A Review of the Field on Children’s Exposure to Environmental Contaminants: A Risk Assessment Approach
Abstract
:1. Introduction
1.1. Studies of Children’s Exposure to Environmental Contaminants
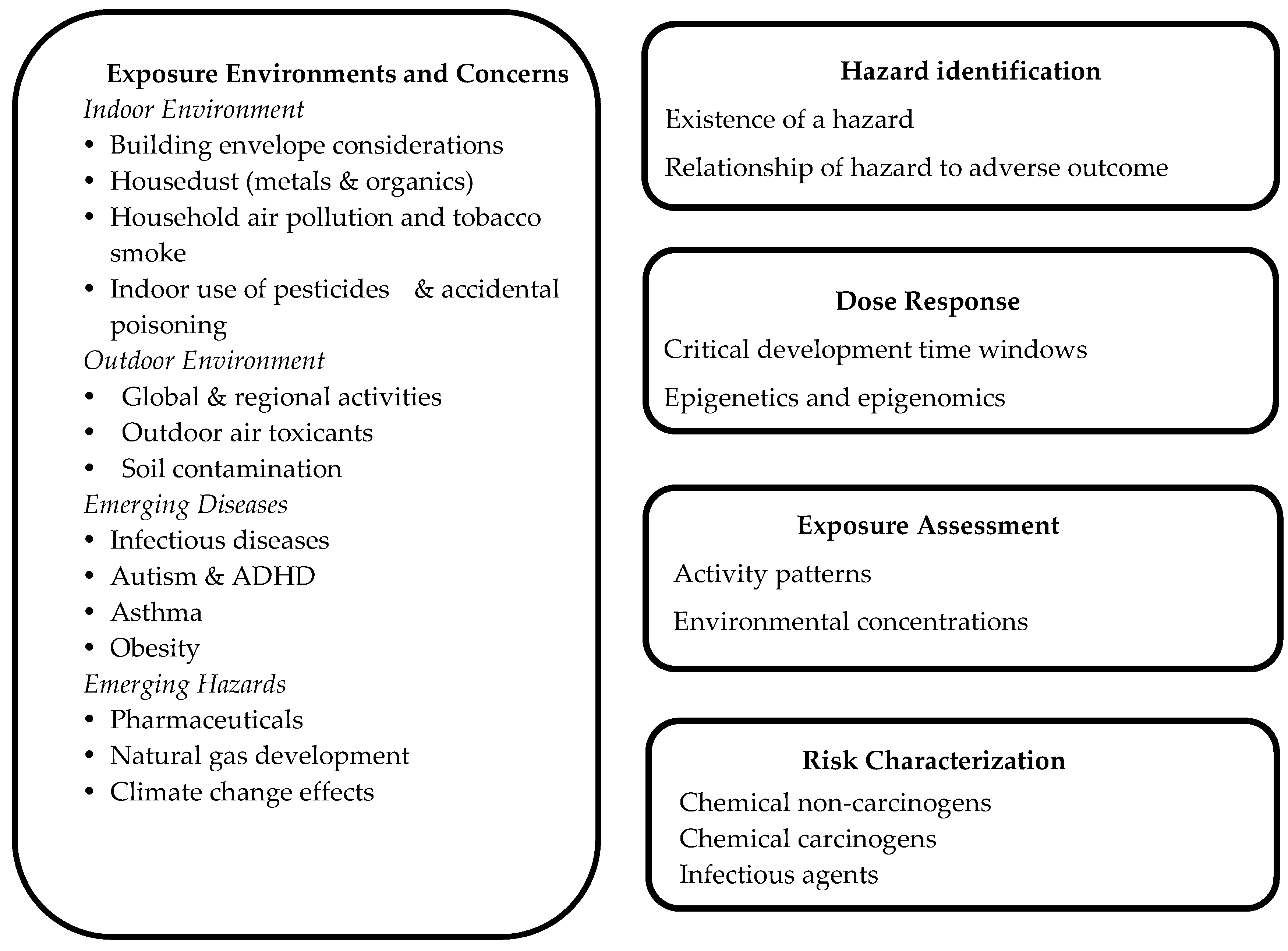
1.2. Children’s Exposures and the Risk Assessment Approach
2. Approach
2.1. Exposure Environments and Concerns
2.1.1. Hazards in the Indoor Environment
2.1.2. Hazards in the Outdoor Environment
2.2. Some Special Diseases of Concern in the 21st Century
2.2.1. Infectious Diseases
2.2.2. Asthma and Allergies
2.2.3. Attention Deficit Hyperactivity Disorder and Autism
2.2.4. Childhood Obesity
2.3. Emerging Hazards
2.3.1. Emerging Contaminants
2.3.2. Climate Change Effects
3. Results and Discussion
3.1. Hazard Identification for Children
3.2. Dose-Response Assessment for Children
3.3. Exposure Assessment for Children
3.3.1. Determining Children’s Activity Patterns
3.3.2. Determining Environmental Concentrations
3.3.3. Biomarker Approach to Look at Exposure
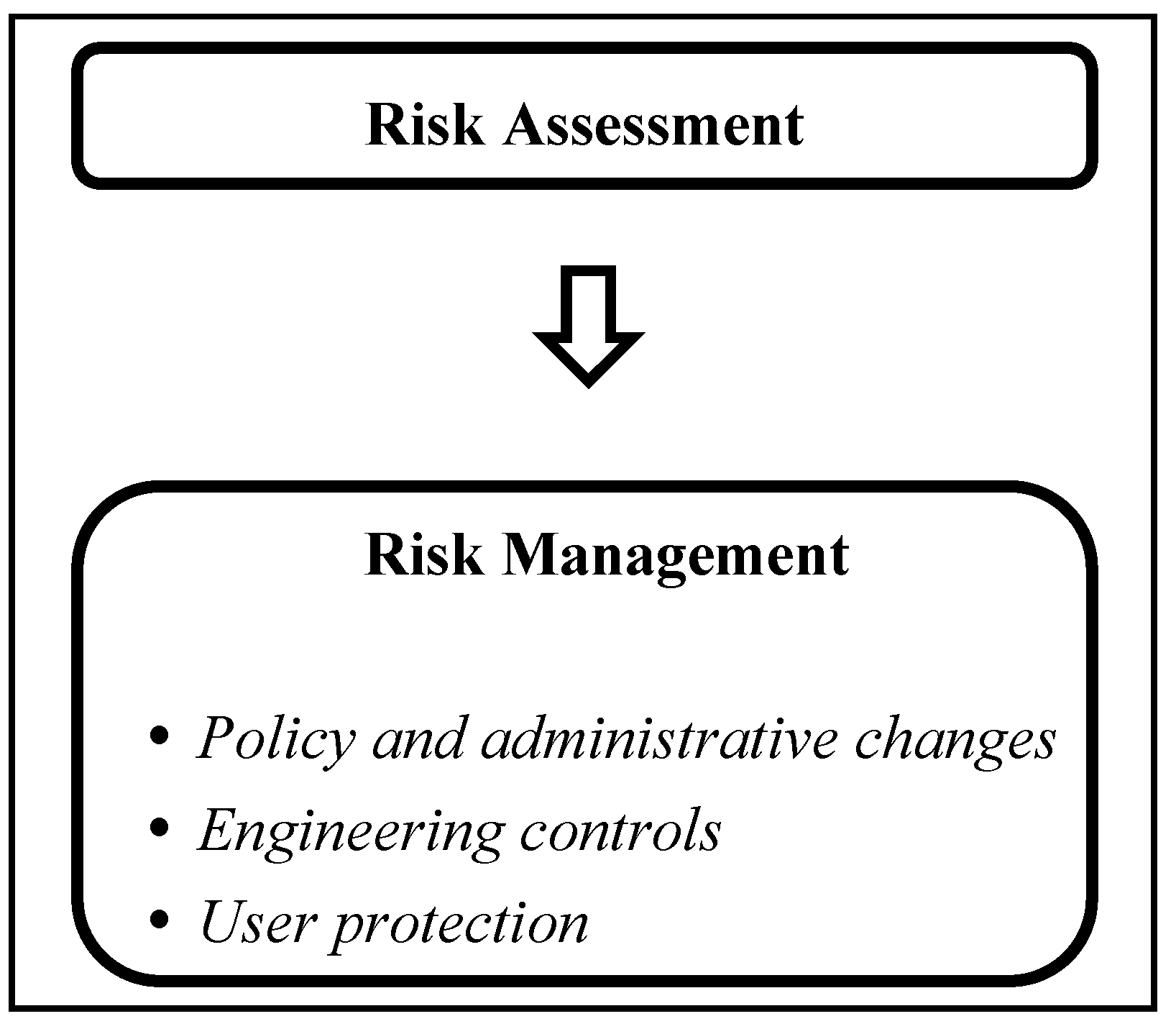
3.4. Risk Characterization and Risk Management
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- National Institute of Health. President’s Task Force on Environmental Health Risks and Safety to Children. Available online: http://ptfceh.niehs.nih.gov (accessed on 2 December 2016).
- Environmental Protection Agency. Agrichemicals Food Quality Protection Act-Children and Consumers. Available online: http://www.epa.gov/laws-regulations/summary-food-quality-protection-act (accessed on 1 March 2016).
- Wolfe, I.; Mckee, M. European Children Health Services and Systems: Lessons with Borders; McGraw Hill Education: Birkshire, UK, 2013. [Google Scholar]
- Laborde, A.; Tomasina, F.; Bianchi, F.; Brune, M.; Buka, I.; Comba, P.; Corra, L.; Cori, L.; Duffert, C.; Harari, R.; et al. Children’s Health in Latin America: The influence of environmental exposures. Environ. Health Perspect. 2015, 123, 201–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, B.; Park, H.; Hong, Y.; Ha, M.; Kim, Y.; Chang, N.; Kim, B.; Kim, Y.J.; Ha, E.H. Prenatal bisphenol A and birth outcomes: MOCEH (Mothers and Children’s Environmental Health) study. Int. J. Hyg. Environ. Health 2014, 217, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Luo, Z.C.; Liu, J.; Fraser, W. Large prospective birth cohort studies on environmental contaminants and child health-goals, challenges, limitations and needs. Med. Hypotheses 2016, 74, 318–324. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Health. National Children’s Study (NCS) Vanguard Data and Sample Archive and Access System (NCS Archive). Available online: https://www.nichd.nih.gov/research/NCS/Pages/researchers.aspx (accessed on 10 February 2017).
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Available online: http://www.cdc.gov/nchs/nhanes.htm (accessed on 20 April 2016).
- Cohen-Hubal, E.; Sheldon, L.S.; McCurdy, T.R.; Berry, M.R.; Rigas, M.L.; Zartarian, V.G.; Freeman, N.C. Children’s exposure assessment: a review of factors influencing Children’s exposure, and the data available to characterize and assess that exposure. Environ. Health Perspect. 2000, 108, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Ott, W.; Steinemann, A.; Wallace, L. Exposure Analysis; Taylor and Francis: New York, NY, USA, 2007. [Google Scholar]
- Cohen Hubal, E.; Selevan, S. A lifestage approach to assessing children’s exposure. Birth Defects Res. B 2008, 83, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Zartarian, V.G.; Ott, W.R.; Duan, N. A quantitative definition of exposure and related concepts. J. Expo. Anal. Environ. Epid. 1997, 7, 411–437. [Google Scholar] [PubMed]
