A Meta-Analysis of Risk Factors for Post-Traumatic Stress Disorder (PTSD) in Adults and Children after Earthquakes
Abstract
:1. Introduction
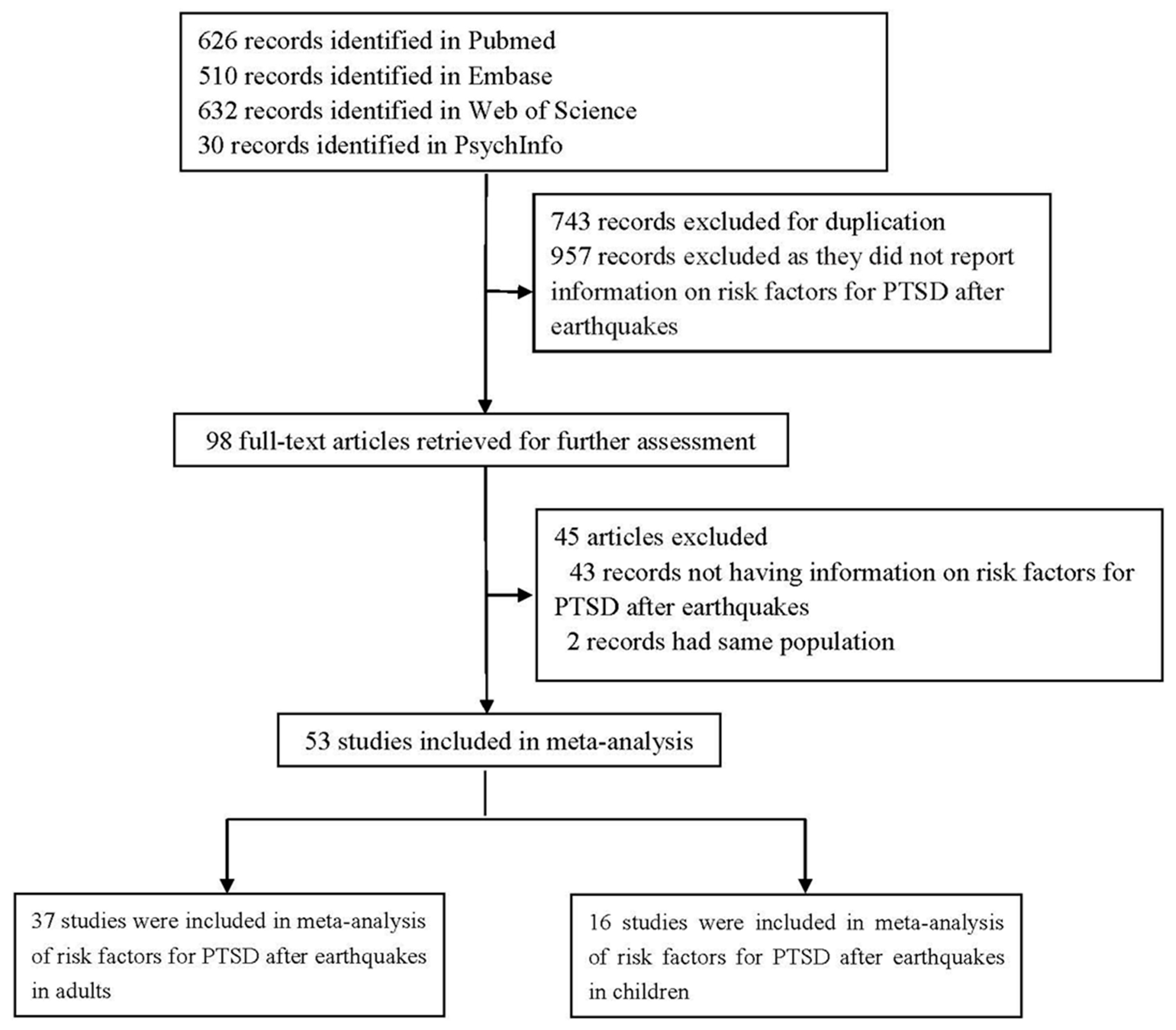
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Quality Assessment
2.4. Classification of Risk Factors
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Studies
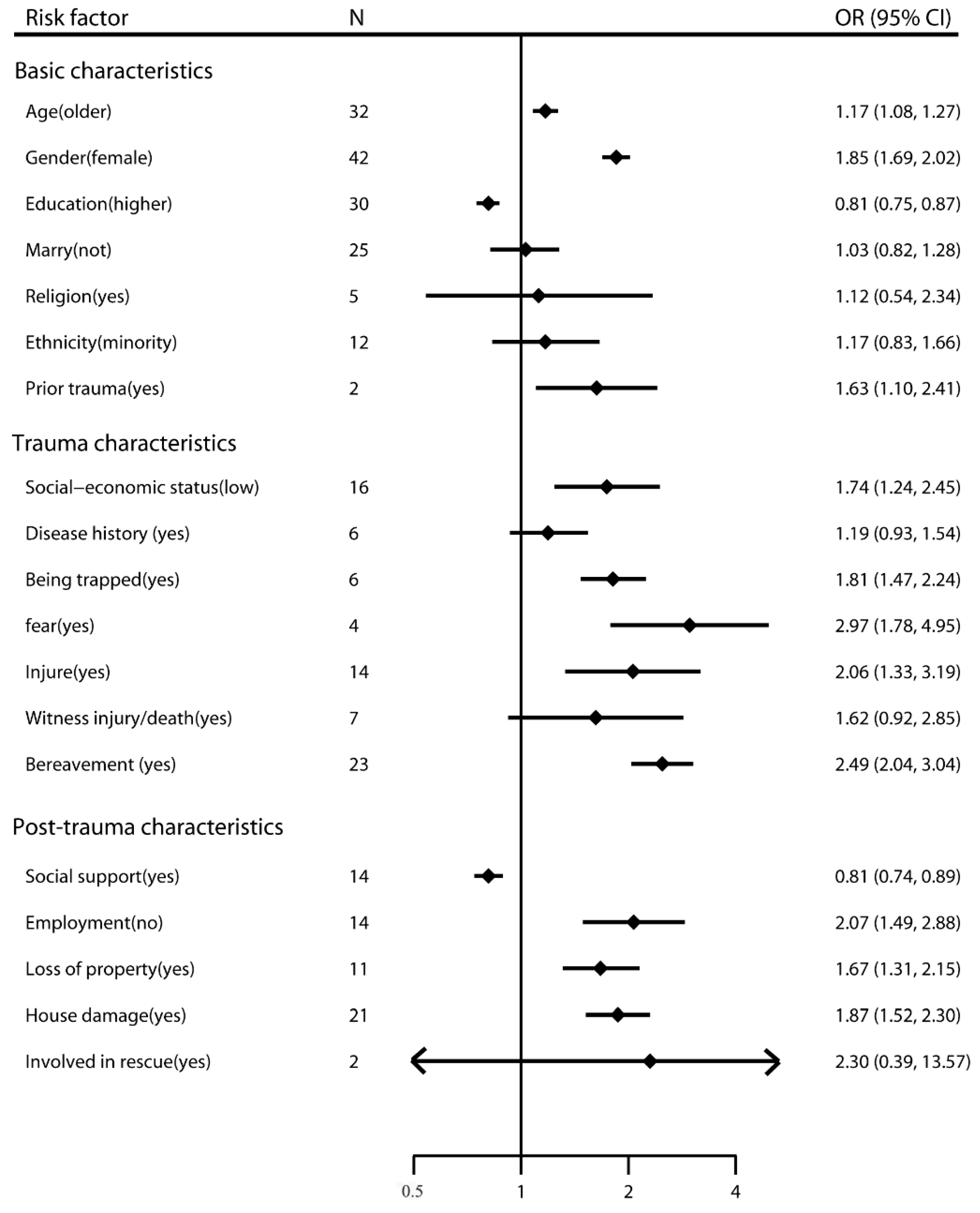
3.2. Risk Factors for PTSD in Adults
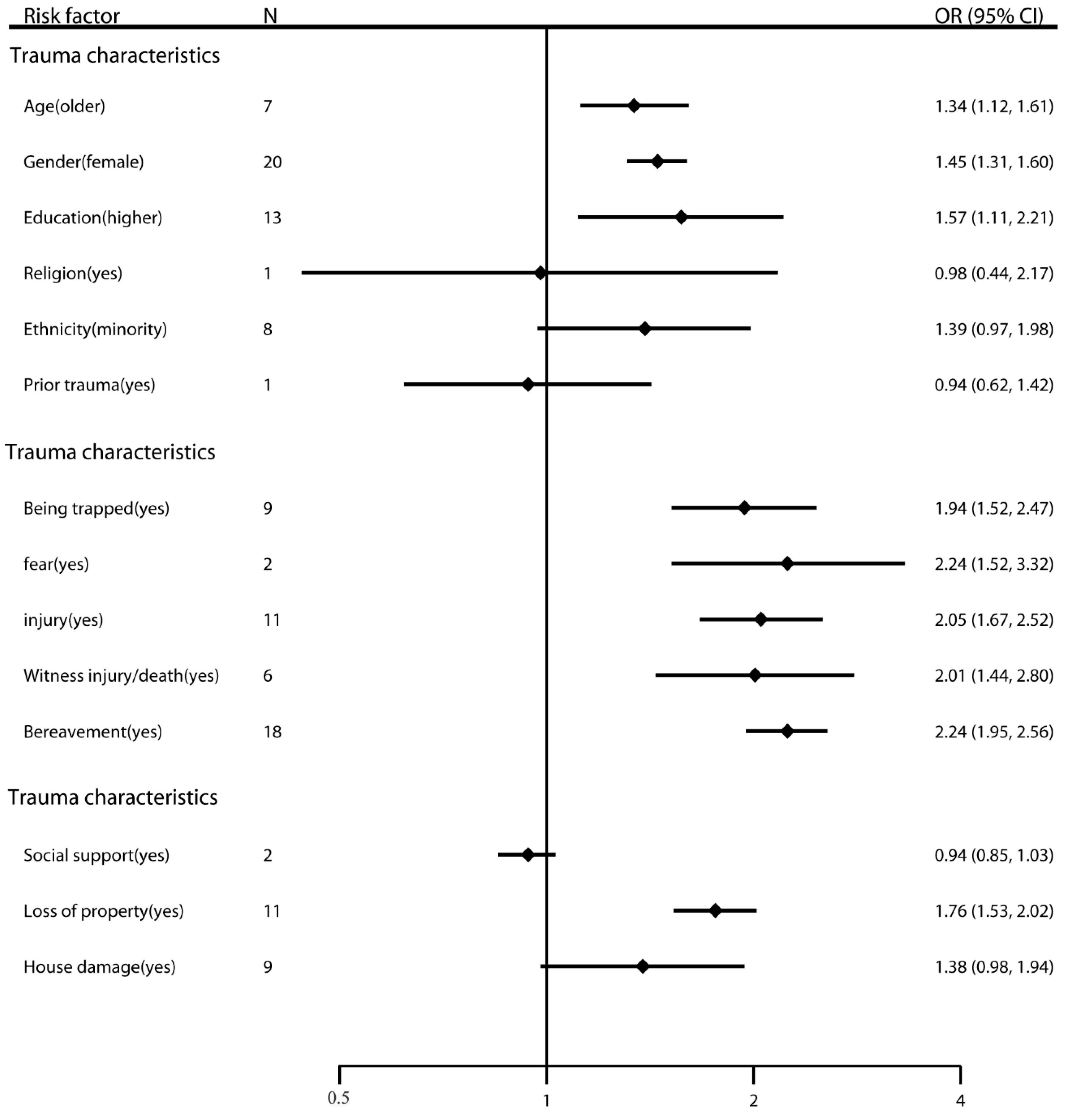
3.3. Risk Factors for PTSD in Children
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| No. | Author | Publication Year | Country | Earthquake Year | Magnitude | Population | Study Design | Identification of PTSD | Sample Size | PTSD Prevalence % | Time after Disaster | Male % | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Ali | 2012 | Pakistan | 2005 | 7.6 | adults | cross-section | Davidson Trauma Scale (DTS) | 300 | 41.30 | 30 months | 60.7 | 8 |
| 2 | Altindag | 2005 | Turkey | 1998 | 6.3 | adults | cross-section | Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition | 105 | 42.00, 23.00 | 1, 13 months | 47.6 | 8 |
| 3 | Cairo | 2010 | Peru | 2007 | 8.0 | adults | cross-section | a Spanish translation of the civilian version of the PTSD Checklist (PCL) | 298 | 25.20 | 5 months | 31.88 | 7 |
| 4 | Armenian | 2000 | Armenia | 1988 | 6.9 | adults | cohort | DSM-III-R | 737 | 49.60 | 2 years | 46.68 | 7 |
| 5 | Cenat | 2014 | Haiti | 2010 | 7.0 | adults | cross-section | Impact of event scale—Revised (IES-R) | 1355 | 36.75 | 30 months | 51.29 | 8 |
| 6 | Cenat | 2015 | Haiti | 2010 | 7.0 | children | cross-section | Impact of event scale—Revised (IES-R) | 872 | 36.93 | 30 months | 43.7 | 8 |
| 7 | Cerda | 2013 | Haiti | 2010 | 7.0 | adults | cross-section | DSM-IV | 1315 | 24.60 | 2–4 months | 28.9 | 7 |
| 8 | Chen | 2007 | China (Taiwan) | 1999 | 7.3 | adults | cross-section | The Davidson Trauma Scale (DTS) | 6412 | 20.90 | 24 months | 38.8 | 8 |
| 9 | Chen | 2012 | China | 2008 | 8.0 | adults | cross-section | the CAPS for DSM-IV | 287 | 22.65 | 36 months | 35.9 | 7 |
| 10 | Cheng | 2014 | China | 2008 | 8.0 | adults | case-control | the civilian version of the PTSD Checklist (PCL) | 565 | 20.00 | 36 months | 41.6 | 8 |
| 11 | Cheng | 2015 | China | 2008 | 8.0 | adults | cross-section | Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/NP) | 182 | 39.60 | 12 months | 34.8 | 8 |
| 12 | Chou | 2005 | China (Taiwan) | 1999 | 7.3 | adults | cross-section | DSM-IV | 442 | 7.90 | 6 months | 48.4 | 8 |
| 13 | Chou | 2007 | China (Taiwan) | 1999 | 7.3 | adults | cross-section | DSM-IV | 216 | 8.30 | 6, 24, 36 months | 45.8 | 8 |
| 14 | Cofini | 2015 | Italy | 2009 | 6.3 | adults | cross-section | Davidson Trauma Scale (DTS) | 281 | 43.00 | 12 months | 46 | 9 |
| 15 | Eksi | 2007 | Turkey | 1999 | 7.4 | children | cross-section | The Clinician-Administered Post-Traumatic Stress Disorder Scale (CAPS) | 160 | 60.00 | 6–20 weeks | 36.25 | 7 |
| 16 | Fan | 2015 | China | 2008 | 8.0 | children | cross-section | The Posttraumatic Stress Disorder Self-Rating Scale (PTSD-SS) | 1573 | 21.00, 23.35, 13.50, 14.70 | 6, 12, 18, 24 months | 45.77 | 9 |
| 17 | Fan | 2011 | China | 2008 | 8.0 | children | cross-section | The Posttraumatic Stress Disorder Self-Rating Scale (PTSD-SS) | 2081 | 15.80 | 6 months | 45.9 | 9 |
| 18 | Gigantesco | 2013 | Italy | 2009 | 6.3 | adults | cross-section | Mini-International Neuropsychiatric Interview (MINI) | 957 | 4.10 | 14–19 months | 49.2 | 8 |
