The Optimal Ethnic-Specific Waist-Circumference Cut-Off Points of Metabolic Syndrome among Low-Income Rural Uyghur Adults in Far Western China and Implications in Preventive Public Health
Abstract
:1. Introduction
2. Methods
2.1. Ethics Statement
2.2. Settings and Study Population
2.3. Questionnaire Survey
2.4. Physical Examinations
2.5. Biochemical Measurements
2.6. Definitions
2.7. Statistical Analysis
3. Results
3.1. Characteristics of the Study Populations
3.2. Relationship between WC and the Components of Metabolic Syndrome Based on IDF Criteria
3.3. The Optimal Ethnic-Specific WC Cut-Off Values of Metabolic Syndrome among Low-Income Rural Uyghur Adults
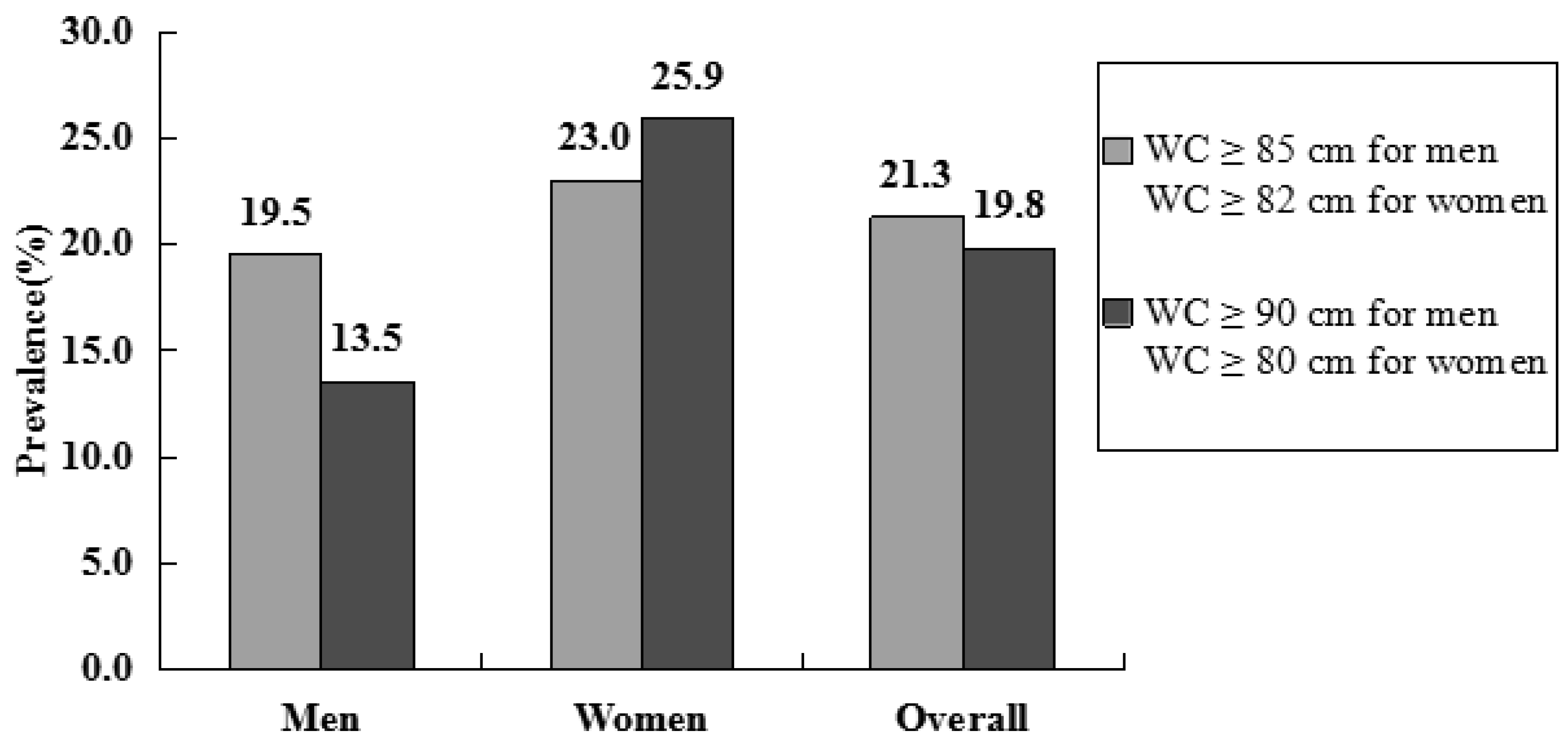
3.4. Prevalence Rates of Metabolic Syndrome Using the Ethnic-Specific and Traditional WC Cut-Off Values by IDF Criteria
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Weiss, R.; Bremer, A.A.; Lustig, R.H. What is metabolic syndrome, and why are children getting it? Ann. N.Y. Acad. Sci. 2013, 1281, 123–140. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: A summary of the evidence. Diabetes Care 2005, 28, 1769–1778. [Google Scholar] [CrossRef] [PubMed]
- Beydoun, M.A.; Kuczmarski, M.T.F.; Wang, Y.; Mason, M.A.; Evans, M.K.; Zonderman, A.B. Receiver-operating characteristics of adiposity formetabolic syndrome: The Healthy Aging in Neighborhoods of Diversity across the Life Span (HANDLS) study. Public Health Nutr. 2011, 14, 77–92. [Google Scholar] [CrossRef] [PubMed]
- Nikolopoulou, A.; Kadoglou, N.P. Obesity and metabolic syndrome as related to cardiovascular disease. Expert Rev. Cardiovasc. Ther. 2012, 10, 933–939. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Katashima, M.; Yasumasu, T.; Li, K.J. Visceral fat area, waist circumference and metabolic risk factors in abdominally obese Chinese adults. Biomed. Environ. Sci. 2012, 25, 141–148. [Google Scholar] [PubMed]
- Takahashi, M.; Shimomura, K.; Proks, P.; Craig, T.J.; Negishi, M.; Akuzawa, M.; Hayashi, R.; Shimomura, Y.; Kobayashi, I. A proposal of combined evaluation of waist circumference and BMI for the diagnosis of metabolic syndrome. Endocr. J. 2009, 56, 1079–1082. [Google Scholar] [CrossRef] [PubMed]
- Ko, K.P.; Oh, D.K.; Min, H.; Kim, C.S.; Park, J.K.; Kim, Y.; Kim, S.S. Prospective study of optimal obesity index cutoffs for predicting development of multiple metabolic risk factors: The Korean genome and epidemiology Study. J. Epidemiol. 2012, 22, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Gharipour, M.; Sarrafzadegan, N.; Sadeghi, M.; Andalib, E.; Talaie, M.; Shafie, D.; Aghababaie, E. Predictors of metabolic syndrome in the Iranian population: Waist circumference, body mass index, or waist to hip ratio? Cholesterol 2013, 2013, 198384. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Huang, W.; Qian, J.; Jin, L. Analysis of genomic admixture in Uyghur and its implication in mapping strategy. Am. J. Hum. Genet. 2008, 82, 883–894. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.; Xie, Z.; Zhang, H.; Zhang, L.; Gao, J. The appropriate cut-off point of waist circumference for identifying metabolic syndrome in Chinese Uygur adults. Chin. J. Diabetes 2008, 16, 79–82. [Google Scholar]
- Wang, Y.; Zhao, L.; Song, X.; Zhang, F.; Ma, Y.; Wu, L.; Ge, J.P.; Xu, Y.C. Recommendations for waist circumference cut-off points for metabolic syndrome diagnosis in Han, Uygur, and Kazak subjects in Xinjiang, China. Chin. J. Diabetes 2012, 20, 907–909. [Google Scholar]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; Report of a WHO consultation; World Health Organization Technical Report Series; WHO: Geneva, Switzerland, 2000; Volume 894, pp. 1–253. [Google Scholar]
- Alberti, K.G.; Zimmet, P.; Shaw, J.; IDF Epidemiology Task Force Consensus Group. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Bewick, V.; Cheek, L.; Ball, J. Statistics review 13: Receiver operating characteristic curves. Crit. Care 2004, 8, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Bener, A.; Yousafzai, M.T.; Darwish, S.; Al-Hamaq, A.O.; Nasralla, E.A.; Abdul-Ghani, M. Obesity index that better predict metabolic syndrome: Body mass index, waist circumference, waist hip ratio, or waist height ratio. J. Obes. 2013, 2013, 269038. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.J.; Ho, C.; Chen, H.J.; Huang, N.; Yeh, J.C.; deFerranti, S. Is the 90th Percentile Adequate? The Optimal Waist Circumference Cutoff Points for Predicting Cardiovascular Risks in 124,643 15-Year-Old Taiwanese Adolescents. PLoS ONE 2016, 11, e0158818. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Bray, G.A.; Greenway, F.L.; Johnson, W.D.; Newton, R.L., Jr.; Ravussin, E.; Ryan, D.H.; Bouchard, C. Ethnic-specific BMI and waist circumference thresholds. Obesity (Silver Spring) 2011, 19, 1272–1278. [Google Scholar] [CrossRef] [PubMed]
- Bao, Y.; Lu, J.; Wang, C.; Yang, M.; Li, H.; Zhang, X.; Zhu, J.; Lu, H.; Jia, W.; Xiang, K. Optimal waist circumference cutoffs for abdominal obesity in Chinese. Atherosclerosis 2008, 201, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Hou, X.; Lu, J.; Weng, J.; Ji, L.; Shan, Z.; Liu, J.; Tian, H.; Ji, Q.; Zhu, D.; Ge, J.; et al. Impact of waist circumference and body mass index on risk of cardiometabolic disorder and cardiovascular disease in Chinese adults: A national diabetes and metabolic disorders survey. PLoS ONE 2013, 8, e57319. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, D.; Kahara, K.; Shigematsu, T.; Fujii, S.; Hayakawa, N. Optimal cut-off point of waist circumference for the diagnosis of metabolic syndrome in Japanese subjects. J. Diabetes Investig. 