Factors Influencing the Accuracy of Infectious Disease Reporting in Migrants: A Scoping Review
Abstract
:1. Introduction
2. Methods
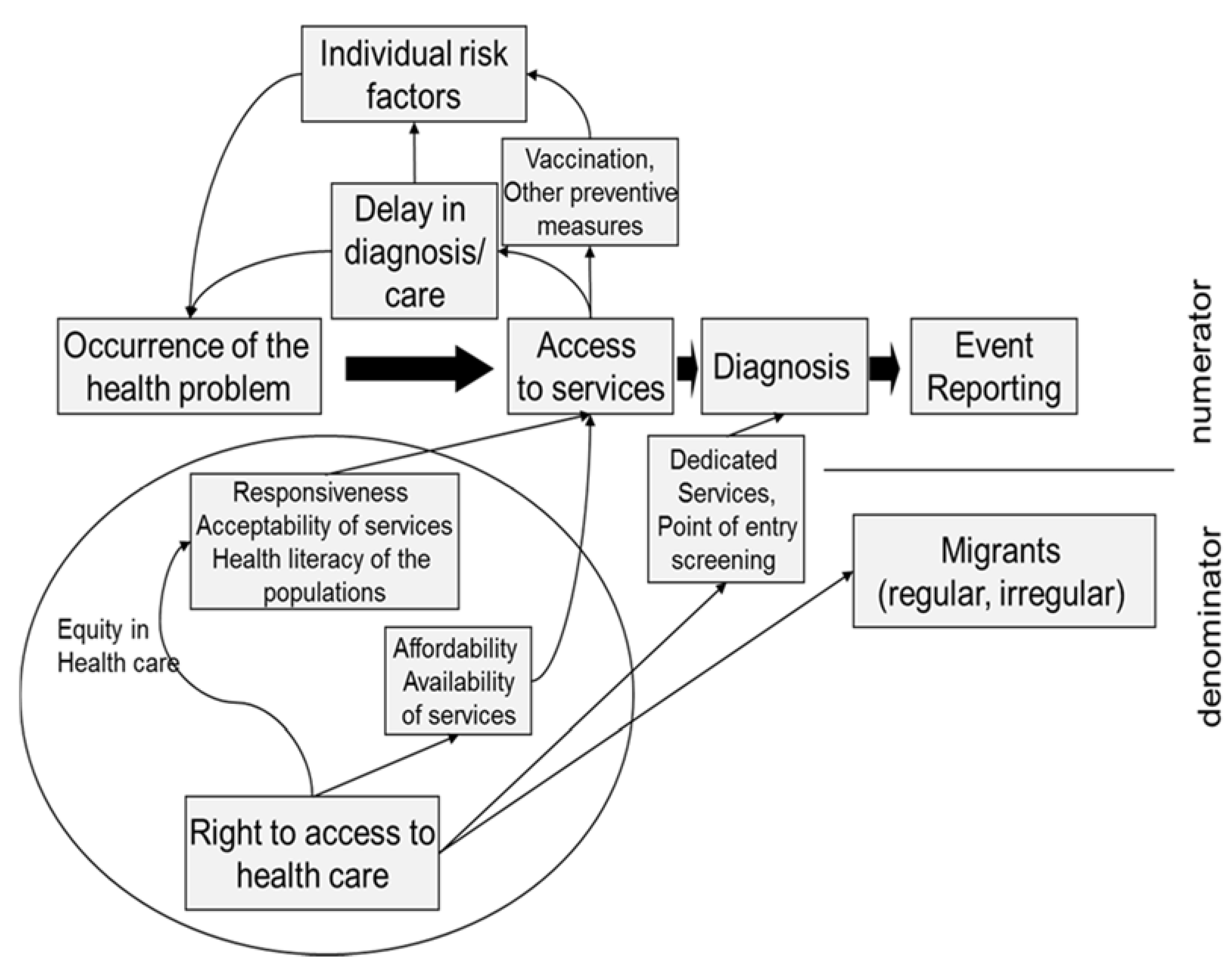
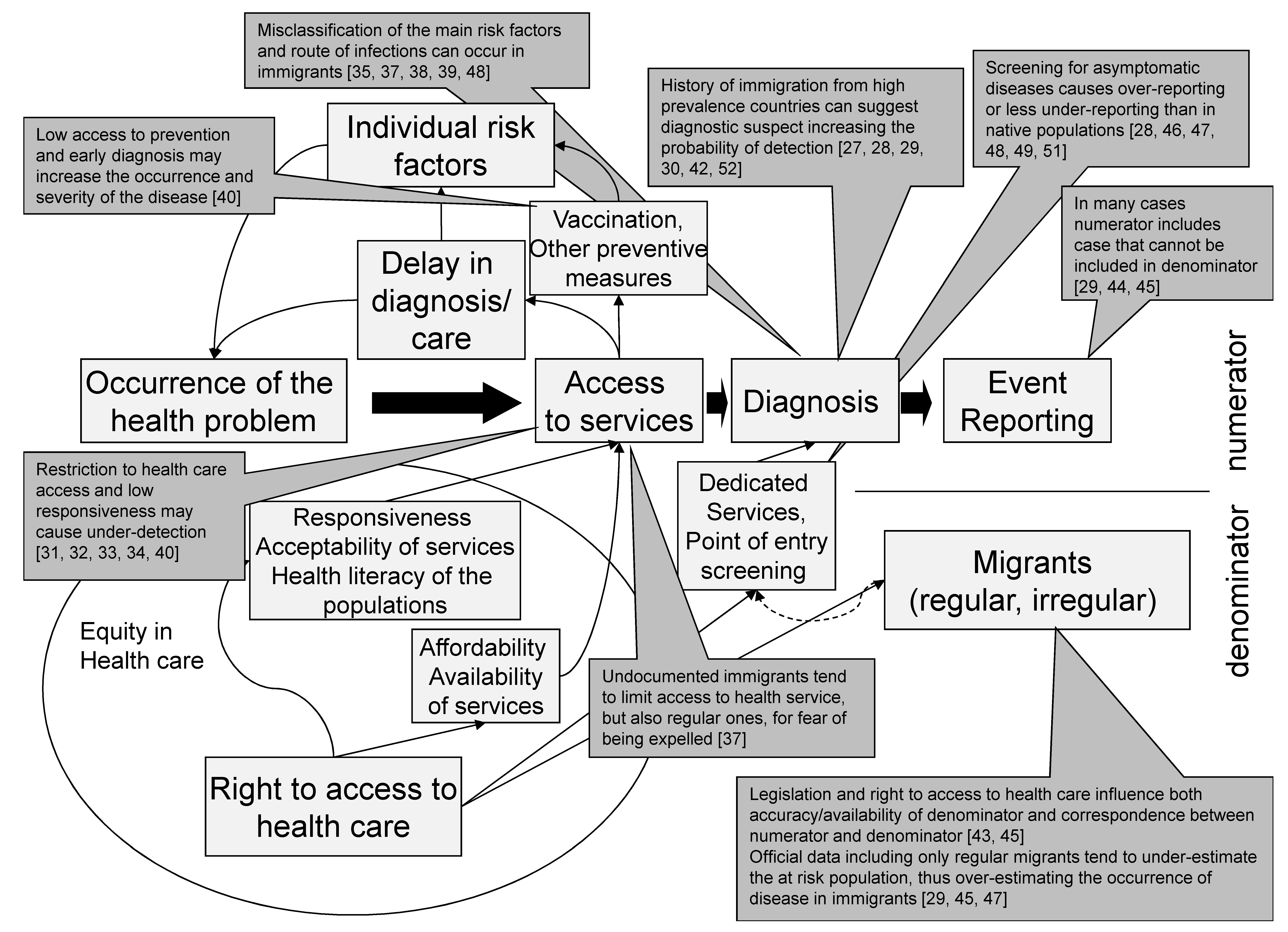
2.1. Mapping the Scoping Review
- Which are the possible barriers in access to health services that cause under-diagnosis and other mechanisms that can affect the number of reported events (under-reporting, over-reporting, biases in reporting).
- What are the key issues with respect to the definition of the at risk population, i.e., the denominator, and how they affect the accuracy of infectious disease occurrence indicators in migrants and their comparability with indicators in native populations.
- How can screening programs for infectious diseases targeting newly arrived migrants introduce bias in event reporting.
