Indoor Temperatures in Patient Waiting Rooms in Eight Rural Primary Health Care Centers in Northern South Africa and the Related Potential Risks to Human Health and Wellbeing
Abstract
:1. Introduction
2. Materials and Methods
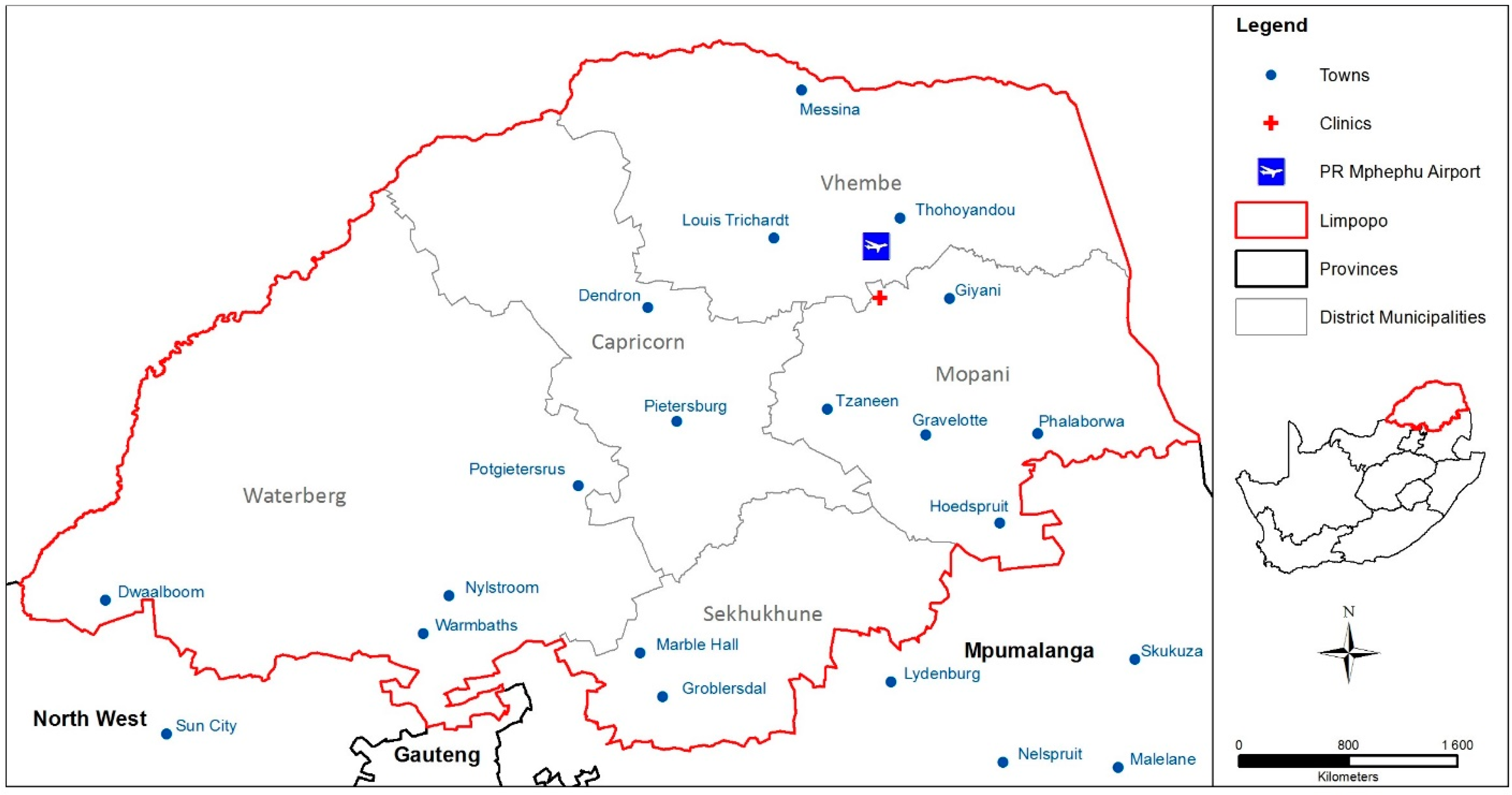
2.1. Study Area and Sample
2.2. Procedures for Data Collection
2.3. Temperature and Humidity Measurements
