Longer Nature-Based Rehabilitation May Contribute to a Faster Return to Work in Patients with Reactions to Severe Stress and/or Depression
Abstract
:1. Introduction
Hypotheses and Objectives
2. Materials and Methods
2.1. Study Population
2.2. Procedure
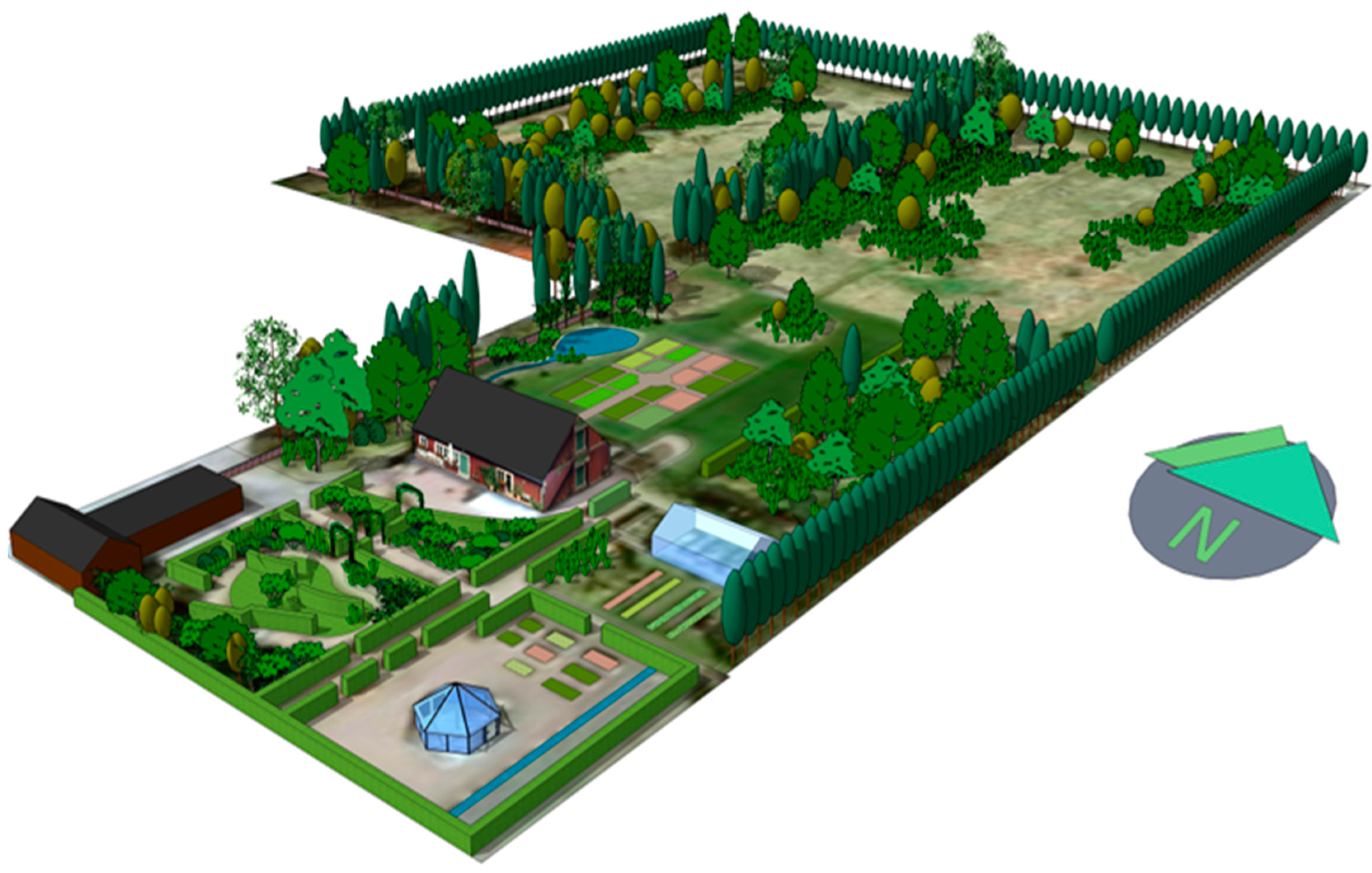
2.3. The Rehabilitation Program
2.4. Outcome Measures
2.4.1. Primary Outcome Measure
- Paid work: “Paid work as employee”, “Self-employed”, “Actively applying for paid work as employee”, or “Student/studying”.
