The Trends in Cardiovascular Diseases and Respiratory Diseases Mortality in Urban and Rural China, 1990–2015
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Statistical Analysis
3. Results
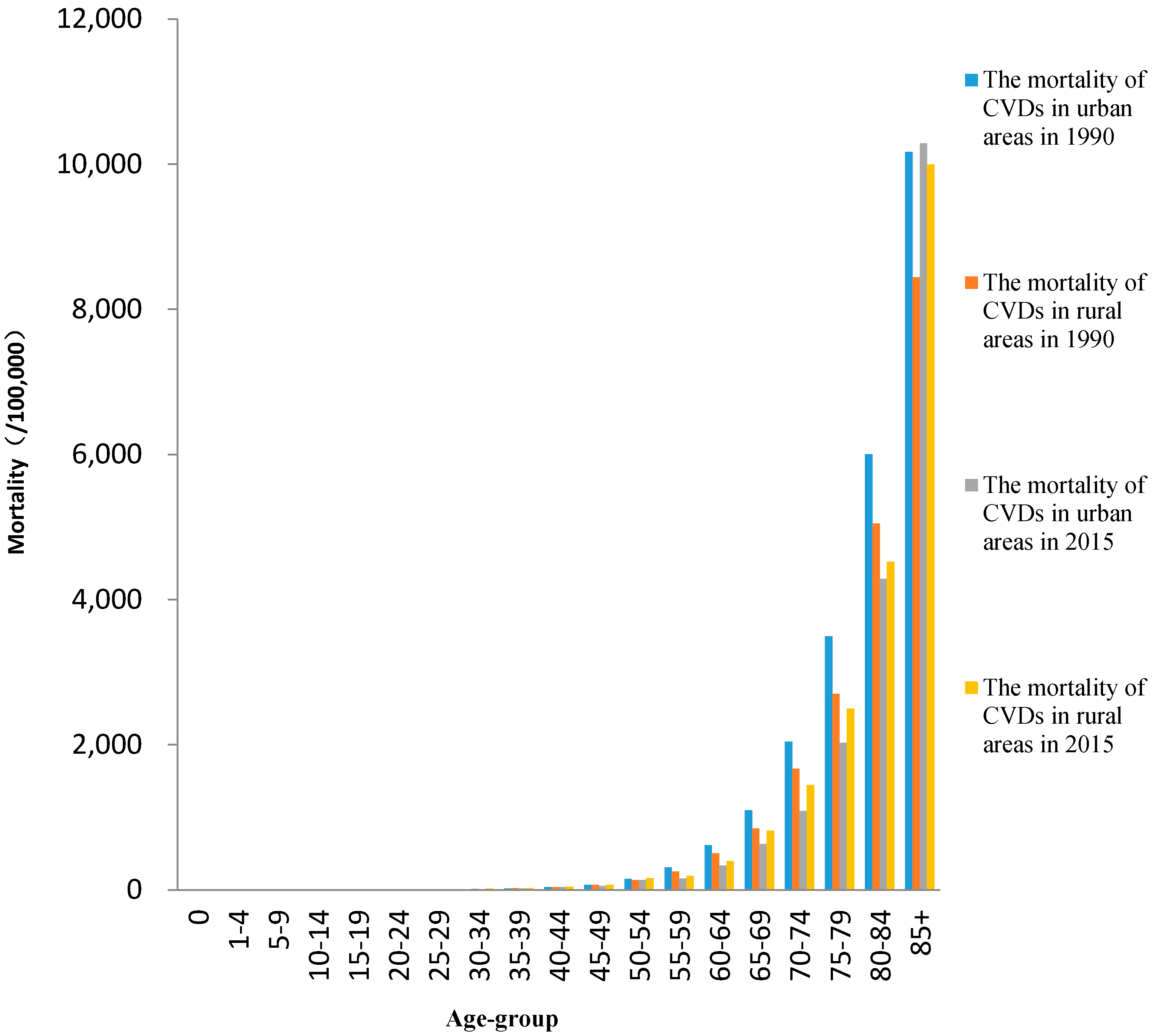
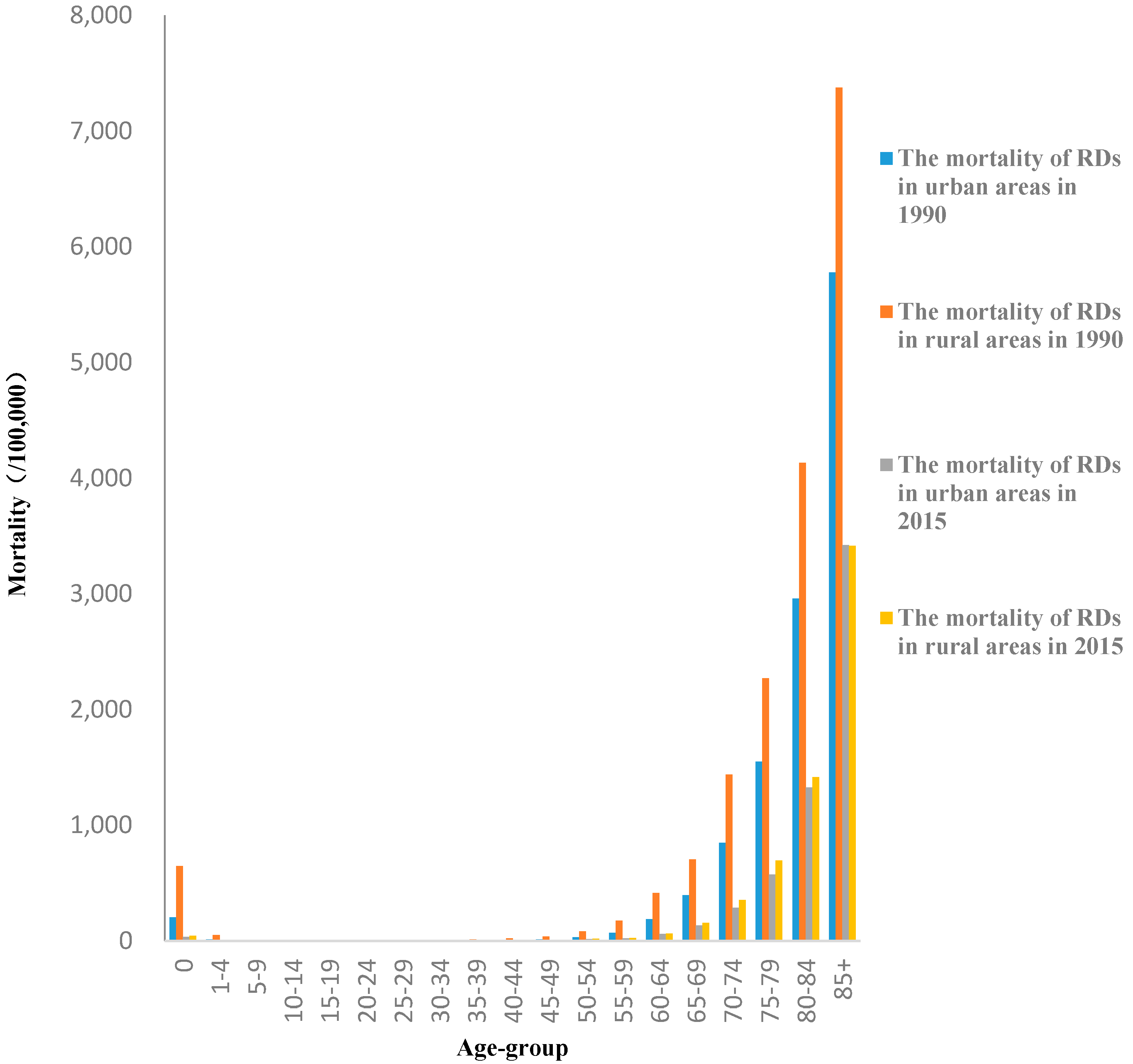
3.1. Trends in Mortality Rates
3.2. YLLs and Age-Standardized YLL Rates
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Murray, C.J.L.; Barber, R.M.; Foreman, K.J.; Ozgoren, A.A.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Abraham, J.P.; Abubakar, I.; Abu-Raddad, L.J.; et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: Quantifying the epidemiological transition. Lancet 2015, 386, 2145–2191. [Google Scholar] [CrossRef]
- Wang, H.; Naghavi, M.; Allen, C.; Barber, R.M.; Bhutta, Z.A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; Coates, M.M.; et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef] [Green Version]
- National Health and Family Planning Commission. China Health and Family Planning Statistics Yearbook; Beijing Union Medical University Press: Beijing, China, 2016.