2.4. Ambient Outdoor Temperature Data
2.5. Apparent Temperature Calculations
2.6. Data Processing and Statistical Analysis
3. Results
3.1. Sample Description
3.2. Indoor Temperature and Relative Humidity Measurements
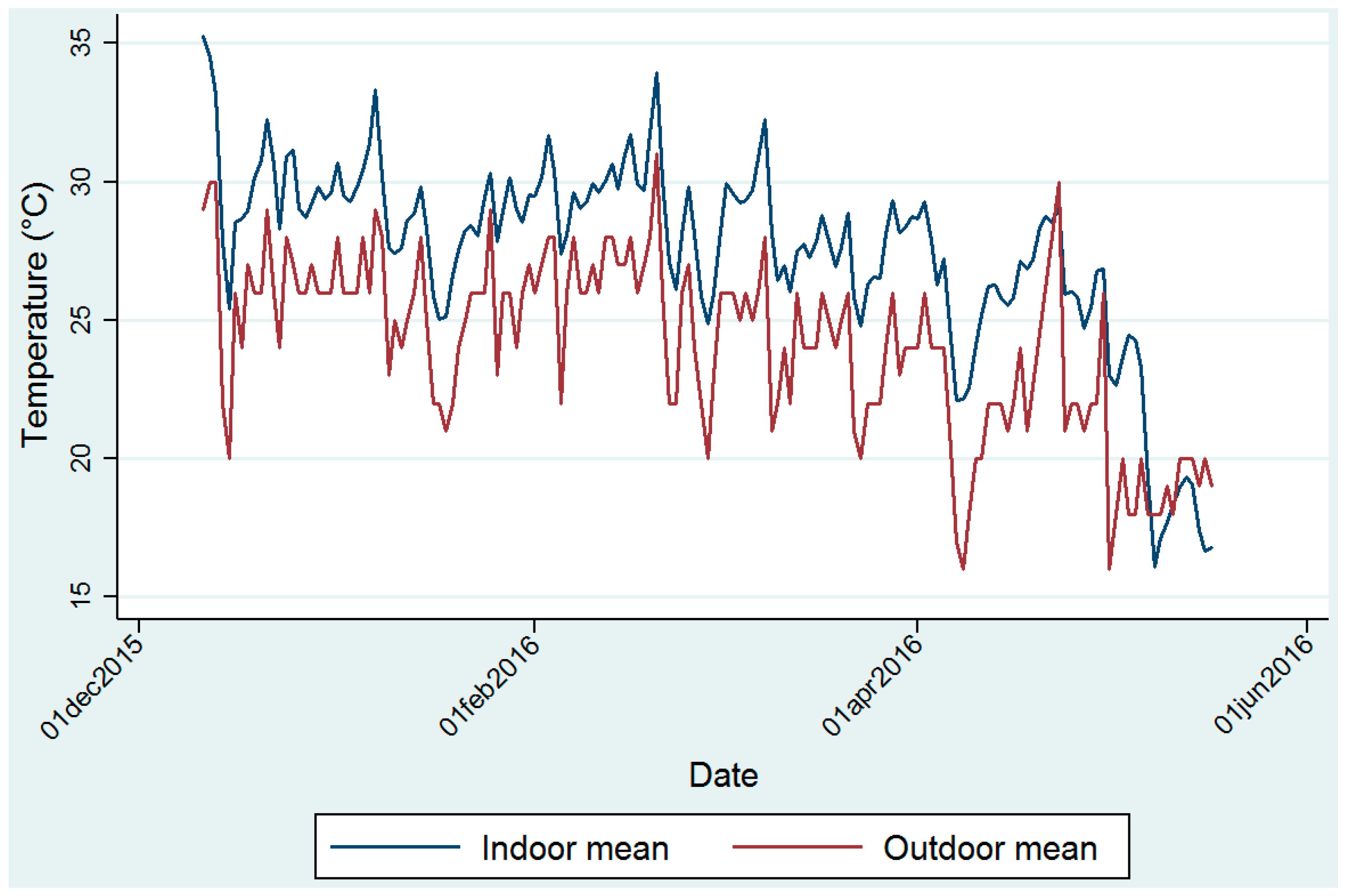
3.3. Ambient Temperature Data
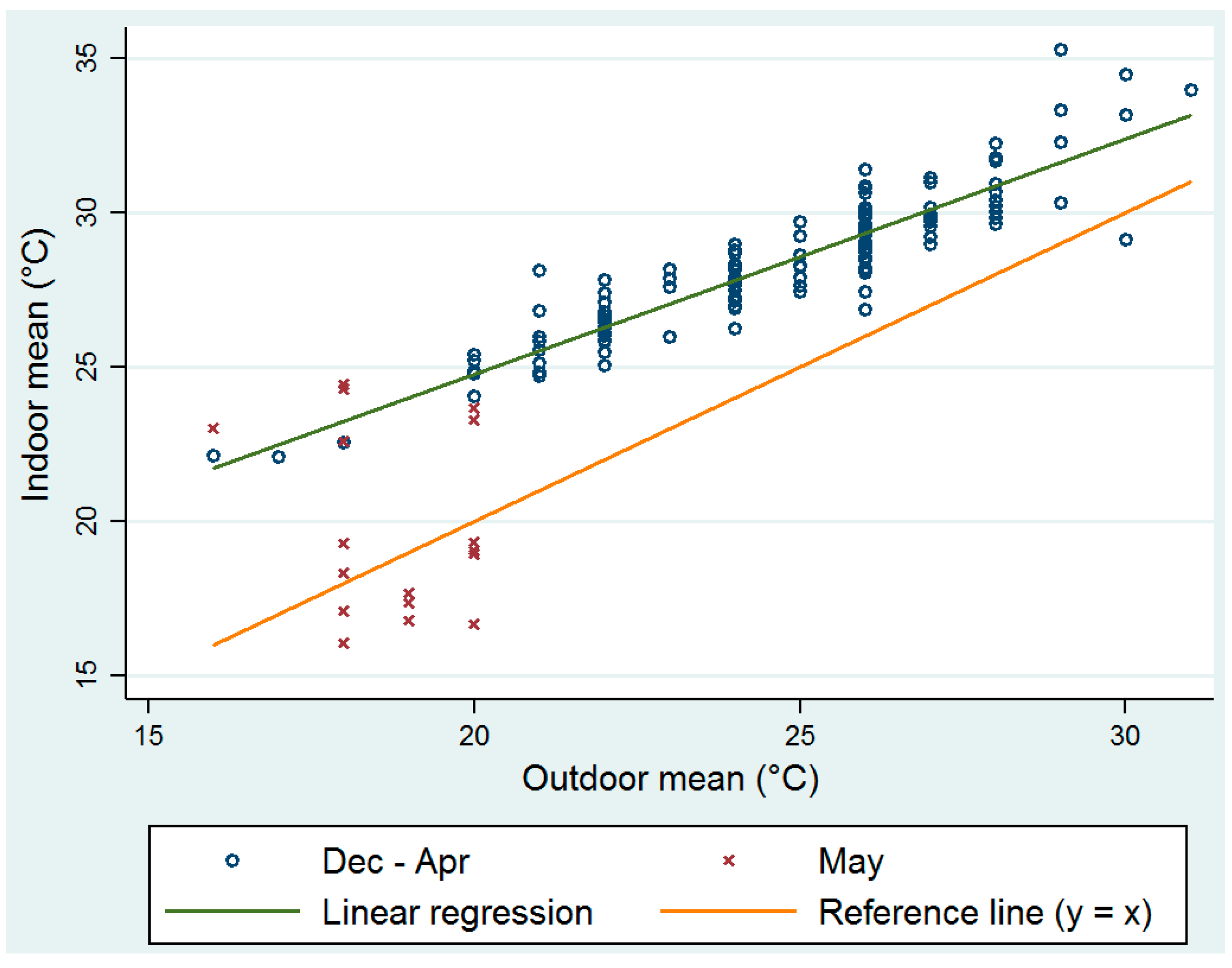
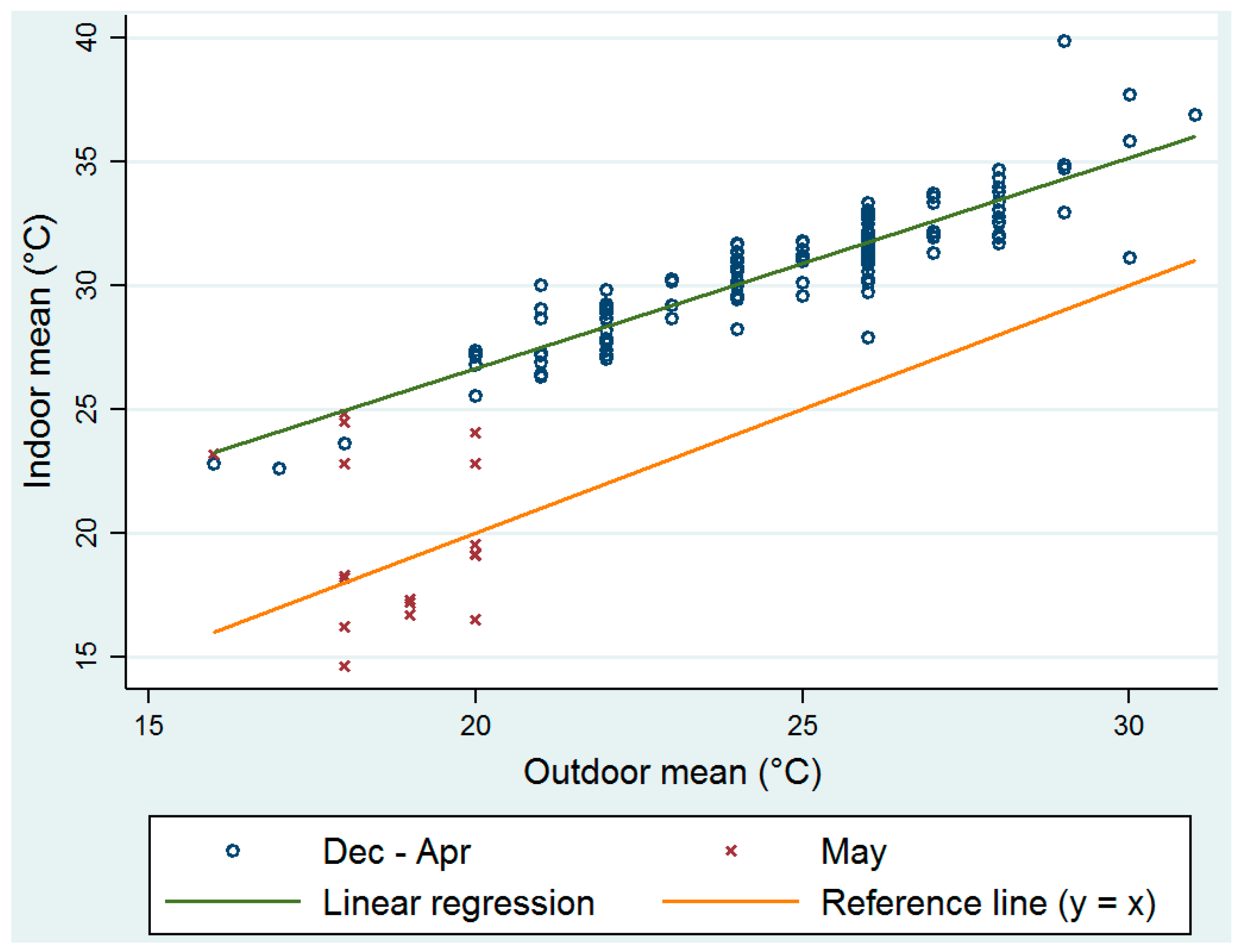