| 19 | Guo | 2015 | China | 2008 | 8.0 | adults | cross-section | Impact of Event Scale-Revised (IES-R) | 1362 | 22.10 | 6 months | 36 | 7 |
| 20 | Guo | 2014 | China | 2008 | 8.0 | adults | cross-section | Impact of Event Scale-Revised (IES-R) | 1066 | 58.20, 22.10, 19.80, 8.00 | 2, 8, 14, 26, 44 months | 37.3 | 7 |
| 21 | Hashmi | 2011 | Pakistan | 2005 | 7.6 | adults | cross-section | the civilian version of the PTSD Checklist (PCL) | 361 | 51.50 | 6 months | 43 | 8 |
| 22 | Hikichi | 2016 | Japan | 2011 | 9.0 | adults | cross-section | the Screening Questionnaire for Disaster-Related Mental Health | 3567 | 11.40 | 30 months | 43.5 | 8 |
| 23 | Jia | 2010 | China | 2008 | 8.0 | children | cross-section | the self-report Child Posttraumatic Stress Disorder Reaction Index (CPTSD-RI) | 596 | 12.40 | 15 months | 49.8 | 9 |
| 24 | Jia | 2010 | China | 2008 | 8.0 | adults | cross-section | the self-report Child Posttraumatic Stress Disorder Reaction Index (CPTSD-RI) | 276 | 15.20 | 15 months | 53.6 | 7 |
| 25 | Jin | 2015 | China | 2010 | 7.1 | children | cross-section | the civilian version of the PTSD Checklist (PCL) | 459 | 10.90, 5.80 | 6, 24 months | 40.50 | 8 |
| 26 | Jin | 2014 | China | 2010 | 7.1 | children | cross-section | the civilian version of the PTSD Checklist (PCL) | 850 | 8.94 | 36 months | 44.8 | 7 |
| 27 | Kadak | 2013 | Turkey | 2011 | 7.2 | children | cross-section | Child Posttraumatic Stress Disorder–Reaction Index (CPTSD-R I) | 738 | 40.69 | 6 months | 55.01 | 8 |
| 28 | Kun | 2009 | China | 2008 | 8.0 | adults | cross-section | The Harvard Trauma Questionnaire (HTQ) | 446 | 45.50 | 2.5 months | 49.5 | 10 |
| 29 | Kun | 2013 | China | 2008 | 8.0 | adults | cross-section | the Harvard Trauma Questionnaire (HTQ) | 992 | 47.30 | 3 months | 49.2 | 10 |
| 30 | Lau | 2010 | China | 2008 | 8.0 | children | cross-section | the Children’s Revised Impact of Event Scale | 3324 | 22.30 | 1 month | 54.3 | 8 |
| 31 | Lee | 2009 | China (Taiwan) | 1999 | 7.3 | adults | cross-section | DSM-IV | 196 | 38.80 | 5 months | 54.6 | 7 |
| 32 | Liu | 2011 | China | 2008 | 8.0 | children | cross-section | Trauma Symptom Checklist for Children-Alternate Version (TSCC-A) | 330 | 11.20, 13.40 | 6, 12 months | 50 | 9 |
| 33 | Liu | 2012 | China | 2008 | 8.0 | adults | cross-section | the civilian version of the PTSD Checklist (PCL) | 9556 | 4.50 | 6 months | 45.3 | 6 |
| 34 | Liu | 2010 | China | 2008 | 8.0 | children | cross-section | the civilian version of the PTSD Checklist (PCL) | 1474 | 5.70 | 12 months | 45 | 8 |
| 35 | Ma | 2011 | China | 2008 | 8.0 | children | cross-section | DSM-IV | 3208 | 2.50 | 6 months | 47.9 | 7 |
| 36 | Pan | 2015 | China | 2008 | 8.0 | children | cross-section | Chinese version of the Impact of Event Scale–Revised (IES-R) | 362 | 29.60 | 36 months | 43.6 | 8 |
| 37 | Peng | 2009 | China | 2008 | 8.0 | adults | cross-section | the Harvard Trauma Questionnaire (HTQ) | 446 | 45.50 | 3 months | 50.9 | 8 |
| 38 | Priebe | 2009 | Italy | 2002 | 5.4 | adults | cross-section | The Breslau scale | 1680 | 14.50 | 6 months | 44.88 | 7 |
| 39 | Roncone | 2013 | Italy | 2009 | 6.3 | adults | cross-section | the Impact of Events Scale-revised (IES-R) | 91 | 56.00 | 6 months | 42.9 | |
| 40 | Tian | 2014 | China | 2008 | 8.0 | children | cross-section | DSM-IV | 4604 | 5.70 | 36 months | 56.8 | 7 |
| 41 | Tural | 2004 | Turkey | 1998 | 6.3 | adults | cross-section | DSM-IV | 910 | 25.40 | 4–12 months | 36.3 | 7 |