- Noncommunicable Diseases Country Profiles. Available online: http://www.who.int/nmh/countries/en/#C (accessed on 30 August 2017).
- Naghavi, M.; Wang, H.D.; Lozano, R.; Davis, A.; Liang, X.F.; Zhou, M.G.; Vollset, S.E.; Ozgoren, A.A.; Abdalla, S.; Abd-Allah, F.; et al. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the global burden of disease study 2013. Lancet 2015, 385, 117–171. [Google Scholar]
- Krishnamurthi, R.V.; Feigin, V.L.; Forouzanfar, M.H.; Mensah, G.A.; Connor, M.; Bennett, D.A.; Moran, A.E.; Sacco, R.L.; Anderson, L.M.; Truelsen, T.; et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990–2010: Findings from the global burden of disease study 2010. Lancet Glob. Health 2013, 1, E259–E281. [Google Scholar] [CrossRef]
- Soriano, J.B.; Abajobir, A.A.; Abate, K.H.; Abera, S.F.; Agrawal, A.; Ahmed, M.B.; Aichour, A.N.; Aichour, I.; Aichour, M.T.E.; Alam, K.; et al. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: A systematic analysis for the global burden of disease study 2015. Lancet Respir. Med. 2017, 5, 691–706. [Google Scholar] [CrossRef]
- Du, S.F.; Lu, B.; Zhai, F.Y.; Popkin, B.M. A new stage of the nutrition transition in China. Public Health Nutr. 2002, 5, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Tzoulaki, I.; Elliott, P.; Kontis, V.; Ezzati, M. Worldwide exposures to cardiovascular risk factors and associated health effects: Current knowledge and data gaps. Circulation 2016, 133, 2314–2333. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, A. Environmental determinants of cardiovascular disease. Circ. Res. 2017, 121, 162–180. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Hong, C.; Kan, H. Exposures and health outcomes from outdoor air pollutants in China. Toxicology 2004, 198, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Shang, Y.; Sun, Z.; Cao, J.; Wang, X.; Zhong, L.; Bi, X.; Li, H.; Liu, W.; Zhu, T.; Huang, W. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ. Int. 2013, 54, 100–111. [Google Scholar] [CrossRef] [PubMed]
- National Bureau of Statistics of People’s Republic of China. Chinese Sixth Population Census. Available online: http://www.stats.gov.cn/tjsj/tjgb/ndtjgb/index.htm (accessed on 30 August 2017).
- Murray, C.J.L.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef]
- World Health Organization. National Burden of Disease Studies: A Practical Guide; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Hu, S.; Tang, S.; Liu, Y.; Zhao, Y.; Escobar, M.L.; de Ferranti, D.; Wagstaff, A.; Lindelow, M. Reform of how health care is paid for in China: Challenges and opportunities. Lancet 2009. [Google Scholar] [CrossRef]
- Moran, A.; Gu, D.F.; Zhao, D.; Coxson, P.; Wang, Y.C.; Chen, C.S.; Liu, J.; Cheng, J.; Bibbins-Domingo, K.; Shen, Y.M.; et al. Future cardiovascular disease in China markov model and risk factor scenario projections from the coronary heart disease policy Model-China. Circ. Cardiovasc. Qual. 2010, 3, 243–252. [Google Scholar] [CrossRef] [PubMed]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the global burden of disease study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
- Weiwei, C.; Runlin, G.; Lisheng, L.; Manlu, Z.; Wen, W.; Yongjun, W.; Zhaosu, W.; Huijun, L.; Zhe, Z.; Lixin, J.; et al. Outline of the report on cardiovascular diseases in China, 2016. Chin. Circ. J. 2017, 32, 521–530. [Google Scholar]
- Department of Population and Employment Statistics of the National Bureau of Statistics of China. China Population and Employment Statistics Yearbook; China Statistics Press: Beijing, China, 2016.
