Validity and Reproducibility of the Iodine Dietary Intake Questionnaire Assessment Conducted for Young Polish Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Designing an Iodine Dietary Intake Questionnaire: Iodine Dietary Intake Evaluation-Food Frequency Questionnaire (IODINE-FFQ)
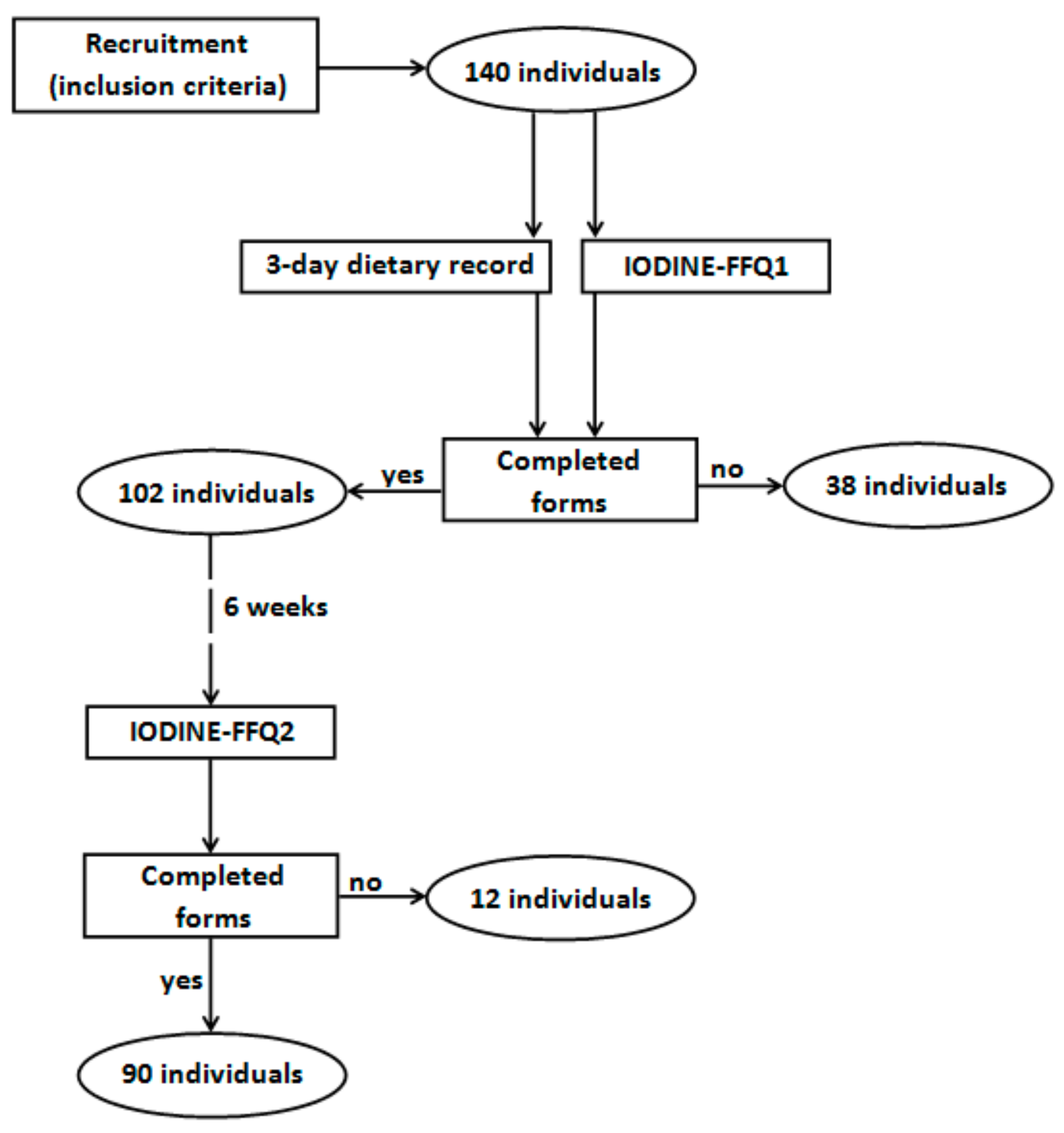
2.2. Validation of the IODINE-FFQ
2.3. Statistical Analysis
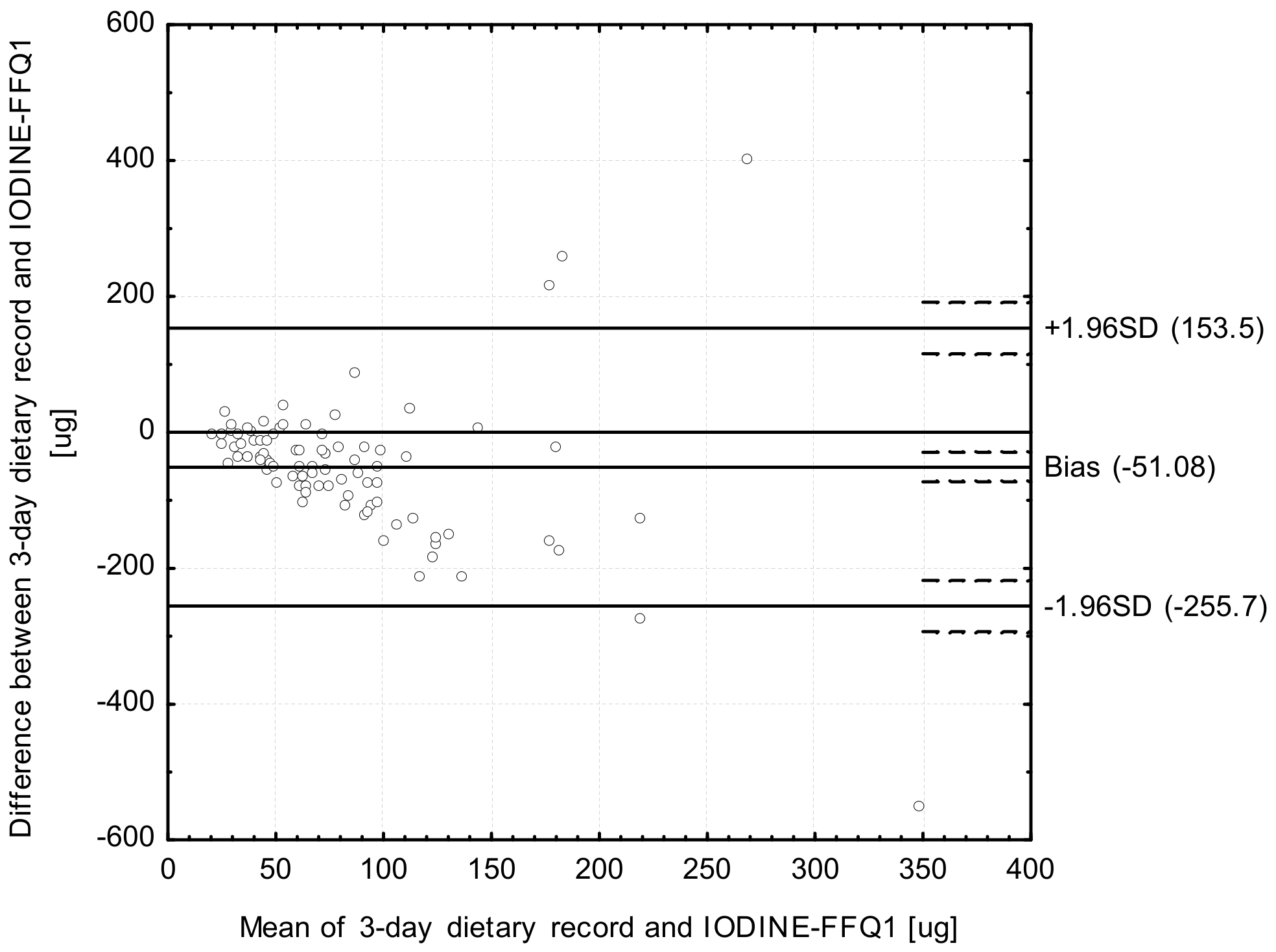
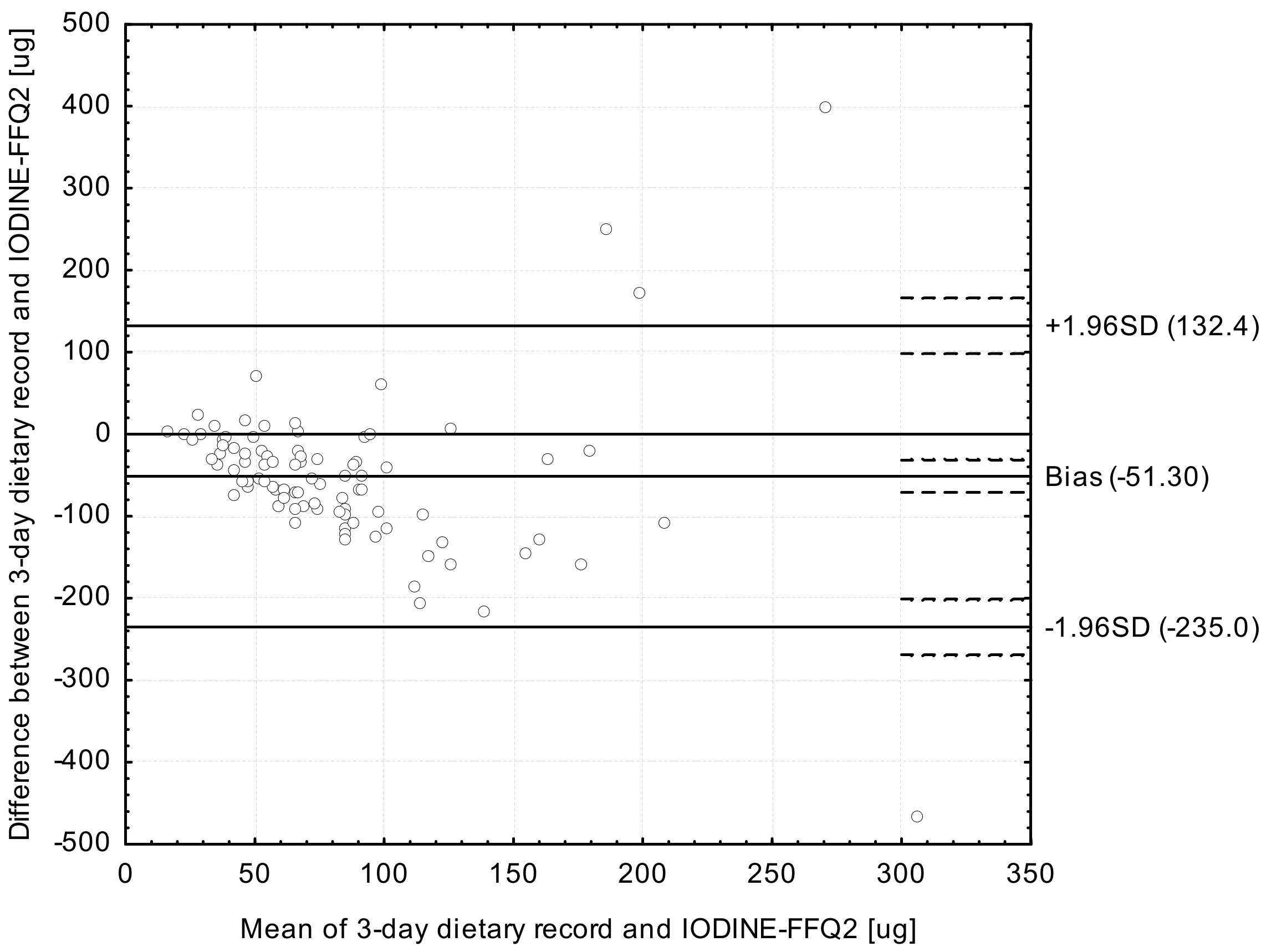
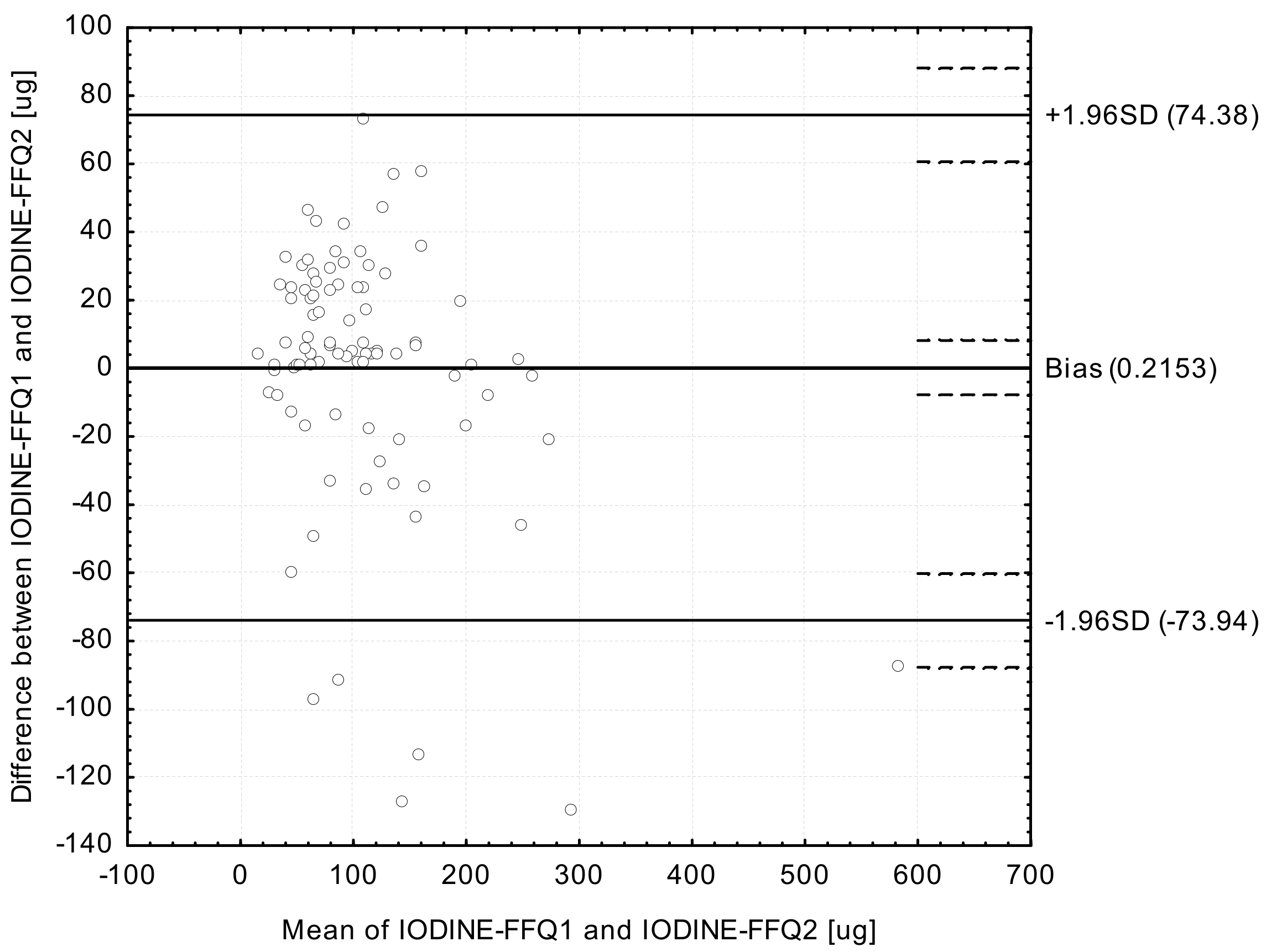
- Analysis of the Bland-Altman plots in the assessment of validity (IODINE-FFQ1 vs. 3-day record; IODINE-FFQ2 vs. 3-day record) and of reproducibility (IODINE-FFQ1 vs. IODINE-FFQ2)—the results were interpreted using the Bland-Altman index, whereas the limit of agreement values (LOA) were calculated as the sum of the mean absolute differences of iodine intake measured by the two methods, and the ± standard deviation of the absolute