- Zartarian, V.; Bahadori, T.; Mckone, T. Adoption of an official ISEA glossary. J. Expo. Anal. Environ. Epid. 2005, 15, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Environmental Protection Agency. A Framework for Assessing Health Risks of Environmental Exposures to Children. Available online: https://ofmpub.epa.gov/eims/eimscomm.getfile?p_download_id=459047 (accessed on 12 February 2016).
- Goldizen, F.; Sly, P.; Knibbs, L. Respiratory effects of air pollution on children. Pediatr. Pulm. 2016, 51, 94–108. [Google Scholar] [CrossRef] [PubMed]
- Branco, P.; Nunes, R.; Alvin-Ferrez, M.; Martins, F.; Sousa, S. Children’s exposure to Radon in nursery and primary schools. Int. J. Environ. Res. Public Health 2016, 13, 386. [Google Scholar] [CrossRef] [PubMed]
- National Center for Healthy Housing. Housing codes. Available online: http://www.nchh.org/Training/HealthyHomesTrainingCenter/StateHousingCodes.aspx (accessed on 20 May 2016).
- Jia, C.; Batterman, S.A. crtitical reveiw of Naphthalene sources and exposures relevant to indoor and outdoor air. Int. J. Environ. Res. Public Health 2010, 7, 2903–2939. [Google Scholar] [CrossRef] [PubMed]
- Morgan, M. Children’s Exposures to pyrethroid insecticides at home: A review of data collected in published exposure measurement studeis conducted in the United States. Int. J. Environ. Res. Public Health 2012, 9, 2964–2985. [Google Scholar] [CrossRef] [PubMed]
- Sarigiannis, D.; Karakitsios, S.; Gotti, A.; Liakos, I.; Katsoyiannis, A. Exposure to major volatile organic compounds and carbonyls in European indoor environments and associated health risks. Environ. Int. 2011, 37, 743–765. [Google Scholar] [CrossRef] [PubMed]
- Vardoulakis, S.; Dimitroulopoulou, C.; Thornes, J. Impact of climate change on the domestic indoor environment and health risks in the UK. Environ. Int. 2015, 85, 299–313. [Google Scholar]
- Korfmacher, K.S.; George, V. Educating refugees to improve their home environmental health. J. Public Health Manag. Pract. 2012, 18, 469–473. [Google Scholar] [CrossRef] [PubMed]
- Glorennec, P.; Lucas, J.; Mandin, C.; Le Bot, B. French children’s exposure to metals via ingestion of indoor dust, outdoor playground dust and soil: Contamination data. Environ. Int. 2012, 45, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, P.; Levesque, C.; Chenier, M.; Gardner, H.; Jones-Otazo, H.; Petrovic, S. Canadian house dust study: Population-based concentrations, loads and loading rates of arsenic, cadmium, chromium, copper, nickel, lead, and zinc inside urban homes. Sci. Total Environ. 2013, 443, 520–529. [Google Scholar] [CrossRef] [PubMed]
- Shin, M.; Lee, S.; Kim, H.; Lee, J.J.; Choi, G.; Choi, S.; Kim, S.; Kim, S.; Park, J.; Moon, H.; et al. Polybrominated diphenyl ethers in maternal serum, breast milk, umbilical cord serum, and house dust in a south korean birth panel of mother-neonate pairs. Int. J. Environ. Res. Public Health 2016, 13, 767. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, A.; Rimmer, T. Navigating the lead laws/rules/standards for renovation, and repair activities: A guide for contractors and laborers. J. Environ. Prot. 2012, 3, 1318–1329. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Blood Lead Level in Children. Available online: http://www.cdc.gov/nceh/lead/acclpp/lead_levels_in_children_fact_sheet.pdf (accessed on 6 December 2016).