| 42 | Wang | 2011 | China | 2008 | 8.0 | adults | cross-section | Posttraumatic Stress Disorder Self-rating Scale (PTSD-SS) | 409 | 62.80 | 1 month | 50.12 | 9 |
| 43 | Wang | 2012 | China | 2008 | 8.0 | children | cross-section | Children’s Revised Impact of Event Scale (CRIES-13) | 1841 | 28.40 | 10 months | 48.7 | 9 |
| 44 | Wen | 2012 | China | 2008 | 8.0 | adults | cross-section | the civilian version of the PTSD Checklist (PCL) | 1206 | 4.46 | 36 months | 46.93 | 9 |
| 45 | Xu | 2011 | China | 2008 | 8.0 | adults | cross-section | the civilian version of the PTSD Checklist (PCL) | 367 | 48.20 | 12 months | 53.4 | 8 |
| 46 | Xu | 2011 | China | 2008 | 8.0 | adults | cross-section | the civilian version of the PTSD Checklist (PCL) | 2080 | 67.07 | 12–16 months | 47.26 | 8 |
| 47 | Zhang | 2015 | China | 2008 | 8.0 | adults | cross-section | the civilian version of the PTSD Checklist (PCL) | 684 | 9.20 | 60 months | 42.1 | 8 |
| 48 | Zhang | 2015 | China | 2008 | 8.0 | adults | cross-section | the civilian version of the PTSD Checklist (PCL) | 360 | 10.30 | 36 months | 55.6 | 9 |
| 49 | Zhang | 2011 | China | 2008 | 8.0 | adults | cross-section | the civilian version of the PTSD Checklist (PCL) | 1181 | 26.30 | 12 months | 37.3 | 10 |
| 50 | Zhang | 2012 | China | 2008 | 8.0 | adults | cross-section | the civilian version of the PTSD Checklist (PCL) | 274 | 26.30 | 14 months | 38 | 8 |
| 51 | Zhang | 2012 | China | 2010 | 7.1 | adults | cross-section | the civilian version of the PTSD Checklist (PCL) | 505 | 33.70 | 3–4 months | 53.5 | 8 |
| 52 | Zhou | 2013 | China | 2008 | 8.0 | adults | cross-section | a Chinese version of the Structured Clinical Interview for Diagnostic and Statistical Manual (DSM)-IV axis I disorders (SCID-I/P) | 14,207 | 15.57 | 6 months | 48.42 | 8 |
| Factors | All Studies | High Quality | Adjustment | Within 6 Months | High Magnitude | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | OR (95% CI) | I2 (p Value) | Egger Test | n | OR (95% CI) | n | OR (95% CI) | n | OR (95% CI) | n | OR (95% CI) | |
| Basic characteristics | ||||||||||||
| Age (older) | 32 | 1.17 (1.08–1.27) | 73.2% (p < 0.001) | p = 0.013 * | 20 | 1.07 (0.98–1.17) | 25 | 1.12 (1.03–1.22) | 12 | 1.49 (1.13–1.97) | 26 | 1.16 (1.07–1.27) |
| Gender (female) | 42 | 1.85 (1.69–2.02) | 51.1% (p < 0.001) | p = 0.855 | 28 | 1.94 (1.74–2.15) | 33 | 1.85 (1.69–2.03) | 16 | 2.01 (1.67–2.42) | 34 | 1.82 (1.66–1.99) |
| Education (higher) | 30 | 0.81 (0.75–0.87) | 33.3% (p = 0.041) | p = 0.550 | 18 | 0.86 (0.78–0.95) | 22 | 0.83 (0.76–0.90) | 12 | 0.78 (0.67–0.89) | 22 | 0.81 (0.74–0.88) |
| Marry (not) | 25 | 1.03 (0.82–1.28) | 79.6% (p < 0.001) | p = 0.226 | 14 | 1.35 (0.93–1.97) | 19 | 1.04 (0.80–1.35) | 11 | 0.95 (0.52–1.72) | 14 | 1.35 (0.93–1.97) |
| Religion (yes) | 5 | 1.12 (0.54–2.34) | 72.0% (p = 0.006) | p = 0.661 | 5 | 1.12 (0.54–2.34) | 3 | 0.97 (0.27–3.52) | 1 | 2.54 (0.86–7.52) | 4 | 1.07 (0.42–2.76) |
| Ethnicity (minority) | 12 | 1.17 (0.83–1.66) | 82.9% (p < 0.001) | p = 0.490 | 11 | 1.19 (0.83–1.73) | 8 | 1.30 (0.83–2.05) | 3 | 1.77 (1.12–2.79) | 12 | 1.17 (0.83–1.66) |
| Prior trauma (yes) | 2 | 1.63 (1.10–2.41) | 55.3% (p = 0.135) | – | 1 | 2.07 (1.33–3.23) | 1 | 1.38 (1.03–1.85) | 1 | 2.07 (1.33–3.23) | 1 | 2.07 (1.33–3.23) |
| Socio-economic status (low) | 16 | 1.74 (1.24–2.45) | 89.0% (p < 0.001) | p = 0.532 | 9 | 2.91 (1.56–5.41) | 15 | 1.68 (1.18–2.40) | 3 | 1.73 (0.71–4.17) | 16 | 1.74 (1.24–2.45) |
