Patterns Associated with Adult Mandibular Fractures in Southern Taiwan—A Cross-Sectional Retrospective Study
Abstract
:1. Background
2. Methods
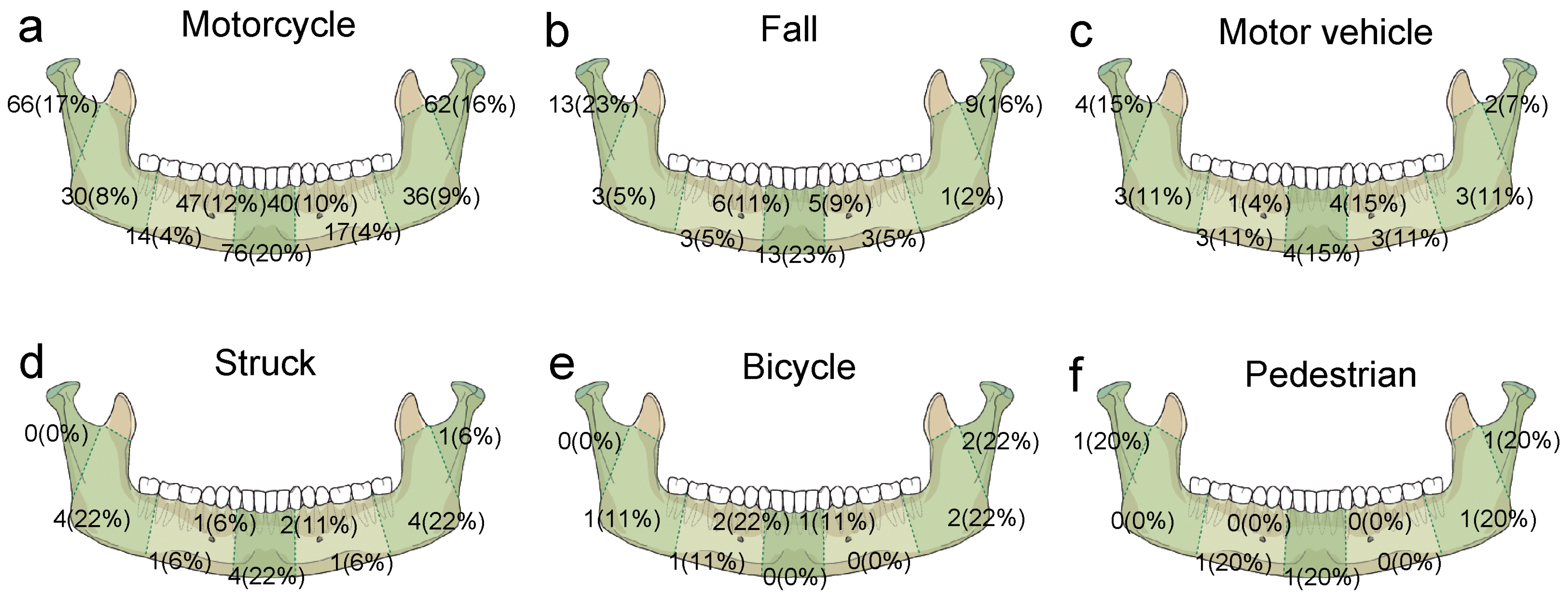
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Czerwinski, M.; Parker, W.; Chehade, A.; Williams, H. Identification of mandibular fracture epidemiology in Canada: Enhancing injury prevention and patient evaluation. Can. J. Plast. Surg. 2008, 16, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.S.; Chen, S.C.; Yang, Y.C.; Huang, L.C.; Guo, H.R.; Yang, H.Y. Epidemiology and patterns of facial fractures due to road traffic accidents in Taiwan: A 15-year retrospective study. Traffic Inj. Prev. 2017, 3, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Olson, R.A.; Fonseca, R.J.; Zeitler, D.L.; Osbon, D.B. Fractures of the mandible: A review of 580 cases. J. Oral Maxillofac. Surg. 1982, 40, 23–28. [Google Scholar] [CrossRef]
- Fridrich, K.L.; Pena-Velasco, G.; Olson, R.A. Changing trends with mandibular fractures: A review of 1067 cases. J. Oral Maxillofac. Surg. 1992, 50, 586–589. [Google Scholar] [CrossRef]
- King, R.E.; Scianna, J.M.; Petruzzelli, G.J. Mandible fracture patterns: A suburban trauma center experience. Am. J. Otolaryngol. 2004, 25, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Kommers, S.C.; Karagozoglu, K.H.; Gallesio, C.; Forouzanfar, T. Mandibular trauma: A two-centre study. Int. J. Oral Maxillofac. Surg. 2015, 44, 998–1004. [Google Scholar] [CrossRef] [PubMed]
- Lamphier, J.; Ziccardi, V.; Ruvo, A.; Janel, M. Complications of mandibular fractures in an urban teaching center. J. Oral Maxillofac. Surg. 2003, 61, 745–749. [Google Scholar] [CrossRef]
- Morris, C.; Bebeau, N.P.; Brockhoff, H.; Tandon, R.; Tiwana, P. Mandibular fractures: An analysis of the epidemiology and patterns of injury in 4143 fractures. J. Oral Maxillofac. Surg. 2015, 73, 951.e1–951.e12. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.H.; Hu, T.Q.; Liu, Q.; Ongodia, D.; Li, Z.B. Does trauma etiology affect the pattern of mandibular fracture? J. Craniofac. Surg. 2012, 23, e494–e497. [Google Scholar] [CrossRef] [PubMed]
- Ogundare, B.O.; Bonnick, A.; Bayley, N. Pattern of mandibular fractures in an urban major trauma center. J. Oral Maxillofac. Surg. 2003, 61, 713–718. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.; Lin, M.R.; Chu, S.F.; Tsai, S.H.; Bai, C.H.; Chiu, W.T. The effect of various types of motorcycle helmets on cervical spine injury in head injury patients: A multicenter study in Taiwan. BioMed Res. Int. 2015, 2015, 487985. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.L.; Lai, C.Y. Using travel socialization and underlying motivations to better understand motorcycle usage in Taiwan. Accid. Anal. Prev. 2015, 79, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.T.; Liang, C.C.; Rau, C.S.; Hsu, S.Y.; Hsieh, C.H. Alcohol-related hospitalizations of adult motorcycle riders. World J. Emerg. Surg. 2015, 10, 2. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.H.; Hsu, S.Y.; Hsieh, H.Y.; Chen, Y.C. Differences between the sexes in motorcycle-related injuries and fatalities at a Taiwanese level I trauma center. Biomed. J. 2017, 40, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.H.; Liu, H.T.; Hsu, S.Y.; Hsieh, H.Y.; Chen, Y.C. Motorcycle-related hospitalizations of the elderly. Biomed. J. 2017, 40, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Liang, C.C.; Liu, H.T.; Rau, C.S.; Hsu, S.Y.; Hsieh, H.Y.; Hsieh, C.H. Motorcycle-related hospitalization of adolescents in a Level I trauma center in Southern Taiwan: A cross-sectional study. BMC Pediatr. 2015, 15, 105. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.T.; Rau, C.S.; Wu, S.C.; Chen, Y.C.; Hsu, S.Y.; Hsieh, H.Y.; Hsieh, C.H. Obese motorcycle riders have a different injury pattern and longer hospital length of stay than the normal-weight patients. Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 50. [Google Scholar] [CrossRef] [PubMed]
- Pontes, H.A.R.; Pontes, F.S.C.; Lameira, A.G.; Salim, R.A.; de Carvalho, P.L.; Guimarães, D.M.; dos Santos Pinto, D. Report of four cases of ameloblastic fibro-odontoma in mandible and discussion of the literature about the treatment. J. Cranio-Maxillofac. Surg. 2012, 40, e59–e63. [Google Scholar] [CrossRef] [PubMed]
- Al Ahmed, H.E.; Jaber, M.A.; Abu Fanas, S.H.; Karas, M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: A review of 230 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 98, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Czerwinski, M.; Parker, W.L.; Williams, H.B. Algorithm for head computed tomography imaging in patients with mandible fractures. J. Oral Maxillofac. Surg. 2008, 66, 2093–2097. [Google Scholar] [CrossRef] [PubMed]
- Sobin, L.; Kopp, R.; Walsh, R.; Kellman, R.M.; Harris, T. Incidence of concussion in patients with isolated mandible fractures. JAMA Facial Plast. Surg. 2016, 18, 15–18. [Google Scholar] [CrossRef] [PubMed]
- Fischer, K.; Zhang, F.; Angel, M.F.; Lineaweaver, W.C. Injuries associated with mandible fractures sustained in motor vehicle collisions. Plast. Reconstr. Surg. 2001, 108, 328–331. [Google Scholar] [CrossRef] [PubMed]
- Salentijn, E.G.; Peerdeman, S.M.; Boffano, P.; van den Bergh, B.; Forouzanfar, T. A ten-year analysis of the traumatic maxillofacial and brain injury patient in Amsterdam: Incidence and aetiology. J. Cranio-Maxillofac. Surg. 2014, 42, 705–710. [Google Scholar] [CrossRef] [PubMed]
- Hooten, K.G.; Murad, G. Helmeted vs. nonhelmeted: A retrospective review of outcomes from 2-wheeled vehicle accidents at a level 1 trauma center. Clin. Neurosurg. 2012, 59, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.C.; Ivers, R.; Norton, R.; Boufous, S.; Blows, S.; Lo, S.K. Helmets for preventing injury in motorcycle riders. Cochrane Libr. 2008. [Google Scholar] [CrossRef]