- Work training: “Vocational training in the workplace”.
- Vocational action: “Work-oriented measures by (or supported by) the Swedish Social Insurance Agency”.
- Still sick: “Sick-listed”.
2.4.2. Secondary Outcome Measures
2.5. Statistical Analyses
3. Results
3.1. Return to Work Rates 12 Months After Rehabilitation
3.2. Associations Between Length of Rehabilitation Period and Return to Paid Work
4. Discussion
4.1. Return to Work
4.2. Psycho-Evolutionary Theory
4.3. Attention Restoration Theory
4.4. The Supportive Environment Theory
4.5. Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Salomon, J.A.; Wang, H.; Freeman, M.K.; Vos, T.; Flaxman, A.D.; Lopez, A.S.; Murray, C.J.L. Healthy life expectancy for 187 countries, 1990–2010: A systematic analysis for the Global Burden Disease Study 2010. Lancet 2012, 380, 2144–2162. [Google Scholar] [CrossRef]
- Steel, Z.; Marnane, C.; Iranpour, C.; Chey, T.; Jackson, J.W.; Patel, V.; Silove, D. The global prevalence of common mental disorders: A systematic review and meta-analysis. 1980–2013. Int. J. Epidemiol. 2014, 43, 476–493. [Google Scholar] [CrossRef] [PubMed]
- Försäkringskassan. Sjukfrånvaro i Psykiska Diagnoser En Studie av Sveriges Befolkning 16–64 år; Försäkringskassan: Stockholm, Sweden, 2014. [Google Scholar]
- Slany, C.; Schutte, S.; Chastang, J.-F.; Parent-Thirion, A.; Vermeylen, G.; Niedhammer, I. Psychosocial work factors and long sickness absence in Europe. Int. J. Environ. Res. Public Health 2014, 20, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Kuoppala, J.; Lamminpää, A. Rehabilitation and work ability: A systematic literature review. J. Rehabil. Med. 2008, 40, 796–804. [Google Scholar] [CrossRef] [PubMed]
- Swedish Government. Rehabiliteringsrådets Slutbetänkande [Final Commission Report from the Rehabilitation Council]; Swedish Government: Stockholm, Sweden, 2011.
- Vingård, E. Psykisk Ohälsa, Arbetsliv och Sjukfrånvaro. En Kunskapsöversikt och Rapport. [Mental Illness, Working Life and Sickness. A Review and Report]. Forte, Swedish Research Council for Health, Working Life and Welfare: Stockholm, Sweden, 2015. Available online: http://forte.se/wp-content/uploads/2015/04/psykisk-ohalsa-arbetsliv.pdf (accessed on 20 October 2017).
- SBU. Arbetsmiljöns Betydelse för Symtom på Depression och Utmattningssyndrom, En Systematisk Litteraturöversikt [The Importance of the Working Environment for Symptoms of Depression and Exhaustion, A Systematic Literature Review], SBU-Rapport nr 223; Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU): Stockholm, Sweden, 2014. [Google Scholar]
- Bratman, G.N.; Hamilson, J.P.; Daily, G.C. The impacts of nature experience on human cognitive function and mental health. Landsc. Urban Plan. 2015, 138, 41–50. [Google Scholar] [CrossRef]
- James, P.; Hart, J.E.; Banay, R.F.; Laden, F. Exposure to greenness and mortality in a nationwide prospective cohort study of women. Environ. Health Perspect. 2016, 124, 1344–1352. [Google Scholar] [CrossRef] [PubMed]
- Jiang, B.; Chang, C.-Y.; Sullivan, W.C. A dose of nature: Tree cover, stress reduction, and gender differences. Landsc. Urban Plan. 2014, 132, 26–36. [Google Scholar] [CrossRef]
