Practicing Dentists’ Self-Efficacy and Associated Factors in Managing the Treatment of Adults with Mental and Physical Disabilities: An Exploratory Cross-Sectional Study in Riyadh, Saudi Arabia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Setting and Participants’ Recruitment
2.2. Data Collection and Measures
2.3. Ethical Considerations
2.4. Statistical Analysis
3. Results
3.1. Sample Characteristics
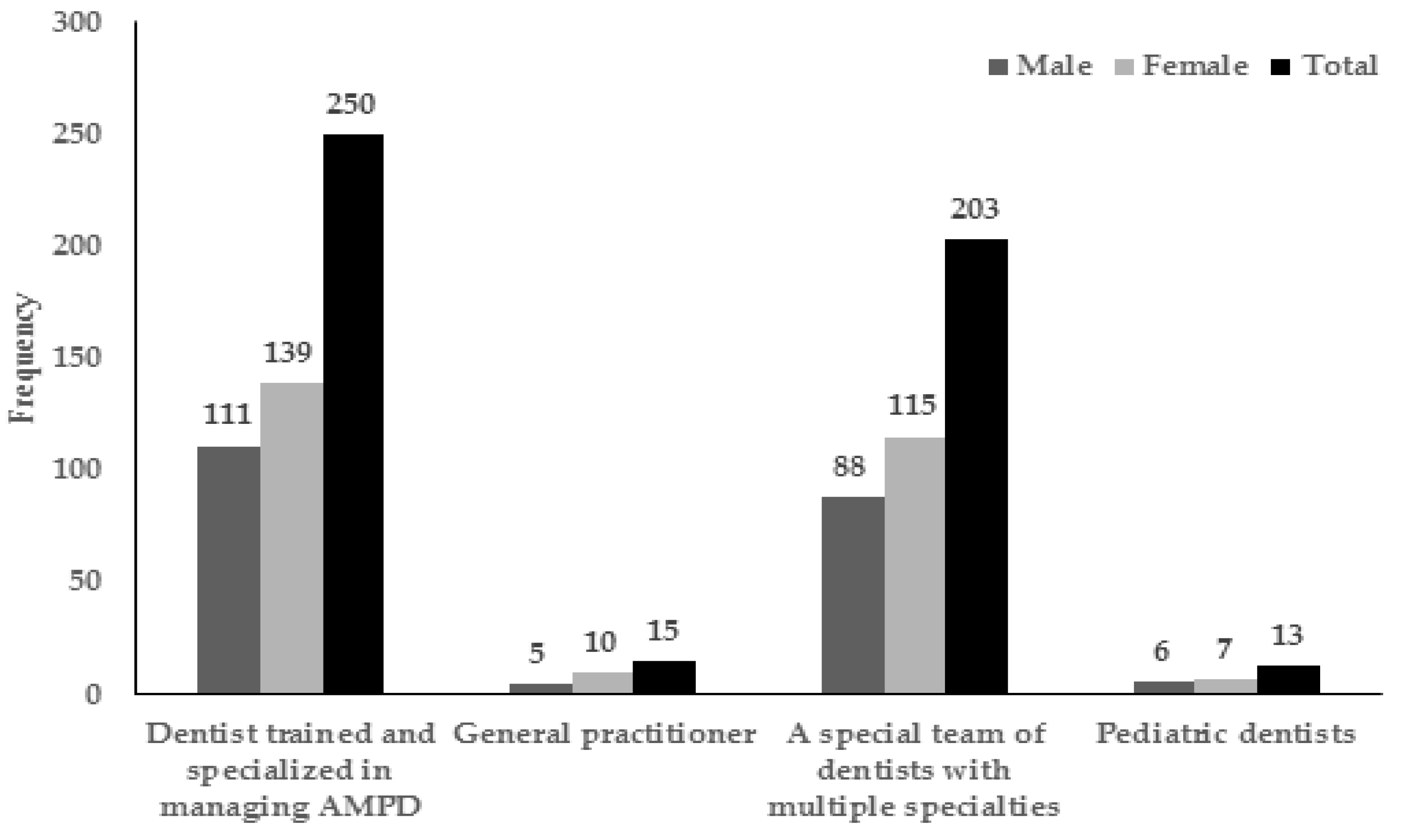
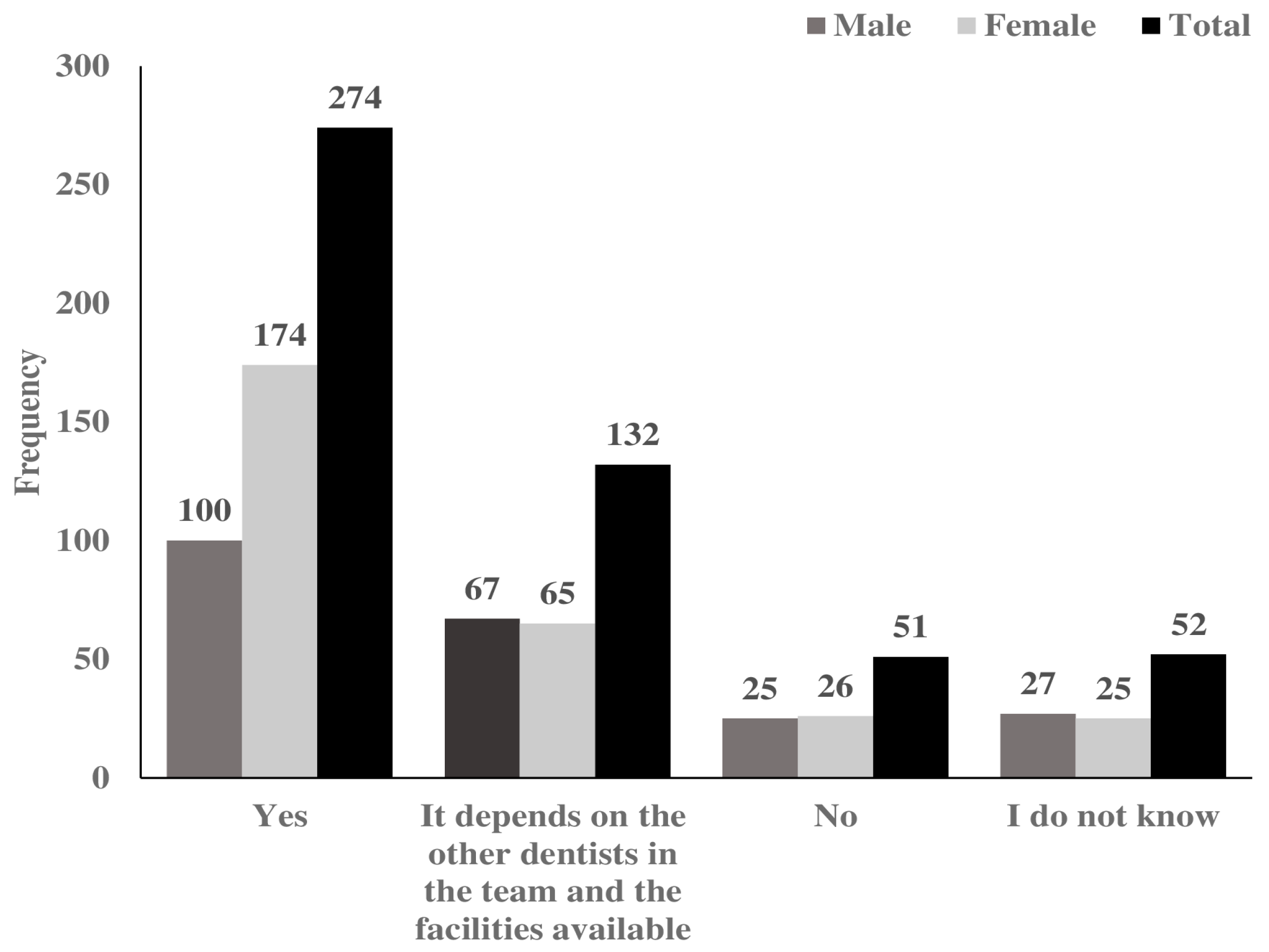
3.2. Descriptive Analyses of Training, Interest, Attitude, Experiences, and Self-Efficacy in Managing AMPD
3.3. Bivariate Analyses of Factors Associated with Self-Efficacy in Managing AMPD
3.4. Multivariable Logistic Regression Analyses of Factors Associated with Self-Efficacy in Managing AMPD
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Disability Law. M/37. R. Decree. 244. Bureau of Experts at the Council of Ministers: Saudi Arabia. Available online: https://boe.gov.sa (accessed on 28 August 2016).