difference of iodine intake recorded for the two methods magnified by 1.96. In the analysis conducted with the Bland-Altman method to assess agreement between the measurements, a Bland-Altman index of a maximum of 5% (95% of individuals observed to be beyond the LOA) was interpreted, as commonly assumed [30], as positive validation of the method of measurement.
- Calculation of the root mean square errors of prediction (RMSEP) and median absolute percentage errors (MdAPE) of iodine intake in the assessment of validity (IODINE-FFQ1 vs. 3-day record; IODINE-FFQ2 vs. 3-day record) and of reproducibility (IODINE-FFQ1 vs. IODINE-FFQ2).
- Assessment of the share of individuals classified into the same tertile and misclassified (classified into opposite tertiles) in the assessment of validity (IODINE-FFQ1 vs. 3-day record; IODINE-FFQ2 vs. 3-day record) and of reproducibility (IODINE-FFQ1 vs. IODINE-FFQ2).
- Calculation of the weighted κ statistic with linear weighting to indicate the level of agreement between the classifications into tertiles in the assessment of validity (IODINE-FFQ1 vs. 3-day record; IODINE-FFQ2 vs. 3-day record) and of reproducibility (IODINE-FFQ1 vs. IODINE-FFQ2)—according to the criteria of Landis and Koch [31], values <0.20 were treated as slight agreement, 0.21–0.40—as fair, 0.41–0.60—as moderate, 0.61–0.80—as substantial, and 0.81–1.0—as almost perfect agreement.
- Assessment of the share of individuals classified into the same category (both of either adequate or inadequate intake) and of the conflicting intake adequacy category (adequate intake and inadequate intake) in the assessment of validity (IODINE-FFQ1 vs. 3-day record; IODINE-FFQ2 vs. 3-day record) and of reproducibility (IODINE-FFQ1 vs. IODINE-FFQ2). The adequate intake was defined according to the Polish recommendations for women on the Estimated Average Requirement (EAR) level as 95 µg [32].