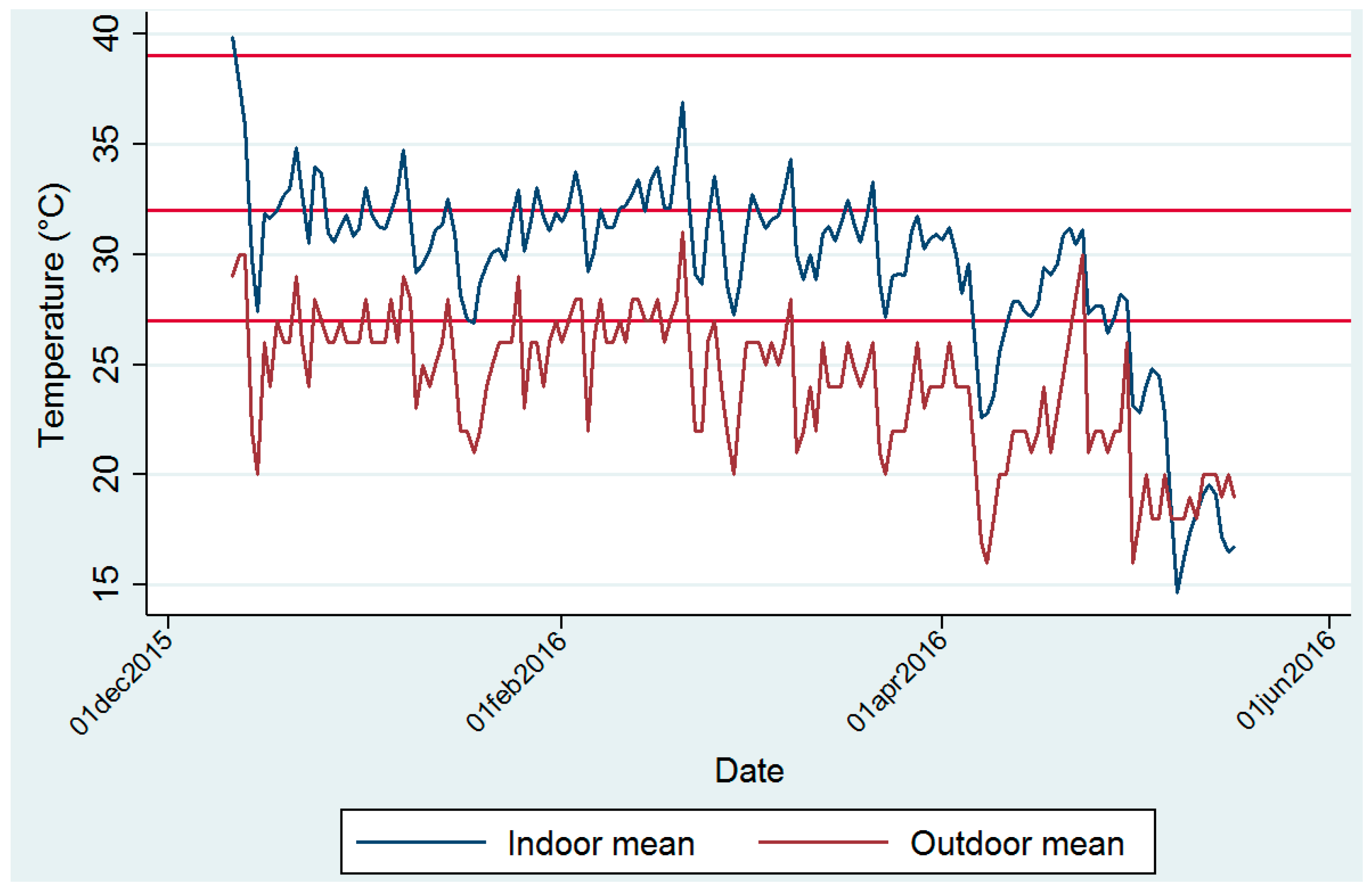
3.4. Comparison between Indoor Measured Temperature and Ambient Outdoor Temperature
3.5. Calculated Clinic Indoor Apparent Temperature
3.6. Clinic Indoor Apparent Temperature and Potential Human Health Impacts during Patient Waiting Times
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Basu, R. High ambient temperature and mortality: A review of epidemiologic studies from 2001 to 2008. Environ. Health Glob. Access Sci. Source 2009, 8, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Hondula, D.M.; Balling, R.C.; Vanos, J.K.; Georgescu, M. Rising Temperatures, Human Health, and the Role of Adaptation. Curr. Clim. Chang. Rep. 2015, 1, 144–154. [Google Scholar] [CrossRef]
- Kovats, R.S.; Hajat, S. Heat stress and public health: A critical review. Ann. Rev. Public Health 2008, 29, 41–55. [Google Scholar] [CrossRef] [PubMed]
- Arbuthnott, K.; Hajat, S. Health Climate Change Impacts Report Card 2015: Hotter Summers and Heat Waves. Available online: http://www.nerc.ac.uk/research/partnerships/ride/lwec/report-cards/health/ (accessed on 20 October 2016).