- Li, Q. Effect of forest bathing trips on human immune function. Environ. Health Prev. Med. 2010, 15, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Ward Thompson, C.; Roe, J.; Aspinall, P.; Mitchell, R.; Clow, A.; Miller, D. More green space is linked to less stress in deprived communities: Evidence from salivary cortisol patterns. Landsc. Urban Plan. 2012, 105, 221–229. [Google Scholar] [CrossRef] [Green Version]
- Cetin, M.; Adiguzel, F.; Kaya, O.; Sahap, A. Mapping of bioclimatic comfort for potential planning using GIS in Aydin. Environ. Dev. Sustain. 2016. [Google Scholar] [CrossRef]
- Stigsdotter, U.K.; Palsdottir, A.M.; Burls, A.; Chermaz, A.; Ferrini, F.; Grahn, P. Nature-based therapeutic interventions. In Forest, Trees and Human Health; Nilsson, K., Sangster, M., Gallis, C., Hartig, T., de Vries, S., Seeland, K., Eds.; Springer: Dordrecht, The Netherlands, 2011; pp. 309–342. [Google Scholar]
- Lidwall, U.; Olsson-Bohlin, C. Lång väg tillbaka till arbete vid sjukskrivning, Psykiatriska diagnose. [Long way back to work when on sick leave, psychiatric diagnoses]. In Korta Analyser, Försäkringskassan; Avdelningen för Analys och Prognos: Stockholm, Sweden, 2017. [Google Scholar]
- Tyson, M.M. The Healing Landscape: Therapeutic Outdoor Environment; Parallel Press: Madison, WI, USA, 2007. [Google Scholar]
- Annerstedt, M.; Währborg, P. Nature assisted therapy: Systematic review of controlled and observational studies. Scand. J. Public Health 2011, 39, 371–388. [Google Scholar] [CrossRef] [PubMed]
- Blake, M.; Mitchell, G. Horticultural therapy in dementia care: A literature review. Nurs. Stand. 2016, 30, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Cipriani, J.; Benz, A.; Holmgren, A.; Kinter, D.; McGarry, J.; Rufino, G. A systematic review of the effects of horticultural therapy on persons with mental health conditions. Occup. Ther. Ment. Health 2017, 33, 47–69. [Google Scholar] [CrossRef]
- Clatworthy, J.; Hinds, J.; Camic, P.M. Gardening as a mental health intervention: A review. Ment. Health Rev. 2013, 18, 214–225. [Google Scholar] [CrossRef]
- Jang, E.J.; Han, G.W.; Hong, J.W.; Yoon, S.E.; Pak, C.H. Meta-analysis of research papers on horticultural therapy program effect. Korean J. Horticult. Sci. Technol. 2010, 28, 701–707. [Google Scholar]
- Kim, J.H.; Kwon, S.B.; Kim, H.J.; Choi, G.H.; Lee, H.M. Effects of horticultural therapy for the Korean elderly: A systematic literature review. J. Korean Biol. Nurs. Sci. 2016, 18, 153–159. [Google Scholar] [CrossRef]
- Kaplan, S. Meditation, restoration, and the management of mental fatigue. Environ. Behav. 2001, 33, 480–506. [Google Scholar] [CrossRef]
- Diamond, A. Executive functions. Annu. Rev. Psychol. 2013, 64, 135–168. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, S.; Berman, M.G. Directed attention as a common resource for executive functioning and self-regulation. Perspect. Psychol. Sci. 2010, 5, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.S. Biophilia, biophobia, and natural landscapes. In The Biophilia Hypothesis; Kellert, S.R., Wilson, E.O., Eds.; Shearwater Books: Washington, DC, USA, 1993; pp. 73–137. [Google Scholar]
- Grahn, P.; Tenngart Ivarsson, C.; Stigsdotter, U.K.; Bengtsson, I.-L. Using affordances as a health promoting tool in a therapeutic garden. In Innovative Approaches to Researching Landscape and Health; Ward Thompson, C., Aspinal, P., Bell, S., Eds.; Routledge: London, UK, 2010; pp. 116–154. [Google Scholar]