2.2. Eligibility Criteria and Search Strategy
2.3. Study Selection and Data Collection Process
2.4. Data Extraction and Synthesis
3. Results
3.1. Synthesis of the Literature Results: Misreporting
3.1.1. Possible Decrease of Under-Reporting
3.1.2. Possible Increase of Under-Reporting
3.1.3. Other Issues in Reporting Accuracy
3.1.4. Methods in Incidence/Prevalence Estimates
3.2. Synthesis of the Literature Results: Denominators
Missing or Estimated Denominator Data
3.3. Synthesis of the Literature Results: Screening
3.4. Risk of Biases of the Included Papers
4. Discussion
4.1. Limits
4.2. Main Findings
4.3. Implication for Surveillance Practice
- We should focus on improving the existing systems for native and migrant populations alike, with specific attention to under reporting in native populations (in particular for TB and meningitis). We believe this approach, as opposed to establishing special surveillance systems for migrant populations, would provide a better picture of the actual epidemiology of these diseases.
- Surveillance systems should be better characterized, through the inclusion of specific surveillance variables, the main risk factors for infectious diseases among migrants, i.e., country of origin [46,49,51], length of stay [48], and history of migration [46,52] in order to better understand the observed trends and plan public health interventions.
- Finally, some of the most relevant biases in estimating disease occurrence could be avoided providing a certain indication about the presence or not of the case reported in the available denominators for foreigners [29,43,44,45]. In most cases it would be sufficient to include a variable on the resident status of the foreigner (i.e., if he/she is formally resident in the host country or not, without any further assessment of regular or irregular state). This would allow to calculate unbiased rates and to make comparisons between different groups of immigrants or with the native population.
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Riccardo, F.; Dente, M.G.; Kärki, T.; Fabiani, M.; Napoli, C.; Chiarenza, A.; Giorgi Rossi, P.; Munoz, C.V.; Noori, T.; Declich, S. Towards a European Framework to Monitor Infectious Diseases among Migrant Populations: Design and Applicability. Int. J. Environ. Res. Public Health 2015, 12, 11640–11661. [Google Scholar] [CrossRef] [PubMed]
- International Organization for Migration. Global Migration Trends: An Overview. 2014. Available online: http://missingmigrants.iom.int/sites/default/files/documents/Global_Migration_Trends_PDF_FinalVH_with%20References.pdf (accessed on 7 October 2016).
- European Centre for Disease Prevention and Control. Assessing the Burden of Key Infectious Diseases Affecting Migrant Populations in the EU/EEA; ECDC: Stockholm, Sweden, 2014; Available online: http://ecdc.europa.eu/en/publications/Publications/assessing-burden-disease-migrant-populations.pdf (accessed on 7 October 2016).
- EC Legal Framework for Communicable Disease Surveillance. Available online: http://ecdc.europa.eu/en/activities/surveillance/Pages/legal_framework.aspx (accessed on 7 October 2016).
- Decision No 2119/98/EC of the European Parliament and of the Council of 24 September 1998 Setting up a Network for the Epidemiological Surveillance and Control of Communicable Diseases in the Community Official Journal L 268, 03/10/1998 P. 0001–0007. Available online: http://eur-lex.europa.eu/legal-content/EN/ALL/?uri=CELEX:31998D2119 (accessed on 7 October 2016).
- Decision No 1082/2013/EU of the European Parliament and of the council of 22 October 2013 on Serious Cross-Border Threats to Health Official Journal of the European Union L.293. Available online: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2013:293:0001:0015:EN:PDF (accessed on 7 October 2016).