- Blackowicz, M.J.; Hryhorczuk, D.O.; Rankin, K.M.; Lewis, D.A.; Haider, D.; Lanphear, B.; Evens, A. The impact of low-level lead toxicity on school performance among Hispanic subgroups in the Chicago public schools. Int. J. Environ. Res. Public Health 2016, 13, 774. [Google Scholar] [CrossRef] [PubMed]
- Attina, T.; Trasande, L. Economic costs of childhood lead exposure in low and middle-income countries. Environ. Health Perspect. 2013, 121, 1097–1102. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Population Using Soil Fule (Estimates): Data by Country. Available online: http://apps.who.int/gho/data/node.main.135 (accessed on 23 February 2016).
- World Health Organization. Ambient and Household Air Pollution and Health Update 2014. Available online: http://www.who.int/phe/health_topics/outdoorair/databases/en/ (accessed on 5 June 2016).
- Bruce, N.; Dherani, M.; Das, J.; Balakrishnan, K.; Adair-Rohanim, H.; Bhutta, Z.; Pope, D. Control of household airpollution for child survival: Estimates for intevention impacts. BMC Public Health J. 2013, 13, S8. [Google Scholar]
- Roth, D.; Caulifield, L.E.; Ezzati, M.; Black, R. Acute lower respiratory infections in childhood: Opportunities for reducing the global burden through nutritional interventions. Bull. World Health Organ. 2016, 86, 321–416. [Google Scholar] [CrossRef]
- Boutayeb, A. The double burden of communicable and non-communicable diseases in develping countries. Trans. R. Soc. Trop. Med. Hyg. 2016, 100, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.B.; Bruce, N.G.; Grigg, J.; Hibberd, P.L.; Kurmi, O.P.; Lam, K.B.; Mortimer, K.; Asante, K.P.; Balakrishman, K.; Balmes, J.; et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir. Med. 2014, 2, 823–860. [Google Scholar] [CrossRef]
- Deziel, N.C.; Rull, R.P.; Colt, J.S.; Reynolds, P.; Whiehead, T.P.; Gunier, R.B.; Month, S.R.; Taggart, D.R.; Buffler, P.; Ward, M.H.; Metayer, C. Polycyclic aromatic hydrocarbons in residential dust and risk of acute lymphoblastic leukemia. Environ. Res. 2014, 133, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Yeramaneni, S.; Dietrich, K.; Yolton, K.; Pedersen, C.; Aldous, K. Secondhand tobacco smoke and neuromotor function in rural children. J. Pediatr. 2015, 167, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Evlampidou, I.; Bagkeris, M.; Vardavas, C.; Koutra, K.; Patelarou, E.; Koutis, A.; Chatzi, L.; Kogevinas, M. Prenatal second-hand smoke exposure measured with urine cotinine may reduce gross motor development at 18 months of age. J. Pediatr. 2015, 167, 246–252. [Google Scholar] [CrossRef]
- Ragnuveer, G.; White, D.; Hayman, L.; Woo, J.; Villafane, J.; Celermajer, D.; Ward, K.; de Ferranti, S.; Zachariah, J.; American Heart Association. Cardiovascular consequences of childhood secondhand tobacco smoke exposure: Prevailing evidence, burden, and racial and socioeconomic disparities: A scientific statement from the American Heart Association. Circulation 2016, 134, e336–e359. [Google Scholar] [CrossRef] [PubMed]
- Kuntz, B.; Lampert, T. Social disparities in parental smoking and young children’s exposure to secondhand smoke at home: A time-trend analysis of repeated cross-sectional data from the German KiGGS study between 2003–2006 and 2009–2012. BMC Public Health 2016, 16, 1–11. [Google Scholar] [CrossRef] [PubMed]
- National Center for Environmental Health. Healthy Homes Manual: Smoke-Free Policies in Multiunit Housing. Available online: http://www.cdc.gov/healthyhomes (accessed on 5 December 2016).
- Ritchie, D.D.; Amos, A.; Shaw, A.; O’Donnell, R.; Semple, S.; Turner, S.; Martin, C. How do policy advisors and practitioners prioritise the protection of children from secondhand smoke exposures in a country with advanced tobacco control policy? Tob. Control 2015, 24, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Oh, A.; Kacker, A. Do electronic cigarettes impart a lower potential disease burden than conventional tobacco cigarettes?: Review on e-cigarette vapor versus tobacco smoke. Laryngoscope 2016, 124, 2702–2706. [Google Scholar] [CrossRef] [PubMed]
- Ward, M.; Lubin, J.; Giglierano, J.; Colt, J.; Wolter, C.; Bekiroglu, N.; Cammann, D.; Hartge, P.; Nuckols, J. Proximity to crops and residential exposure to agricultural herbicides in Iowa. Environ. Health Persp. 2006, 114, 893–897. [Google Scholar] [PubMed]
- Carmichael, S.L.; Yang, W.; Roberts, E.; Kegley, S.; Brown, T.; English, P.; Lammer, E.; Shaw, G. Residential agricultural pesticide exposures and risks of selected birth defects among offspring in the San Joaquin Valley of California. Birth Defects Res. A 2016, 106, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Bouchard, M.; Chevrier, J.; Harley, K.; Kogut, K.; Vedar, M.; Calderon, N.; Trujillo, C.; Johnson, C.; Bradman, A.; Boyd Barr, D.; et al. Prenatal exposures to organophosphate pesticides and IQ in 7-year old children. Environ. Health Perspect. 2011, 119, 1189–1195. [Google Scholar] [CrossRef] [PubMed]
- Rahbar, M.H.; Sams-Vaughan, M.; Hessabi, M.; Dickerson, A.S.; Lee, M.; Bresslet, J.; Tomechko, S.; Moreno, E.K.; Lovelan, K.A.; Desai, C.C.; et al. Concentrations of polychlorinated biphenyls (PCBs) and organochlorine (OC) pesticides in umbilical cord blood serum of Jamaican newborns. Int. J.Environ. Res. Public Health 2016, 13, 1032. [Google Scholar] [CrossRef] [PubMed]
- Narayan, S.; Liew, Z.; Paul, K.; Lee, P.; Sinsheimer, J.; Bronstein, J.; Ritz, B. Household Organophosphates pesticide use and Parkinson’s disease. Int. J. Epidmiol. 2013, 42, 1476–1485. [Google Scholar] [CrossRef] [PubMed]
- Perkins, A.; Walters, F.; Sievert, J.; Rhodes, B.; Morrissey, B.; Karr, C. Home use of a pyrethroid-containing pesticide and facial paresthesia in a toddler: A case report. Int. J.Environ. Res. Public Health 2016, 13, 829. [Google Scholar] [CrossRef] [PubMed]
- Arcury, T.; Laurienti, P.; Chen, H.; Howard, T.; Barr, D.; Mora, D.; Summers, P.; Quandt, S. Organophosphates pesticide urinary metabolites among Latino immigrants: North Carolina farmworkers and non-farmworkers compared. J. Occup. Environ. Med. 2016, 58, 1079–1086. [Google Scholar] [CrossRef] [PubMed]
- Andiran, N.; Sarikayalar, F. Patterns of acute poisoning in childhood in Ankara: What has changed in twenty years? Turk. J. Pediatr. 2004, 46, 147–152. [Google Scholar] [PubMed]
- American Lung Association. State of the Air Report. Available online: http://www.stateoftheair.org/2014/key-findings/ (accessed on 5 December 2016).