- Zhou, M.G.; Wang, H.D.; Zhu, J.; Chen, W.Q.; Wang, L.H.; Liu, S.W.; Li, Y.C.; Wang, L.J.; Liu, Y.N.; Yin, P.; et al. Cause-specific mortality for 240 causes in China during 1990–2013: A systematic subnational analysis for the global burden of disease study 2013. Lancet 2016, 387, 251–272. [Google Scholar] [CrossRef]
- Liu, Y.; Rao, K.; Wu, J.; Gakidou, E. China’s health system performance. Lancet 2008, 372, 1914–1923. [Google Scholar] [CrossRef]
- Jiang, G.; Wang, D.; Li, W.; Pan, Y.; Zheng, W.; Zhang, H.; Sun, Y.V. Coronary heart disease mortality in China: Age, gender, and urban-rural gaps during epidemiological transition. Rev. Panam. Salud Publica 2012, 31, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Mingbao, L.; Wen, W.; Maigeng, Z. Analysis of trends and characteristics of mortality of ischemic heart disease over the age of 35 years old in China, 2004–2011. Chin. J. Prev. Med. 2014. [Google Scholar] [CrossRef]
- Nowbar, A.N.; Howard, J.P.; Finegold, J.A.; Asaria, P.; Francis, D.P. 2014 global geographic analysis of mortality from ischaemic heart disease by country, age and income: Statistics from World Health Organisation and United Nations. Int. J. Cardiol. 2014, 174, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Thaker, A.M.; Frishman, W.H. Sortilin the mechanistic link between genes, cholesterol, and coronary artery disease. Cardiol. Rev. 2014, 22, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Roerecke, M.; Rehm, J. Irregular heavy drinking occasions and risk of ischemic heart disease: A systematic review and meta-analysis. Am. J. Epidemiol. 2010, 171, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Georgiopoulou, V.V.; Kalogeropoulos, A.P.; Raggi, P.; Butler, J. Prevention, diagnosis, and treatment of hypertensive heart disease. Cardiol. Clin. 2010, 28, 675–691. [Google Scholar] [CrossRef] [PubMed]
- Zhaokang, Y.; Yuxi, L.; Yong, L.; Yunchang, X.; Yuanjun, G.; Harris, M. A model for community health service development in depressed rural areas in China. BMC Health Serv. Res. 2012, 12, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Hu, T.W.; Mao, Z.; Liu, Y.; de Beyer, J.; Ong, M. Smoking, standard of living, and poverty in China. Tob. Control. 2005, 14, 247–250. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Gu, H.; Teo, K.K.; Bo, J.; Wang, Y.; Yang, J.; Wang, X.; Zhang, H.; Sun, Y.; Jia, X.; et al. ypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47,000 people from China. J. Hypertens. 