| Disease history (yes) | 6 | 1.19 (0.93–1.54) | 0.0% (p = 0.972) | p = 0.381 | 6 | 1.19 (0.93–1.54) | 2 | 1.21 (0.89–1.65) | 1 | 1.27 (0.49–3.33) | 4 | 1.20 (0.92–1.56) |
| Trauma characteristics | ||||||||||||
| Being trapped (yes) | 6 | 1.81 (1.47–2.24) | 0.0% (p = 0.664) | p = 0.784 | 3 | 1.68 (1.21–2.34) | 5 | 1.75 (1.41–2.18) | 2 | 1.85 (1.41–2.44) | 5 | 1.89 (1.50–2.37) |
| fear (yes) | 4 | 2.97 (1.78–4.95) | 92.9% (p < 0.001) | p = 0.659 | 4 | 2.97 (1.78–4.95) | 3 | 3.55 (1.90–6.63) | – | – | 4 | 2.97 (1.78–4.95) |
| Injure (yes) | 14 | 2.06 (1.33–3.19) | 90.0% (p < 0.001) | p = 0.185 | 9 | 1.79 (0.92–3.50) | 6 | 1.45 (0.80–2.62) | 5 | 1.89 (0.79–4.54) | 10 | 2.08 (1.22–3.56) |
| Witness injury/death (yes) | 7 | 1.62 (0.92–2.85) | 90.5% (p < 0.001) | p = 0.383 | 4 | 1.64 (0.59–4.54) | 4 | 1.19 (0.70–2.03) | 2 | 0.98 (0.45–2.11) | 7 | 1.62 (0.92–2.85) |
| Bereavement (yes) | 23 | 2.49 (2.04–3.04) | 70.8% (p < 0.001) | p = 0.465 | 17 | 2.56 (1.97–3.32) | 15 | 2.36 (1.89–2.93) | 8 | 2.65 (1.78–3.93) | 17 | 2.61 (2.07–3.29) |
| Post-trauma characteristics | ||||||||||||
| Social support (yes) | 14 | 0.81 (0.74–0.89) | 94.7% (p < 0.001) | p = 0.103 | 8 | 0.82 (0.74–0.91) | 8 | 0.72 (0.65–0.80) | 4 | 1.11 (0.83–1.48) | 8 | 0.83 (0.76–0.92) |
| Employment (no) | 14 | 2.07 (1.49–2.88) | 85.5% (p < 0.001) | p = 0.996 | 12 | 2.19 (1.50–3.20) | 10 | 2.34 (1.59–3.43) | 6 | 2.61 (1.55–4.39) | 12 | 2.31 (1.63–3.29) |
| Loss of property (yes) | 11 | 1.67 (1.31–2.15) | 60.2% (p = 0.005) | p = 0.005 * | 9 | 1.68 (1.25–2.25) | 7 | 1.40 (1.15–1.71) | 4 | 1.47 (1.07–2.02) | 10 | 1.58 (1.24–2.03) |
| House damage (yes) | 21 | 1.87 (1.52–2.30) | 60.6% (p < 0.001) | p = 0.475 | 17 | 2.12 (1.71–2.63) | 13 | 1.92 (1.49–2.49) | 8 | 2.06 (1.45–2.94) | 16 | 1.98 (1.58–2.48) |
| Involved in rescue (yes) | 2 | 2.30 (0.39–13.57) | 98.1% (p < 0.001) | – | 2 | 2.30 (0.39–13.57) | 2 | 2.30 (0.39–13.57) | 1 | 5.69 (4.04–8.00) | 1 | 5.69 (4.04–8.00) |
| Factors | All Studies | High Quality | Adjustment | Within 6 Months | High Magnitude | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | OR (95% CI) | I2 (p Value) | Egger Test | n | OR (95% CI) | n | OR (95% CI) | n | OR (95% CI) | n | OR (95% CI) | |
| Basic characteristics | ||||||||||||
| Age (older) | 7 | 1.34 (1.12–1.61) | 42.2% (p = 0.109) | p = 0.402 | 6 | 1.40 (1.15–1.71) | 5 | 1.43 (1.16–1.76) | 4 | 1.38 (1.06–1.78) | 6 | 1.40 (1.15–1.70) |
| Gender (female) | 20 | 1.45 (1.31–1.60) | 26.5% (p = 0.135) | p = 0.138 | 16 | 1.47 (1.33–1.62) | 12 | 1.43 (1.20–1.70) | 8 | 1.48 (1.21–1.81) | 19 | 1.43 (1.29–1.60) |
| Education (higher) | 13 | 1.57 (1.11–2.21) | 77.7% (p < 0.001) | p = 0.115 | 12 | 1.55 (1.08–2.23) | 7 | 1.36 (0.78–2.37) | 5 | 1.38 (0.70–2.74) | 13 | 1.57 (1.11–2.21) |
| Religion (yes) | 1 | 0.98 (0.44–2.17) | - | - | 1 | 0.98 (0.44–2.17) | 1 | 0.98 (0.44–2.17) | 1 | 0.98 (0.44–2.17) | 1 | 0.98 (0.44–2.17) |
| Ethnicity (minority) | 8 | 1.39 (0.97–1.98) | 0.0% (p = 0.900) | p = 0.645 | 6 | 1.35 (0.94–1.94) | 8 | 1.39 (0.97–1.98) | 2 | 1.04 (0.36–2.99) | 8 | 1.39 (0.97–1.98) |
| Prior trauma (yes) | 1 | 0.94 (0.62–1.42) | - | - | 1 | 0.94 (0.62–1.42) | 1 | 0.94 (0.62–1.42) | 1 | 0.94 (0.62–1.42) | 1 | 0.94 (0.62–1.42) |
| Trauma characteristics | ||||||||||||
| Being trapped (yes) | 9 | 1.94 (1.52–2.47) | 0% (p = 0.812) | p = 0.463 | 8 | 1.97 (1.52–2.56) | 7 | 2.21 (1.67–2.92) | 4 | 1.90 (1.33–2.72) | 9 | 1.94 (1.52–2.47) |