- Analysis of the correlations between results obtained in the assessment of validity (IODINE-FFQ1 vs. 3-day record; IODINE-FFQ2 vs. 3-day record) and of reproducibility (IODINE-FFQ1 vs. IODINE-FFQ2)—the normality of distribution of the results was analysed using the Shapiro-Wilk test and then Spearman’s rank correlation was applied for nonparametric distribution.
3. Results
4. Discussion
4.1. Iodine Intake
4.2. Comprehensive Food Frequency Questionnaires to Assess Iodine Intake
4.3. Validation of Brief Iodine-Specific Food Frequency Questionnaire
5. Conclusions
Author Contributions
Conflicts of Interest
References
- World Health Organization (WHO). Iodine Status Worldwide; WHO: Geneva, Switzerland, 2004. [Google Scholar]
- De Benois, B.; McLean, E.; Andersson, M.; Rogers, L. Iodine deficiency in 2007: Global progress since 2003. Food Nutr. Bull. 2008, 29, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Andersson, M.; Karumbunathan, V.; Zimmermann, M.B. Global iodine status in 2011 and trends over the past decade. J. Nutr. 2012, 142, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Szybinski, Z.; Delange, F.; Lewinski, A.; Podoba, J.; Rybakowa, M.; Wasik, R.; Szewczyk, L.; Huszno, B.; Gołkowski, F.; Przybylik-Mazurek, E.; et al. A programme of iodine supplementation using only iodised household salt is efficient—The case of Poland. Eur. J. Endocrinol. 2001, 144, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Rapa, A.; Marinello, D.; Chiorboli, E.; Sacco, F.; Bona, G. Iodine deficiency in Italy. Italian study group on urinary iodine of SIEDP. Lancet 1999, 354, 596–597. [Google Scholar] [CrossRef]
- Valeix, P.; Zarebska, M.; Preziosi, P.; Galan, P.; Pelletier, B.; Hercberg, S. Iodine deficiency in France. Lancet 1999, 353, 1766–1767. [Google Scholar] [CrossRef]
- Delange, F.; Van Onderbergen, A.; Shabana, W.; Vandemeulebroucke, E.; Vertongen, F.; Gnat, D.; Dramaix, M. Silent iodine prophylaxis in Western Europe only partly corrects iodine deficiency: The case of Belgium. Eur. J. Endocrinol. 2000, 143, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.B.; Ovesen, L.; Bülow, I.; Jørgensen, T.; Knudsen, N.; Laurberg, P.; Pertild, H. Dietary iodine intake and urinary iodine excretion in a Danish population: Effect of geography, supplements and food choice. Br. J. Nutr. 2002, 87, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B.; Jooste, P.L.; Pandav, C.S. Iodine-deficiency disorders. Lancet 2008, 372, 1251–1262. [Google Scholar] [CrossRef]
- Garnweidner-Holme, L.; Aakre, I.; Lilleengen, A.M.; Brantsæter, A.L.; Henjum, S. Knowledge about iodine in pregnant and lactating women in the Oslo area, Norway. Nutrients 2017, 9, 493. [Google Scholar] [CrossRef] [PubMed]
- Cade, J.; Thompson, R.; Burley, V.; Warm, D. Development, validation and utilisation of food-frequency questionnaires—A review. Public Health Nutr. 2002, 5, 567–587. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Pfrimer, K.; Doreste-Alonso, J.; Ribas-Barba, L.; Sánchez-Villegas, A.; Ortiz-Andrellucchi, A.; Henríquez-Sánchez, P. Dietary assessment methods for intakes of iron, calcium, selenium, zinc and iodine. Br. J. Nutr. 2009, 102, 38–55. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, L.B.; Ovesen, L.; Bülow, I.; Jørgensen, T.; Knudsen, N.; Laurberg, P.; Perrild, H. Evaluation of a semi-quantitative food frequency questionnaire to estimate iodine intake. Eur. J. Clin. Nutr. 2001, 55, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.; Quayle, A.; Phillips, D.I. Iodine intake and excretion in two British Towns: Aspects of questionnaire validation. Hum. Nutr. Appl. Nutr. 1987, 41, 187–192. [Google Scholar] [PubMed]
- Combet, E.; Lean, M.E. Validation of a short food frequency questionnaire specific for iodine in UK Females of childbearing age. J. Hum. Nutr. Diet. 2014, 27, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Condo, D.; Makrides, M.; Skeaff, S.; Zhou, S.J. Development and validation of an iodine-specific FFQ to estimate iodine intake in Australian pregnant women. Br. J. Nutr. 2015, 113, 944–952. [Google Scholar] [CrossRef] [PubMed]
- Taib, S.; Isa, Z. Dietary iodine from interview-based semi-quantitative food frequency questionnaire: Correlation with 24 h dietary recall. Pakistan J. Nutr. 2013, 12, 688–691. [Google Scholar] [CrossRef]
- Kowalkowska, J.; Slowinska, M.A.; Slowinski, D.; Dlugosz, A.; Niedzwiedzka, E.; Wadolowska, L. Comparison of a full food-frequency questionnaire with the three-day unweighted food records in young Polish adult women, implications for dietary assessment. Nutrients 2013, 19, 2747–2776. [Google Scholar] [CrossRef] [PubMed]
- Kunachowicz, H.; Nadolna, J.; Przygoda, B.; Iwanow, K. Food Composition Tables; PZWL Państwowy Zakład Wydawnictw Lekarskich (State Publishing House for Medicine): Warsaw, Poland, 2005. (In Polish) [Google Scholar]
- Finglas, P.; Weichselbaum, E.; Buttriss, J.L. The 3rd International EuroFIR Congress 2009: European food composition data for better diet, nutrition and food quality. Eur. J. Clin. Nutr. 2010, 64, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Głąbska, D.; Włodarek, D. Minerals. In Diet Therapy; Włodarek, D., Lange, E., Kozłowska, L., Głąbska, D., Eds.; PZWL Medical Publishing Group: Warsaw, Poland, 2014. (In Polish) [Google Scholar]
- Lewiński, A.; Zygmunt, A. Iodine prophylaxis in Poland—New, old challenges. Ann. Agric. Environ. Med. 2014, 21, 1–4. [Google Scholar] [PubMed]
- Głąbska, D.; Guzek, D.; Sidor, P.; Włodarek, D. Vitamin D Dietary intake questionnaire validation conducted among young Polish women. Nutrients 2016, 8, 36. [Google Scholar] [CrossRef] [PubMed]
- Głąbska, D.; Guzek, D.; Ślązak, J.; Włodarek, D. Assessing the validity and reproducibility of an iron dietary intake questionnaire conducted in a group of young Polish women. Nutrients 2017, 9, 199. [Google Scholar] [CrossRef] [PubMed]
- Szponar, L.; Wolnicka, K.; Rychlik, E. Atlas of Food Products and Dishes Portion Sizes; IŻŻ: Warsaw, Poland, 2012. (In Polish) [Google Scholar]
- Willett, W.; Lenart, E. Reproducibility ad validity of food frequency questionnaires. In Nutritional Epidemiology, 3rd ed.; Oxford University Press: Oxford, UK, 1985. [Google Scholar]
- European Commission. Opinion of the Scientific Committee on Food on the Tolerable Upper Intake Level of Iodine. Available online: https://ec.europa.eu/food/sites/food/files/safety/docs/sci-com_scf_out146_en.pdf (accessed on 10 June 2017).