- Catchpole, M.; Coulombier, D. Refugee crisis demands European Union-wide surveillance! Euro Surveill. 2015, 20. [Google Scholar] [CrossRef] [PubMed]
- Riccardo, F.; Giorgi Rossi, P.; Chiarenza, A.; Noori, T.; Declich, S. Letter to the editor: Responding to a call for action—Where are we now? Euro Surveill. 2015, 20. [Google Scholar] [CrossRef] [PubMed]
- Riccardo, F.; Napoli, C.; Bella, A.; Rizzo, C.; Rota, M.C.; Dente, M.G.; De Santis, S.; Declich, S. Syndromic surveillance of epidemic-prone diseases in response to an influx of migrants from North Africa to Italy, May to October 2011. Euro Surveill. 2011, 16, 2–6. [Google Scholar]
- Napoli, C.; Riccardo, F.; Declich, S.; Dente, M.G.; Pompa, M.G.; Rizzo, C.; Rota, M.C.; Bella, A.; National Working Group. An early warning system based on Syndromic surveillance to detect potential health emergencies among migrants: Results of a two-year experience in Italy. Int. J. Environ. Res. Public Health 2014, 11, 8529–8541. [Google Scholar] [CrossRef] [PubMed]
- Riccardo, F.; Dente, M.G.; Kojouharova, M.; Fabiani, M.; Alfonsi, V.; Kurchatova, A.; Vladimirova, N.; Declich, S. Migrant’s access to immunization in Mediterranean Countries. Health Policy 2012, 105, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Kärki, T.; Napoli, C.; Riccardo, F.; Fabiani, M.; Dente, M.G.; Carballo, M.; Noori, T.; Declich, S. Screening for infectious diseases among newly arrived migrants in EU/EEA countries—Varying practices but consensus on the utility of screening. Int. J. Environ. Res. Public Health 2014, 11, 11004–11014. [Google Scholar] [CrossRef] [PubMed]
- Napoli, C.; Dente, M.G.; Kärki, T.; Riccardo, F.; Rossi, P.; Declich, S.; Network for the Control of Cross-Border Health Threats in the Mediterranean Basin and Black Sea. Screening for Infectious Diseases among Newly Arrived Migrants: Experiences and Practices in Non-EU Countries of the Mediterranean Basin and Black Sea. Int. J. Environ. Res. Public Health 2015, 12, 15550–15558. [Google Scholar] [CrossRef] [PubMed]
- Greenaway, C.; Sandoe, A.; Vissandjee, B.; Kitai, I.; Gruner, D.; Wobeser, W.; Pottie, K.; Ueffing, E.; Menzies, D.; Schwartzman, K. Canadian Collaboration for Immigrant and Refugee Health. Tuberculosis: Evidence review for newly arriving immigrants and refugees. CMAJ 2011, 183, E939–E951. [Google Scholar] [CrossRef] [PubMed]
- Pareek, M.; Watson, J.P.; Ormerod, L.P.; Kon, O.M.; Woltmann, G.; White, P.J.; Abubakar, I.; Lalvani, A. Screening of immigrants in the UK for imported latent tuberculosis: A multicentre cohort study and cost-effectiveness analysis. Lancet Infect. Dis. 2011, 11, 435–444. [Google Scholar] [CrossRef]
- Pareek, M.; Baussano, I.; Abubakar, I.; Dye, C.; Lalvani, A. Evaluation of immigrant tuberculosis screening in industrialized countries. Emerg. Infect. Dis. 2012, 18, 1422–1429. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.E.; Gushulak, B. Screening and treatment of immigrants and refugees to Canada for tuberculosis: Implications of the experience of Canada and other industrialized countries. Can. J. Infect. Dis. 1995, 6, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol 2005, 8, 19–32. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Migrant health: Background Note to the ECDC Report on Migration and Infectious Diseases in the EU; ECDC: Stockholm, Sweden, 2009; Available online: http://ecdc.europa.eu/en/publications/Publications/0907_TER_Migrant_health_Background_note.pdf (accessed on 7 October 2016).
- European Centre for Disease Prevention and Control. Migrant Health: Access to HIV Prevention, Treatment and Care for Migrant Populations in EU/EEA Countries; ECDC: Stockholm, Sweden, 2009; Available online: http://ecdc.europa.eu/en/publications/Publications/0907_TER_Migrant_health_HIV_Access_to_treatment.pdf (accessed on 7 October 2016).
- European Centre for Disease Prevention and Control. Migrant Health: HIV Testing and Counselling in Migrant Populations and Ethnic Minorities in EU/EEA/EFTA Member States; ECDC: Stockholm, Sweden, 2011; Available online: http://ecdc.europa.eu/en/publications/Publications/1108_TER_HIV_in_migrants.pdf (accessed on 7 October 2016).
- European Centre for Disease Prevention and Control. Improving HIV Data Comparability in Migrant Populations and Ethnic Minorities in EU/EEA/EFTA Countries: Findings from A Literature Review and Expert Panel; ECDC: Stockholm, Sweden, 2011; Available online: http://ecdc.europa.eu/en/publications/Publications/1108_TER_Improving_HIV_data_comparability_in_migrants.pdf (accessed on 7 October 2016).