| fear (yes) | 2 | 2.24 (1.52–3.32) | 0.0% (p = 0.777) | – | 2 | 2.24 (1.52–3.32) | 1 | 2.32 (1.47–3.67) | 1 | 2.04 (0.95–4.36) | 2 | 2.24 (1.52–3.32) |
| injury (yes) | 11 | 2.05 (1.67–2.52) | 4.9% (p = 0.397) | p = 0.379 | 8 | 2.04 (1.59–2.62) | 9 | 2.17 (1.69–2.80) | 5 | 2.43 (1.77–3.35) | 11 | 2.05 (1.67–2.52) |
| Witness injury/death (yes) | 6 | 2.01 (1.44–2.80) | 64.9% (p = 0.014) | p = 0.027 * | 4 | 2.26 (1.59–3.22) | 4 | 2.00 (1.32–3.04) | 2 | 2.68 (1.59–4.54) | 6 | 2.01 (1.44–2.80) |
| Bereavement (yes) | 18 | 2.24 (1.95–2.56) | 19.7% (p = 0.219) | p = 0.217 | 15 | 2.33 (2.02–2.69) | 11 | 2.33 (1.82–2.99) | 8 | 2.30 (1.72–3.07) | 17 | 2.28 (1.97–2.65) |
| Post-trauma characteristics | ||||||||||||
| Social support (yes) | 2 | 0.94 (0.85–1.03) | 95.4% (p < 0.001) | - | - | - | 2 | 0.94 (0.85–1.03) | 1 | 0.89 (0.86–0.93) | 2 | 0.94 (0.85–1.03) |
| Loss of property (yes) | 11 | 1.76 (1.53–2.02) | 0.0% (p = 0.696) | p = 0.276 | 10 | 1.93 (1.60–2.33) | 7 | 1.63 (1.39–1.92) | 4 | 1.80 (1.35–2.39) | 11 | 1.76 (1.53–2.02) |
| House damage (yes) | 9 | 1.38 (0.98–1.94) | 55.1% (p = 0.023) | p = 0.308 | 7 | 1.32 (0.87–1.98) | 8 | 1.22 (0.94–1.59) | 6 | 1.17 (0.85–1.62) | 9 | 1.38 (0.98–1.94) |
References
- Aker, A.T. 1999 Marmara earthquakes: A review of epidemiologic findings and community mental health policies. Turk Psikiyatr. Derg. 2006, 17, 204–212. [Google Scholar]
- Ali, M.; Farooq, N.; Bhatti, M.A.; Kuroiwa, C. Assessment of prevalence and determinants of posttraumatic stress disorder in survivors of earthquake in Pakistan using Davidson Trauma Scale. J. Affect. Disord. 2012, 136, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Duan, G.; Xu, Q.; Jia, Z.; Bai, Z.; Liu, W. A Cross-sectional study on posttraumatic stress disorder and general psychiatric morbidity among adult survivors 3 years after the Wenchuan earthquake, China. Asia Pac. J. Public Health 2015, 27, 860–870. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Hong, C.; Efferth, T. Systematic review on post-traumatic stress disorder among survivors of the Wenchuan earthquake. Trauma Violence Abuse 2016, 17, 542–561. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Li, J. Prospective study of posttraumatic stress in adolescents 6 and 24 months after the 2010 Yushu earthquake in China. J. Nerv. Ment. Dis. 2015, 203, 679–683. [Google Scholar] [CrossRef] [PubMed]
- McFarlane, A.C. Posttraumatic stress disorder: A model of the longitudinal course and the role of risk factors. J. Clin. Psychiatry 2000, 61, 15–20. [Google Scholar] [PubMed]
- Harvey, A.G.; Bryant, R.A. The relationship between acute stress disorder and posttraumatic stress disorder: A prospective evaluation of motor vehicle accident survivors. J. Consult. Clin. Psychol. 1998, 66, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Wang, L.; Shi, Z.; Zhang, Z.; Zhang, K.; Shen, J. Mental health problems among children one-year after Sichuan earthquake in China: A follow-up study. PLoS ONE 2011, 6, e14706. [Google Scholar] [CrossRef] [PubMed]
- Cerdá, M.; Paczkowski, M.; Galea, S.; Nemethy, K.; Péan, C.; Desvarieux, M. Psychopathology in the aftermath of the Haiti earthquake: A population-based study of posttraumatic stress disorder and major depression. Depression Anxiety 2013, 30, 413–424. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Shen, H. A cross-sectional study on posttraumatic stress disorder among elderly Qiang citizens 3 years after the Wenchuan earthquake in China. Can. J. Psychiatry 2012, 57, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Wang, X.; Yuan, J.; Zhang, W.; Tian, D.; Qu, Z. The symptoms of posttraumatic stress disorder and depression among adult earthquake survivors in China. J. Nerv. Ment. Dis. 2015, 203, 469–472. [Google Scholar] [CrossRef] [PubMed]