- Schalock, R.L.; Borthwick-Duffy, S.A.; Bradley, V.J.; Buntinx, W.H.E.; Coulter, D.L.; Craig, E.M.; Gomez, S.C.; Lachapelle, Y.; Luckasson, R.; Reeve, A. Intellectual Disability: Definition, Classification, and Systems of Supports. Available online: https://eric.ed.gov/?id=ED509596–2010 (accessed on 28 August 2017).
- WHO (World Health Organization). The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Available online: https://scholar.google.com/citations?view_op=view_citation&continue=/scholar%3Fq%3DThe%2BICD-10%2Bclassification%2Bof%2Bmental%2Band%2Bbehavioural%2Bdisorders:%2Bclinical%2Bdescriptions%2Band%2Bdiagnostic%2Bguidelines%26hl%3Den%26as_sdt%3D0,5&citilm=1&citation_for_view=oFDmaucAAAAJ:zYLM7Y9cAGgC&hl=en&oi=saved-1992 (accessed on 28 August 2016).
- Anders, P.L.; Davis, E.L. Oral health of patients with intellectual disabilities: A systematic review. Spec. Care Dent. 2010, 30, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Waldman, H.B.; Perlman, S.P. Disability and rehabilitation: Do we ever think about needed dental care? A case study: The USA. Disabil. Rehabil. 2010, 32, 947–951. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Chen, Y.W.; Tsai, T.P.; Shih, W.Y. Oral health status of children with special health care needs receiving dental treatment under general anesthesia at the dental clinic of Taipei Veterans General Hospital in Taiwan. J. Chin. Med. Assoc. 2014, 77, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Daly, B.; Smith, K. Promoting good dental health in older people: Role of the community nurse. Br. J. Community Nurs. 2015, 20, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Perusini, D.J.; Llacuachaqui, M.; Sigal, M.J.; Dempster, L.J. Dental Students’ Clinical Expectations and Experiences Treating Persons with Disabilities. J. Dent. Educ. 2016, 80, 301–310. [Google Scholar] [PubMed]
- Murshid, E.Z. Oral health status, dental needs, habits and behavioral attitude towards dental treatment of a group of autistic children in Riyadh, Saudi Arabia. Saudi Dent. J. 2005, 17, 132–139. [Google Scholar]
- Al-Hussyeen, A. Child’s dental visits, oral health, knowledge and source of dental information among mothers of children with Down’s Syndrome in Riyadh. Saudi Dent. J. 2006, 18, 8–17. [Google Scholar]
- Brennan, D.S.; Spencer, A.J.; Roberts-Thomson, K.F. Tooth loss, chewing ability and quality of life. Qual. Life Res. 2008, 17, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Nelson, L.P.; Getzin, A.; Graham, D.; Zhou, J.; Wagle, E.M.; McQuiston, J.; McLaughlin, S.; Govind, A.; Sadof, M.; Huntington, N.L. Unmet dental needs and barriers to care for children with significant special health care needs. Pediatr. Dent. 2011, 33, 29–36. [Google Scholar] [PubMed]
- Williams, J.J.; Spangler, C.C.; Yusaf, N.K. Barriers to dental care access for patients with special needs in an affluent metropolitan community. Spec. Care Dent. 2015, 35, 190–196. [Google Scholar] [CrossRef] [PubMed]
- AL-Shehri, S.A. Access to dental care for persons with disabilities in Saudi Arabia (Caregivers’ perspective). J. Disabil. Oral Health 2012, 13, 51. [Google Scholar]
- Murshid, E.Z. Characteristics and dental experiences of autistic children in Saudi Arabia: Cross-sectional study. J. Autism Dev. Disord. 2011, 41, 1629–1634. [Google Scholar] [CrossRef] [PubMed]