- Zanobetti, A.; O’Neill, M.S.; Gronlund, C.J.; Schwartz, J.D. Summer temperature variability and long-term survival among elderly people with chronic disease. Proc. Natl. Acad. Sci. USA 2012, 109, 6608–6613. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Cheng, Y.; Cui, G.; Peng, C.; Xu, Y.; Wang, Y.; Jin, Y. Association between high temperature and mortality in metropolitan areas of four cities in various climatic zones in China: A time-series study. Environ. Health 2014, 13, 65. [Google Scholar] [CrossRef] [PubMed]
- Portier, C.J.; Thigpen, T.K.; Carter, S.R.; Dilworth, C.H.; Grambsch, A.E.; Gohlke, J.; Whung, P.Y. A Human Health Perspective on Climate Change: A Report Outlining the Research Needs on the Human Health Effects of Climate Change. 2010. Available online: https://www.niehs.nih.gov/health/materials/a_human_health_perspective_on_climate_change_full_report_508.pdf (accessed on 20 October 2016). [Google Scholar]
- Seltenrich, M. Between Extremes: Health effects of Heat and Cold. Environ. Health Perspect. 2015, 123, A275–A280. [Google Scholar] [CrossRef] [PubMed]
- Wright, C.Y.; Garland, R.M.; Norval, M.; Vogel, C. Human health impacts in a changing South African climate. S. Afr. Med. J. 2014, 104, 579–582. [Google Scholar] [CrossRef] [PubMed]
- Garland, R.M.; Matooane, M.; Engelbrecht, F.A.; Bapope, M.M.; Landman, W.A.; Naidoo, M.; Wright, C.Y. Regional Projections of Extreme Apparent Temperature Days in Africa and the Related Potential Risk to Human Health. Int. J. Environ. Res. Public Health 2015, 12, 12577–12604. [Google Scholar] [CrossRef] [PubMed]
- Mathee, A.; Oba, J.; Rose, A. Climate change impacts on working people (the HOTHAPS initiative): Findings of the South African pilot study. Glob. Health Action 2010, 3. [Google Scholar] [CrossRef] [PubMed]
- Bruijns, S.R.; Wallis, L.A.; Burch, V.C. Effect of introduction of nurse triage on waiting times in a South African emergency department. Emerg. Med. J. 2008, 25, 395–397. [Google Scholar] [CrossRef] [PubMed]
- Rauf, W.; Blittz, J.J.; Geyser, M.M.; Rauf, A. Quality improvement cycles that reduced waiting times at Tshwane District Hospital Emergency Department. S. Afr. Fam. Pract. 2008, 50, 43. [Google Scholar] [CrossRef]
- Gray, A.; Vawda, Y. Health Policy and Legislation. In South African Health Review 2014/15; Padarath, A., King, J., English, R., Eds.; Health Systems Trust: Pretoria, South Africa, 2015. [Google Scholar]
- Fryatt, R.; Hunter, J. The Ideal Clinic in South Africa: Planning for Implementation. South African Health Review 2014–2015. 2015. Available online: http://www.profnetmedical.co.za/media/1179/south-african-health-review-2014-15-part-2compressed.pdf (accessed on 20 October 2016).