- Jia, Z.; Tian, W.; He, X.; Liu, W.; Jin, C.; Ding, H. Mental health and quality of life survey among child survivors of the 2008 Sichuan earthquake. Qual. Life Res. 2010, 19, 1381–1391. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Song, X. Posttraumatic stress disorder among survivors of the Wenchuan earthquake 1 year after: Prevalence and risk factors. Compr. Psychiatry 2011, 52, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Altindag, A.; Ozen, S.; Sir, A. One-year follow-up study of posttraumatic stress disorder among earthquake survivors in Turkey. Compr. Psychiatry 2005, 46, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Wu, P.; Tian, D.; Wang, X.; Zhang, W.; Zhang, X. Post-traumatic stress disorder among adult survivors of the Wenchuan earthquake in China: A repeated cross-sectional study. J. Anxiety Disord. 2014, 28, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Kang, L.; Sun, X.; Song, H.; Mao, W.; Huang, X. Risk factors of mental illness among adult survivors after the Wenchuan earthquake. Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 907–915. [Google Scholar] [CrossRef] [PubMed]
- Teramoto, C.; Matsunaga, A.; Nagata, S. Cross-sectional study of social support and psychological distress among displaced earthquake survivors in Japan. Jpn. J. Nurs. Sci. 2015, 12, 320–329. [Google Scholar] [CrossRef] [PubMed]
- Ozer, E.J.; Best, S.R.; Lipsey, T.L.; Weiss, D.S. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychol. Bull. 2003, 129, 52–73. [Google Scholar] [CrossRef] [PubMed]
- Trickey, D.; Siddaway, A.P.; Meiser-Stedman, R.; Serpell, L.; Field, A.P. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clin. Psychol. Rev. 2012, 32, 122–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brewin, C.R.; Andrews, B.; Valentine, J.D. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J. Consult. Clin. Psychol. 2000, 68, 748–766. [Google Scholar] [CrossRef] [PubMed]
- Berger, W.; Coutinho, E.S.; Figueira, I.; Marques-Portella, C.; Luz, M.P.; Neylan, T.C. Rescuers at risk: A systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 1001–1011. [Google Scholar] [CrossRef] [PubMed]
- Machtinger, E.L.; Wilson, T.C.; Haberer, J.E.; Weiss, D.S. Psychological trauma and PTSD in HIV-positive women: A meta-analysis. AIDS Behav. 2012, 16, 2091–2100. [Google Scholar] [CrossRef] [PubMed]
- Porter, M.; Haslam, N. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: A meta-analysis. JAMA 2005, 294, 602–612. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhu, S.; Du, C.; Zhang, Y. Posttraumatic stress disorder and somatic symptoms among child and adolescent survivors following the Lushan earthquake in China: A six-month longitudinal study. J. Psychosom. Res. 2015, 79, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Eksi, A.; Braun, K.L.; Ertem-Vehid, H.; Peykerli, G.; Saydam, R.; Toparlak, D. Risk factors for the development of PTSD and depression among child and adolescent victims following a 7.4 magnitude earthquake. Int. J. Psychiatry Clin. Pract. 2007, 11, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Celiac Disease. Evidence Reports/Technology Assessments NAD. Available online: http://www.ncbi.nlm.nih.gov/books/NBK35156 (accessed on 18 July 2016).