- European Centre for Disease Prevention and Control. Migrant Health: Infectious Diseases of Specific Relevance to Newly-Arrived Migrants in the EU/EEA; ECDC: Stockholm, Sweden, 2015; Available online: http://ecdc.europa.eu/en/publications/Publications/Infectious-diseases-of-specific-relevance-to-newly-arrived-migrants-in-EU-EEA.pdf (accessed on 7 October 2016).
- European Centre for Disease Prevention and Control. Migrant Health: Rapid Risk Assessment: Communicable Disease Risks Associated with the Movement of Refugees in Europe during the Winter Season; ECDC: Stockholm, Sweden, 2015; Available online: http://ecdc.europa.eu/en/publications/Publications/refugee-migrant-health-in-european-winter-rapid-risk-assessment.pdf (accessed on 7 October 2016).
- European Centre for Disease Prevention and Control. Migrant Health: Expert Opinion on the Public Health Needs of Irregular Migrants, Refugees or Asylum Seekers across the EU's Southern and Aouth-Eastern Borders; ECDC: Stockholm, Sweden, 2015; Available online: http://ecdc.europa.eu/en/publications/Publications/Expert-opinion-irregular-migrants-public-health-needs-Sept-2015.pdf (accessed on 7 October 2016).
- IOM Glossary on migration. 2004. Available online: http://www.iomvienna.at/sites/default/files/IML_1_EN.pdf (accessed on 7 October 2016).
- Melosini, L.; Vetrano, U.; Dente, F.L.; Cristofano, M.; Giraldi, M.; Gabbrielli, L.; Novelli, F.; Aquilini, F.; Rindi, L.; Menichetti, F.; et al. Evaluation of underreporting tuberculosis in Central Italy by means of record linkage. BMC Public Health 2012, 12, 472. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, S.; Stormon, M.O.; Day, A.S.; Webber, M.T.; Ward, K.A.; O’Loughlin, E.V. Chronic hepatitis B and C infection in children in New South Wales. Med. J. Aust. 2009, 190, 670–673. [Google Scholar] [PubMed]
- Farchi, S.; Mantovani, J.; Borgia, P.; Giorgi, R.P. Tuberculosis incidence, hospitalisation prevalence and mortality in Lazio, Italy, 1997–2003. Int. J. Tuberc. Lung Dis. 2008, 12, 193–198. [Google Scholar] [PubMed]
- Giorgi Rossi, P.; Mantovani, J.; Ferroni, E.; Forcina, A.; Stanghellini, E.; Curtale, F.; Borgia, P. Incidence of bacterial meningitis (2001–2005) in Lazio, Italy: The results of a integrated surveillance system. BMC Infect. Dis. 2009, 9, 13. [Google Scholar] [CrossRef] [PubMed]
- Jelastopulu, E.; Alexopoulos, E.C.; Venieri, D.; Tsiros, G.; Komninou, G.; Constantinidis, T.C.; Chrysanthopoulos, K. Substantial underreporting of tuberculosis in West Greece: Implications for local and national surveillance. Euro Surveill. 2009, 14. [Google Scholar]
- Cohen, C.; Evans, A.A.; London, W.T.; Block, J.; Conti, M.; Block, T. Underestimation of chronic hepatitis B virus infection in the United States of America. J. Viral Hepat. 2008, 15, 12–13. [Google Scholar] [CrossRef] [PubMed]
- Wohl, A.R.; Lu, S.; Turner, J.; Kovacs, A.; Witt, M.; Squires, K.; Towner, W.; Beer, V. Risk of opportunistic infection in the HAART era among HIV-infected Latinos born in the United States compared to Latinos born in Mexico and Central America. AIDS Patient Care STDS 2003, 17, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Somerville, R.L.; Grant, C.C.; Grimwood, K.; Murdoch, D.; Graham, D.; Jackson, P.; Meates-Dennis, M.; Nicholson, R.; Purvis, D. Infants hospitalised with pertussis: Estimating the true disease burden. J. Paediatr. Child Health 2007, 43, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Ashrani, A.A.; Key, N.S.; Soucie, J.M.; Duffy, N.; Forsyth, A.; Geraghty, S. Universal Data Collection Project Investigators. Septic arthritis in males with haemophilia. Haemophilia 2008, 14, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Le Vu, S.; Le Strat, Y.; Barin, F.; Pillonel, J.; Cazein, F.; Bousquet, V.; Brunet, S.; Thierry, D.; Semaille, C.; Meyer, L.; et al. Population-based HIV-1 incidence in France, 2003–2008: A modelling analysis. Lancet Infect. Dis. 2010, 10, 682–687. [Google Scholar] [CrossRef]