- Melchert, T.P. Biopsychosocial Practice; American Psychological Association: Washington, DC, USA, 2015. [Google Scholar]
- Grahn, P. Om stödjande miljöer och rofyllda ljud. [On supportive environments and serene sounds]. In Ljudmiljö, Hälsa Och Stadsbyggnad; Mossberg, F., Ed.; Ljudmiljöcentrum vid Lunds Universitet: Lund, Sweden, 2011; pp. 42–55. [Google Scholar]
- Adevi, A.A. Supportive Nature—And Stress. Wellbeing in Connection to Our Inner and Outer Landscape; Acta Universitatis Agriculturae Sueciae [Swedish University of Agricultural Sciences]: Alnarp, Sweden, 2012. [Google Scholar]
- Pálsdóttir, A.M. The Role of Nature in Rehabilitation for Individuals with Stress-Related Mental Disorders. Alnarp. Rehabilitation Garden as Supportive Environment; Acta Universitatis Agriculturae Sueciae [Swedish University of Agricultural Sciences]: Alnarp, Sweden, 2014. [Google Scholar]
- Stigsdotter, U.; Grahn, P. Experiencing a garden: A healing garden for people suffering from burnout diseases. J. Ther. Hort. 2003, 14, 38–49. [Google Scholar]
- Pálsdóttir, A.M.; Persson, D.; Persson, B.; Grahn, P. The journey of recovery and empowerment embraced by nature—Clients’ perspectives on nature-based rehabilitation in relation to the role of the natural environment. Int. J. Environ. Res. Public Health 2014, 11, 7094–7115. [Google Scholar]
- Gonzalez, M.T.; Hartig, T.; Patil, G.G.; Martinsen, E.W.; Kirkevold, M. Therapeutic horticulture in clinical depression: A prospective study. Res. Theory Nurs. Pract. 2009, 23, 312–328. [Google Scholar] [CrossRef] [PubMed]
- Pálsdóttir, A.M.; Grahn, P.; Persson, D. Changes in experienced value of everyday occupations after nature-based vocational rehabilitation. Scand. J. Occup. Ther. 2014, 21, 58–68. [Google Scholar]
- Poulsen, D.V.; Stigsdotter, U.K.; Djernis, D.; Sidenius, U. “Everything just seems much more right in nature”: How veterans with post-traumatic stress disorder experience nature-based activities in a forest therapy garden. Health Psychol. Open 2016, 3, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Sahlin, E.; Ahlborg, G., Jr.; Tenenbaum, A.; Grahn, P. Using nature-based rehabilitation to restart a stalled process of rehabilitation in individuals with stress-related mental illness. Int. J. Environ. Res. Public Health 2015, 12, 1928–1951. [Google Scholar] [CrossRef] [PubMed]
- Währborg, P.; Petersson, I.F.; Grahn, P. Nature-assisted rehabilitation for reactions to severe stress and/or depression in a rehabilitation garden: Long-term follow-up including comparisons with a matched population-based reference cohort. J. Rehab. Med. 2014, 46, 271–276. [Google Scholar]
- Kam, M.C.Y.; Siu, A.M.H. Evaluation of a horticultural activity programme for persons with psychiatric illness. Hong Kong J. Occup. Ther. 2010, 20, 80–86. [Google Scholar] [CrossRef]
- Nordh, H.; Grahn, P.; Währborg, P. Meaningful activities in the forest, a way back from exhaustion and long-term sick leave. Urban For. Urban Green. 2009, 8, 207–219. [Google Scholar] [CrossRef]
- Nyman, P. Experimentell Design Inom Samhällsvetenskapen. Available online: http://www.parnyman.com/files/texts/experiment.pdf (accessed on 29 May 2017). (In Swedish).