- Watters, A.L.; Stabulas-Savage, J.; Toppin, J.D.; Janal, M.N.; Robbins, M.R. Incorporating Experiential Learning Techniques to Improve Self-Efficacy in Clinical Special Care Dentistry Education. J. Dent. Educ. 2015, 79, 1016–1023. [Google Scholar] [PubMed]
- Alkahtani, Z.M.; Stark, P.C.; Loo, C.Y.; Wright, W.G.; Morgan, J.P. Saudi and U.S. dental student attitudes toward treating individuals with developmental disabilities. J. Dent. Educ. 2014, 78, 1145–1153. [Google Scholar] [PubMed]
- Bandura, A. Self-Efficacy: The Exercise of Control; Freeman: New York, NY, USA, 1997. [Google Scholar]
- Buglar, M.E.; White, K.M.; Robinson, N.G. The role of self-efficacy in dental patients’ brushing and flossing: Testing an extended Health Belief Model. Patient Educ. Couns. 2010, 78, 269–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DiIorio, C.; Shafer, P.O.; Letz, R.; Henry, T.R.; Schomer, D.L.; Yeager, K. Behavioral, social, and affective factors associated with self-efficacy for self-management among people with epilepsy. Epilepsy Behav. 2006, 9, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.L.; Betz, N.E. Sources of social self-efficacy expectations: Their measurement and relation to career development. J. Vocat. Behav. 2001, 58, 98–117. [Google Scholar] [CrossRef]
- Al-Abdulwahab, S.S.; Al-Gain, S.I. Attitudes of Saudi Arabian health care professionals towards people with physical disabilities. Asia Pac. Disabil. Rehabil. J. 2003, 14, 63–70. [Google Scholar]
- AlSarheed, M.; Bedi, R.; Alkhatib, M.N.; Hunt, N.P. Dentists’ attitudes and practices toward provision of orthodontic treatment for children with visual and hearing impairments. Spec. Care Dent. 2006, 26, 30–36. [Google Scholar] [CrossRef]
- AlSarheed, M.; Bedi, R.; Hunt, N.P. Attitudes of dentists, working in Riyadh, toward people with a sensory impairment. Spec. Care Dent. 2001, 21, 113–116. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice-Hall: Upper Saddle River, NJ, USA, 1986. [Google Scholar]
- Thierer, T.; Meyerowitz, C. Education of dentists in the treatment of patients with special needs. J. Calif. Dent. Assoc. 2005, 33, 723–729. [Google Scholar] [PubMed]
- Waldman, B.; Al-Nowaiser, A.; Hamed, M.; Perlman, S. Dentistry for individuals with special needs in Saudi Arabia: A commentary. J. Disabil. Oral Health 2010, 11/2, 57–60. [Google Scholar]
- Abed, H. Special Care Dentistry in Saudi Arabia: Development as a Dental Specialty—An Opinion Paper. Available online: http://www.saudident.com/special-care-dentistry-in-saudi-arabia-development-as-a-dental-specialty-an-opinion-paper/ (accessed on 19 September 2017).
- Scambler, S.; Low, E.; Zoitopoulos, L.; Gallagher, J.E. Professional attitudes towards disability in special care dentistry. J. Disabil. Oral Health 2011, 12, 51–58. [Google Scholar]
- NSHR. The Chairman of the National Society for the Human Rights Participates in the 4th International Conference for Disability andRehabilitation. Available online: http://nshr.org.sa/en/?news=the-chairman-of-the-national-society-for-human-rights-participates-in-the-4th-international-conference-for-disability-and-rehabilitation (accessed on 11 November 2017).
