Interventions for Preventing Childhood Obesity with Smartphones and Wearable Device: A Protocol for a Non-Randomized Controlled Trial
Abstract
:1. Introduction
2. Methods
2.1. Study Participants
2.1.1. Control Group
2.1.2. Intervention Group
HAPPY ME Platform
Intervention for Children
Intervention for Parents
Intervention for Teachers
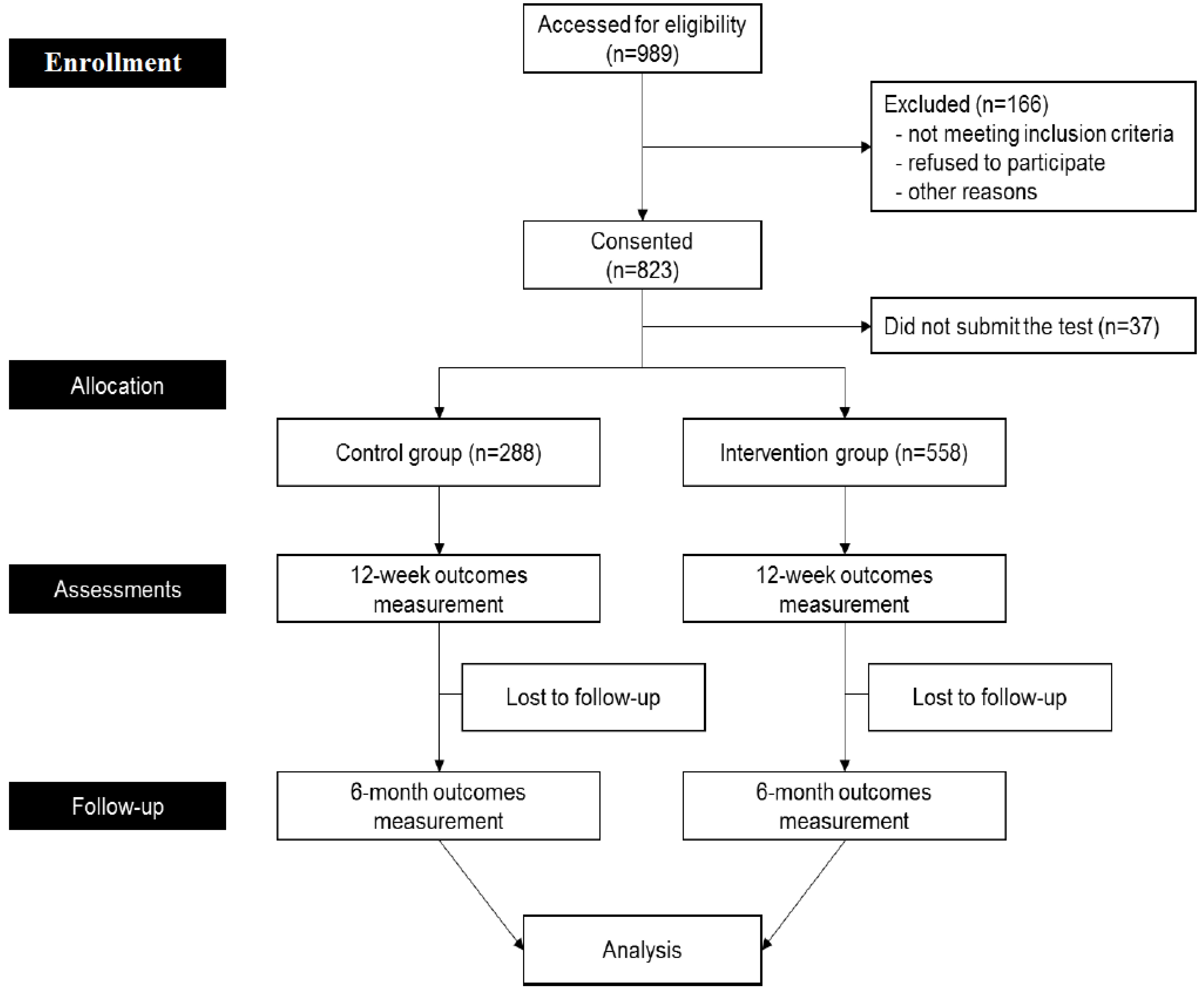
2.2. Study Design
2.2.1. Phase 1: Safety Test
2.2.2. Phase 2: Efficacy Test
2.2.3. Phase 3: Long-Term Effect Test
2.3. Data Collection
2.4. Statistical Analysis
2.5. Ethical Aspects of the Study
3. Discussion
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Oh, K.; Jang, M.J.; Lee, N.Y.; Moon, J.S.; Lee, C.G.; Yoo, M.H.; Kim, Y.T. Prevalence and trends in obesity among Korean children and adolescents in 1997 and 2005. Korean J. Pediatr. 2008, 51, 950–955. [Google Scholar] [CrossRef]
- OECD. Overweight and obesity among children. In Health at a Glance 2015 ed; OECD Publishing: Paris, France, 2015; pp. 76–77. [Google Scholar]
- Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/obesity/childhood/defining.html (accessed on 19 November 2015).