- Wells, G.A.; Shea, B.J.; O’Connell, D.; Peterson, J.E.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis. Appl. Eng. Agric. 2014, 18, 727–734. [Google Scholar]
- Tang, B.; Liu, X.; Liu, Y.; Xue, C.; Zhang, L. A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health 2014, 14, 623. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Armenian, H.K.; Morikawa, M.; Melkonian, A.K.; Hovanesian, A.P.; Haroutunian, N.; Saigh, P.A. Loss as a determinant of PTSD in a cohort of adult survivors of the 1988 earthquake in Armenia: Implications for policy. Acta Psychiatr. Scand. 2000, 102, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Cénat, J.M.; Derivois, D. Long-term outcomes among child and adolescent survivors of the 2010 Haitian earthquake. Depression Anxiety 2015, 32, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Cairo, J.B.; Dutta, S.; Nawaz, H.; Hashmi, S.; Kasl, S.; Bellido, E. The prevalence of posttraumatic stress disorder among adult earthquake survivors in Peru. Disaster Med. Public Health Prep. 2010, 4, 39–46. [Google Scholar] [CrossRef]
- Cenat, J.M.; Derivois, D. Assessment of prevalence and determinants of posttraumatic stress disorder and depression symptoms in adults survivors of earthquake in Haiti after 30 months. J. Affect. Disord. 2014, 159, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Tan, H.K.; Liao, L.R.; Chen, H.H.; Chan, C.C.; Cheng, J.J. Long-term psychological outcome of 1999 Taiwan earthquake survivors: A survey of a high-risk sample with property damage. Compr. Psychiatry 2007, 48, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Wang, F.; Wen, J.; Shi, Y. Risk Factors of Post-Traumatic Stress Disorder (PTSD) after Wenchuan Earthquake: A Case Control Study. PLoS ONE 2014, 9, e96644. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.; Ma, N.; Yang, L.; Agho, K.; Stevens, G.; Raphael, B. Depression and Posttraumatic Stress Disorder in Temporary Settlement Residents 1 Year After the Sichuan Earthquake. Asia Pac. J. Public Health 2015, 27, NP1962–NP1972. [Google Scholar] [CrossRef] [PubMed]
- Chou, F.H.C.; Su, T.T.P.; Chou, P.; Ou-Yang, W.C.; Lu, M.K.; Chien, I.C. Survey of psychiatric disorders in a Taiwanese village population six months after a major earthquake. J. Formos. Med. Assoc. 2005, 104, 308–317. [Google Scholar] [PubMed]
- Chou, F.H.C.; Wu, H.C.; Chou, P.; Su, C.Y.; Tsai, K.Y.; Chao, S.S. Epidemiologic psychiatric studies on post-disaster impact among Chi-Chi earthquake survivors in Yu-Chi, Taiwan. Psychiatry Clin. Neurosci. 2007, 61, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Cofini, V.; Carbonelli, A.; Cecilia, M.R.; Binkin, N.; di Orio, F. Post traumatic stress disorder and coping in a sample of adult survivors of the Italian earthquake. Psychiatry Res. 2015, 229, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Fan, F.; Long, K.; Zhou, Y.; Zheng, Y.; Liu, X. Longitudinal trajectories of post-traumatic stress disorder symptoms among adolescents after the Wenchuan earthquake in China. Psychol. Med. 2015, 45, 2885–2896. [Google Scholar] [CrossRef] [PubMed]
- Fan, F.; Zhang, Y.; Yang, Y.; Mo, L.; Liu, X. Symptoms of posttraumatic stress disorder, depression, and anxiety among adolescents following the 2008 Wenchuan earthquake in China. J. Trauma. Stress 2011, 24, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Gigantesco, A.; Mirante, N.; Granchelli, C.; Diodati, G.; Cofini, V.; Mancini, C. Psychopathological chronic sequelae of the 2009 earthquake in L’Aquila, Italy. J. Affect. Disord. 2013, 148, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Hashmi, S.; Petraro, P.; Rizzo, T.; Nawaz, H.; Choudhary, R.; Tessier-Sherman, B. Symptoms of anxiety, depression, and posttraumatic stress among survivors of the 2005 Pakistani earthquake. Disaster Med. Public Health Prep. 2011, 5, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Hikichi, H.; Aida, J.; Tsuboya, T.; Kondo, K.; Kawachi, I. Can community social cohesion prevent posttraumatic stress disorder in the aftermath of a disaster? A natural experiment from the 2011 Tohoku earthquake and tsunami. Am. J. Epidemiol. 2016, 183, 902–910. [Google Scholar] [CrossRef] [PubMed]
- Jia, Z.; Tian, W.; Liu, W.; Cao, Y.; Yan, J.; Shun, Z. Are the elderly more vulnerable to psychological impact of natural disaster? A population-based survey of adult survivors of the 2008 Sichuan earthquake. BMC Public Health 2010, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Wang, G. Individual risk factors for PTSD in adolescents from the 2010 earthquake in Yushu: The predictor effect of rumination. Afr. J. Psychiatry 2014, 17. [Google Scholar] [CrossRef]
- Kadak, M.T.; Nasiroglu, S.; Boysan, M.; Aydin, A. Risk factors predicting posttraumatic stress reactions in adolescents after 2011 Van earthquake. Compr. Psychiatry 2013, 54, 982–990. [Google Scholar] [CrossRef] [PubMed]
- Kun, P.; Chen, X.; Han, S.; Gong, X.; Chen, M.; Zhang, W.; Yao, L. Prevalence of post-traumatic stress disorder in Sichuan Province, China after the 2008 Wenchuan earthquake. Public Health 2009, 123, 703–707. [Google Scholar] [CrossRef] [PubMed]
- Kun, P.; Tong, X.; Liu, Y.; Pei, X.; Luo, H. What are the determinants of post-traumatic stress disorder: Age, gender, ethnicity or other? Evidence from 2008 Wenchuan earthquake. Public Health 2013, 127, 644–652. [Google Scholar] [CrossRef]
- Lau, J.T.F.; Yu, X.; Zhang, J.; Mak, W.W.S.; Choi, K.C.; Lui, W.W.S. Psychological distress among adolescents in Chengdu, Sichuan at 1 month after the 2008 Sichuan earthquake. J. Urban Health 2010, 87, 504–523. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Chang, J.C.; Liu, C.Y.; Chang, C.J.; Chen, T.H.H.; Chen, C.H. Acculturation, psychiatric comorbidity and posttraumatic stress disorder in a Taiwanese aboriginal population. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Ma, X.; Hu, X.; Qiu, C.; Wang, Y.; Wang, Q. A risk score for predicting post-traumatic stress disorder in adults in a Chinese earthquake area. J. Int. Med. Res. 2012, 40, 2191–2198. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Yang, Y.; Ye, Y.; Zeng, Z.; Xiang, Y.; Yuan, P. One-year follow-up study of post-traumatic stress disorder among adolescents following the Wenchuan earthquake in China. Biosci. Trends 2010, 4, 96–102. [Google Scholar] [PubMed]