- Baumeister, S.E.; Davidson, P.L.; Carreon, D.C.; Nakazono, T.T.; Gutierrez, J.J.; Andersen, R.M. What influences dental students to serve special care patients? Spec. Care Dent. 2007, 27, 15–22. [Google Scholar] [CrossRef]
- Jones, K.; Brennan, D.S.; Parker, E.J.; Mills, H.; Jamieson, L. Does self-efficacy mediate the effect of oral health literacy on self-rated oral health in an Indigenous population? J. Public Health Dent. 2016, 76, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Vozza, I.; Cavalle, E.; Corridore, D.; Ripari, F.; Spota, A.; Brugnoletti, O.; Guerra, F. Preventive strategies in oral health for special needs patients. Ann. Stomatol. 2015, 6, 96–99. [Google Scholar] [CrossRef] [PubMed]
- Halawany, H.S. Career motivations, perceptions of the future of dentistry and preferred dental specialties among saudi dental students. Open Dent. J. 2014, 8, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Al-Dlaigan, Y.H.; Albarakati, S.F.; Al-Habeeb, F.; Al-Hulaily, M. Career characteristics and postgraduate education of female dentist graduates of the College of Dentistry at King Saud University, Saudi Arabia. Saudi Dent. J. 2012, 24, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Nayak, P.P.; Prasad, K.V.; Jyothi, C.; Roopa, G.; Sanga, R. Preferences and barriers for continuing professional development among dental practitioners in the twin cities of Hubli-Dharwad, India. J. Indian Assoc. Public Health Dent. 2015, 13, 429. [Google Scholar] [CrossRef]
- Rajeh, M.; Nicolau, B.; Pluye, P.; Qutob, A.; Esfandiari, S. Are There Barriers for Professional Development of Women Dentists? A Qualitative Study in Saudi Arabia. JDR Clin. Transl. Res. 2017, 2, 119–131. [Google Scholar] [CrossRef]
- Cooper, B.R.; Monson, A.L. Allied restorative functions training in Minnesota: A case study. J. Dent. Educ. 2007, 71, 373–377. [Google Scholar] [PubMed]
- Skapetis, T.; Gerzina, T.; Hu, W. Managing dental emergencies: A descriptive study of the effects of a multimodal educational intervention for primary care providers at six months. BMC Med. Educ. 2012, 12, 103. [Google Scholar] [CrossRef] [PubMed]
- Al-Dabaan, R.; Asimakopoulou, K.; Newton, J.T. Effectiveness of a web-based child protection training programme designed for dental practitioners in Saudi Arabia: A pre- and post-test study. Eur. J. Dent. Educ. 2016, 20, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Ashri, N.; Al-Amro, H.; Hamadah, L.; Al-Tuwaijri, S.; El Metwally, A. Dental and medical practitioners’ awareness and attitude toward evidence based practice in Riyadh, Saudi Arabia. A comparative study. Saudi J. Dent. Res. 2014, 5, 109–116. [Google Scholar] [CrossRef]
- Bowling, A. Research Methods in Health: Investigating Health and Health Services; McGraw-Hill Education: Berkshire, UK, 2014. [Google Scholar]
- Trochim, W.M. Research Methods Knowledge Base. Available online: https://www.socialresearchmethods.net/kb/sampnon.phpcited-2006 (accessed on 16 June 2017).