- Ogden, C.L.; Yanovski, S.Z.; Carroll, M.D.; Flegal, K.M. The epidemiology of obesity. Gastroenterology 2007, 132, 2087–2102. [Google Scholar] [CrossRef] [PubMed]
- Ebbeling, C.B.; Pawlak, D.B.; Ludwig, D.S. Childhood obesity: Public-health crisis, common sense cure. Lancet 2002, 360, 473–482. [Google Scholar] [CrossRef]
- Waters, E.; de Silva-Sanigorski, A.; Burford, B.J.; Brown, T.; Campbell, K.J.; Summerbell, C.D. Interventions for preventing obesity in children (Review). Cochrane Database Syst. Rev. 2011, 12. [Google Scholar] [CrossRef]
- Sisson, S.B.; Krampe, M.; Anundson, K.; Castle, S. Obesity prevention and obesogenic behavior interventions in child care: A systematic review. Prev. Med. 2016, 87, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Benjamin Neelon, S.E.; Ostbye, T.; Hales, D.; Vaughn, A.; Ward, D.S. Preventing childhood obesity in early care and education settings: Lessons from two intervention studies. Child Care Health Dev. 2016, 42, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Eldridge, G.; Paul, L.; Bailey, S.J.; Ashe, C.B.; Martz, J.; Lynch, W. Effects of parent-only childhood obesity prevention programs on BMIz and body image in rural preteens. Body Image 2016, 16, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Lazorick, S.; Fang, X.; Crawford, Y. The MATCH Program: Long-Term Obesity Prevention through a Middle School Based Intervention. Child Obes. 2016, 12, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Granado-Font, E.; Flores-Mateo, G.; Sorli-Aguilar, M.; Montana-Carreras, X.; Ferre-Grau, C.; Barrera-Uriarte, M.L.; Oriol-Colominas, E.; Rey-Renones, C.; Caules, I.; Satue-Gracia, E.M. Effectiveness of a Smartphone application and wearable device for weight loss in overweight or obese primary care patients: Protocol for a randomised controlled trial. BMC Public Health 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, S.S.; Whitehead, M.; Sheats, J.Q.; Mastromonico, J.; Smith, S. A Review of Smartphone Applications for Promoting Physical Activity. Jacobs J. Community Med. 2016, 2, 1–13. [Google Scholar]
- Wang, Y.; Cai, L.; Wu, Y.; Wilson, R.F.; Weston, C.; Segal, J. What Childhood Obesity Prevention Programs work? A systemic review and Meta-Aanalysis. Obes. Rev. 2015, 16, 547–565. [Google Scholar] [CrossRef] [PubMed]
- Avis, J.L.; Cave, A.L.; Donaldson, S.; Ellendt, C.; Holt, N.L.; Jelinski, S.; Martz, P.; Maximova, K.; Padwal, R.; Wild, T.C.; et al. Working With Parents to Prevent Childhood Obesity: Protocol for a Primary Care-Based eHealth Study. JMIR Res. Protoc. 2015, 4. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.J.; Morgan, P.J.; Plotnikoff, R.C.; Dally, K.A.; Salmon, J.; Okely, A.D.; Finn, T.L.; Babic, M.J.; Skinner, G.; Lubans, D.R. Rationale and study protocol for the “active teen leaders avoiding screen-time” (ATLAS) group randomized controlled trial: An obesity prevention intervention for adolescent boys from schools in low-income communities. Contemp. Clin. Trials 2014, 37, 106–119. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Joh, H.K.; Yun, J.M.; Kwon, H.T.; Lee, H.; Min, H.; Shin, J.H.; Chung, W.J.; Park, J.H.; Cho, B. Design and baseline characteristics of participants in the Enhancing Physical Activity and Reducing Obesity through Smartcare and Financial Incentives (EPAROSFI): A pilot randomized controlled trial. Contemp. Clin. Trials 2016, 47, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Carriere, C.; Cabaussel, C.; Bader, C.; Barberger-Gateau, P.; Thilbault, H. Multidisciplinary care management has a positive effect on pediatric obesity and social and individual factors are associated with better outcomes. Acta Paediatr. 2016, 105, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Amini, M.; Djazayery, A.; Taghdisi, M.H.; Nourmohammadi, M. A school-based intervention to reduce excess weight in overweight and obese primary school students. Biol. Res. Nurs. 2016, 18, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Franklin, C.G.; Kim, J.S.; Montgomery, K.L. Teacher involvement in school mental health interventions: A systematic review. Child Youth Serv. Rev. 2012, 34, 973–982. [Google Scholar] [CrossRef]