- Thompson, A.A.; Matamale, L.; Kharidza, S.D. Impact of climate change on children’s health in Limpopo Province, South Africa. Int. J. Environ. Res. Public Health 2012, 9, 831–854. [Google Scholar] [CrossRef] [PubMed]
- Malatji, D.P.; Tsotetsi, A.M.; van Marie-Koster, E.; Muchadeyi, F.C. A Description of Village Chicken Production Systems and Prevalence of Gastrointestinal Parasites: Case Studies in Limpopo and KwaZulu-Natal Provinces of South Africa. Onderstepoort J. Vet. Res. 2016, 83, a968. [Google Scholar] [CrossRef] [PubMed]
- Environmental Systems Research Institute (ESRI). ArcGIS Desktop: Release 10; Environmental Systems Research Institute: Redlands, CA, USA, 2011. [Google Scholar]
- Weather Underground. Available online: www.weatherunderground.com (accessed on 20 October 2016).
- Bidassey-Manilal, S.; Wright, C.Y.; Engelbrecht, J.C.; Albers, P.N.; Garland, R.M.; Matooane, M. Students’ perceived heat-health symptoms increased with warmer temperatures. Int. J. Environ. Res. Public Health 2016, 13, 566. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, J.L.; Scwartz, J.; Dockery, D.W. The relationship between indoor and outdoor temperature, relative humidity, and absolute humidity. Indoor Air 2014, 24, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Baccini, M.; Biggeri, A.; Accetta, G.; Kosatsky, T.; Katsouyanni, K.; Analitis, A.; Anderson, H.R.; Bisanti, L.; D’Ippoliti, D.; Danova, J.; et al. Heat effects on mortality in 15 European cities. Epidemiology 2008, 19, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; O’Neill, M.S.; Ranjit, N.; Borja-Aburto, V.H.; Cifuentes, L.A.; Gouveia, N.C. Vulnerability to heat-related mortality in Latin America: A case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int. J. Epidemiol. 2008, 37, 796–804. [Google Scholar] [CrossRef] [PubMed]
- Steadman, R.G. Norms of Apparent Temperature in Australia. Aust. Meteorol. Mag. 1994, 43, 6. [Google Scholar]
- National Weather Service Weather Forecast Office: Amarillo, TX. What Is the Heat Index? Available online: http://www.srh.noaa.gov/ama/?n=heatindex (accessed on 14 October 2016).
- Kilbourne, E.M. The spectrum of illness during heatwaves. Am. J. Prev. Med. 1999, 16, 359–360. [Google Scholar] [PubMed]
- Olivier, D. Temperature, human health, and adaptation: A review of the empirical literature. Energy Econ. 2014, 46, 606–619. [Google Scholar]
- Haines, A.; Kovats, R.S.; Campbell-Lendrum, D.; Corvalan, C. Climate change and human health: Impacts, vulnerability and public health. Lancet 2006, 367, 2101–2109. [Google Scholar] [CrossRef]
- Verkuijl, S.; Middelkoop, K. Protecting Our Front-liners: Occupational Tuberculosis Prevention through Infection Control Strategies. Clin. Infect. Dis. 2016, 62 (Suppl. 3), S231–S237. [Google Scholar] [CrossRef] [PubMed]
- Naidoo, S.; Seevnarain, K.; Nordstrom, D.L. Tuberculosis infection control in primary health clinics in eThekwini, KwaZulu-Natal, South Africa. Int. J. Tuberc. Lung Dis. 2012, 16, 1600–1604. [Google Scholar] [CrossRef] [PubMed]
- National Department of Health. Towards Quality Care for Patients. National Core Standards for Health Establishments in South Africa. Republic of South Africa, 2011. Available online: http://www.rhap.org.za/wp-content/uploads/2014/05/National-Core-Standards-2011-1.pdf (accessed on 20 October 2016).