- Joint FAO/WHO Expert Consultation on Human Vitamin and Mineral Requirements. Vitamin and Mineral Requirements in Human Nutrition: Report of a Joint Fao/Who Expert Consultation. Available online: http://www.fao.org/docrep/004/y2809e/y2809e00.htm#Contents (accessed on 10 June 2017).
- Ortega, R.M.; Pérez-Rodrigo, C.; López-Sobaler, A.M. Dietary assessment methods: Dietary records. Nutr. Hosp. 2015, 26, 38–45. [Google Scholar] [CrossRef]
- Myles, P.S.; Cui, J. Using the Bland-Altman method to measure agreement with repeated measures. Br. J. Anaesth. 2007, 99, 309–311. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Jarosz, M. Human Nutrition Recommendations for Polish Population; IŻŻ Instytut Żywności i Żywienia (National Food and Nutrition Institute): Warsaw, Poland, 2012. (In Polish) [Google Scholar]
- Gunnarsdottir, I.; Gustavsdottir, A.G.; Steingrimsdottir, L.; Maage, A.; Johannesson, A.J.; Thorsdottir, I. Iodine status of pregnant women in a population changing from high to lower fish and milk consumption. Public Health Nutr. 2013, 16, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Birgisdottir, B.E.; Knutsen, H.K.; Haugen, M.; Gjelstad, I.M.; Jenssen, M.T.; Ellingsen, D.G.; Thomassen, Y.; Alexander, J.; Meltzer, H.M.; Brantsæter, A.L. Essential and toxic element concentrations in blood and urine and their associations with diet: Results from a Norwegian population study including high-consumers of seafood and game. Sci. Total Environ. 2013, 1, 836–844. [Google Scholar] [CrossRef] [PubMed]
- Gunnarsdottir, I.; Gunnarsdottir, B.E.; Steingrimsdottir, L.; Maage, A.; Johannesson, A.J.; Thorsdottir, I. Iodine status of adolescent girls in a population changing from high to lower fish consumption. Eur. J. Clin. Nutr. 2010, 64, 958–964. [Google Scholar] [CrossRef] [PubMed]
- Kunachowicz, H.; Stos, K.; Stibilj, V.; Szponar, L.; Okolska, G.; Wojtasik, A.; Ratkovska, B. Studies on iodine content in daily diets, particularly elderly people’s diets. J. Nutr. Health Aging 2002, 6, 127–129. [Google Scholar] [PubMed]
- Zatońska, K.; Campos, H.; Ilow, R.; Janik-Koncewicz, K.; Różańska, D.; Regulska-Ilow, B.; Połtyn-Zaradna, K.; Szuba, A.; Zatoński, W.A. Dietary intake and adipose tissue level of specific fatty acids in a selected group from the Lower Silesia population. Ann. Agric. Environ. Med. 2012, 19, 389–394. [Google Scholar] [PubMed]
- Rasmussen, L.B.; Carlé, A.; Jørgensen, T.; Knudsen, N.; Laurberg, P.; Pedersen, I.B.; Perrild, H.; Vejbjerg, P.; Ovesen, L. Iodine intake before and after mandatory iodization in Denmark: Results from the Danish Investigation of Iodine Intake and Thyroid Diseases (DanThyr) study. Br. J. Nutr. 2008, 100, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Brantsaeter, A.L.; Haugen, M.; Thomassen, Y.; Ellingsen, D.G.; Ydersbond, T.A.; Hagve, T.A.; Alexander, J.; Meltzer, H.M. Exploration of biomarkers for total fish intake in pregnant Norwegian women. Public Health Nutr. 2010, 13, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Dahl, L.; Mæland, C.A.; Bjørkkjær, T. A short food frequency questionnaire to assess intake of seafood and n-3 supplements: Validation with biomarkers. Nutr. J. 2011, 19, 127. [Google Scholar] [CrossRef] [PubMed]
- World Bank. Enriching lives. In Overcoming Vitamin and Mineral Malnutrition in Developing Countries; World Bank: Washington, DC, USA, 1994. [Google Scholar]
- Rasmussen, L.B.; Jørgensen, T.; Perrild, H.; Knudsen, N.; Krejbjerg, A.; Laurberg, P.; Pedersen, I.B.; Bjergved, L.; Ovesen, L. Mandatory iodine fortification of bread and salt increases iodine excretion in adults in Denmark—A 11-year follow-up study. Clin. Nutr. 2014, 33, 1033–1040. [Google Scholar] [CrossRef] [PubMed]
- Phillips, D.I. Iodine, milk, and the elimination of endemic goitre in Britain: The story of an accidental public health triumph. J. Epidemiol. Community Health 1997, 51, 391–393. [Google Scholar] [CrossRef] [PubMed]
- Foo, L.C.; Zainab, T.; Goh, S.Y.; Letchuman, G.R.; Nafikudin, M.; Doraisingam, P.; Khalid, B. Iodization of village water supply in the control of endemic iodine deficiency in rural Sarawak, Malaysia. Biomed. Environ. Sci. 1996, 9, 236–241. [Google Scholar] [PubMed]
- Štimec, M.; Kobe, H.; Smole, K.; Kotnik, P.; Sirca-Campa, A.; Zupancic, M.; Battelino, T.; Krzisnik, C.; Fidler Mis, N. Adequate iodine intake of Slovenian adolescents is primarily attributed to excessive salt intake. Nutr. Res. 2009, 29, 888–896. [Google Scholar] [CrossRef] [PubMed]
- Skeaff, S.A.; Lonsdale-Cooper, E. Mandatory fortification of bread with iodised salt modestly improves iodine status in schoolchildren. Br. J. Nutr. 2013, 109, 1109–1113. [Google Scholar] [CrossRef] [PubMed]