- Jane, M.; Foster, J.; Hagger, M.; Pal, S. Using new technologies to promote weight management: A randomised controlled trial study protocol. BMC Public Health 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Park, B.K.; Nahm, E.S.; Rogers, V.E.; Choi, M.; Friedmann, E.; Wilson, M.; Koru, G. A Facebook-Based Obesity Prevention Program for Korean American Adolescents: Usability Evaluation. J. Pediatr. Health Care 2017, 1, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Wilkie, H.J.; Standage, M.; Gillison, F.B.; Cumming, S.P.; Katzmarzyk, P.T. Multiple lifestyle behaviors and overweight and obesity among children aged 9–11 years: Results from the UK site of the International Study of Childhood Obesity, Lifestyle and the Environment. BMJ Open 2016, 6. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.A.; Park, H. The mediation effect of individual eating behaviors on the relationship between socioeconomic status and dietary quality in children: The Korean National Health and Nutrition Examination Survey. Eur. J. Nutr. 2016, 56. [Google Scholar] [CrossRef]
- Neufel, N.D. Outcome analysis of the B.E. S.T.R.O.N.G. Childhood obesity treatment program: Effectiveness of an eight-week family-based childhood obesity program using an internet-based health tracker. Child Obes. 2016, 12, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Rollo, M.E.; Aquiar, E.J.; Collins, C.E. eHealth technologies to support nutrition and physical activity behaviors in diabetes self-management. Diabetes Metab. Syndr. Obes. 2016, 4, 381–390. [Google Scholar] [CrossRef] [PubMed]
- Schoeppe, S.; Alley, S.; Van Lippevelde, W.; Vandelanotte, C. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behavior: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 127. [Google Scholar] [CrossRef] [PubMed]
- Fisher, E.B.; Fitzgibbon, M.L.; Glasgow, R.E.; Haire-Joshu, D.; Hayman, L.L.; Kaplan, R.M.; Nanney, M.S.; Ockene, J.K. Behavior matters. Am. J. Prev. Med. 2011, 40, e15–e30. [Google Scholar] [CrossRef] [PubMed]
- Tate, E.B.; Spruijt-Metz, D.; O’Reilly, G.; Jordan-Marsh, M.; Gotsis, M.; Dunton, G.F. mHealth approaches to child obesity prevention: Successes, unique challenges, and next directions. TBM 2013, 3, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.D.; Duncombe, K.M.; Woolford, S.J. An Evaluation of a smartphone-assisted behavioral weight control intervention for adolescents: Pilot study. JMIR Mhealth Uhealth 2016, 4. [Google Scholar] [CrossRef] [PubMed]
- Quelly, S.B.; Norris, A.E.; DiPietro, J.L. Impact of mobile apps to combat obesity in children and adolescents: A systematic literature review. J. Spec. Pediatr. Nur. 2016, 21, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H. Analysis in cell phone use in children and adolescents. KISDI Stat. Rep. 2015, 15, 1–7. [Google Scholar]
- Kim, H.; Kang, J.-H.; Park, H.A.; Cho, S.H.; Jeon, S.; Jung, J.-H.; Sung, E. Development of a Smartphone Application Prototype for Child Obesity Prevention: Rationale and Study Design of Acceptability and Feasibility Tests. Korean J. Health Promot. 2015, 15, 194–201. [Google Scholar] [CrossRef]
- Korea Centers for Disease Control and Prevention. Available online: http://cdc.go.kr/CDC/notice/CdcKrInfo0201.jsp?menuIds=HOME001-MNU1154-MNU0005-MNU1889&cid=1235 (accessed on 12 March 2016).