2016, 34, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.S.; Liu, Y.; Zhu, Z.J.; Li, Z.G. Does where you live matter to your health? Investigating factors that influence the self-rated health of urban and rural Chinese residents: Evidence drawn from Chinese general social survey data. Health Qual. Life Outcomes 2017, 15, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Bobak, M.; Pikhart, H.; Pajak, A.; Kubinova, R.; Malyutina, S.; Sebakova, H.; Topor-Madry, R.; Nikitin, Y.; Marmot, M. Depressive symptoms in urban population samples in Russia, Poland and the Czech Republic. Br. J. Psychiatry 2006, 188, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Leinsalu, M.; Stirbu, I.; Vagero, D.; Kalediene, R.; Kovacs, K.; Wojtyniak, B.; Wroblewska, W.; Mackenbach, J.P.; Kunst, A.E. Educational inequalities in mortality in four Eastern European countries: Divergence in trends during the post-communist transition from 1990 to 2000. Int. J. Epidemiol. 2009, 38, 512–525. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Surveillance, Prevention and Control of Chronic Respiratory Diseases: A Comprehensive Approach; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- National Center for Cardiovascular Diseases, China. Report on Cardiovascular Disease in China 2016; Encyclopedia of China Publishing House: Beijing, China, 2017. [Google Scholar]
- Chen, Z. Launch of the health-care reform plan in China. Lancet 2009, 373, 1322–1324. [Google Scholar] [CrossRef]
- Mackay, J. China: The tipping point in tobacco control. Br. Med. Bull. 2016, 120, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Mandel, J.H.; Wendt, C.; Lo, C.; Zhou, G.; Hertz, M.; Ramachandran, G. Ambient air pollution and lung disease in China: Health effects, study design approaches and future research. Front. Med. 2015, 9, 392–400. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Q.; Wu, Z.T.; Jiang, G.H.; Wu, X.Y.; Li, P.; Ni, Y.; Xiong, X.Q.; Wang, X.Y.; Li, G.; Pan, X.; et al. The association between ambient inhalable particulate matter and the disease burden of respiratory disease: An ecological study based on ten-year time series data in Tianjin, China. Environ. Res. 2017, 157, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Maji, K.J.; Arora, M.; Dikshit, A.K. Burden of disease attributed to ambient PM2.5 and PM10 exposure in 190 cities in China. Environ. Sci. Pollut. Res. Int. 2017, 24, 11559–11572. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.N.; Minino, A.M.; Hoyert, D.L.; Rosenberg, H.M. Comparability of cause of death between ICD-9 and ICD-10: Preliminary estimates. Natl. Vital. Stat. Rep. 2001, 49, 1–32. [Google Scholar] [PubMed]
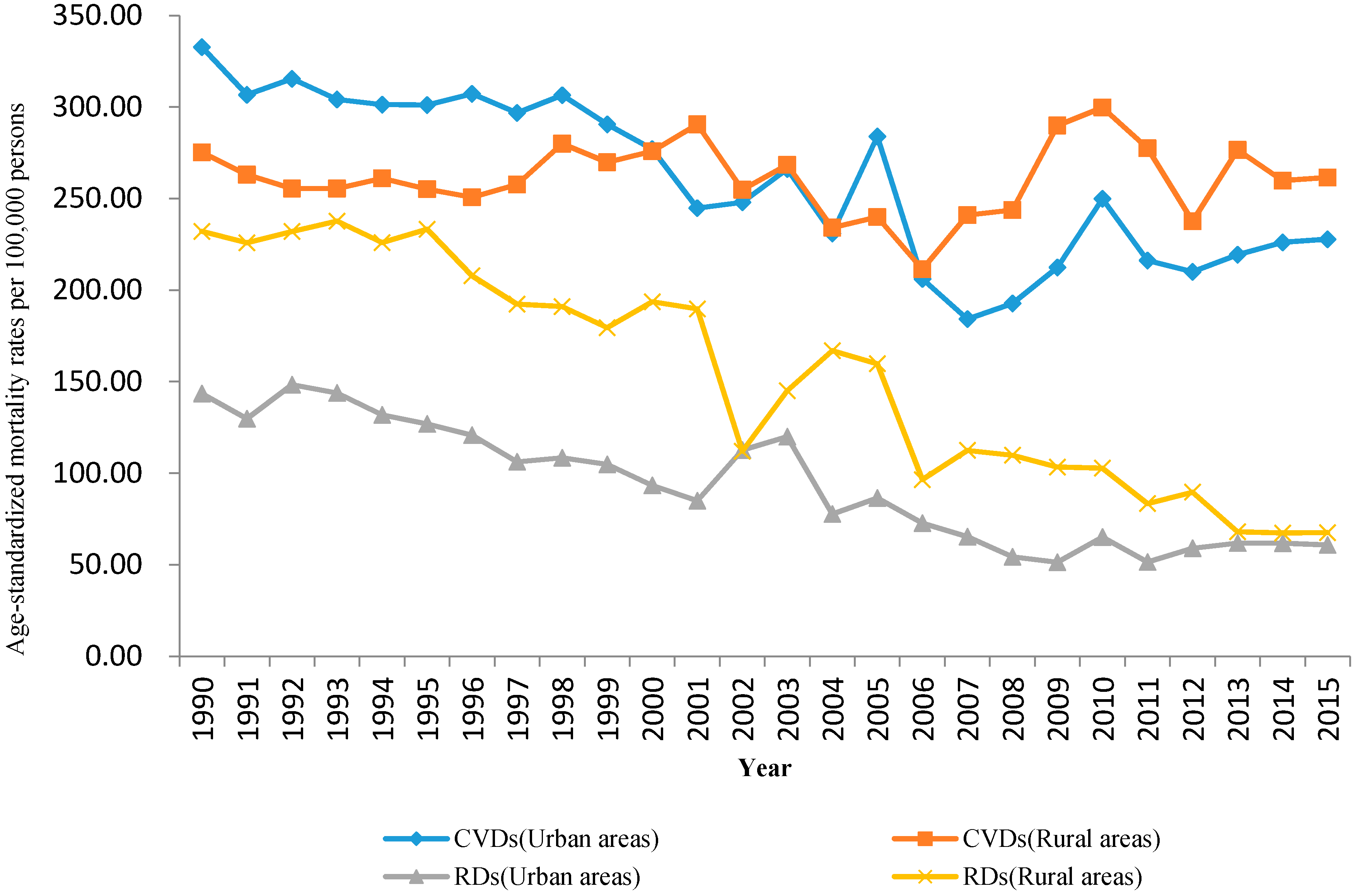
| Mortality Rate (per 100,000) | Total Study Period b | Period 1 | Period 2 | Period 3 | Period 4 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2015 | Average APC (%) | 95% CI | Years | APC (%) | Years | APC (%) | Years | APC (%) | Years | APC (%) | |
| CVDs in urban areas | 332.7 | 227.7 | −1.9 c | (−2.4, −1.4) | - | |||||||
| Chronic rheumatic heart diseases | 10.4 | 2.7 | −6.1 c | (−6.9, −5.2) | 1990–2011 | −7.2 c | 2011–2015 | 8.3 | ||||
| Hypertensive heart disease | 8.3 | 10.8 | 1.3 | (−0.3, 2.9) | 1990–2007 | −1.6 | 2007–2015 | 10.6 c | ||||
| Ischemic heart disease | 29.1 | 47.3 | 0.8 | (−0.2, 1.9) | 1990–1998 | 3.3 | 1998–2006 | −5.4 c | 2006–2015 | 8.5 c | ||
| Cerebrovascular disease | 181.1 | 107.2 | −2.8 c | (−3.4, −2.2) | 1990–2008 | −3.7 c | 2008–2015 | 0.8 | ||||
| CVDs in rural areas | 275.2 | 261.4 | 0.0 | (−0.5, 0.4) | 1990–2001 | 0.7 | 2001–2006 | −4.6 | 2006–2009 | 9.19 | 2009–2015 | −1.71 |
| Chronic rheumatic heart diseases | 10.8 | 2.9 | −5.9 c | (−6.8, −5.1) | - | |||||||
| Hypertensive heart disease | 9.9 | 16.5 | 1.0 | (−0.9, 2.9) | 1990–2006 | −3.2 c | 2006–2015 | 11.2 c | ||||
| Ischemic heart disease | 18.7 | 60.0 | 5.2 c | (3.7, 6.7) | 1990–2000 | 4.1 c | 2000–2005 | −8.2 | 2005–2008 | 37.0 | 2008–2015 | 5.7 |
| Cerebrovascular disease | 159.5 | 131.6 | −0.6 c | (−1.1, −0.2) | - | |||||||
| RDs in urban areas | 143.5 | 60.7 | −4.2 c | (−4.9, −3.5) | 1990–2005 | −3.5 c | 2005–2008 | −14.4 | 2008–2015 | 1.9 | ||
| Chronic lower respiratory diseases | 117.9 | 44.0 | −5.6 c | (−6.7, −4.6) | - | |||||||
| Pneumonia | 13.9 | 11.7 | 0.0 | (−1.0, 1.0) | 1990–2005 | −2.7 c | 2005–2015 | 5.0 | ||||
| Pneumoconiosis | 0.8 | 0.6 | −2.3 c | (−3.4, −1.1) | - | |||||||
| RDs in rural areas | 232.1 | 67.5 | −5.3 c | (−6.0, −4.5) | - | |||||||
| Chronic lower respiratory diseases | 199.0 | 56.3 | −5.3 c | (−6.0, −4.5) | - | |||||||