2010, 1, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.K.; Kim, C.H.; Park, J.Y.; Lee, K.U. Lower waist-circumference cutoff point for the assessment of cardiometabolic risk in Koreans. Diabetes Res. Clin. Pract. 2009, 85, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.E.; Ma, S.; Wai, D.; Chew, S.K.; Tai, E.S. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care 2004, 27, 1182–1186. [Google Scholar] [CrossRef] [PubMed]
- Misra, A.; Wasir, J.S.; Pandey, R.M. An evaluation of candidate definitions of the metabolic syndrome in adult Asian Indians. Diabetes Care 2005, 28, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Gozashti, M.H.; Najmeasadat, F.; Mohadeseh, S.; Najafipour, H. Determination of most suitable cut off point of waist circumference for diagnosis of metabolic syndrome in Kerman. Diabetes Metab. Syndr. 2014, 8, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.C.; Lai, Y.X.; Shan, Z.Y.; Jia, W.P.; Yang, W.Y.; Lu, J.M.; Weng, J.P.; Ji, L.N.; Liu, J.; Tian, H.M.; et al. Effectiveness of different waist circumference cut-off values in predicting metabolic syndrome prevalence and risk factors in adults in China. Biomed. Environ. Sci. 2014, 27, 325–334. [Google Scholar] [PubMed]
- Sarrafzadegan, N.; Kelishadi, R.; Baghaei, A.; Hussein Sadri, G.; Malekafzali, H.; Mohamma-difard, N.; Rabiei, K.; Bahonar, A.; Sadeghi, M.; O’Laughlin, J. Metabolic syndrome: An emerging public health problem in Iranian Women: Isfahan Healthy Heart Program. Int. J. Cardiol. 2008, 131, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Seo, J.A.; Kim, B.G.; Cho, H.; Kim, H.S.; Park, J. The cutoff values of visceral fat area and waist circumference for identifying subjects at risk for metabolic syndrome in elderly Korean: Ansan Geriatric (AGE) cohort study. BMC Public Health 2009, 9, 443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the Third Report on the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 265, 2486–2497. [Google Scholar]
- Gu, D.; Reynolds, K.; Wu, X.; Chen, J.; Duan, X.; Reynolds, R.F.; Whelton, P.K.; He, J.; InterASIA Collaborative Group. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet 2005, 365, 1398–1405. [Google Scholar] [CrossRef]
- He, J.; Guo, S.; Liu, J.; Zhang, M.; Ding, Y.; Zhang, J.; Li, S.; Xu, S.; Niu, Q.; Guo, H.; et al. Ethnic Differences in Prevalence of General Obesity and Abdominal Obesity among Low-Income Rural Kazakh and Uyghur Adults in Far Western China and Implications in Preventive Public Health. PLoS ONE 2014, 9, e106723. [Google Scholar] [CrossRef] [PubMed]