- Muller, A. Florida’s motorcycle helmet law repeal and fatality rates. Am. J. Public Health 2004, 94, 556–558. [Google Scholar] [CrossRef] [PubMed]
- Vaca, F. National Highway Traffic Safety Administration (NHTSA) notes. Evaluation of the repeal of the all-rider motorcycle helmet law in Florida. Ann. Emerg. Med. 2006, 47. [Google Scholar] [CrossRef]
- Cavalcante, J.R.; Oka, S.C.; de Santana Santos, T.; Dourado, E.; de Oliveira, E.S.E.D.; Gomes, A.C. Influence of helmet use in facial trauma and moderate traumatic brain injury victims of motorcycle accidents. J. Craniofac. Surg. 2012, 23, 982–985. [Google Scholar] [CrossRef] [PubMed]
- Chuang, J.F.; Rau, C.S.; Kuo, P.J.; Chen, Y.C.; Hsu, S.Y.; Hsieh, H.Y.; Hsieh, C.H. Traumatic injuries among adult obese patients in Southern Taiwan: A cross-sectional study based on a trauma registry system. BMC Public Health 2016, 16, 275. [Google Scholar] [CrossRef] [PubMed]
| Variables | Patients N = 312 |
|---|---|
| Gender (%) | |
| Male | 207(66.3) |
| Female | 105(33.7) |
| Age | 36.5 ± 15.2 |
| Cause (%) | |
| Motorcycle accident | 238(76.3) |
| Fall | 34(10.9) |
| Motor vehicle accident (MVA) | 15(4.8) |
| Struck by/against objects | 14(4.5) |
| Bicycle accident | 7(2.2) |
| Pedestrian | 4(1.3) |
| GCS | 13.5 ± 3.1 |
| ≤8 (%) | 35(11.2) |
| 9–12 (%) | 23(7.4) |
| ≥13 (%) | 254(81.4) |
| Associated head injury (%) | |
| Cranial fracture | 36(11.5) |
| Epidural hematoma (EDH) | 18(5.8) |
| Subdural hematoma (SDH) | 32(10.3) |
| Subarachnoid hemorrhage (SAH) | 34(10.9) |
| Intracerebral hematoma (ICH) | 8(2.6) |
| Cerebral contusion | 14(4.5) |
| Cervical vertebral fracture | 4(1.3) |
| Site of mandibular fracture (%) | n = 503 |
| Symphysis | 98(19.5) |
| Parasymphysis | 109(21.7) |
| Body | 47(9.3) |
| Angle and Ramus | 88(17.5) |
| Condylar neck and Head | 161(32.0) |
| Variables | Fall n = 56 (II) | MVA n = 27 (III) | Struck by/against n = 18 (IV) | Bicycle n = 9 (V) | Pedestrian n = 5 (VI) | |||||
| Symphysis | 13(23.2) | 4(14.8) | 4(22.2) | 0(0.0) | 1(20.0) | |||||
| Parasymphysis | 11(19.6) | 5(18.5) | 3(16.7) | 3(33.3) | 0(0.0) | |||||
| Body | 6(10.7) | 6(22.2) | 2(11.1) | 1(11.1) | 1(20.0) | |||||
| Angle and Ramus | 4(7.1) | 6(22.2) | 8(44.4) | 3(33.3) | 1(20.0) | |||||
| Condylar neck and Head | 22(39.3) | 6(22.2) | 1(5.6) | 2(22.2) | 2(40.0) | |||||
| Variables | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p |
| II vs. I | III vs. I | IV vs. I | V vs. I | VI vs. I | ||||||
| Symphysis | 1.2(0.64–2.42) | 0.527 | 0.7(0.24–2.13) | 0.545 | 1.2(0.38–3.66) | 0.784 | - | 0.999 | 1.0(0.11–9.34) | 0.982 |
| Parasymphysis | 0.8(0.421.71) | 0.639 | 0.8(0.29–2.14) | 0.637 | 0.7(0.20–2.45) | 0.567 | 1.7(0.42–7.06) | 0.445 | - | 0.999 |