- Edmonds, J.C.; McLean, R.M.; Williams, S.M.; Skeaff, S.A. Urinary iodine concentration of New Zealand adults improves with mandatory fortification of bread with iodised salt but not to predicted levels. Eur. J. Nutr. 2016, 55, 1201–1212. [Google Scholar] [CrossRef] [PubMed]
- McNulty, B.A.; Nugent, A.P.; Walton, J.; Flynn, A.; Tlustos, C.; Gibney, M.J. Iodine intakes and status in Irish adults: Is there cause for concern? Br. J. Nutr. 2017, 117, 422–431. [Google Scholar] [CrossRef] [PubMed]
- Brantsæter, A.L.; Abel, M.H.; Haugen, M.; Meltzer, H.M. Risk of suboptimal iodine intake in pregnant Norwegian women. Nutrients 2013, 5, 424–440. [Google Scholar] [CrossRef] [PubMed]
- Lumen, A.; George, N.I. Estimation of iodine nutrition and thyroid function status in late-gestation pregnant women in the United States: Development and application of a population-based pregnancy model. Toxicol. Appl. Pharmacol. 2017, 1, 24–38. [Google Scholar] [CrossRef] [PubMed]
- Beck, K.L.; Kruger, R.; Conlon, C.; Heath, A.L.; Coad, J.; Matthys, C.; Jones, B.; Stonehouse, W. The relative validity and reproducibility of an iron food frequency questionnaire for identifying iron-related dietary patterns in young women in New Zealand. J. Acad. Nutr. Diet. 2012, 112, 1177–1187. [Google Scholar] [CrossRef] [PubMed]
- Roman-Viñas, B.; Ortiz-Andrellucchi, A.; Mendez, M.; Sánchez-Villegas, A.; Peña Quintana, L.; Aznar, L.A.; Hermoso, M.; Serra-Majem, L. Is the food frequency questionnaire suitable to assess micronutrient intake adequacy for infants, children and adolescents? Matern. Child. Nutr. 2010, 6, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Gibson, R.S. Sources of error and variability in dietary assessment methods, a review. J. Can. Diet. Assoc. 1987, 48, 150–155. [Google Scholar]
- Yang, Y.J.; Kim, M.K.; Hwang, S.H.; Ahn, Y.; Shim, J.E.; Kim, D.H. Relative validities of 3-day food records and the food frequency questionnaire. Nutr. Res. Pract. 2010, 4, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Food and Agriculture Organization of the United Nations/World Health Organization (FAO/WHO). Preparation and Use of Food-Based Dietary Guidelines, Report of a Joint FAO/WHO Consultation Nicosia, Cyprus; WHO: Geneva, Switzerland, 1996. [Google Scholar]
- Welch, A.A. Dietary intake measurement—Methodology. In Encyclopedia of Human Nutrition; Elsevier Academic Press: Oxford, UK, 2005; pp. 7–16. [Google Scholar]
- Córdoba-Caro, L.G.; Luego Pérez, M.L.; García Preciado, V. Nutritional adequacy of students of compulsory secondary education in Badajoz. Nutr. Hosp. 2012, 27, 1065–1071. [Google Scholar] [PubMed]
- Balali-Mood, M.B.; Zilaee, M.; Ghayour-Mobarhan, M.G.; Sheikh-Andalibi, M.S.; Mohades-Ardabili, H.; Dehghani, H.; Ferns, G. Comparison of dietary Macro and micro nutrient intake between Iranian patients with long-term complications of sulphur mustard poisoning and healthy subjects. Malays. J. Med. Sci. 2014, 21, 19–26. [Google Scholar]
- Moreira, P.; Sampaio, D.; Almeida, M.D.V. Validade relativa de um questionário de frequência de consumo alimentar através da comparação com um registo alimentar de quatro dias. Acta Med. Port. 2003, 16, 412–420. [Google Scholar] [PubMed]
- Sauvageot, N.; Alkerwi, A.; Albert, A.; Guillaume, M. Use of food frequency questionnaire to assess relationships between dietary habits and cardiovascular risk factors in NESCAV study: Validation with biomarkers. Nutr. J. 2013, 12, 143. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Moon, S.J.; Kim, K.R.; Sohn, C.Y.; Oh, J.J. Dietary iodine intake and urinary iodine excretion in normal Korean adults. Yonsei. Med. J. 1998, 39, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Feng, R.N.; Du, S.S.; Chen, Y.; Li, Z.; Zhang, Y.F.; Sun, C.H.; Jiang, Y.S. An internet-based food frequency questionnaire for a large Chinese population. Asia Pac. J. Clin. Nutr. 2016, 25, 841–848. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, K.; Jwa, S.C.; Kobayashi, M.; Morisaki, N.; Sago, H.; Fujiwara, T. Validation of a food frequency questionnaire for Japanese pregnant women with and without nausea and vomiting in early pregnancy. J. Epidemiol. 2017, 27, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Mouratidou, T.; Ford, F.; Fraser, R.B. Validation of a food-frequency questionnaire for use in pregnancy. Public Health Nutr. 2006, 9, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Khalesi, S.; Doshi, D.; Buys, N.; Sun, J. Validation of a short food frequency questionnaire in Australian adults. Int. J. Food Sci. Nutr. 2017, 68, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Qiu, X.; Zhong, C.; Zhang, K.; Xiao, M.; Yi, N.; Xiong, G.; Wang, J.; Yao, J.; Hao, L.; et al. Reproducibility and relative validity of a semi-quantitative food frequency questionnaire for Chinese pregnant women. Nutr. J. 2015, 4, 56. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Codling, K.; Chang, S.; Zhang, S.; Shen, H.; Su, X.; Chen, Z.; Scherpbier, W.; Yan, J. Eliminating Iodine Deficiency in China: Achievements, Challenges and Global Implications. Nutrients 2017, 9, 361. [Google Scholar] [CrossRef] [PubMed]