- Delavari, A.; Forouzanfar, M.H.; Alikhani, S.; Sharifian, A.; Kelishadi, R. First nationwide study of the prevalence of the metabolic syndrome and optimal cutoff points of waist circumference in the Middle East: The national survey of risk factors for noncommunicable diseases of Iran. Diabetes Care 2009, 32, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Motala, A.A.; Esterhuizen, T.; Pirie, F.J.; Omar, M.A. The Prevalence of Metabolic Syndrome and Determination of the Optimal Waist Circumference Cutoff Points in a Rural South African Community. Diabetes Care 2011, 34, 1032–1037. [Google Scholar] [CrossRef] [PubMed]
- Crowther, N.J.; Norris, S.A. The Current Waist Circumference Cut Point Used for the Diagnosis of Metabolic Syndrome in Sub-Saharan African Women Is Not Appropriate. PLoS ONE 2012, 7, e48883. [Google Scholar] [CrossRef] [PubMed]
- Yao, M.H.; He, J.; Ma, R.L.; Ding, Y.S.; Guo, H.; Yan, Y.Z.; Zhang, J.Y.; Liu, J.M.; Zhang, M.; Rui, D.S.; et al. Association between Polymorphisms and Haplotype in the ABCA1 Gene and Overweight/Obesity Patients in the Uyghur Population of China. Int. J. Environ. Res. Public Health 2016, 13, 220. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Hu, Y.; Ding, Y.; Liu, J.; Zhang, M.; Ma, R.; Guo, H.; Wang, K.; He, J.; Yan, Y.; et al. Association between Eight Functional Polymorphisms and Haplotypes in the Cholesterol Ester Transfer Protein (CETP) Gene and Dyslipidemia in National Minority Adults in the Far West Region of China. Int. J. Environ. Res. Public Health 2015, 12, 15979–15992. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Lu, W.; Jia, J.; Zhang, S.; Shi, L.; Li, Y.; Yang, Q.; Kan, H. Relationships between indices of obesity and its cardiovascular comorbidities in a Chinese population. Circ. J. 2008, 72, 973–978. [Google Scholar] [CrossRef] [PubMed]
- Cong, L.; Zhan, J.Q.; Yang, L.; Zhang, W.; Li, S.G.; Chen, C.; Zhang, H.Y.; Ma, Z.P.; Hao, X.L.; Simayi, D.; et al. Overweight and Obesity among Low-Income Muslim Uyghur Women in Far Western China: Correlations of Body Mass Index with Blood Lipids and Implications in Preventive Public Health. PLoS ONE 2014, 9, e90262. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.J.; Li, F.; Wang, Y.H.; Simayi, D.; Saimaiti, A.; Zou, X.G.; Xiong, C.L.; Gong, F.L.; Cao, Y.G. The case for semi-mandatory HPV vaccination in China. Nat. Biotechnol. 2013, 31, 590–591. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Pang, H.; Guo, H.; Zhang, M.; He, J.; Yan, Y.; Niu, Q.; Muratbek; Rui, D.; Li, S.; et al. Ethnic differences in the prevalence of high homocysteine levels among low-income rural Kazakh and Uyghur adults in far western China and its implications for preventive public health. Int. J. Environ. Res. Public Health 2015, 12, 5373–5385. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, J.; Ding, Y.; Zhang, M.; Liu, J.; Ma, J.; Guo, H.; Yan, Y.; He, J.; Wang, K.; et al. Prevalence of Hypertension among Adults in Remote Rural Areas of Xinjiang, China. Int. J. Environ. Res. Public Health 2016, 13, 524. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Men | Women | Total |