| Pneumonia | 24.2 | 7.5 | −5.6 c | (−6.7, −4.5) | 1990–2000 | −2.5 c | 2000–2003 | 21.7 | 2003–2015 | −1.4 | ||
| Pneumoconiosis | 0.5 | 0.5 | 0.9 | (−1.1, 3.0) | - | |||||||
| Age Group | CVDs in Urban Areas | CVDs in Rural Areas | RDs in Urban Areas | RDs in Rural Areas | ||||
|---|---|---|---|---|---|---|---|---|
| Average APC (%) | 95% CI | Average APC (%) | 95% CI | Average APC (%) | 95% CI | Average APC (%) | 95% CI | |
| 0 | 3.7 a | (0.4, 7.2) | 6.4 a | (2.5, 10.4) | −7.4 a | (−9.1, −5.8) | −13.6 a | (−15.4, −11.5) |
| 1–4 | 3.8 a | (1.6, 6.0) | 3.8 a | (1.1, 6.6) | −3.2 a | (−4.5, −1.8) | −9.1 a | (−11.1, −7.1) |
| 5–9 | 1.4 | (−0.6, 3.4) | 1.3 | (−0.8, 3.5) | −3.6 a | (−5.0, −2.1) | −10.9 a | (−13.7, −8.0) |
| 10–14 | 0.6 | (−0.9, 2.0) | 1.6 | (−0.0, 3.3) | −1.9 a | (−3.6, −0.1) | −9.9 a | (−12.8, −6.9) |
| 15–19 | 2.2 | (1.1, 3.3) | 0.9 | (−0.9, 2.7) | −1.2 | (−2.9, 0.5) | −5.8 a | (−9.1, −2.3) |
| 20–24 | 0.1 | (−0.9, 1.2) | −2.0 a | (−3.3, −0.6) | −2.4 a | (−3.9, 0.8) | −7.0 a | (−8.8, −5.1) |
| 25–29 | −0.2 | (−0.8, 0.5) | −1.8 a | (−3.4, −0.1) | −2.1 a | (−3.0, −1.1) | −8.0 a | (−10.2, −5.7) |
| 30–34 | −0.1 | (−0.8, 0.6) | −1.1 | (−2.7, 0.6) | −3.0 a | (−3.9, −2.0) | −7.4 a | (−9.4, −5.4) |
| 35–39 | −0.5 a | (−0.5, −0.0) | −0.0 | (−0.7, 0.6) | −3.4 a | (−4.3, −2.5) | −6.7 a | (−7.9, −5.4) |
| 40–44 | −0.4 | (−0.9, 0.1) | −0.1 | (−0.8, 0.7) | −3.4 a | (−4.1, −2.6) | −7.2 a | (−8.5, −5.7) |
| 45–49 | −1.3 a | (−2.0, −0.6) | −1.2 a | (−2.4, −0.1) | −3.6 a | (−4.5, −2.7) | −8.1 a | (−9.6, −6.5) |
| 50–54 | −1.0 a | (−1.7, −0.4) | −0.8 a | (−1.5, −0.1) | −3.3 a | (−4.3, −2.4) | −7.7 a | (−8.9, −6.6) |
| 55–59 | −2.6 a | (−3.2, −2.1) | −0.9 a | (−1.4, −0.5) | −4.6 a | (−5.5, −3.6) | −7.6 a | (−8.8, −6.5) |
| 60–64 | −3.4 a | (−4.2, −2.5) | −1.6 a | (−2.1, −1.0) | −5.7 a | (−6.8, −4.6) | −8.1 a | (−9.2, −7.1) |
| 65–69 | −3.3 a | (−4.1, −2.5) | −0.9 a | (−1.6, −0.3) | −5.6 a | (−6.6, −4.5) | −7.1 a | (−8.1, −6.0) |
| 70–74 | −3.1 a | (−3.8, −2.5) | −1.2 a | (−1.8, −0.6) | −5.5 a | (−6.4, −4.6) | −6.6 a | (−7.5, −5.7) |
| 75–79 | −2.3 a | (−2.8, −1.9) | −0.0 | (−0.5, 0.5) | −4.7 a | (−5.5, −4.0) | −5.1 a | (−5.9, −4.3) |
| 80–84 | −1.5 a | (−2.0, −1.1) | 0.4 | (−0.1, 0.9) | −4.0 a | (−4.7, −3.3) | −4.3 a | (−5.0, −3.6) |
| 85+ | 0.0 | (−0.6, 0.7) | 2.2 a | (1.2, 3.2) | −2.7 a | (−3.3, −2.2) | −2.4 a | (−3.2, −1.5) |
| YLLs (10,000) | Age-Standardized YLL Rate (per 100,000) | |||||