- Watkins, R.E.; Plant, A.J.; Sang, D.; O’Rourke, T.F.; Eltom, A.A.; Streeton, J.; Gushulak, B. The association between subjective and clinical indicators of health in prospective Vietnamese migrants. Asia Pac. J. Public Health 2005, 17, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Porta, D.; Perucci, C.A.; Forastiere, F.; De Luca, A. Lazio HIV Surveillance Collaborative Group. Temporal trend of HIV infection: An update of the HIV surveillance system in Lazio, Italy, 1985–2000. Eur. J. Public Health 2004, 14, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Winston, C.A.; Menzies, H.J. Pediatric and adolescent tuberculosis in the United States, 2008–2010. Pediatrics 2012, 130, e1425–e1432. [Google Scholar] [CrossRef] [PubMed]
- Rose, A.M.; Sinka, K.; Watson, J.M.; Mortimer, J.Y.; Charlett, A. An estimate of the contribution of HIV infection to the recent rise in tuberculosis in England and Wales. Thorax 2002, 57, 442–445. [Google Scholar] [CrossRef] [PubMed]
- Marschall, T.; Kretzschmar, M.; Mangen, M.J.; Schalm, S. High impact of migration on the prevalence of chronic hepatitis B in The Netherlands. Eur. J. Gastroenterol. Hepatol. 2008, 20, 1214–1225. [Google Scholar] [CrossRef] [PubMed]
- Baussano, I.; Bugiani, M.; Gregori, D.; van Hest, R.; Borraccino, A.; Raso, R.; Merletti, F. Undetected burden of tuberculosis in a low-prevalence area. Int. J. Tuberc. Lung Dis. 2006, 10, 415–421. [Google Scholar] [PubMed]
- Odone, A.; Riccò, M.; Morandi, M.; Borrini, B.M.; Pasquarella, C.; Signorelli, C. Epidemiology of tuberculosis in a low-incidence Italian region with high immigration rates: Differences between not Italy-born and Italy-born TB cases. BMC Public Health 2011, 11, 376. [Google Scholar] [CrossRef] [PubMed]
- Das, D.; Baker, M.; Calder, L. Tuberculosis epidemiology in New Zealand: 1995–2004. N. Z. Med. J. 2006, 119, U2249. [Google Scholar] [PubMed]
- Marc, L.G.; Patel-Larson, A.; Hall, H.I.; Hughes, D.; Alegría, M.; Jeanty, G.; Eveillard, Y.S.; Jean-Louis, E. National Haitian-American Health Alliance. HIV among Haitian-born persons in the United States, 1985–2007. AIDS 2010, 24, 2089–2097. [Google Scholar] [CrossRef] [PubMed]
- Arshad, S.; Bavan, L.; Gajari, K.; Paget, S.N.; Baussano, I. Active screening at entry for tuberculosis among new immigrants: A systematic review and meta-analysis. Eur. Respir. J. 2010, 35, 1336–1345. [Google Scholar] [CrossRef] [PubMed]
- Pace-Asciak, A.; Mamo, J.; Calleja, N. Tuberculosis among undocumented boat migrants to Malta: Implications for a migrant tuberculosis policy. Int. J. Tuberc. Lung Dis. 2013, 17, 1065–1070. [Google Scholar] [CrossRef] [PubMed]
- Verver, S.; van Soolingen, D.; Borgdorff, M.W. Effect of screening of immigrants on tuberculosis transmission. Int. J. Tuberc. Lung Dis. 2002, 6, 121–129. [Google Scholar] [PubMed]
- Erkens, C.; Slump, E.; Kamphorst, M.; Keizer, S.; van Gerven, P.J.; Bwire, R.; Berkel, M.; Borgdorff, M.W.; Verver, S. Coverage and yield of entry and follow-up screening for tuberculosis among new immigrants. Eur. Respir. J. 2008, 32, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Fernández Sanfrancisco, M.T.; Díaz Portillo, J.; Sánchez Romero, J.M.; Pérez Fernández, A.; Vadillo Andrade, J. Prevalence of tuberculosis among the immigrant population in Ceuta, Spain. Rev. Esp. Salud Publica 2001, 75, 551–558. [Google Scholar] [PubMed]