- Heinzerling, A.; Hsu, J.; Yip, F. Respiratory health effects of ultrafine particles in children: A literature review. Water Air Soil Pollut. 2016, 227. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.H.; Lovinsky-Desir, S.; Yan, B.; Camann, D.; Sjodin, A.; Ki, Z.; Perera, F.; Kinney, P.; Chillrud, S.; Miller, R.L. Time trends of polycyclic aromatic hydrocarbon exposure in New York City from 2001 to 2012: Assessed by repeat air and urine samples. Environ. Res. 2014, 131, 95–103. [Google Scholar] [CrossRef] [PubMed]
- HEI Collaborative Working Group; Le, T.; Ngo, l.; Do, V.; Thach, T.; Nguyen, D.; Cohen, A. Effects of short-term exosure to air polluton on hospital admissions of young children for acute lower respiratory infections in Ho CHi Minh City, Vietnam. Res. Rep. Health Eff. Inst. 2012, 169, 5–72. [Google Scholar]
- Somers, C. Ambient air pollution exposure and damage to male gamtes: Human studies and in situ 'sentinel" animal experiments. Sys. Biol. Reprod. Med. 2016, 57, 63–71. [Google Scholar] [CrossRef] [PubMed]
- De Miguel, E.; Iribarren, I.; Chacon, E.; Ordonez, A.; Charlesworth, S. Risk-based evaluation of the exposure of children to trace elements in playgrounds in Madrid (Spain). Chemospere 2007, 66, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Black, J.; Welday, J.; Buckley, B.; Ferguson, A.; Gurian, P.; Mena, K.; Yang, I.; McCandish, E.; Solo-Gabriele, H. Risk assessment for children exposed to beach sands impacted by oil spill chemicals. Int. J.Environ. Res. Public Health 2016, 13, 853. [Google Scholar] [CrossRef] [PubMed]
- GRD 2013 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioral, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 5–11. [Google Scholar] [CrossRef]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
- Kirk, M.; Pires, S.; Black, R.; Caipo, M.; Crump, J.; Devleesschauwer, B.; Dopfer, D.; Fazil, A.; Fischer-Walker, C.; Hald, T.; et al. World Health Organization estimates of the global and regional disease burden of 22 fodo borne bacterial a, protozoal and viral diseases, 2010: A data sysnthesis. PLoS Med. 2015, 12, e1001921. [Google Scholar]
- Hall, A.; Wikswo, M.; Pringle, K.; Gould, H.; Parashar, U. Vital signs: Foodborne norovirus outbreaks-United States, 2009-2012. MMWR Morb. Mortal Wkly. Rep. 2014, 63, 491–495. [Google Scholar] [PubMed]
- Centers for Disease Control and Prevention. Norovirus Is Now the Leading Cause of Severe Gastroenteritis in US Children. Available online: http://www.cdc.gov/media/releases/2013/p0321_norovirus_children.html (accessed on 6 May 2016).
- Orata, F. The 2010 Cholera Outbreak in haiti: How science solved a controvery. PLoS Pathog. 2014, 10, e1003967. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalenc, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 743–800. [Google Scholar]
- Fellner, C. Zika virus: Anatomy of a global health crisis. P. T. Community 2016, 41, 242–253. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Zika Virus Disease in the United States, 2015–2016. Available online: http://www.cdc.gov/zika/geo/united-states.html (accessed on 24 October 2016).
- Nascimento, M.; Rodrigues, J.C.; Reis, L.; Nogueira, I.; Carvalho, P.; Brandao, J.; Duarte, A.; Jordao, L. Pathogens in ornamental waters. Int. J.Environ. Res. Public Health 2016, 13, 216. [Google Scholar] [CrossRef] [PubMed]
- Wright, M.E.; Solo-Gabriele, H.M.; Abdelzaher, A.M.; Elmir, S.; Fleming, L.E. The inter-tidal zone is the geographic location of elevated concentrations of enterococci. Water Sci. Technol. 2011, 63, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.H.; Abdelzaher, A.M.; Phillips, M.; Hernandez, R.; Solo-Gabriele, H.M.; Kish, J.; Scorzetti, G.; Fell, J.W.; Diaz, M.R.; Scott, T.M.; et al. Indicator microbes correlate with pathogenic bacteria, yeasts, and helminthes in sand at a subtropical recreational beach site. J.Appl. Microbiol. 2011, 110, 1571–1583. [Google Scholar] [CrossRef] [PubMed]
- Solo-Gabriele, H.; Brandao, J.; Gordon, B.; Ferguson, A. Pathogenic Fungi in Public Places, Information Gaps in Assessing Public Health Risk. In Environmental Mycology in Public Health; Elsevier, Inc.: Waltham, MA, USA, 2016; pp. 167–192. [Google Scholar]
- Gilliland, F. Outdoor air pollution, genetic susceptibility, and asthma management: Opportunities for intervention to reduce the burden of asthma. Pediatrics 2009, 123 (Suppl. 3), S168–S173. [Google Scholar] [CrossRef] [PubMed]
- Sheik, S.; Pitts, J.; Ryan-Wenger, N.; McCoy, K.; Hayes, D. Environmental exposures and family history of asthma. J. Asthma 2016, 20, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Timm, S.; Frydenberg, M.; Janson, C.; Campbell, B.; Forsberg, B.; Gislason, T.; Holm, M.; Jogi, R. The urban-rural gradient in asthma: A population-based study in Northern Europe. Int. J.Environ. Res. Public Health 2016, 13, 93. [Google Scholar] [CrossRef] [PubMed]
- Matelski, L.; Van de Water, J. Risk factors in autism: Thinking outside the brain. J. Autoimmun. 2015, S0896-8411, 30054–30058. [Google Scholar] [CrossRef] [PubMed]
- Burte, E.; Nadif, R.; Jacquemin, B. Susceptibility factors relevant for the association between long-term air pollution exposure and incident asthma. Curr. Environ. Health Rep. 2016, 3, 23–39. [Google Scholar] [CrossRef] [PubMed]
- Feng, M.; Yang, Z.; Pan, L.; Lai, X.; Xian, M.; Huang, X.; Chen, Y.; Schroder, P.C.; Roponnen, M.; Schaub, B.; et al. Associations of early life exposures and environmental factors with asthma amoong children in rural and urban areas in Guangdong. China. Chest 2016, S0012-3692, 00450–00455. [Google Scholar]
- Grutta, S.; Indinnimeno, L.; Di Coste, A.; Ferrante, G.; Landi, M.; Pelosi, U.; Rusconi, F. Environmental risk factors and lung diseases in children: From guidelines to health effects. Early Hum. Dev. 2013, 89, S59–S62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Institute of Medicine. Clearing the Air: Asthma and Indoor Air Exposures. Available online: http://www.nationalacademies.org/hmd/Reports/2000/Clearing-the-Air-Asthma-and-Indoor-Air-Exposures.aspx (accessed on 6 May 2016).