|---|---|---|---|
| n | 1728 | 1814 | 3542 |
| Age (years) # | 42.58 ± 16.18 | 43.13 ± 15.82 | 42.86 ± 15.99 |
| Age-group (years) ## | |||
| 18–24 | 254 (14.7) | 248 (13.7) | 502 (14.2) |
| 25–34 | 373 (21.6) | 369 (20.3) | 742 (20.9) |
| 35–44 | 391 (22.6) | 420 (23.2) | 811 (22.9) |
| 45–54 | 288 (16.7) | 315 (17.4) | 603 (17.0) |
| 55–64 | 228 (13.2) | 269 (14.8) | 497 (14.0) |
| ≥65 | 194 (11.2) | 193 (10.6) | 387 (10.9) |
| WC (cm) # | 85.15 ± 9.50 * | 82.77 ± 10.93 | 83.93 ± 10.32 |
| SBP (mmHg) # | 126.84 ± 18.96 * | 122.87 ± 21.55 | 124.81 ± 20.42 |
| DBP (mmHg) # | 79.95 ± 12.30 * | 76.94 ± 13.30 | 78.41 ± 12.91 |
| TG (mmol/L) # | 1.37 ± 1.20 * | 1.19 ± 0.75 | 1.28 ± 1.00 |
| HDL-C (mmol/L) # | 1.18 ± 0.62 * | 1.28 ± 0.66 | 1.23 ± 0.64 |
| FPG (mmol/L) # | 4.45 ± 1.10 * | 4.33 ± 1.04 | 4.39 ± 1.07 |
| High blood pressure (%) ** | 46.8 * | 36.8 | 41.7 |
| Low HDL-C (%) ** | 43.7 * | 67.2 | 55.7 |
| High TG (%) ** | 22.0 * | 17.0 | 19.4 |
| High FPG (%) ** | 6.5 * | 4.6 | 5.5 |
| WC (cm) | n | One or More Components # | Two or More Components # | ||
|---|---|---|---|---|---|
| n | Risk * | n | Risk * | ||
| Men | |||||
| <80 | 486 | 322 | 1.00 | 103 | 1.00 |
| 80–84 | 431 | 319 | 1.38 (1.04–1.84) | 124 | 1.45 (1.07–1.97) |
| 85–89 | 295 | 224 | 1.49 (1.07–2.07) | 103 | 1.88 (1.35–2.60) |
| 90–94 | 235 | 193 | 2.03 (1.37–3.00) | 83 | 1.80 (1.26–2.56) |
| 95–99 | 137 | 118 | 2.80 (1.65–4.77) | 66 | 3.12 (2.08–4.70) |
| 100–104 | 85 | 82 | 11.48 (3.55–37.07) | 50 | 4.57 (2.79–7.49) |
| ≥105 | 59 | 53 | 3.84 (1.60–9.20) | 35 | 4.69 (2.65–8.30) |
| χ2trend | 64.242 | 94.014 | |||
| p value | <0.001 | <0.001 | |||
| Women | |||||
| <75 | 441 | 324 | 1.00 | 80 | 1.00 |
| 75–79 | 293 | 240 | 1.56 (1.07–2.26) | 75 | 1.34 (0.92–1.94) |
| 80–84 | 351 | 282 | 1.34 (0.95–1.89) | 127 | 2.25 (1.61–3.15) |
| 85–89 | 278 | 228 | 1.46 (1.00–2.15) | 109 | 2.26 (1.58–3.22) |
| 90–94 | 188 | 168 | 2.58 (1.54–4.33) | 89 | 3.20 (2.17–4.71) |
| 95–99 | 130 | 116 | 2.51 (1.38–4.58) | 65 | 3.49 (2.26–5.40) |
| ≥100 | 133 | 125 | 4.70 (2.22–9.96) | 79 | 5.05 (3.26–7.81) |
| χ2trend | 46.283 | 129.871 | |||
| p value | <0.001 | <0.001 | |||
| Gender | WC (cm) | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Youden Index |
|---|---|---|---|---|---|---|
| Men | ||||||
| ≥80 | 81.7 | 32.9 | 37.1 | 78.8 | 0.146 | |
| ≥81 | 75.7 | 39.9 | 37.9 | 77.2 | 0.156 | |
| ≥82 | 72.9 | 44.0 | 38.7 | 77.0 | 0.169 | |
| ≥83 | 67.6 | 50.2 | 39.6 | 76.1 | 0.178 | |
| ≥84 | 63.7 | 55.2 | 40.7 | 75.8 | 0.189 | |
