, S. Emergency department visits and primary care among adults with chronic conditions. Med. Care 2010, 48, 972–980. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Thomas, S.L.; Guthridge, S.L.; Wakerman, J. Better health outcomes at lower costs: The benefits of primary care utilization for chronic disease management in remote Indigenous communities in Australia’s Northern Territory. BMC Health Serv. Res. 2014, 14, 463. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Bishwajit, G.; Ji, L.; Feng, D.; Fang, H.; Fu, H.; Shao, T.; Shao, P.; Liu, C.; Feng, Z.; et al. Improving the Blood Pressure Control with the Pro-Active Attitude of Hypertensive Patients Seeking Follow-up Services: Evidence From China. Medicine 2016, 95, e3233. [Google Scholar] [CrossRef] [PubMed]
- Hanley, J.; Fairbrother, P.; McCloughan, L.; Pagliari, C.; Paterson, M.; Pinnock, H.; Sheikh, A.; Wild, S.; McKinstry, B. Qualitative study of telemonitoring of blood glucose and blood pressure in type 2 diabetes. BMJ Open 2015, 5, e008896. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.R.; Campbell, K.M. Home monitoring of glucose and blood pressure. Am. Fam. Phys. 2007, 76, 255–260. [Google Scholar]
- Cramer, J.A.; Cramer, J.A.; Benedict, A.; Muszbek, N.; Keskinaslan, A.; Khan, Z.M. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: A review. Int. J. Clin. Pract. 2008, 62, 76–87. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z. Hypertension Control in Communities (HCC): Evaluation result of blood pressure management among hypertensive. Chin. J. Epidemiol. 2010, 31, 1–4. (In Chinese) [Google Scholar]
- Neufeld, E.; Viau, K.A.; Hirdes, J.P.; Warry, W. Predictors of frequent emergency department visits among rural older adults in Ontario using the Resident Assessment Instrument-Home Care. Aust. J. Rural Health 2016, 24, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Rowan, C.G.; Flory, J.; Stempniewicz, N.; Cuddeback, J.; Brunelli, S.M. Stage 2 hypertension: Predictors of failure to achieve blood pressure control and the impact of adding one additional antihypertensive class. Pharmacoepidemiol. Drug Saf. 2015, 24, 1170–1179. [Google Scholar] [CrossRef] [PubMed]
- Miao, Y.; Ye, T.; Qian, D.; Li, J.; Zhang, L. Utilization of Rural Primary Care Physicians’ Visit Services for Diabetes Management of Public Health in Southwestern China: A Cross-Sectional Study from Patients’ View. Iran. J. Public Health 2014, 43, 769–777. [Google Scholar] [PubMed]
- Seo, Y.; Park, J.; Lim, J. Factors Affecting Regular Medical Services Utilization of Chronic Disease Patients—Focusing on the Hypertension, Diabetes Mellitus, Hyperlipidemia. Korean J. Health Educ. Promot. 2014, 31, 27–37. [Google Scholar] [CrossRef]
- Nicolas, S.; Zeynep, O. Disparities in Regular Health Care Utilisation in Europe. In The Individual and the Welfare State; Börsch-Supan, A., Brandt, M., Hank, K., Schröder, M., Eds.; Springer: Berlin/Heidelberg, Germany; Paris, France, 2011; pp. 241–251. [Google Scholar]
- Fang, P.; Han, S.; Zhao, L.; Fang, Z.; Zhang, Y.; Zou, X. What limits the utilization of health services among the rural population in the Dabie Mountains—Evidence from Hubei province, China? BMC Health Serv. Res. 2014, 14, 379. [Google Scholar] [CrossRef] [PubMed]
- Wang, J. Home blood pressure monitoring: A consensus document. Chin. J. Front. Med. Sci. 2012, 4, 43–47. (In Chinese) [Google Scholar]
- Wang, J. The Chinese medical association of diabetes, Chinese Type 2 Diabetes Prevention Guidance (2010 edition). Chin. J. Diabetes 2012, 20, 81–117. (In Chinese) [Google Scholar]