- Hoffman, A.J. Enhancing self-efficacy for optimized patient outcomes through the theory of symptom self-management. Cancer Nurs. 2013, 36, E16–E26. [Google Scholar] [CrossRef] [PubMed]
- Yohannes, A.M.; Dodd, M.; Morris, J.; Webb, K. Reliability and validity of a single item measure of quality of life scale for adult patients with cystic fibrosis. Health Qual. Life Outcomes 2011, 9, 105. [Google Scholar] [CrossRef] [PubMed]
- Saudi Human Rights Commission. Available online: http://www.sa.undp.org/content/saudi_arabia/en/home/presscenter/articles/2017/01/10/hrc-and-ohchr-seminar-.html/2017 (accessed on 7 December 2017).
- Dougall, A.; Pani, S.; Thompson, S.; Faulks, D.; Romer, M.; Nunn, J. Developing an undergraduate curriculum in Special Care Dentistry-by consensus. Eur. J. Dent. Educ. 2013, 17, 46–56. [Google Scholar] [CrossRef]
| Variable | Males (N) | Females (N) | Total a N (%) |
|---|---|---|---|
| Age | |||
| ≤25–35 | 116 | 207 | 323 (62.4) |
| 36–45 | 76 | 49 | 125 (24.1) |
| 46–55 | 23 | 34 | 57 (11.0) |
| 56–65 | 6 | 5 | 11 (2.1) |
| ≥66 | 2 | 0 | 2 (0.4) |
| Place of work | |||
| Government education institute | 86 | 120 | 207 (39.9) |
| Private clinic | 53 | 71 | 124 (24.0) |
| Private education institute | 12 | 40 | 52 (10.1) |
| Government hospital | 60 | 49 | 109 (21.1) |
| Private general hospital | 12 | 13 | 25 (4.8) |
| Years of experience | |||
| ≤10 years | 150 | 218 | 368 (71.2) |
| ≥11 years | 73 | 76 | 149 (28.8) |
| Degree/certificate attained | |||
| Bachelor (BDS †) degree | 75 | 155 | 230 (44.8) |
| Master degree | 56 | 77 | 133 (25.9) |
| Board certification | 49 | 26 | 75 (14.6) |
| Doctorate/PhD degree | 24 | 19 | 43 (8.4) |
| Other (e.g., fellowship) | 16 | 16 | 32 (6.2) |
| Origin of highest degree | |||
| North America or Europe | 68 | 33 | 101 (19.8) |
| Elsewhere i.e., Local (Saudi Arabia), Asia, Africa | 152 | 258 | 410 (80.2) |
| Variable | Males (N) | Females (N) | Total a N (%) |
|---|---|---|---|
| Attended workshop for managing AMPD | |||
| Yes | 41 | 55 | 96 (18.4) |
| No | 182 | 243 | 425 (81.6) |
| Interest in attending workshop for managing AMPD in the future | |||
| Yes | 158 | 228 | 386 (74.1) |
| No | 65 | 70 | 135 (25.9) |
| Interest in treating patients with PD a,b | |||
| Yes | 169 | 212 | 382 (73.1) |
| No | 54 | 86 | 140 (26.9) |
| Interest in treating patients with MD † | |||
| Yes | 123 | 142 | 265 (50.9) |
| No | 156 | 100 | 256 (49.1) |
| Attitude towards treating AMPD | |||
| Try to examine and treat | 144 | 163 | 307 (58.9) |
| Examine and refer or refer directly | 64 | 80 | 144 (27.6) |
| Other responses | 15 | 55 | 70 (13.4) |
| Previous experience in managing AMPD | |||
| Negative or extremely negative | 26 | 24 | 48 (9.2) |
| Positive or extremely positive | 144 | 137 | 281 (53.9) |
| Had no previous experience | 60 | 132 | 192 (36.9) |
| Managed to complete the treatment for AMPD in the dental clinic (with or without conscious sedation) * | |||
| Yes | 135 | 128 | 263 (79.9) |
| No | 28 | 38 | 66 (20.1) |