- Beggs, C.B.; Sheperd, S.J.; Kerr, K.G. Potential for airborne transmission of infection in the waiting areas of healthcare premises: Stochastic analysis using a Monte Carlo model. BMC Infect. Dis. 2010, 10, 247. [Google Scholar] [CrossRef] [PubMed]
- McMichael, A.J.; Campbell-Lendrum, D.H.; Corvalan, C.F.; Ebi, K.L.; Githeko, A.; Scheraga, J.J.; Woodward, A. Climate Change and Human Health—Risk and Responses; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Woodward, A.; Smith, K.R.; Campbell-Lendrum, D.; Chadee, D.D.; Honda, Y.; Liu, Q.; Haines, A. Climate change and health: On the latest IPCC report. Lancet 2014, 383, 1185–1189. [Google Scholar] [CrossRef]
| Sub-District | Clinic No. | Installation | Collection | Type of Building and Roof | ||
|---|---|---|---|---|---|---|
| Date | Time | Date | Time | |||
| Greater Giyani | 9 | 17 December 2015 | - * | 5 May 2016 | - * | Brick walls, metal roof |
| 11 | 17 December 2015 | - * | 5 May 2016 | - * | Brick walls, metal roof, wide front veranda | |
| 3 | 11 December 2015 | 16:52 | 4 May 2016 | 9:17 | Brick walls, metal roof | |
| 1 | 11 December 2015 | 10:08 | 4 May 2016 | 10:31 | Brick walls, metal roof | |
| 8 | 11 December 2015 | 11:32 | 4 May 2016 | 12:32 | Brick walls, metal roof | |
| Greater Letaba | 6 | 17 December 2015 | 9:40 | 5 May 2016 | 11:00 | Brick walls, metal roof |
| 5 | 17 December 2015 | 12:00 | 4 May 2016 | 14:05 | Brick walls, metal roof | |
| 4 | 17 December 2015 | 13:20 | 5 May 2016 | 12:00 | Brick walls, metal roof | |
| 7 | 17 December 2015 | 10:55 | 5 May 2016 | 10:30 | Brick walls, metal roof | |
| Ba-Phalaborwa | 2 | 11 December 2015 | 18:06 | 4 May 2016 | 10:00 | Brick walls, metal roof |
| Greater Tzaneen | 10 | 11 December 2015 | - * | Not collected | - * | Brick walls, metal roof |
| Symptom Band | US NWS Classification | Apparent Temperature Range (°C) | US NWS Classified ‘Effect on Body‘ |
|---|---|---|---|
| I | Caution | 27–32 | Fatigue possible with prolonged exposure and/or physical activity |
| II | Extreme caution | 32–39 | Heat stroke, heat cramps, or heat exhaustion possible with prolonged exposure and/or physical activity |
| III | Danger | 39–51 | Heat cramps or heat exhaustion likely, and heat stroke possible with prolonged exposure and/or physical activity |
| IV | Extreme danger | 51 | Heat stroke highly likely |
© 2017 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wright, C.Y.; Street, R.A.; Cele, N.; Kunene, Z.; Balakrishna, Y.; Albers, P.N.; Mathee, A. Indoor Temperatures in Patient Waiting Rooms in Eight Rural Primary Health Care Centers in Northern South Africa and the Related Potential Risks to Human Health and Wellbeing. Int. J. Environ. Res. Public Health 2017, 14, 43. https://doi.org/10.3390/ijerph14010043
Wright CY, Street RA, Cele N, Kunene Z, Balakrishna Y, Albers PN, Mathee A. Indoor Temperatures in Patient Waiting Rooms in Eight Rural Primary Health Care Centers in Northern South Africa and the Related Potential Risks to Human Health and Wellbeing. International Journal of Environmental Research and Public Health. 2017; 14(1):43. https://doi.org/10.3390/ijerph14010043
Chicago/Turabian StyleWright, Caradee Y., Renée A. Street, Nokulunga Cele, Zamantimande Kunene, Yusentha Balakrishna, Patricia N. Albers, and Angela Mathee. 2017. "Indoor Temperatures in Patient Waiting Rooms in Eight Rural Primary Health Care Centers in Northern South Africa and the Related Potential Risks to Human Health and Wellbeing" International Journal of Environmental Research and Public Health 14, no. 1: 43. https://doi.org/10.3390/ijerph14010043