- Wong, M.C.; Wang, H.H.; Kwan, M.W.; Fong, B.C.; Chan, W.M.; de Zhang, X.; Li, S.T.; Yan, B.P.; Coats, A.J.; Griffiths, S.M. Dietary counselling has no effect on cardiovascular risk factors among Chinese Grade 1 hypertensive patients: A randomized controlled trial. Eur. Heart J. 2015, 36, 2598–2607. [Google Scholar] [CrossRef] [PubMed]
- Elixhauser, A.; Steiner, C.; Harris, D.R.; Coffey, R.M. Comorbidity measures for use with administrative data. Med. Care 1998, 36, 8–27. [Google Scholar] [CrossRef] [PubMed]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multi-morbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- Xu, L.; Meng, Q. The Fifth National Health Service Survey—Family Economic Status. The Fifth National Health Service Survey; Center for Health Statistics and Information; China Union Medical College Hospital Press: Beijing, China, 2015; p. 332. [Google Scholar]
- Jones, A.L.; Cochran, S.D.; Leibowitz, A.; Wells, K.B.; Kominski, G.; Mays, V.M. Usual Primary Care Provider Characteristics of a Patient-Centered Medical Home and Mental Health Service Use. J. Gen. Intern. Med. 2015, 30, 1828–1836. [Google Scholar] [CrossRef] [PubMed]
- Niu, H.; Tian, M.; Ma, A.; Wang, C.; Zhang, L. Differences and determinants in access to essential public health services in China: A case study with hypertension people and under-sixes as target population. Chin. Med. J. 2014, 127, 1626–1632. [Google Scholar] [PubMed]
- Zhang, P.; Zhao, L.; Liang, J.; Qiao, Y.; He, Q.; Zhang, L.; Wang, F.; Liang, Y. Societal determination of usefulness and utilization wishes of community health services: A population-based survey in Wuhan city, China. Health Policy Plan. 2015, 30, 1243–1250. [Google Scholar] [CrossRef] [PubMed]
- Ionescu-Ittu, R.; McCusker, J.; Ciampi, A.; Vadeboncoeur, A.M.; Roberge, D.; Larouche, D.; Verdon, J.; Pineault, R. Continuity of primary care and emergency department utilization among elderly people. Can. Med. Assoc. J. 2007, 177, 1362–1368. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, O.; Delu, Y.; Wong, S.T.; Bowen, C. Evolution of primary care in China 1997–2009. Health Policy 2011, 100, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.H.; Wang, J.J.; Wong, S.Y.; Wong, M.C.; Li, F.J.; Wang, P.X.; Zhou, Z.H.; Zhu, C.Y.; Griffiths, S.M.; Mercer, S.W. Epidemiology of multimorbidity in China and implications for the healthcare system: Cross-sectional survey among 162,464 community household residents in southern China. BMC Med. 2014, 12, 188. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.H.; Wong, S.Y.; Wong, M.C.; Wei, X.L.; Wang, J.J.; Li, D.K.; Tang, J.L.; Gao, G.Y.; Griffiths, S.M. Patients’ Experiences in Different Models of Community Health Centers in Southern China. Ann. Fam. Med. 2013, 11, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Wolff, J.L.; Starfield, B.; Anderson, G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch. Intern. Med. 2002, 162, 2269–2276. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.H.; Wang, J.J.; Wong, S.Y.; Wong, M.C.; Mercer, S.W.; Griffiths, S.M. The development of urban community health centres for strengthening primary care in China: A systematic literature review. Br. Med. Bull. 2015, 116, 139–153. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Ji, L.; Hu, T.; Bishwajit, G.; Da, F.; Ming, H.; Xian, Y.; Fu, Q.; He, Z.; Fu, H.; et al. Determinants of public malaria awareness during the national malaria elimination programme: A cross-sectional study in rural China. Malar. J. 2016, 15, 372. [Google Scholar] [PubMed]