| ≥85 | 60.0 | 59.3 | 41.6 | 75.2 | 0.193 | |
| ≥86 | 56.1 | 63.1 | 42.4 | 74.8 | 0.192 | |
| ≥87 | 53.0 | 66.1 | 43.1 | 74.4 | 0.191 | |
| ≥88 | 49.8 | 69.2 | 44.0 | 74.0 | 0.190 | |
| ≥89 | 44.7 | 72.9 | 44.4 | 73.1 | 0.176 | |
| ≥90 | 41.5 | 75.8 | 45.3 | 72.8 | 0.173 | |
| ≥95 | 26.8 | 88.8 | 53.7 | 71.5 | 0.156 | |
| ≥100 | 15.1 | 94.9 | 59.0 | 69.8 | 0.100 | |
| ≥105 | 6.2 | 97.6 | 59.3 | 68.3 | 0.038 | |
| Women | ||||||
| ≥75 | 87.2 | 30.3 | 39.6 | 81.9 | 0.175 | |
| ≥80 | 75.2 | 48.7 | 43.4 | 78.9 | 0.239 | |
| ≥81 | 69.4 | 53.6 | 44.0 | 77.0 | 0.230 | |
| ≥82 | 67.0 | 57.3 | 45.1 | 76.8 | 0.243 | |
| ≥83 | 61.5 | 61.1 | 45.3 | 75.2 | 0.226 | |
| ≥84 | 57.7 | 64.0 | 45.7 | 74.3 | 0.217 | |
| ≥85 | 54.8 | 67.5 | 46.9 | 74.0 | 0.223 | |
| ≥86 | 50.2 | 71.3 | 47.9 | 73.2 | 0.215 | |
| ≥87 | 46.2 | 74.9 | 49.1 | 72.6 | 0.211 | |
| ≥88 | 43.1 | 77.1 | 49.7 | 72.1 | 0.202 | |
| ≥89 | 39.9 | 79.9 | 51.0 | 71.7 | 0.198 | |
| ≥90 | 37.4 | 81.7 | 51.7 | 71.3 | 0.191 | |
| ≥95 | 23.1 | 90.0 | 54.8 | 69.1 | 0.131 | |
| ≥100 | 12.7 | 95.5 | 59.4 | 67.6 | 0.082 |
| Country [Reference Number] | n | Prevalence of Metabolic Syndrome (%) | Cut-Off Point for Men (cm) | Cut-Off Point for Women (cm) |
|---|---|---|---|---|
| Japan [20] | 5972 | 32.8 # | 84 | 80 |
| Singapore [22] | 4723 | 17.9 * | 90 | 80 |
| India [23] | 640 | 29.9 * | 90 | 80 |
| Korea [21] | 31,076 | - | 83 | 76 |
| Iran [24] | 5332 | 30.4 & | 89 | 86 |
| China [25] | 47,325 | 24.2 & | 90 | 85 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
He, J.; Ma, R.; Liu, J.; Zhang, M.; Ding, Y.; Guo, H.; Mu, L.; Zhang, J.; Wei, B.; Yan, Y.; et al. The Optimal Ethnic-Specific Waist-Circumference Cut-Off Points of Metabolic Syndrome among Low-Income Rural Uyghur Adults in Far Western China and Implications in Preventive Public Health. Int. J. Environ. Res. Public Health 2017, 14, 158. https://doi.org/10.3390/ijerph14020158
He J, Ma R, Liu J, Zhang M, Ding Y, Guo H, Mu L, Zhang J, Wei B, Yan Y, et al. The Optimal Ethnic-Specific Waist-Circumference Cut-Off Points of Metabolic Syndrome among Low-Income Rural Uyghur Adults in Far Western China and Implications in Preventive Public Health. International Journal of Environmental Research and Public Health. 2017; 14(2):158. https://doi.org/10.3390/ijerph14020158
Chicago/Turabian StyleHe, Jia, Rulin Ma, Jiaming Liu, Mei Zhang, Yusong Ding, Heng Guo, Lati Mu, Jingyu Zhang, Bin Wei, Yizhong Yan, and et al. 2017. "The Optimal Ethnic-Specific Waist-Circumference Cut-Off Points of Metabolic Syndrome among Low-Income Rural Uyghur Adults in Far Western China and Implications in Preventive Public Health" International Journal of Environmental Research and Public Health 14, no. 2: 158. https://doi.org/10.3390/ijerph14020158