- Kanchongkittiphon, W.; Mendell, M.J.; Gaffin, J.M.; Wang, G.; Phipatanakul, W. Indoor environmental exposures and exacerbation of asthma: An update to the 2000 review by the Institute of Medicine. Environ. Health Perspect. 2015, 123, 6–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hauptman, M.; Phipatanakul, W. Recent advances in environmental controls outside the home setting. Curr. Opin. Allergy CL 2016, 16, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Halken, S. Prevention of allergic disease in childhood: Clinical and epidemiological aspects of primary and secondary allergy prevention. Pediatr. Allergy Immu. 2004, 15, 9–32. [Google Scholar] [CrossRef] [PubMed]
- Rava, M.; Smit, L.; Nadif, R. Gene-environment interactions in the study of asthma in the postgenomewide association studies era. Curr. Opin. Allergy CL 2015, 15, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.B.; Zhou, J.H.; Habre, R.; Bastin, T.M.; Gilliland, F.D. Lifetime prevalence of childhood eczema and the effect of indoor environmental factors: Analysis in Hispanic and non-Hispanic white children. Allergy Asthma Proc. 2016, 37, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Torrelo, A. Atopic dermatitis in different skin types. What is to know? J. Eur. Acad. Dermatol. Vernereol. 2014, 28, 2–4. [Google Scholar] [CrossRef] [PubMed]
- Toskala, E.; Kennedy, D. Asthma risk factors. Int. Forum. Allergy Rhinol. 2015, 5, S11–S16. [Google Scholar] [CrossRef] [PubMed]
- Leonard, M.R.; Cambi, S.; Huedo-Medina, T.B.; Fasano, A. Celiac disease genomic, environmental, microbiome, and metabolic (CDGEMM) study design: Approach to the future of personalized prevention of celiac disease. Nutirents 2015, 7, 9325–9336. [Google Scholar] [CrossRef] [PubMed]
- Yolton, K.; Cornelius, M.; McGough, J.; Makris, S.; Schantz, S. Exposure to neurotoxicants and the development of attention deficit hyperactivity disorder and its related behaviors in childhood. Neurotoxicol. Teratol. 2016, 44, 30–45. [Google Scholar] [CrossRef] [PubMed]
- Ploanska, K.; Jurewicz, J.; Hanke, W. Review of current evidence on the impact of pesticides, polychlorinated biphenyls and selected metals on attention deficit/hyperactivity disorder in children. Int. J. Occup. Environ. Health 2013, 26, 16–38. [Google Scholar] [CrossRef]
- Braun, J.; Kahn, R.; Froehlich, T.; Auinger, P.; Lanphear, B. Exposures to environmental toxicants and attention deficit hyperactivity disorder in U.S. children. Environ. Health Persp. 2006, 114, 1904–1909. [Google Scholar]
- Amihaesei, I.C.; Zamfir, C.L. ADHD (Attention deficit hyperactivity disorder)-A troubling entity, sometime perpetuating during adult life. Rev. Med. Chir. Soc. Med. Nat. lasi. 2016, 120, 10–14. [Google Scholar] [PubMed]
- Domingues, V.; Nasuti, C.; Piangerelli, M.; Correia-Sa, L.; Ghezzo, A.; Marina, M.; Abruzzo, P. Pyrethroid pesticide metabolite in urine and microelements in hair of children affected by autism spectrum disorders: A preliminary investigation. Int. J.Environ. Res. Public Health 2016, 13, 388. [Google Scholar] [CrossRef] [PubMed]
- Lyall, K.; Schmidt, R.; Hertz-Piccioto, I. Maternal lifestyle and environmental risk factors for autism spectrum disorders. Int. J. Epidmiol. 2014, 43, 443–462. [Google Scholar] [CrossRef] [PubMed]
- Massion, S.; Wickham, S.; Pearce, A.; Barr, B.; Law, C.; Taylor-Robinson, D. Exploring the impact of early life factors on inequalities in risk of overweight in UK children: Findings from the UK Millennium Cohort Study. Arch. Dis. Child 2016. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Childhood Obesity Causes and Consequences. Available online: http://www.cdc.gov/obesity/childhood/causes.html (accessed on 19 May 2016).