- Prvu Bettger, J.A.; Stineman, M.G. Effectiveness of multidisciplinary rehabilitation services in postacute care: State-of-the-science. A review. Arch. Phys. Med. Rehabil. 2007, 88, 1526–1534. [Google Scholar] [CrossRef] [PubMed]
- Craig, P.; Cooper, C.; Gunnell, D.; Haw, S.; Lawson, K.; Macintyre, S.; Ogilvie, D.; Petticrew, M.; Reeves, B.; Sutton, M.; et al. Using natural experiments to evaluate population health interventions: New Medical Research Council guidance. J. Epidemiol. Community Health 2012, 66, 1182–1186. [Google Scholar] [CrossRef] [PubMed]
- Hallberg, K.; Eno, J. Quasi-Experimental Designs. In International Encyclopedia of the Social & Behavioral Sciences, 2nd ed.; Wright, J., Ed.; Elsevier: Amsterdam, The Netherlands, 2015; pp. 742–746. [Google Scholar]
- Rockers, P.C.; Røttingen, J.-A.; Shemilt, I.; Tugwell, P.; Bärnighausen, T. Inclusion of quasi-experimental studies in systematic reviews of health systems research. Health Policy 2015, 119, 511–521. [Google Scholar] [CrossRef] [PubMed]
- Montori, V.M.; Guyatt, G.H. Intention-to-treat principle. CMAJ 2001, 165, 1339–1341. [Google Scholar] [PubMed]
- World Health Organization. ICD-10. International Statistical Classification of Diseases and Related Health Problems, 10th Revision, 2nd ed.; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Stigsdotter, U.; Grahn, P. What makes a garden a healing garden? J. Ther. Hortic. 2002, 13, 60–69. [Google Scholar]
- Orians, G.H. An ecological and evolutionary approach to landscape aesthetics. In Landscape Meanings and Values; Penning-Rowsell, E.C., Lowenthal, D., Eds.; Allen & Unwin: London, UK, 1986; pp. 3–25. [Google Scholar]
- Appleton, J. The Experience of Landscape; Wiley: London, UK, 1975. [Google Scholar]
- Coss, R.G. All that glistens: Water connotations in surface finishes. Ecol. Psychol. 1990, 2, 367–380. [Google Scholar] [CrossRef]
- Tenngart Ivarsson, C.; Hägerhäll, C.M. The perceived restorativeness of gardens—Assessing the restorativeness of a mixed built and natural scene type. Urban For. Urban Green. 2008, 7, 107–118. [Google Scholar] [CrossRef]
- Grahn, P.; Stigsdotter, U.K. The relation between perceived sensory dimensions of urban green space and stress restoration. Landsc. Urban Plan. 2010, 94, 264–275. [Google Scholar] [CrossRef]
- Kielhofner, G. A Model of Human Occupation: Theory and Application, 3rd ed.; Williams and Wilkins: Lippincott, PA, USA, 2002. [Google Scholar]
- Kielhofner, G.; Forsyth, K. Measurement properties of a client self-report for treatment planning and documenting occupational therapy outcomes. Scand. J. Occup. Ther. 2001, 8, 131–139. [Google Scholar]
- Pearlin, L.I.; Schooler, C. The structure of coping. J. Health Soc. Behav. 1978, 18, 2–21. [Google Scholar] [CrossRef]
- Pearlin, L.I.; Menaghan, E.G.; Lieberman, M.A.; Mullen, J.T. The stress process. J. Health Soc. Behav. 1981, 22, 337–356. [Google Scholar] [CrossRef] [PubMed]