- Štimec, M.; Mis, N.F.; Smole, K.; Sirca-Campa, A.; Kotnik, P.; Zupancic, M.; Battelino, T.; Krizisnik, C. Iodine intake of Slovenian adolescents. Ann. Nutr. MeTable 2007, 51, 439–447. [Google Scholar] [CrossRef] [PubMed]
- Willett, W. Nutritional Epidemiology, 2nd ed.; Oxford University Press: New York, NY, USA, 1998. [Google Scholar]
- Barrett, J.S.; Gibson, P.R. Development and validation of a comprehensive semi-quantitative food frequency questionnaire that includes FODMAP intake and glycemic index. J. Am. Diet. Assoc. 2010, 110, 1469–1476. [Google Scholar] [CrossRef] [PubMed]
- Tucker, K.L. Dietary surveys. In Encyclopedia of Human Nutrition; Elsevier Academic Press: Oxford, UK, 2005; pp. 27–32. [Google Scholar]
- Dahl, L.; Meltzer, H.M.; Opsahl, J.A.; Julshamn, K. Iodine intake and status in two groups of Norwegians. Scand. J. Food Nutr. 2007, 47, 170–178. [Google Scholar] [CrossRef]
- Fuse, Y.; Shishiba, Y.; Irie, M. Gestational changes of thyroid function and urinary iodine in thyroid antibody-negative Japanese women. Endocr. J. 2013, 60, 1095–1106. [Google Scholar] [CrossRef] [PubMed]
- Willett, W. Invited commentary, a further look at dietary questionnaire validation. Am. J. Epidemiol. 2001, 154, 1100–1102. [Google Scholar] [CrossRef] [PubMed]
- Brantsæter, A.L.; Haugen, M.; Alexander, J.; Meltzer, H.M. Validity of a new food frequency questionnaire for pregnant women in the Norwegian Mother and Child Cohort Study (MoBa). Matern. Child. Nutr. 2008, 4, 28–43. [Google Scholar] [CrossRef] [PubMed]
- Brantsæter, A.L.; Haugen, M.; Julshamn, K.; Alexander, J.; Meltzer, H.M. Evaluation of urinary iodine excretion as a biomarker for intake of milk and dairy products in pregnant women in the Norwegian Mother and Child Cohort Study (MoBa). Eur. J. Clin. Nutr. 2009, 63, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Vioque, J.; Navarrete-Muñoz, E.M.; Gimenez-Monzó, D.; García-de-la-Hera, M.; Granado, F.; Young, I.S.; Ramón, R.; Ballester, F.; Murcia, M.; Rebagliato, M.; et al. INMA-Valencia Cohort Study. Reproducibility and validity of a food frequency questionnaire among pregnant women in a Mediterranean area. Nutr. J. 2013, 19, 26. [Google Scholar] [CrossRef] [PubMed]
- Cade, J.E.; Burley, V.J.; Warm, D.L.; Thompson, R.L.; Margetts, B.M. Food-frequency questionnaires: A review of their design, validation and utilisation. Nutr. Res. Rev. 2004, 17, 5–22. [Google Scholar] [CrossRef] [PubMed]
| Group of Products | Products | Serving Size | Number of Servings per Week |
|---|---|---|---|
| Dairy products | Whet, sheep milk | 300 g (large glass) | |
| Milk and milk beverages (yoghurt, kefir, buttermilk, cream) | 300 g (large glass) | ||
| Milk powder | 10 g (tablespoon) | ||
| Condensed milk | 10 g (tablespoon) | ||
| Camembert, brie cheese | 150 g (packaging) | ||
| Rennet cheese | 20 g (thin slice) | ||
| Cottage cheese | 200 g (packaging) | ||
| Curd cheese, cream cheese spread | 30 g (thin slice, tablespoon) | ||
| Fromage frais | 150 g (packaging) | ||
| Processed cheese | 25 g (slice, triangle serving) | ||
| Eggs | 50 g (egg) | ||
| Meat | Offal, lamb | 100 g (palm of small hand) | |
| Veal | |||
| Other types of meat | |||
| Cold cuts | 15 g (thin slice of ham, 1/3 of wiener) | ||
| Fish | Cod, pollock | 100 g (palm of small hand) | |
| Plaice, halibut, tuna, mackerel, salmon | |||
| Flounder, herring, sole, sardine | |||
| Trout, pike, perch, eel, carp | |||
| Smoked eel | 50 g (half of palm of small hand) | ||
| Other smoked fishes | |||
| Fish products in tins and pickled herring | 50 g (half of small tin, rollmop) | ||
| Herring in a creamy sauce | 50 g (2 tablespoons) | ||
| Fats | 10 g (tablespoon) | ||
| Cereal products | Crispbread | 10 g (slice) | |
| Other types of bread | 30 g (slice, half of a roll) | ||
| Wheat bran | 5 g (tablespoon) | ||
| Cereals, cereal grains | 5 g (tablespoon) | ||
| Rice, pasta, groats | 100 g of cooked (glass) | ||
| Vegetables | Broccoli, spinach | 100 g (half of a glass, 1 glass of leafy vegetables) | |
| Radish, turnip, asparagus, broad bean, kale, green peas, chives | |||
| Other vegetables | |||
| Legumes | Peas | 15 g of dry (tablespoon) | |
| Other dry legumes | |||
| Potatoes | 50 g (2 tablespoons of puree) | ||
| Fruits | 100 g (half of a glass) | ||
| Nuts and seeds | Hazelnuts, peanuts | 30 g (handful) | |