- Hatch, E.; Nelson, J.; Stahlhut, R.; Webster, T. Association of endocrine disruptors and obesity: Perspectives from epidemiological studies. Environ. Health Perspect. 2010, 33, 324–332. [Google Scholar] [CrossRef]
- Buckley, J.P.; Engel, S.M.; Braun, J.M.; Whyatt, R.M.; Daniels, J.L.; Mendez, M.A.; Richardson, D.B.; Xu, Y.; Clafat, A.M.; Wolff, M.S.; et al. Prenatal phthalate exposures and body mass index amoung 4 to 7 year old children: A pooled analysis. Epidemiology 2016, 27, 449–458. [Google Scholar] [CrossRef] [PubMed]
- DiVall, S.A. The influence of endocrine disruptors on growth and development of children. Curr. Opin. Endocrinol. Diabetes Obes. 2013, 20, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Valvi, D.; Casas, M.; Mendez, M.; Ballesteros-Gomez, A.; Luque, N.; Rubio, S.; Sunyer, J.; Vrijheid, M. Prenatal Bisphenol A urine concentrations and early rapid growth and overweight risk in the offspring. Epidemiology 2013, 24, 791–799. [Google Scholar] [CrossRef] [PubMed]
- Desai, M.; Jellyman, J.; Ross, M. Epigenomics, gestational programming and risk of metabolic syndrome. Int. J. Obesity 2015, 39, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Versini, M.; Aljadeff, G.; Jeandel, P.; Shoenfeld, Y. Obesity: An additional piece in the mosaic of autoimunity. Israel Med. Assoc. J. 2014, 16, 619–621. [Google Scholar]
- Li, C.; Ford, E.S.; Zhao, Z.; Mokdad, A.H. Prevalence of pre-diabetes and its association with clustering of cardiometabolic risk factors and hyperinsulinemia among US adolescents: NHANES 2005-2006. Diabetes Care 2009, 32, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Hanley, M.J.; Abernethy, D.R.; Greenblatt, D.J. Effect of obesity on the pharmacokinetics of drugs in humans. Clin. Pharmacokinet. 2010, 49, 71–87. [Google Scholar] [CrossRef] [PubMed]
- Mangalgiri, K.; He, K.; Blaney, L. Emerging contaminants: A potential human health concern for sensitve populations. PDA J. Pharm. Sci. Tech. 2015, 69, 2150–2218. [Google Scholar] [CrossRef] [PubMed]
- Schaider, l.; Ackerman, J.; Rudel, R. Septic systems as sources of organic wastewater compounds in domestice drinking water wells in a shallow sand and gravel aquifer. Sci. Total Environ. 2016, 547, 470–481. [Google Scholar] [CrossRef] [PubMed]
- Malchi, T.; Maor, Y.; Shenker, M.; Chefetz, B. Irrigation of root vegetables with treated wastewater: Evaluating uptake of pharmaceiticals and the associated human health risks. Environ. Sci. Tech. 2014, 48, 9325–9333. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Dodgen, L.; Conkle, J.; Gan, J. Plant uptake of pharmaceutical and personal care products from recycled water and biosolids: A review. Sci. Total. Environ. 2015, 536, 655–666. [Google Scholar] [CrossRef] [PubMed]
- Casey, J.; Savitz, D.; Rasmussen, S.; Ogburn, E.; Pollack, J.; Mercer, D.; Schwartz, B. Unconventional natural gas development and birth outcome in Pennsylvania, USA. Epidemiology 2016, 27, 163–172. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Lui, Y.; Xia, X.; Ma, W.; Lin, H.; Kan, H.; Lu, J.; Feng, Q.; Mo, W.; Wang, P.; et al. Ambient temperature and the risk of preterm birth in Guangzhou, China (2001–2011). Environ. Health Perspect. 2016, 124, 1100–1106. [Google Scholar] [CrossRef] [PubMed]
- Auger, N.; Naimi, A.; Smargiassi, A.; Lo, E.; Kosatsky, T. Extreme heat and risk of early delivery among preterm and term pregnancies. Epidemiology 2014, 25, 344–350. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Climate Change and Human Health—Risks and Responses. Summary: Climate Change and Infectious Diseases. Available online: http://www.who.int/globalchange/summary/en/index5.html (accessed on 6 May 2016).
- Korotkov, Y.; Kozlova, T.; Kozlovskaya, L. Observation on changes in abundance of questing Ixodes ricinus, castor bean tick, over a 35-year period in the eastern part of its range (Russia, Tula region). Med. Vet. Entomol. 2015, 29, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Bernard, S.; Samet, J.; Grambsch, A.; Ebi, K.; Romieu, I. The potential impacts of climate variability and change on air-pollution-related health effects in the United States. Environ. Health Perspect. 2001, 109, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Casajus, N.; Perie, C.; Logan, T.; Lambert, M.; de Bois, S.; Berteaaux, D. An objective approach to select climate scenarios when projecting species distribution under climate change. PLoS ONE 2016. [Google Scholar] [CrossRef] [PubMed]
- Bickton, F. Climate change as the biggest threat to public health in Southern Africa and measures to reduce its impact. Malawi. Med. 2016, 28, 70–72. [Google Scholar] [CrossRef]
- U.S.Global Change Research Program. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. Available online: http://www.globalchange.gov/browse/reports/impacts-climate-change-human-health-united-states-scientific-assessment (accessed on 10 February 2017).
- D’Amato, G.; Vitale, C.; De Martino, A.; Viegi, G.; Lanza, M.; Molino, A.; Sanduzzi, A.; Vatrella, A.; Annesi-Maesano, I.; D’Amato, M. Effects on asthma and respiratory allergy of Climate change and air pollution. Mutidiscip. Respir. Med. 2015, 10, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samet, J.M. Risk assessment and child health. Pediatrics 2004, 113, 952–956. [Google Scholar] [PubMed]
- Armstrong, T.; Zaleski, R.; Konkel, W.; Parkerton, T. A tiered approach to assessing children’s exposure: A review of methods and data. Toxicol. Lett. 2002, 127, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Georgopoulos, P.; Brinkerhoff, C.; Isukapalli, S.; Dellarco, M.; Landrigan, P.; Lioy, P. A tiered framework for risk-relevant characterization and ranking of chemical exposures: Applications to the National Children Study (NCS). Risk Anal. 2014, 34, 1299–1316. [Google Scholar] [CrossRef] [PubMed]
- Driver, J.; Ross, J.; Pandian, M.; Assaf, N.; Osimitz, T.; Holden, L. Evaluation of predictive algorithms used for estimating potential postapplication, nondietary ingestion exposures to pesticides associated with children’s hand-to-mouth behavior. J. Toxicol. Environ. Health 2013, 76, 556–586. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.; Grice, J.; Cullen, A.; Fausten, E. A toxicological framework for the prioritization of children’s safe product act data. Int. J. Environ. Res. Public Health 2016, 13, 431. [Google Scholar] [CrossRef] [PubMed]
- Hines, R.; Sargent, D.; Autrup, H.; Birnbaum, L.; Brent, R.; Dorrer, N.; Hubal, E.; Juberg, D.; Laurent, C.; Luebke, R.; et al. Approaches for assessing risks to sensitive populations: Lessons learned from evaluating risks in the pediatric population. Toxicol. Sci. 2010, 113, 4–26. [Google Scholar] [CrossRef] [PubMed]
- Environmental Protection Agency. Products and Publications Relating to Risk Assessment Produced by the Office of the Science Advisor. Available online: http://www.epa.gov/osa/products-and-publications-relating-risk-assessment-produced-office-science-advisor (accessed on 3 October 2016).
- Environmental Protection Agency. U.S. EPA Supplemental Guidance for Assessing Susceptibility from Early-Life Exposure to Carcinogens. Available online: https://www3.epa.gov/airtoxics/childrens_supplement_final.pdf (accessed on 5 November 2016).