| Body | 1.4(0.55–3.48) | 0.492 | 3.3(1.24–8.76) | 0.017 | 1.4(0.32–6.55) | 0.637 | 1.4(0.17–11.89) | 0.735 | 2.9(0.31–26.56) | 0.351 |
| Angle and Ramus | 0.4(0.13–1.07) | 0.068 | 1.4(0.54–3.59) | 0.491 | 3.9(1.48–10.26) | 0.006 | 2.4(0.60–10.00) | 0.215 | 1.2(0.13–11.09) | 0.860 |
| Variables | Symphysis n = 76 | Parasymphysis n = 87 | Body n = 31 | Angle and Ramus n = 66 | Condyle and Head n = 128 | |||||
| Age | 32.2 ± 10.9 | 32.2 ± 12.2 | 39.0 ± 16.4 | 35.5 ± 17.1 | 33.6 ± 13.4 | |||||
| Gender (M/F) | 29/47 | 30/57 | 7/24 | 24/42 | 60/68 | |||||
| BMI classification | ||||||||||
| Obese | 4(5.3) | 8(9.2) | 0(0.0) | 3(4.5) | 5(3.9) | |||||
| Overweight | 16(21.1) | 19(21.8) | 9(29.0) | 14(21.2) | 22(17.2) | |||||
| Underweight | 7(9.2) | 5(5.7) | 2(6.5) | 3(4.5) | 11(8.6) | |||||
| Normal | 45(59.2) | 53(60.9) | 20(64.5) | 43(65.2) | 83(64.8) | |||||
| Unknown | 4(5.3) | 2(2.3) | 0(0.0) | 3(4.5) | 7(5.5) | |||||
| Helmet use | ||||||||||
| Yes | 58(76.3) | 71(81.6) | 29(93.5) | 50(75.8) | 112(87.5) | |||||
| No | 13(17.1) | 14(16.1) | 2(6.5) | 13(19.7) | 14(10.9) | |||||
| Unknown | 5(6.6) | 2(2.3) | 0(0.0) | 3(4.5) | 2(1.6) | |||||
| Variables | Symphysis | Parasymphysis | Body | Angle and Ramus | Condyle and Head | |||||
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | OR (95% CI) | p | OR (95% CI) | p | ||
| BMI classification | BMI classification | |||||||||
| Obese | 1.2(0.38–3.91) | 0.739 | 1.9(0.72–5.21) | 0.192 | - | Obese | 1.2(0.38–3.91) | 0.739 | 1.9(0.72–5.21) | 0.192 |
| Overweight | 1.3(0.65–2.51) | 0.486 | 1.2(0.66–2.31) | 0.502 | 1.0(0.41–2.35) | Overweight | 1.3(0.65–2.51) | 0.486 | 1.2(0.66–2.31) | 0.502 |
| Underweight | 1.5(0.56–4.05) | 0.418 | 1.0(0.34–2.70) | 0.933 | 1.3(0.28–6.38) | Underweight | 1.5(0.56–4.05) | 0.418 | 1.0(0.34–2.70) | 0.933 |
| Helmet use | Helmet use | |||||||||
| Yes | 0.6(0.29–1.22) | 0.158 | 0.9(0.45–1.84) | 0.803 | 3.9(0.87–17.26) | Yes | 0.6(0.29–1.22) | 0.158 | 0.9(0.45–1.84) | 0.803 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, K.-C.; Peng, S.-H.; Kuo, P.-J.; Chen, Y.-C.; Rau, C.-S.; Hsieh, C.-H. Patterns Associated with Adult Mandibular Fractures in Southern Taiwan—A Cross-Sectional Retrospective Study. Int. J. Environ. Res. Public Health 2017, 14, 821. https://doi.org/10.3390/ijerph14070821
Lin K-C, Peng S-H, Kuo P-J, Chen Y-C, Rau C-S, Hsieh C-H. Patterns Associated with Adult Mandibular Fractures in Southern Taiwan—A Cross-Sectional Retrospective Study. International Journal of Environmental Research and Public Health. 2017; 14(7):821. https://doi.org/10.3390/ijerph14070821
Chicago/Turabian StyleLin, Ko-Chien, Shu-Hui Peng, Pao-Jen Kuo, Yi-Chun Chen, Cheng-Shyuan Rau, and Ching-Hua Hsieh. 2017. "Patterns Associated with Adult Mandibular Fractures in Southern Taiwan—A Cross-Sectional Retrospective Study" International Journal of Environmental Research and Public Health 14, no. 7: 821. https://doi.org/10.3390/ijerph14070821