| Other | |||
| Beverages | Coffee, tea | 250 g (glass) | |
| Fruit juices, beer | |||
| Wine | 150 g (wineglass) | ||
| Other | Chocolate | 20 g (3–4 chocolate bar squares) | |
| Iodine-fortified salt | 5 g (teaspoon) | ||
| Gelatin | |||
| Group of Products | Products | Serving Size | Iodine Content/Serving (µg) |
|---|---|---|---|
| Dairy products | Whet, sheep milk | 300 g (large glass) | 27.0 |
| Milk and milk beverages (yoghurt, kefir, buttermilk, cream) | 300 g (large glass) | 10.2 | |
| Milk powder | 10 g (tablespoon) | 3.2 | |
| Condensed milk | 10 g (tablespoon) | 1.2 | |
| Camembert, brie cheese | 150 g (packaging) | 17.4 | |
| Rennet cheese | 20 g (thin slice) | 6.9 | |
| Cottage cheese | 200 g (packaging) | 20.0 | |
| Curd cheese, cream cheese spread | 30 g (thin slice, tablespoon) | 1.0 | |
| Fromage frais | 150 g (packaging) | 4.2 | |
| Processed cheese | 25 g (slice, triangle serving) | 1.8 | |
| Eggs | 50 g (egg) | 4.7 | |
| Meat | Offal, lamb | 100 g (palm of small hand) | 3.3 |
| Veal | 2.2 | ||
| Other types of meat | 1.3 | ||
| Cold cuts | 15 g (thin slice of ham, 1/3 of wiener) | 2.1 | |
| Fish | Cod, pollock | 100 g (palm of small hand) | 94.4 |
| Plaice, halibut, tuna, mackerel, salmon | 48.6 | ||
| Flounder, herring, sole, sardine | 26.3 | ||
| Trout, pike, perch, eel, carp | 5.6 | ||
| Smoked eel | 50 g (half of palm of small hand) | 2.2 | |
| Other smoked fishes | 33.3 | ||
| Fish products in tins and pickled herring | 50 g (half of small tin, rollmop) | 23.9 | |
| Herring in a creamy sauce | 50 g (2 tablespoons) | 3.9 | |
| Fats | 10 g (tablespoon) | 0.3 | |
| Cereal products | Crispbread | 10 g (slice) | 1.4 |
| Other types of bread | 30 g (slice, half of a roll) | 0.7 | |
| Wheat bran | 5 g (tablespoon) | 1.6 | |
| Cereals, cereal grains | 5 g (tablespoon) | 0.2 | |
| Rice, pasta, groats | 100 g of cooked (glass) | 0.7 | |
| Vegetables | Broccoli, spinach | 100 g (half of a glass, 1 glass of leafy vegetables) | 13.5 |
| Radish, turnip, asparagus, broad bean, kale, green peas, chives | 5.9 | ||
| Other vegetables | 2.1 | ||
| Legumes | Peas | 15 g of dry (tablespoon) | 2.1 |
| Other dry legumes | 0.6 | ||
| Potatoes | 50 g (2 tablespoons of puree) | 1.5 | |
| Fruits | 100 g (half of a glass) | 1.6 | |
| Nuts and seeds | Hazelnuts, peanuts | 30 g (handful) | 15.0 |
| Other | 4.1 | ||
| Beverages | Coffee, tea | 250 g (glass) | 2.5 |
| Fruit juices, beer | 1.5 | ||
| Wine | 150 g (wineglass) | 52.5 | |
| Other | Chocolate | 20 g (3–4 chocolate bar squares) | 0.8 |
| Iodine-fortified salt | 5 g (teaspoon) | 114.6 | |
| Gelatin | 0.2 | ||
| 3-Day Dietary Record | IODINE-FFQ1 | IODINE-FFQ2 | |||
|---|---|---|---|---|---|
| Mean (µg) | 57.90 | 108.98 | 109.19 | ||
| Standard deviation (µg) | 65.78 | 86.28 | 72.95 | ||
| Median (µg) | 40.02 * | 90.06 * | 97.34 * | ||
| Minimum (µg) | 4.06 | 12.37 | 15.36 | ||
| Maximum (µg) | 469.18 | 625.11 | 537.95 | ||
| Share of individuals characterized in comparison with recommendation by Jarosz [25] | adequate intake | n | 9 | 41 | 46 |
| (%) | 10.00 | 45.46 | 51.11 | ||
| inadequate intake | n | 81 | 49 | 44 | |
| (%) | 90.00 | 54.44 | 48.89 | ||
| IODINE-FFQ1 vs. 3-Day Dietary Record | IODINE-FFQ2 vs. 3-Day Dietary Record | IODINE-FFQ1 vs. IODINE-FFQ2 | |||
|---|---|---|---|---|---|
| Individuals classified into the same tertile | n | 34 | 31 | 65 | |
| % | 37.78 | 34.44 | 72.22 | ||
| Individuals misclassified (classified into opposite tertiles) | n | 12 | 15 | 1 | |
| % | 13.33 | 16.67 | 1.11 | ||
| Weighted κ statistic | 0.15 | 0.075 | 0.675 | ||
| Individuals of the | same iodine intake adequacy category | n | 56 | 47 | 77 |
| % | 54.90 | 52.22 | 85.56 | ||
| conflicting iodine intake adequacy category | n | 46 | 43 | 13 | |
| % | 45.10 | 47.78 | 14.44 | ||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Głąbska, D.; Malowaniec, E.; Guzek, D. Validity and Reproducibility of the Iodine Dietary Intake Questionnaire Assessment Conducted for Young Polish Women. Int. J. Environ. Res. Public Health 2017, 14, 700. https://doi.org/10.3390/ijerph14070700
Głąbska D, Malowaniec E, Guzek D. Validity and Reproducibility of the Iodine Dietary Intake Questionnaire Assessment Conducted for Young Polish Women. International Journal of Environmental Research and Public Health. 2017; 14(7):700. https://doi.org/10.3390/ijerph14070700
Chicago/Turabian StyleGłąbska, Dominika, Ewa Malowaniec, and Dominika Guzek. 2017. "Validity and Reproducibility of the Iodine Dietary Intake Questionnaire Assessment Conducted for Young Polish Women" International Journal of Environmental Research and Public Health 14, no. 7: 700. https://doi.org/10.3390/ijerph14070700