- Bengtsson-Tops, A. Mastery in patients with schizophrenia living in the community. J. Psychiatr. Ment. Health Nurs. 2004, 11, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Boscarino, J.A.; Figley, C.R.; Adams, R.E. Compassion fatigue following the September 11 terrorist attacks: A study of secondary trauma among New York City social workers. Int. J. Emerg. Ment. Health 2004, 6, 57–66. [Google Scholar] [PubMed]
- Stephens, T.; Dulberg, C.; Joubert, N. Mental health of the Canadian population: A comprehensive analysis. Chronic Dis. Can. 2000, 20, 118–126. [Google Scholar]
- Nyqvist, F.; Forsman, A.K.; Cattan, M. A comparison of older workers’ and retired older people’s social capital and sense of mastery. Scand. J. Public Health 2013, 41, 792–798. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, M.; Lindström, B. Validity of Antonovsky’s sense of coherence scale: A systematic review. J. Epidemiol. Community Health 2005, 59, 460–466. [Google Scholar] [CrossRef] [PubMed]
- Ahola, A.J.; Saraheimo, M.; Forsblom, C.; Hietala, K.; Groop, P.-H. The cross-sectional associations between sense of coherence and diabetic microvascular complications, glycaemic control, and patients’ conceptions of type 1 diabetes. Health Qual. Life Outcomes 2010, 8, 142. [Google Scholar] [PubMed]
- Miles, J.; Shevlin, M. Applying Regression and Correlation; Sage: London, UK, 2001. [Google Scholar]
- Norman, G.R.; Streiner, D.L. Biostatistics: The Bare Essentials, 3rd ed.; BC Decker Inc.: Hamilton, ON, Canada, 2008. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Earlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Hedges, L.V. Distribution theory for Glass’ estimator of effect size and related estimators. J. Educ. Stat. 1981, 6, 107–128. [Google Scholar] [CrossRef]
- Sullivan, G.M.; Feinn, R. Using effect size—Or why the p value is not enough. J. Grad Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Shanahan, D.F.; Bush, R.; Gaston, K.J.; Lin, B.B.; Dean, J.; Barber, E.; Fuller, R.A. Health benefits from nature experiences depend on dose. Sci. Rep. 2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ottosson, J.; Grahn, P. The role of natural settings in crisis rehabilitation. Landsc. Res. 2008, 33, 51–70. [Google Scholar] [CrossRef]
- Beil, K.; Hanes, D. The influence of urban natural and built environments on physiological and psychological measures of stress. Int. J. Environ. Res. Public Health 2013, 10, 1250–1267. [Google Scholar] [CrossRef] [PubMed]
- Berto, R. The role of nature in coping with psycho-physiological stress: A literature review on restorativeness. Behav. Sci. 2014, 4, 394–409. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.S.; Simons, R.F.; Losito, B.D.; Fiorito, E.; Miles, M.A.; Zelson, M. Stress recovery during exposure to natural and urban environments. J. Environ. Psychol. 1991, 11, 201–230. [Google Scholar] [CrossRef]