- Ha, K.; Chung, S.; Lee, H.S.; Kim, C.I.; Joung, H.; Paik, H.Y.; Song, Y. Association of Dietary Sugars and Sugar-Sweetened Beverage Intake with Obesity in Korean Children and Adolescents. Nutrients 2016, 8, 31. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.K.; Kim, M.K. Relationship of sodium intake with obesity among Korean children and adolescents: Korea National Health and Nutrition Examination Survey. Br. J. Nutr. 2016, 115, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Song, Y.H.; Park, S.; Park, M.J. Impact of lifestyle factors on trends in lipid profiles among Korean adolescents: The Korea National Health and Nutrition Examination Surveys study, 1998 and 2010. Korean J. Pediatr. 2016, 59, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Finch, M.; Jones, J.; Yoong, S.; Wiggers, J.; Wolfenden, L. Effectiveness of centre-based childcare interventions in increasing child physical activity: A systematic review and meta-analysis for policymakers and practitioners. Obes. Rev. 2016, 17, 412–428. [Google Scholar] [CrossRef] [PubMed]
- O’Malley, G.; Clarke, M.; Burls, A.; Murphy, S.; Murphy, N.; Perry, I.J. A smartphone intervention for adolescent obesity: Study protocol for a randomised controlled non-inferiority trial. Trials 2014, 15. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.-H.; Jeon, S.H.; Bae, H.J.; Cho, Y.-G.; Hur, Y.-I.; Sung, E.J.; Kang, J.-H. Development of a Smartphone Application for 4th–6th Grade Elementary Students Aimed to Prevent Childhood Obesity. Korean J. Obes. 2016, 25, 99–104. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Beets, M.W.; Belton, S.; Cardon, G.M.; Duncan, S.; Hatano, Y.; Lubans, D.R.; Olds, T.S.; Raustorp, A.; et al. How many steps/day are enough? For children and adolescents. Int. J. Behav. Nutr. Phys. Act. 2011, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Green Cross Health Care. Report on the Accuracy of an Exercise Index of an Activity Tracker (Report); Kyunghee University: Seoul, Korea, 2014. [Google Scholar]
| Study Procedure | Safety Test | Efficacy Test | Long-Term Effect Test | |||
|---|---|---|---|---|---|---|
| A Week before | Baseline | Week 4 | Week 8 | Week 12 | Month 6 | |
| 1. Workshop for intervention group | I | I | ||||
| 2. Screen-time monitoring | I | I | I | I | I | |
| 3. Group education session | I, C | I, C | ||||
| 4. Lifestyle questionnaire | I, C | I, C | I, C | |||
| 5. PAPS measurement | I, C | I, C | I, C | |||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, H.J.; Kang, J.-H.; Kim, O.H.; Choi, M.; Oh, M.; Nam, J.; Sung, E. Interventions for Preventing Childhood Obesity with Smartphones and Wearable Device: A Protocol for a Non-Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2017, 14, 184. https://doi.org/10.3390/ijerph14020184
Yang HJ, Kang J-H, Kim OH, Choi M, Oh M, Nam J, Sung E. Interventions for Preventing Childhood Obesity with Smartphones and Wearable Device: A Protocol for a Non-Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2017; 14(2):184. https://doi.org/10.3390/ijerph14020184
Chicago/Turabian StyleYang, Hye Jung, Jae-Heon Kang, Ok Hyun Kim, Mona Choi, Myungju Oh, Jihyun Nam, and Eunju Sung. 2017. "Interventions for Preventing Childhood Obesity with Smartphones and Wearable Device: A Protocol for a Non-Randomized Controlled Trial" International Journal of Environmental Research and Public Health 14, no. 2: 184. https://doi.org/10.3390/ijerph14020184