- Tian, M.; Chen, Y.; Zhao, R.; Chen, L.; Chen, X.; Feng, D.; Feng, Z. Chronic disease knowledge and its determinants among chronically ill adults in rural areas of Shanxi Province in China: A cross-sectional study. BMC Public Health 2011, 11, 948. [Google Scholar] [CrossRef] [PubMed]
- Egan, B.M.; Zhao, Y.; Axon, R.N. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA 2010, 303, 2043–2050. [Google Scholar] [CrossRef] [PubMed]
- Reeves, D.; Blickem, C.; Vassilev, I.; Brooks, H.; Kennedy, A.; Richardson, G.; Rogers, A. The contribution of social networks to the health and self-management of patients with long-term conditions: A longitudinal study. PLoS ONE 2014, 9, e98340. [Google Scholar] [CrossRef] [PubMed]
- Sang, S.; Wang, Z.; Yu, C. Evaluation of Health Care System Reform in Hubei Province, China. Int. J. Environ. Res. Public Health 2014, 11, 2262–2277. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, W.R.; Godley, P.A.; Clark, J.A.; Talcott, J.A.; Finnegan, T.; Mishel, M.; Bensen, J.; Rayford, W.; Su, L.J.; Fontham, E.T.H.; et al. Racial differences in trust and regular source of patient care and the implications for prostate cancer screening use. Cancer 2009, 115, 5048–5059. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Participants (N = 510) | Percent (%) |
|---|---|---|
| Gender | ||
| Male | 251 | 49.2 |
| Female | 259 | 50.8 |
| Age | ||
| <50 | 62 | 12.1 |
| 50–59 | 109 | 21.4 |
| 60–69 | 155 | 30.4 |
| ≥70 | 184 | 36.1 |
| Education level | ||
| No formal education | 92 | 18.0 |
| 1–6 years study | 155 | 30.4 |
| 7–9 years study | 150 | 29.4 |
| >9 years study | 113 | 22.2 |
| Marital status | ||
| Unmarried | 11 | 2.1 |
| Married | 422 | 82.8 |
| Divorced | 11 | 2.2 |
| Widowed | 66 | 12.9 |
| Chronic disease | ||
| Hypertension | 363 | 71.18 |
| Diabetes | 73 | 14.31 |
| Hypertension and Diabetes | 74 | 14.51 |
| Type of health insurance | ||
| Medical insurance for urban works | 234 | 45.9 |
| Medical insurance for resident or NRCM 1 | 276 | 54.1 |
| Household income (CNY) 2 | ||
| Low 3 | 209 | 40.9 |
| Fair 4 | 127 | 25.0 |
| Good 5 | 174 | 34.1 |
| Household members | ||
| 1 | 31 | 6 |
| ≥2 | 479 | 94 |
| Severity of chronic disease | ||
| Grade 1 6 | 186 | 36.5 |
| Grade 2 7 | 203 | 39.8 |
| Grade 3 8 | 121 | 23.7 |
| Place of residence | ||
| Rural | 250 | 49.0 |
| Urban | 260 | 51.0 |
| Assessment of Health-Seeking Behavior | ||
| Regular | 215 | 42.2 |
| Irregular | 295 | 57.8 |
| Regular 1 N (%) | Irregular 2 N (%) | p-Value | |
|---|---|---|---|
| Individual factors | 215 (42.2) | 295 (57.8) | |
| Age | |||
| <50 | 15 (7.0) | 47 (15.9) | 0.001 |
| 50–59 | 38 (17.7) | 71 (24.1) | |
| 60–69 | 71 (33.0) | 84 (28.5) | |
| ≥70 | 91 (42.3) | 93 (31.5) | |
| Education level | |||
| No formal education | 35 (16.3) | 57 (19.3) | 0.065 |
| 1–6 years study | 62 (28.8) | 93 (31.5) | |
| 7–9 years study | 58 (27.0) | 92 (31.2) | |
| >9 years study | 60 (27.9) | 53 (18.0) | |
| Marital status | |||
| Unmarried | 5 (2.3) | 6 (2.0) | 0.412 |
| Married | 171 (79.5) | 251 (82.7) | |
| Divorced | 6 (2.8) | 5 (2.2) | |
| Widowed | 33 (15.3) | 33 (12.9) | |
| Comorbidity 3 | |||
| 1 sort | 86 (40.0) | 187 (63.4) | <0.001 |
| 2 sorts | 108 (50.2) | 87 (29.5) | |
| ≥3 sorts | 21 (9.8) | 21 (7.1) | |
| Self-reported health score | |||
| Low (<60) | 24 (11.2) | 51 (17.2) | 0.091 |
| Medium (60–80) | 105 (48.8) | 122 (41.4) | |
| High (>80) | 86 (40.0) | 122 (41.4) | |
| Economic factors | |||
| Economic burden of disease | |||
| High 4 | 42 (19.5) | 163 (55.3) | <0.001 |
| Normal | 173 (80.5) | 132 (44.7) | |
| Health insurance | |||
| Medical insurance for urban works | 117 (54.4) | 117 (39.7) | 0.001 |