- Bailey, C.E. Cognitive accuracy and intelligent executive function in the brain and in business. Ann. N. Y. Acad. Sci. 2007, 1118, 122–141. [Google Scholar] [CrossRef] [PubMed]
- Duncan, G.J.; Dowsett, C.J.; Claessens, A.; Magnuson, K.; Huston, A.C.; Klebanov, P.; Pagani, L.S.; Feinstein, L.; Engel, M.; Brooks-Gunn, J.; et al. School readiness and later achievement. Dev. Psychol. 2007, 43, 1428–1446. [Google Scholar] [CrossRef] [PubMed]
- Berman, M.G.; Kross, E.; Krpan, K.M.; Askren, M.K.; Burson, A.; Deldin, P.J.; Kaplan, S.; Sherdell, L.; Gotlib, I.H.; Jonides, J. Interacting with nature improves cognition and affect for individuals with depression. J. Affect. Disord. 2012, 140, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.E.; Williams, K.J.H.; Sargent, L.D.; Williams, N.S.G.; Johnson, K.A. 40-second green roof views sustain attention: The role of micro-breaks in attention restoration. J. Environ. Psychol. 2015, 42, 182–189. [Google Scholar] [CrossRef]
- Ohly, H.; White, M.P.; Wheeler, B.W.; Bethel, A.; Ukoumunne, O.C.; Nikolaou, V.; Garside, R. Attention restoration theory: A systematic review of the attention restoration potential of exposure to natural environments. J. Toxicol. Environ. Health B 2016. [Google Scholar] [CrossRef] [PubMed]
- Berman, M.G.; Jonides, J.; Kaplan, S. The cognitive benefits of interacting with nature. Psychol. Sci. 2008, 19, 1207–1212. [Google Scholar] [CrossRef] [PubMed]
- Ottosson, J.; Grahn, P. A comparison of leisure time spent in a garden with leisure time spent indoors: On measures of restoration in residents in geriatric care. Landsc. Res. 2005, 30, 23–55. [Google Scholar] [CrossRef]
- Kaplan, S. Parks for the future–A psychologist view. In Parks for the Future; Sorte, G.J., Ed.; Movium: Alnarp, Sweden, 1990; pp. 4–22. [Google Scholar]
- Grahn, P.; Ottosson, Å. Trädgårdsterapi Alnarpsmetoden: Att Ta Hjälp Av Naturen Vid Stress Och Utmattning; Bonnier Existens: Stockholm, Sweden, 2010. [Google Scholar]
- Sahlin, E.; Matuszczyk, J.V.; Ahlborg, G., Jr.; Grahn, P. How do participants in nature-based therapy experience and evaluate their rehabilitation? J. Ther. Hortic. 2012, 22, 8–22. [Google Scholar]
- Schaufeli, W.B.; Leiter, M.P.; Maslach, C. Burnout: 35 years of research and practice. Career Dev. Int. 2009, 14, 204–220. [Google Scholar] [CrossRef]
- Andrews, K. The limitations of randomized controlled trials in rehabilitation research. Clin. Rehabil. 1991, 5, 5–8. [Google Scholar] [CrossRef]
- Graham, J.E.; Karmarkar, A.M.; Ottenbacher, K.J. Small sample research designs for evidence-based rehabilitation: Issues and methods. Arch. Phys. Med. Rehabil. 2012, 93, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Hart, T.; Whyte, J.; Poulsen, I.; Spangsberg Kristensen, K.; Nordenbo, A.M.; Chervoneva, I.; Vaccaro, M.J. How do intensity and duration of rehabilitation services affect outcomes from severe traumatic brain injury? A natural experiment comparing health care delivery systems in 2 developed nations. Arch. Phys. Med. Rehabil. 2016, 97, 2045–2053. [Google Scholar] [CrossRef] [PubMed]