- Cohen-Hubal, E.; de Wet, T.; Du Toit, L.; Firestone, M.; Ruchirawat, M.; van Engelen, J.; Vickers, C. Identifying important life stages for monitoring and assessing risks from exposures to environmental contaminants: Results of a World Health Organization review. Regul. Toxicol. Pharm. 2014, 69, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Selevan, S.; Kimmel, C.A.; Mendola, P. Identifying critical windows of exposure for children’s health. Environ. Health Perspect. 2000, 208, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.; Barone, S.; LaMantia, A.; Philen, R.; Rice, D.C.; Spear, L.; Susser, E. Workshop to identify critical windows of exposure for children’s health: Neurobehavioral work group summary. Environ. Health Perspect. 2000, 108, 535–544. [Google Scholar] [CrossRef] [PubMed]
- Barr, M.; DeSesso, J.; Lua, C.; Osmond, C.; Ozanne, S.; Sadler, T.; Simmons, R.A.; Sonawane, B.R. Workshop to identify critical windows of exposure for children’s health: Cardiovascular and endocrine work group summary. Environ. Health Perspect. 2000, 108, 475–486. [Google Scholar] [CrossRef]
- Dietert, R.R.; Etzel, R.A.; Chen, D.; Halonen, M.; Holladay, S.D.; jarabek, A.M.; Landreth, K.; Peden, D.B.; Pinkenton, K.; Smialowicz, R.J. Workshop to identify critical windows of exposure for children’s health: Immune and respiratory group summary. Environ. Health Perspect. 2000, 108, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Lemasters, G.K.; Perreault, S.D.; Hales, B.F.; Hatch, M.; Hirshfield, A.N.; Huges, C.L.; Lamb, J.C.; Pryor, J.L.; Rubin, C.; Seed, J.G. Workshop to identify critical windows of exposure for children’s health: Reproductive health in children and adolescents work group summary. Environ. Health Perspect. 2000, 108, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Olshan, A.F.; Anderson, L.; Roman, E.; Fear, N.; Wolfe, M.; Whyatt, R.; Vu, V.; Diwan, B.A.; Potischan, M. Workshop to identify critical windows of exposure for children’s health: Cancer work group summary. Environ. Health Perspect. 2000, 108, 595–597. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.; Barone, S.; Kimmel, C. Children’s health risk assessment: Incorporating a lifestage approach into the risk assessment process. Birth Defects Res. B 2008, 83, 511–521. [Google Scholar] [CrossRef] [PubMed]
- Felter, S.; Daston, G.; Euling, S.; Pierson, A.; Tassinari, M. Assessment of health risks resulting from early-life exposures: Are current chemical toxicity testing protocols and risk assessment methods adequate. Crit. Rev. Toxicol. 2015, 45, 219–344. [Google Scholar] [CrossRef] [PubMed]
- Environmental Protection Agency. Contaminants of Emerging Concern Including Pharmaceuticals and Personal Care Products. Environmental Protection Agency. Available online: https://www.epa.gov/wqc/contaminants-emerging-concern-including-pharmaceuticals-and-personal-care-products (accessed on 5 October 2016).
- Loss, G.J.; Depner, M.; Hose, A.J.; Getuneit, J.; Kavonen, A.M.; Hyvarinen, A.; Roduit, C.; Kabesch, M.; Lauener, R.; Pfefferle, P.I.; et al. The early development of wheeze. Am. J. Resp. Crit. Care 2016, 193, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Gundacker, C.; Gencik, M.; Hengstchlager, M. The relevance of the individual genetic background for the toxicokinetics of two significant neurodevelomental toxicants: Mercury and lead. Mutat. Res. 2010, 705, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Chow, E.; Puumala, S.; Mueller, B.; Carozza, S.; Fox, E.; Horel, S.; Johnson, K.; Mclaughlin, C.; Reynolds, P.; Von Behren, J.; et al. Childhood cancer in relation to parental race and ethnicity: A 5-state pooled analysis. Cancer 2010, 116, 3045–3053. [Google Scholar] [CrossRef] [PubMed]
- Burris, H.; Baccarelli, A.; Wright, R.O.; Wright, R.J. Epigenetics: Linking social and environmental exposures to preterm birth. Pediatr. Res. 2016, 79, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Ginsberg, G.; Hattis, D.; Miller, R.; Sonawane, B. Pediatric pharmacokinetic data: Implications for environmental risk assessment for children. Pediatrics 2004, 113, 973–983. [Google Scholar] [PubMed]
- Ginsberg, G.; Hattis, D.; Sonawane, B.; Russ, A.; Banati, P.; Kozlak, M.; Smolenski, S.; Goble, R. Evaluationof child/adult pharmacokinetic differences from a database derived from the therapeutic drug literature. Toxicol. Sci. 2002, 66, 185–200. [Google Scholar] [CrossRef] [PubMed]
- Kutanzi, K.R.; Lumen, A.; Korturbash, I.; Miousse, I.R. Pediatric exposures to radiation: Carcinogenic considerations. Int. J. Environ. Res. Public Health 2016, 13, 1057. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, A.; Coleman, S.; Biddle, D.; Bursac, Z.; Johnson, W. In-vitro soil adherence for dermal exposure using a controlled mechanical chamber. J. Appl. Sci. Res. 2009, 5, 232–243. [Google Scholar]
- Young, B.; Tulve, N.; Egeghy, P.; Driver, J.; Zartaran, V.; Johnston, J.; Delmar, C.; Evans, J.; Smith, L.; Glen, G.; et al. Comparison of four probabilistic models (CARES, Calendex, ConsExpo, and SHEDS) to estimate aggregate residential exposures to pesticides. J. Expo. Sci. Environ. Epid. 2012, 22, 522–532. [Google Scholar] [CrossRef] [PubMed]
- Firestone, M.; Moya, J.; Cohen-Hubal, E.; Zartarian, V.; Xue, J. Identyfing childhood age groups exposure assessment and monitoring. Risk Anal. 2007, 27, 701–714. [Google Scholar]
- Hosapple, M.P.; Paustenbauch, D.J.; Charnley, G.; West, L.J.; Luster, M.I.; Dietert, R.R.; Burns-Nass, L.A. Symposium summary: Children’s health risk-what’s so special about the developing immune system. Toxicol. Appl. Pharm. 2004, 199, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, A.; Canales, C.; Beamer, P.; AuYeung, W.; Key, M.; Lee, T.-W.; Robertson, A.; Leckie, J. Video methods in the quantification of children’s exposure. J. Expo. Anal. Environ. Epid. 2006, 16, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Zartarian, V.; Ferguson, A.; Leckie, J. Quantified dermal activity data from a four-child pilot field study. J. Expos. Anal. Environ. Epidem. 1997, 7, 543–553. [Google Scholar]
- Kwong, L.; Ercumen, A.; Pickering, A.J.; Unicomb, L.; Davis, J.; Luby, S. Hand- and object-mouthing of rural Bangladeshi children 3–18 months old. Int. J. Environ. Public Health 2016, 13, 521. [Google Scholar] [CrossRef] [PubMed]
- Environmental Protection Agency. Children’s Specific Exposure Factors Handbook; EPA/600/R-06/096F; Environmental Protection Agency: Washington, DC, USA, 2008.