| Medical insurance for residents or NRCM | 98 (45.6) | 178 (60.3) | |
| Household income (CNY) 5 | |||
| Low 6 | 56 (26.0) | 153 (51.9) | <0.001 |
| Fair 7 | 69 (32.1) | 58 (19.7) | |
| Good 8 | 90 (41.9) | 84 (28.5) | |
| Social factors | |||
| Head of household | |||
| No | 96 (44.7) | 129 (43.7) | 0.836 |
| Yes | 119 (55.3) | 166 (56.3) | |
| Number of household members with chronic diseases | |||
| 1 | 80 (37.2) | 130 (44.1) | 0.072 |
| ≥2 | 135 (62.8) | 165 (55.9) | |
| Areas of residence | |||
| Rural | 127 (59.1) | 123 (41.7) | <0.001 |
| Urban | 88 (40.9) | 172 (58.3) | |
| The economic contribution of the family | |||
| Major 9 | 121 (56.3) | 147 (49.8) | 0.301 |
| Minor 10 | 66 (30.7) | 109 (36.9) | |
| No 11 | 28 (13.0) | 39 (13.3) | |
| Social Support (escort/someone to accompany to hospital visits) | |||
| No | 87 (40.5) | 48 (16.3) | <0.001 |
| Yes 12 | 128 (59.5) | 247 (83.7) | |
| Usual provider | |||
| Others 13 | 162 (75.3) | 114 (38.6) | <0.001 |
| Usual primary care provider 14 | 53 (24.7) | 181 (61.4) |
| Predictors | Adjusted | Unadjusted | ||||
|---|---|---|---|---|---|---|
| B 1 | OR 2 | 95% CI 3 | B | OR | 95% CI | |
| Age (ref < 50) | ||||||
| 50–59 | 0.891 | 2.437 | 0.996–5.964 | 0.517 | 1.677 | 0.831–3.384 |
| 60–69 | 0.867 * | 2.379 | 1.026–5.514 | 0.974 ** | 2.648 | 1.367–5.132 |
| ≥70 | 1.325 ** | 3.762 | 1.617–8.751 | 1.12 ** | 3.066 | 1.602–5.868 |
| Comorbidity (ref = 1 sorts) | ||||||
| 2 sorts | 0.943 ** | 2.567 | 1.512–4.359 | 0.993 ** | 2.699 | 1.845–3.950 |
| ≥2 sorts | 1.498 ** | 4.473 | 1.843–10.855 | 0.777 * | 2.174 | 1.128–4.193 |
| Economic burden of disease (ref = High) | ||||||
| Normal | 1.725 ** | 5.611 | 3.273–9.618 | 1.627 ** | 5.086 | 3.383–7.648 |
| Household income (CNY) 4 (ref = Low 5) | ||||||
| Fair 6 | 1.797 ** | 6.031 | 3.153–11.535 | 1.179 ** | 3.25 | 2.043–5.171 |
| Good 7 | 1.808 ** | 6.097 | 3.341–11.126 | 1.074 ** | 2.927 | 1.910–4.485 |
| Place of residence (ref = rural) | ||||||
| Urban | 0.87 ** | 2.387 | 1.352–4.212 | 0.702 ** | 2.018 | 1.412–2.884 |
| Hospital accompaniment (ref = No) | ||||||
| Yes | 1.598 ** | 4.945 | 2.813–8.691 | 1.252 ** | 3.498 | 2.317–5.281 |
| Usual provider (ref = Primary hospitals) | ||||||
| Others | 2.13 ** | 8.418 | 4.812–14.727 | 1.58 ** | 4.853 | 3.290–7.159 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feng, D.; Serrano, R.; Ye, T.; Tang, S.; Duan, L.; Xu, Y.; Yang, J.; Liang, Y.; Chen, S.; Feng, Z.; et al. What Contributes to the Regularity of Patients with Hypertension or Diabetes Seeking Health Services? A Pilot Follow-Up, Observational Study in Two Sites in Hubei Province, China. Int. J. Environ. Res. Public Health 2016, 13, 1268. https://doi.org/10.3390/ijerph13121268
Feng D, Serrano R, Ye T, Tang S, Duan L, Xu Y, Yang J, Liang Y, Chen S, Feng Z, et al. What Contributes to the Regularity of Patients with Hypertension or Diabetes Seeking Health Services? A Pilot Follow-Up, Observational Study in Two Sites in Hubei Province, China. International Journal of Environmental Research and Public Health. 2016; 13(12):1268. https://doi.org/10.3390/ijerph13121268
Chicago/Turabian StyleFeng, Da, Ray Serrano, Ting Ye, Shangfeng Tang, Lei Duan, Yuan Xu, Jian Yang, Yuan Liang, Shanquan Chen, Zhanchun Feng, and et al. 2016. "What Contributes to the Regularity of Patients with Hypertension or Diabetes Seeking Health Services? A Pilot Follow-Up, Observational Study in Two Sites in Hubei Province, China" International Journal of Environmental Research and Public Health 13, no. 12: 1268. https://doi.org/10.3390/ijerph13121268