| 8 Weeks | 12 Weeks | 24 Weeks | |
|---|---|---|---|
| n | 44 | 48 | 14 |
| Mean period (range) | 7.8 (4.0–9.4) | 13.4 (10.0–17.0) | 23.2 (18.0–29.8) |
| Mean age | 46.3 | 45.7 | 44.1 |
| Sex F/M | 39/5 | 43/5 | 14/0 |
| Marital status: Married or living with another adult/Single | 30/14 | 32/16 | 8/6 |
| Socioeconomic status | 2.82 | 2.61 | 3.22 |
| Time on sick leave (year) | 3.68 | 3.71 | 3.82 |
| Primary Diagnosis F43/F32 | 30/14 | 34/14 | 13/1 |
| Additional consultation (%) | 8 (18) | 10 (21) | 3 (21) |
| Percent | Paid Work (%) | Job Training (%) | Customized Job Training (%) | Combined (Paid Work, Job Training, and Customized Job Training) (%) |
|---|---|---|---|---|
| 0 | 53 (55.8) | 78 (82.1) | 89 (93.7) | 30 (31.6) |
| 25 | 8 (8.4) | 7 (7.3) | 1 (1.0) | 16 (16.8) |
| 50 | 11 (11.6) | 5 (5.3) | 3 (3.2) | 19 (20.0) |
| 75 | 9 (9.5) | 0 (0.0) | 0 (0.0) | 9 (9.5) |
| 100 | 14 (14.7) | 5 (5.3) | 2 (2.1) | 21 (22.1) |
| Rehabilitation Period | 8 Weeks | 12 Weeks | 24 Weeks | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | n | Mean Start–End | Diff | ES (Magn.) | t | p | n | Mean Start–End | Diff | ES (Magn.) | t | p | n | Mean Start–End | Diff | ES (Magn.) | t | p |
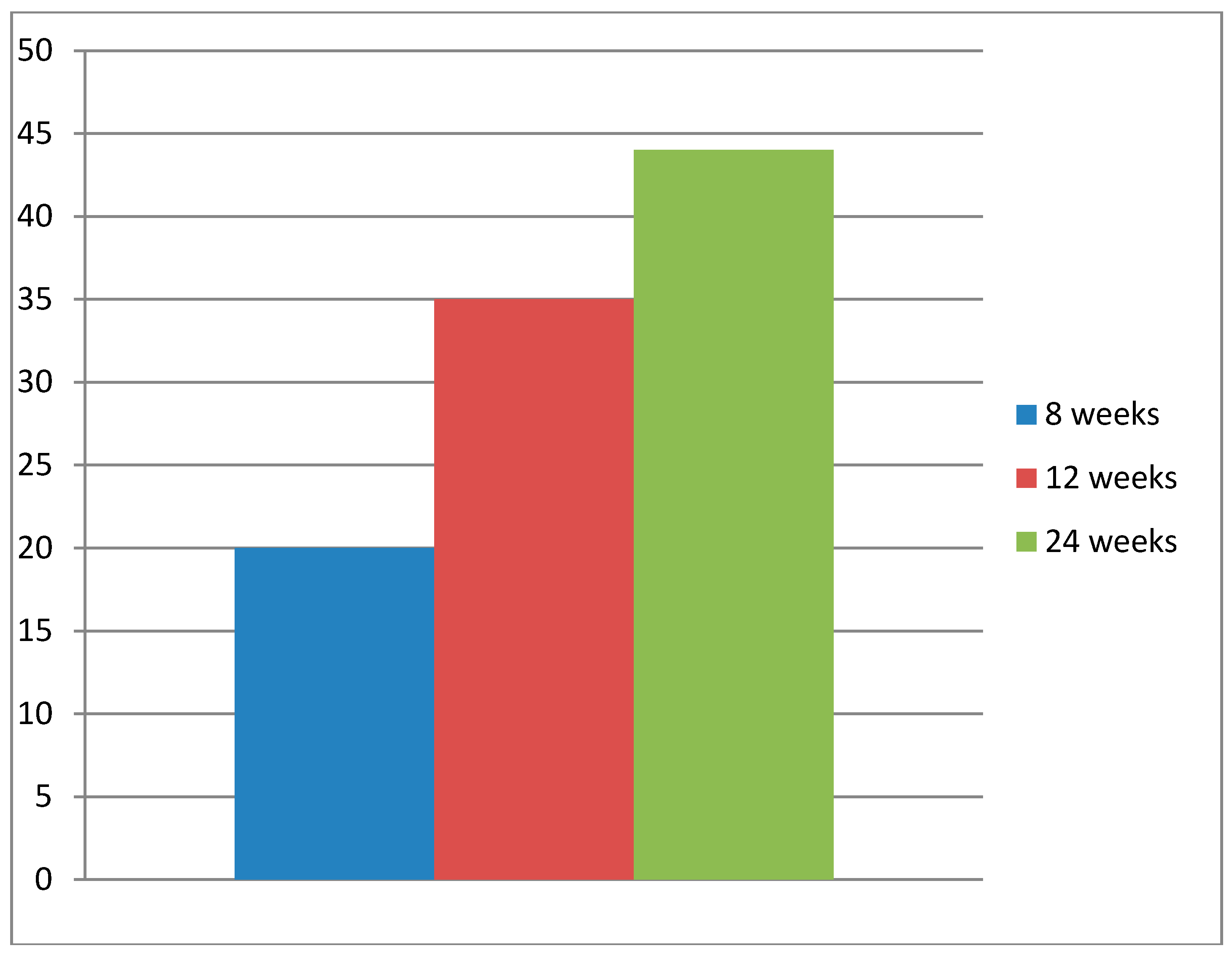
| RTW | 40 | 0–20.0 | 20.0 | 0.85 (H) | 3.77 | <0.001 | 43 | 0.0–34.9 | 34.9 | 1.22 (H) | 5.65 | <0.0001 | 12 | 0.0–43.8 | 43.8 | 1.49 (H) | 3.66 | <0.01 |
| OSA | 34 | 36.5–41.5 | 5.0 | 0.64 (M) | 4.22 | <0.001 | 37 | 36.8–44.9 | 8.1 | 1.07 (H) | 6.23 | <0.0001 | 10 | 35.4–44.9 | 9.5 | 1.46 (H) | 3.34 | <0.01 |
| Mastery | 36 | 17.0–20.0 | 3.0 | 0.67 (M) | 4.94 | <0.0001 | 40 | 17.5–20.7 | 3.2 | 0.70 (M) | 4.98 | <0.0001 | 12 | 18.5–21.7 | 3.2 | 0.68 (M) | 3.01 | =0.01 |
| SoC | 34 | 47.2–54.8 | 7.6 | 0.60 (M) | 3.84 | <0.001 | 37 | 46.7–59.7 | 13.0 | 1.10 (H) | 6.28 | <0.0001 | 10 | 49.8–59.1 | 9.3 | 0.56 (M) | 2.67 | <0.05 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grahn, P.; Pálsdóttir, A.M.; Ottosson, J.; Jonsdottir, I.H. Longer Nature-Based Rehabilitation May Contribute to a Faster Return to Work in Patients with Reactions to Severe Stress and/or Depression. Int. J. Environ. Res. Public Health 2017, 14, 1310. https://doi.org/10.3390/ijerph14111310
Grahn P, Pálsdóttir AM, Ottosson J, Jonsdottir IH. Longer Nature-Based Rehabilitation May Contribute to a Faster Return to Work in Patients with Reactions to Severe Stress and/or Depression. International Journal of Environmental Research and Public Health. 2017; 14(11):1310. https://doi.org/10.3390/ijerph14111310
Chicago/Turabian StyleGrahn, Patrik, Anna María Pálsdóttir, Johan Ottosson, and Ingibjörg H. Jonsdottir. 2017. "Longer Nature-Based Rehabilitation May Contribute to a Faster Return to Work in Patients with Reactions to Severe Stress and/or Depression" International Journal of Environmental Research and Public Health 14, no. 11: 1310. https://doi.org/10.3390/ijerph14111310