- Environmental Protection Agency. Child-Specific Exposures Scenario Examples; EPA 600/R-14/217F; Environmental Protection Agency: Washington, DC, USA, 2014.
- Environmental Protection Agency. Exposure Factors Handbook 2011 Edition (Final); EPA/600/R-09/052F; Environmental Protection Agency: Washington, DC, USA, 2011.
- Kumar, N. The exposure uncertainty analysis: Of the association between birth weight and trimester specific exposure to particulate matter (PM2.5 vs. PM10). Int. J. Environ. Res. Public Health 2016, 13, 906. [Google Scholar] [CrossRef] [PubMed]
- Ginsberg, G.; Ginsberg, J.; Foos, B. Approaches to children’s exposure assessment: Case study with diethylhexylphthalate (DEHP). Int. J. Environ. Res. Public Health 2016, 13, 670. [Google Scholar] [CrossRef] [PubMed]
- Calafat, A.M.; Longnecker, M.; Koch, H.; Swan, S.; Hauser, R.; Goldman, L.; Lanphear, B.; Rudel, R.; Engel, S.; Teitelbaum, S.; et al. Optimal exposure biomarkers for nonpersistent chemical in environmental epidemiology. Environ. Health Perspect. 2015, 123, A166–A167. [Google Scholar] [CrossRef] [PubMed]
- Sly, P.; Eskenazi, B.; Pronczuk, J.; Sram, R.; Diaz-Barriga, F.; Gonzalez Machin, D.; Carpenter, D.; Surdu, S.; Meslin, E. Ethical issues in measuring biomarkers in children’s environmental health. Environ. Health Perspect. 2009, 117, 1185–1190. [Google Scholar] [CrossRef] [PubMed]
- Neri, M.; Bonassi, S.; Knudsen, L.; Sram, R.; Holland, N.; Ugolini, D.; Merlo, D. Children’s exposure to environmental pollutants and biomarkers of genetic change. I. Overview of critical issues. Mutat. Res. 2016, 612, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Arbuckle, T. Maternal-infant biomonitoring of environmental chemicals: The epidemiologic challenges. Birth Defects Res. A Clin. Mol. Teratol. 2010, 88, 931–937. [Google Scholar] [CrossRef] [PubMed]
- Schoeters, G.; Hond, D.; Koppen, G.; Smolders, R.; Bloemen, K.; De Boever, P.; Govarts, E. Biomonitoring and biomarkers to unravel the risks from prenatal environmental exposures for later health outcomes. Am. J. Clin. Nutr. 2016, 94, 1964S–1969S. [Google Scholar] [CrossRef] [PubMed]
- Environmental Protection Agency. Science Policy Council Handbook: Risk Characterization. Available online: https://www.epa.gov/sites/production/files/2015-10/documents/osp_risk_characterization_handbook_2000.pdf (accessed on 2 December 2016).
- Environmental Protection Agency. Human Health Risk Assessment. Available online: https://www.epa.gov/risk/human-health-risk-assessment (accessed on 2 December 2016).
- Haas, C.N.; Rose, J.B.; Gerba, C.P. Quantitative Microbial Risk Assessment, 1st ed.; John Wiley & Sons, Inc.: New York, NY, USA, 1999. [Google Scholar]
- Cifuentes, E.; Trasande, L.; Ramirez, M.; Landrigan, P. A qualitative analysis of environmental policy and children’s health in Mexico. Environ. Health 2010, 9, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldman, L. Linking research and policy to ensure children’s environmental health. Environ. Health Perspect. 1998, 106, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Environmental Protection Agency. About the TSCA Chemical Substance Inventory. Available online: https://www.epa.gov/tsca-inventory/about-tsca-chemical-substance-inventory#whatdoesitmean (accessed on 12 December 2016).
- ECHA: European Chemical Agency. REACH. Available online: https://echa.europa.eu/regulations/reach (accessed on 5 December 2016).
- Environmental Protection Agency. The U.S. Environmental Protection Agency’s Strategic Plan for Evaluating the Toxicity of Chemical. 2009. Available online: https://nepis.epa.gov/Exe/ZyNET.exe/P1003351.TXT?ZyActionD=ZyDocument&Client=EPA&Index=2006+Thru+2010&Docs=&Query=&Time=&EndTime=&SearchMethod=1&TocRestrict=n&Toc=&TocEntry=&QField=&QFieldYear=&QFieldMonth=&QFieldDay=&IntQFieldOp=0&ExtQFieldOp=0&XmlQuery=&File=D%3A%5Czyfiles%5CIndex%20Data%5C06thru10%5CTxt%5C00000007%5CP1003351.txt&User=ANONYMOUS&Password=anonymous&SortMethod=h%7C-&MaximumDocuments=1&FuzzyDegree=0&ImageQuality=r75g8/r75g8/x150y150g16/i425&Display=hpfr&DefSeekPage=x&SearchBack=ZyActionL&Back=ZyActionS&BackDesc=Results%20page&MaximumPages=1&ZyEntry=1&SeekPage=x&ZyPURL (accessed on 1 March 2009). [Google Scholar]
- Krewski, D.; Westphal, M.; Anderson, M.; Paoli, G.; Weihsueh, A.; Zoughool, M.; Croteau, M.; Burgoon, L.; Cote, I. A framework for the next generation of risk science. Environ. Health Perspect. 2014, 122, 796–805. [Google Scholar] [CrossRef] [PubMed]
- Environmental Protection Agency. The Frank R. Lautenberg Checial Safety for the 21rst Century Act. Available online: https://www.epa.gov/assessing-and-managing-chemicals-under-tsca/frank-r-lautenberg-chemical-safety-21st-century-act. (accessed on 27 February 2017).
- Pratt, G.C.; Vadali, M.L.; Kyale, D.L.; Ellickson, K.M. Traffic, air pollution, minority and socio-economic status: Addressing inequities in exposure and risk. Int. J. Environ. Res. Public Health 2015, 19, 5355–5372. [Google Scholar] [CrossRef] [PubMed]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferguson, A.; Penney, R.; Solo-Gabriele, H. A Review of the Field on Children’s Exposure to Environmental Contaminants: A Risk Assessment Approach. Int. J. Environ. Res. Public Health 2017, 14, 265. https://doi.org/10.3390/ijerph14030265
Ferguson A, Penney R, Solo-Gabriele H. A Review of the Field on Children’s Exposure to Environmental Contaminants: A Risk Assessment Approach. International Journal of Environmental Research and Public Health. 2017; 14(3):265. https://doi.org/10.3390/ijerph14030265
Chicago/Turabian StyleFerguson, Alesia, Rosalind Penney, and Helena Solo-Gabriele. 2017. "A Review of the Field on Children’s Exposure to Environmental Contaminants: A Risk Assessment Approach" International Journal of Environmental Research and Public Health 14, no. 3: 265. https://doi.org/10.3390/ijerph14030265