- Ma, X.; Liu, X.; Hu, X.; Qiu, C.; Wang, Y.; Huang, Y. Risk indicators for post-traumatic stress disorder in adolescents exposed to the 5.12 Wenchuan earthquake in China. Psychiatry Res. 2011, 189, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.; Liu, W.; Deng, G.; Liu, T.; Yan, J.; Tang, Y. Symptoms of posttraumatic stress disorder, depression, and anxiety among junior high school students in worst-hit areas 3 years after the Wenchuan earthquake in China. Asia Pac. J. Public Health 2015, 27, NP1985–NP1994. [Google Scholar] [CrossRef] [PubMed]
- Peng, K.; Shucheng, H.; Xunchui, C.; Lan, Y. Prevalence and risk factors for posttraumatic stress disorder: A cross-sectional study among survivors of the Wenchuan 2008 earthquake in China. Depression Anxiety 2009, 26, 1134–1140. [Google Scholar]
- Priebe, S.; Grappasonni, I.; Mari, M.; Dewey, M.; Petrelli, F.; Costa, A. Posttraumatic stress disorder six months after an earthquake: Findings from a community sample in a rural region in Italy. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Roncone, R.; Giusti, L.; Mazza, M.; Bianchini, V.; Ussorio, D.; Pollice, R. Persistent fear of aftershocks, impairment of working memory, and acute stress disorder predict post-traumatic stress disorder: 6-month follow-up of help seekers following the L’Aquila earthquake. Springerplus 2013, 2, 636. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Wong, T.K.S.; Li, J.; Jiang, X. Posttraumatic stress disorder and its risk factors among adolescent survivors three years after an 8.0 magnitude earthquake in China. BMC Public Health 2014, 14, 1073. [Google Scholar] [CrossRef] [PubMed]
- Tural, U.; Coşkun, B.; Onder, E.; Corapçioglu, A.; Yildiz, M.; Kesepara, C. Psychological consequences of the 1999 earthquake in Turkey. J. Trauma. Stress 2004, 17, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Ni, C.; Chen, J.; Liu, X.; Wang, A.; Shao, Z. Posttraumatic stress disorder 1 month after 2008 earthquake in China: Wenchuan earthquake survey. Psychiatry Res. 2011, 187, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Fu, W.; Wu, J.; Ma, X.-C.; Sun, X.-L.; Huang, Y. Prevalence of PTSD and depression among junior middle school students in a rural town far from the epicenter of the Wenchuan earthquake in China. PLoS ONE 2012, 7, e41665. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Shi, Y.-K.; Li, Y.-P.; Yuan, P.; Wang, F. Quality of life, physical diseases, and psychological impairment among survivors 3 years after Wenchuan earthquake: A population based survey. PLoS ONE 2012, 7, e43081. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Song, X. A cross-sectional study among survivors of the 2008 Sichuan earthquake: Prevalence and risk factors of posttraumatic stress disorder. Gen. Hosp. Psychiatry 2011, 33, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.-P.; Zhao, Q.; Luo, Z.-C.; Lei, Y.-X.; Wang, Y.; Wang, P.-X. Prevalence and risk factors of posttraumatic stress disorder among survivors five years after the “Wenchuan” earthquake in China. Health Qual. Life Outcomes 2015, 13, 75. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ho, S.M.Y. Risk factors of posttraumatic stress disorder among survivors after the 512 Wenchuan earthquake in China. PLoS ONE 2011, 6, e22371. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Shi, Z.; Wang, L.; Liu, M. Post-traumatic stress disorder, anxiety and depression among the elderly: A survey of the hard-hit areas a year after the Wenchuan earthquake. Stress Health 2012, 28, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Wang, W.; Shi, Z.; Wang, L.; Zhang, J. Mental health problems among the survivors in the hard-hit areas of the Yushu earthquake. PLoS ONE 2012, 7, e46449. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Kang, L.; Sun, X.; Song, H.; Mao, W.; Huang, X. Prevalence and risk factors of post-traumatic stress disorder among adult survivors six months after the Wenchuan earthquake. Compr. Psychiatry 2013, 54, 493–499. [Google Scholar] [CrossRef] [PubMed]
- WHO. Determinants of Mental and Behavioural Disorders. 2016. Available online: http://www.who.int/whr/2001/chapter2/en/index7.html (accessed on 18 July 2016).
- Korol, M.; Green, B.L.; Gleser, G.C. Children’s responses to a nuclear waste disaster: PTSD symptoms and outcome prediction. J. Am. Acad. Child Adolesc. Psychiatry 1999, 38, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Galea, S.; Tracy, M.; Norris, F.; Coffey, S.F. Financial and social circumstances and the incidence and course of PTSD in Mississippi during the first two years after Hurricane Katrina. J. Trauma. Stress 2008, 21, 357–368. [Google Scholar] [CrossRef] [PubMed]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, B.; Deng, Q.; Glik, D.; Dong, J.; Zhang, L. A Meta-Analysis of Risk Factors for Post-Traumatic Stress Disorder (PTSD) in Adults and Children after Earthquakes. Int. J. Environ. Res. Public Health 2017, 14, 1537. https://doi.org/10.3390/ijerph14121537
Tang B, Deng Q, Glik D, Dong J, Zhang L. A Meta-Analysis of Risk Factors for Post-Traumatic Stress Disorder (PTSD) in Adults and Children after Earthquakes. International Journal of Environmental Research and Public Health. 2017; 14(12):1537. https://doi.org/10.3390/ijerph14121537
Chicago/Turabian StyleTang, Bihan, Qiangyu Deng, Deborah Glik, Junqiang Dong, and Lulu Zhang. 2017. "A Meta-Analysis of Risk Factors for Post-Traumatic Stress Disorder (PTSD) in Adults and Children after Earthquakes" International Journal of Environmental Research and Public Health 14, no. 12: 1537. https://doi.org/10.3390/ijerph14121537