- Pareek, M.; Abubakar, I.; White, P.J.; Garnette, G.P.; Lalvani, A. Tuberculosis screening of migrants to low-burden nations: Insights from evaluation of UK practice. Eur. Respir. J. 2011, 37, 1175–1182. [Google Scholar] [CrossRef] [PubMed]
- Kruijshaar, M.E.; Abubakar, I.; Stagg, H.R.; Pedrazzoli, D.; Lipman, M. Migration and tuberculosis in the UK: Targeting screening for latent infection to those at greatest risk of disease. Thorax 2013, 68, 1172–1174. [Google Scholar] [CrossRef] [PubMed]
- Diel, R.; Rüsch-Gerdes, S.; Niemann, S. Molecular epidemiology of tuberculosis among immigrants in Hamburg, Germany. J. Clin. Microbiol. 2004, 42, 2952–2960. [Google Scholar] [CrossRef] [PubMed]
| Issue | Main Findings | Type of Evidence | References |
|---|---|---|---|
| Misreporting | |||
| Decrease under-reporting | TB and meningitis are more often reported in migrants | Certain and quantified | [27,29,30,42] |
| Improvement in TB surveillance was stronger for immigrants | Certain and quantified | [29] | |
| Increase under-reporting | Illegal immigrant could be under-diagnosed for TB | Possible | [31] |
| Lower response in surveys could under represent immigrants | Certain not quantified | [32,41] | |
| Language barriers decrease probability of syndromic diagnoses | Possible | [33] | |
| Under-diagnosis in minorities | Possible | [40] | |
| Under-diagnosis in minorities | Certain not quantified | [34] | |
| Other effects | Biases in systemic infection diagnosis | Possible | [35] |
| Biases in reporting information | Possible | [36,37] | |
| Inaccuracy about the route of infection for TB and HIV | Certain not quantified | [38,39] | |
| Denominator | Under-estimation of the real at-risk population for immigrants | Certain not quantified | [29,43] |
| People included in the numerator are not always part of the denominator | Certain not quantified | [29,43,44,45] | |
| Screening | Screening increases the probability of diagnosis | Certain and quantified | [28,46,47,48,49,51] |
| Misreporting of prevalent cases as incident | Possible | [50] | |
| Screening modalities and implementation impact on detection | Certain and quantified | [51] | |
| Screening could leave less cases to be detected in the routine surveillance | Possible | [52] | |
| Screen-detected cases are less often first cases of a cluster | Certain and quantified | [48] | |
| Small effect on overall incidence | Certain not quantified | [53] |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giorgi Rossi, P.; Riccardo, F.; Pezzarossi, A.; Ballotari, P.; Dente, M.G.; Napoli, C.; Chiarenza, A.; Velasco Munoz, C.; Noori, T.; Declich, S. Factors Influencing the Accuracy of Infectious Disease Reporting in Migrants: A Scoping Review. Int. J. Environ. Res. Public Health 2017, 14, 720. https://doi.org/10.3390/ijerph14070720
Giorgi Rossi P, Riccardo F, Pezzarossi A, Ballotari P, Dente MG, Napoli C, Chiarenza A, Velasco Munoz C, Noori T, Declich S. Factors Influencing the Accuracy of Infectious Disease Reporting in Migrants: A Scoping Review. International Journal of Environmental Research and Public Health. 2017; 14(7):720. https://doi.org/10.3390/ijerph14070720
Chicago/Turabian StyleGiorgi Rossi, Paolo, Flavia Riccardo, Annamaria Pezzarossi, Paola Ballotari, Maria Grazia Dente, Christian Napoli, Antonio Chiarenza, Cesar Velasco Munoz, Teymur Noori, and Silvia Declich. 2017. "Factors Influencing the Accuracy of Infectious Disease Reporting in Migrants: A Scoping Review" International Journal of Environmental Research and Public Health 14, no. 7: 720. https://doi.org/10.3390/ijerph14070720