|---|---|---|---|---|---|---|
| 1990 | 2015 | Percent Change (%), 1990–2015 | 1990 | 2015 | Percent Change (%), 1990–2015 | |
| CVDs in urban areas | 800.9 | 2385.6 | 197.9 | 4365.6 | 2828.4 | −35.2 |
| Chronic rheumatic heart disease | 50.9 | 34.4 | −32.4 | 234.1 | 40.7 | −82.6 |
| Hypertensive heart disease | 16.0 | 95.7 | 498.1 | 93.9 | 113.5 | 20.9 |
| Ischemic heart disease | 166.7 | 919.0 | 451.3 | 920.4 | 1085.7 | 18.0 |
| Cerebrovascular disease | 428.3 | 1144.7 | 167.3 | 2369.5 | 1359.1 | −42.6 |
| CVDs in rural areas | 1983.3 | 2656.8 | 34.0 | 3745.4 | 3434.3 | −8.3 |
| Chronic rheumatic heart disease | 152.5 | 34.4 | −77.4 | 252.3 | 45.5 | −82.0 |
| Hypertensive heart disease | 60.3 | 139.7 | 131.7 | 118.8 | 175.0 | 47.3 |
| Ischemic heart disease | 281.0 | 941.4 | 235.0 | 524.5 | 1221.4 | 132.9 |
| Cerebrovascular disease | 1069.9 | 1366.3 | 27.7 | 2069.5 | 1754.6 | −15.2 |
| RDs in urban areas | 371.0 | 532.5 | 43.5 | 1790.4 | 640.5 | −64.2 |
| Chronic lower respiratory disease | 226.8 | 361.8 | 59.5 | 1317.5 | 432.4 | −67.2 |
| Pneumonia | 117.6 | 120.0 | 2.0 | 337.1 | 147.4 | −56.3 |
| Pneumoconiosis | 2.5 | 5.6 | 124.0 | 12.8 | 6.8 | −46.9 |
| RDs in rural areas | 2783.0 | 590.9 | −78.8 | 3571.0 | 751.5 | −79.0 |
| Chronic lower respiratory disease | 1299.8 | 457.9 | −64.8 | 2511.4 | 568.1 | −77.4 |
| Pneumonia | 1420.1 | 88.1 | −93.8 | 937.7 | 121.5 | −87.0 |
| Pneumoconiosis | 5.3 | 7.7 | 45.3 | 10.1 | 10.5 | 4.0 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, W.; Zhou, Y.; Zhang, Z.; Cao, L.; Chen, W. The Trends in Cardiovascular Diseases and Respiratory Diseases Mortality in Urban and Rural China, 1990–2015. Int. J. Environ. Res. Public Health 2017, 14, 1391. https://doi.org/10.3390/ijerph14111391
Sun W, Zhou Y, Zhang Z, Cao L, Chen W. The Trends in Cardiovascular Diseases and Respiratory Diseases Mortality in Urban and Rural China, 1990–2015. International Journal of Environmental Research and Public Health. 2017; 14(11):1391. https://doi.org/10.3390/ijerph14111391
Chicago/Turabian StyleSun, Weiwei, Yun Zhou, Zhuang Zhang, Limin Cao, and Weihong Chen. 2017. "The Trends in Cardiovascular Diseases and Respiratory Diseases Mortality in Urban and Rural China, 1990–2015" International Journal of Environmental Research and Public Health 14, no. 11: 1391. https://doi.org/10.3390/ijerph14111391