| Self-efficacy in managing AMPD | |||
| Low | 39 | 90 | 129 (24.9) |
| Moderate | 131 | 185 | 316 (60.9) |
| High | 52 | 22 | 74 (14.2) |
| Variable | Category | N (%) | OR | 95% CI | p |
|---|---|---|---|---|---|
| Gender | Female | 22 (7.4) | 0.0005 | ||
| Male | 52 23.4) | 3.82 | 2.24–6.52 | ||
| Age | ≤45 Years | 54 (12.1) | 0.001 | ||
| ≥46 Years | 19 (27.5) | 2.77 | 1.52–5.05 | ||
| Education | Bachelor degree | 19 (8.3) | 0.001 | ||
| Postgraduate training | 53 (18.8) | 2.57 | 1.47–4.48 | ||
| Origin of degree | Elsewhere | 45 (11.0) | 0.0001 | ||
| North America and Europe | 28 (28.0) | 3.15 | 1.84–5.38 | ||
| Rank | Other | 23 (8.0) | 0.0001 | ||
| Consultant/specialist | 50 (21.9) | 3.22 | 1.90–5.47 | ||
| Specialty | Other specialties | 65 (13.3) | 0.008 | ||
| Pediatric dentistry | 7 (38.9) | 4.16 | 1.58–11.12 | ||
| Years of experience | ≤10 Years | 34 (9.3) | 0.0001 | ||
| ≥11 Years | 40 (26.8) | 3.26 | 2.17–5.96 | ||
| Previous experience in managing AMPD | No | 6 (3.1) | 0.0001 | ||
| Yes | 68 (20.7) | 8.11 | 3.45–19.18 | ||
| Aware of rules for managing AMPD | No | 29 (8.6) | 0.0001 | ||
| Yes | 43 (27.0) | 3.96 | 2.63–6.65 | ||
| Attended workshop on AMPD management | No | 50 (11.8) | 0.001 | ||
| Yes | 24 (24.7) | 2.45 | 1.42–4.25 |
| Explanatory Variable | Categories | Wald Value | AOR (95% CI) | p-Value |
|---|---|---|---|---|
| Gender | Female | 5.64 | 1 | 0.018 |
| Male | 2.39 (1.16–4.89) | |||
| Age x Gender | 4.85 | 6.45 (1.23–33.91) | 0.028 | |
| Years of experience | ≤10 Years | 4.28 | 1 | 0.039 |
| ≥11 years | 2.19 (1.04–4.47) | |||
| Specialty | Other specialties | 5.93 | 1 | 0.015 |
| Pediatric dentistry | 3.98 (1.31–12.07) | |||
| Previous experience in managing AMPD | No | 8.36 | 1 | 0.004 |
| Yes | 4.23 (1.59–11.22) | |||
| Aware of rules for managing AMPD | No | 7.49 | 1 | 0.002 |
| Yes | 2.62 (1.42–4.38) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
AlQahtani, S.; Murshid, E.Z.; Fadel, H.T.; Kassim, S. Practicing Dentists’ Self-Efficacy and Associated Factors in Managing the Treatment of Adults with Mental and Physical Disabilities: An Exploratory Cross-Sectional Study in Riyadh, Saudi Arabia. Int. J. Environ. Res. Public Health 2017, 14, 1549. https://doi.org/10.3390/ijerph14121549
AlQahtani S, Murshid EZ, Fadel HT, Kassim S. Practicing Dentists’ Self-Efficacy and Associated Factors in Managing the Treatment of Adults with Mental and Physical Disabilities: An Exploratory Cross-Sectional Study in Riyadh, Saudi Arabia. International Journal of Environmental Research and Public Health. 2017; 14(12):1549. https://doi.org/10.3390/ijerph14121549
Chicago/Turabian StyleAlQahtani, Sakher, Ebtissam Zakaria Murshid, Hani Talal Fadel, and Saba Kassim. 2017. "Practicing Dentists’ Self-Efficacy and Associated Factors in Managing the Treatment of Adults with Mental and Physical Disabilities: An Exploratory Cross-Sectional Study in Riyadh, Saudi Arabia" International Journal of Environmental Research and Public Health 14, no. 12: 1549. https://doi.org/10.3390/ijerph14121549






