Smoke-Free Recovery from Trauma Surgery: A Pilot Trial of an Online Smoking Cessation Program for Orthopaedic Trauma Patients
Abstract
:1. Introduction
2. Methods
3. Analysis
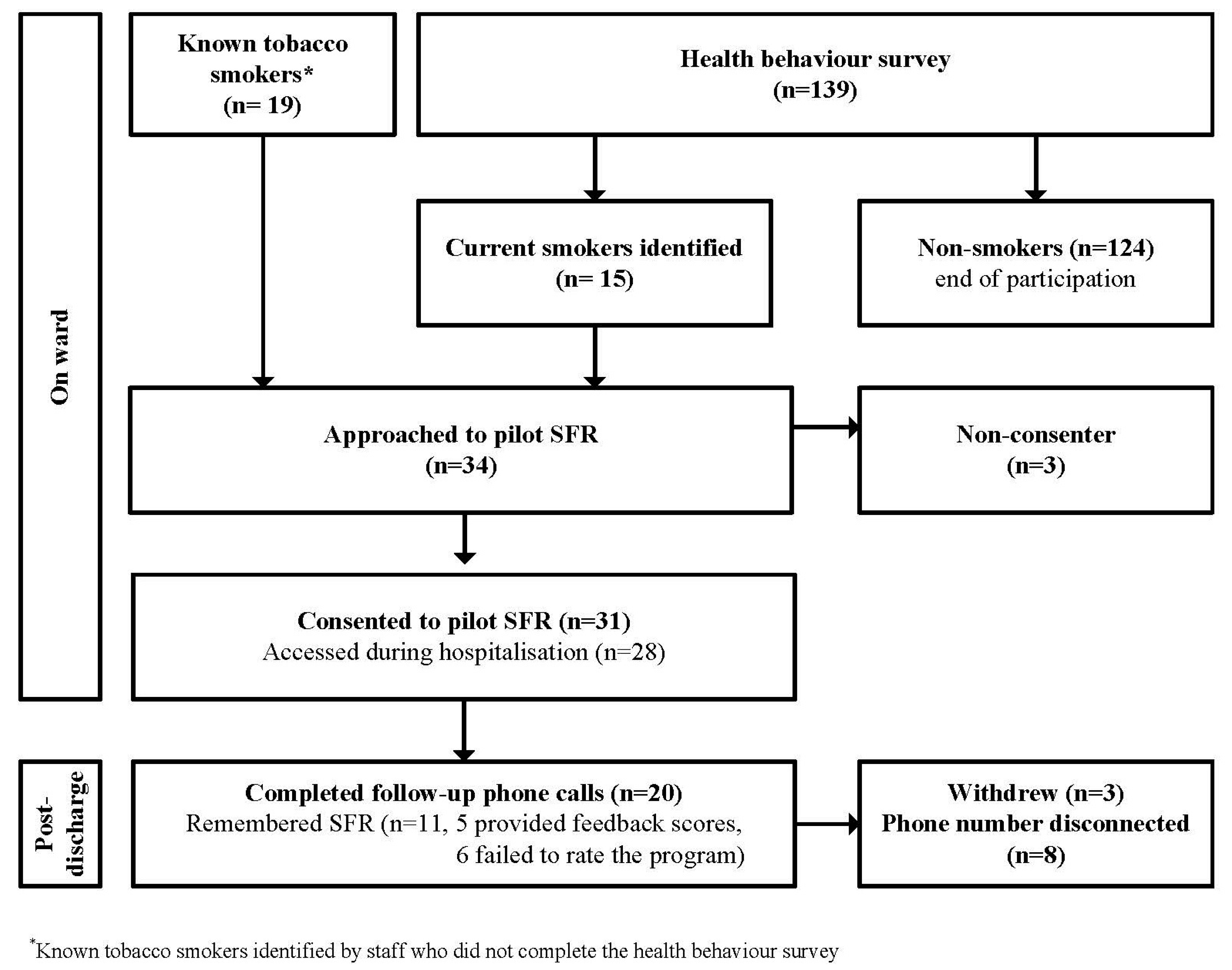
4. Results
5. Discussion
6. Implications for Current Practice
7. Limitations
8. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Australian Institute of Health and Welfare. National Drug Strategy Household Survey Report; Australian Institute of Health and Welfare: Canberra, Australia, 2011.
- National Preventative Health Taskforce. Australia: The Healthiest Country by 2020. National Preventative Health Strategy the Roadmap for Action. Available online: http://www.health.gov.au/internet/preventativehealth/publishing.nsf/Content/nphs-roadmap-toc (accessed on 13 June 2017).
- Sørensen, L.T. Wound healing and infection in surgery: The pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: A systematic review. Ann. Surg. 2012, 255, 1069–1079. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, L.T. Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: A systematic review and meta-analysis. Arch. Surg. 2012, 147, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Ahn, C.; Mulligan, P.; Salcido, R.S. Smoking-the bane of wound healing: Biomedical interventions and social influences. Adv. Skin Wound Care 2008, 21, 227–236. [Google Scholar] [CrossRef]
- Kanneganti, P.; Harris, J.D.; Brophy, R.H.; Carey, J.L.; Lattermann, C.; Flanigan, D.C. The effect of smoking on ligament and cartilage surgery in the knee: A systematic review. Am. J. Sports Med. 2012, 40, 2872–2878. [Google Scholar] [CrossRef] [PubMed]
- Castillo, R.C.; Bosse, M.J.; MacKenzie, E.J.; Patterson, B.M.; Group, L.S. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J. Orthop. Trauma 2005, 19, 151–157. [Google Scholar] [CrossRef]
- Baumgarten, K.M.; Gerlach, D.; Galatz, L.M.; Teefey, S.A.; Middleton, W.D.; Ditsios, K.; Yamaguchi, K. Cigarette smoking increases the risk for rotator cuff tears. Clin. Orthop. Relat. Res. 2010, 468, 1534–1541. [Google Scholar] [CrossRef]
- Moller, A.M.; Pedersen, T.; Villebro, N.; Munksgaard, A. Effect of smoking on early complications after elective orthopaedic surgery. J. Bone Jt. Surg. 2003, 85, 178–181. [Google Scholar] [CrossRef]
- Neptune, D.; Bonevski, B.; Enninghorst, N.; Balogh, Z.J. The prevalence of smoking and interest in quitting among surgical patients with acute extremity fractures. Drug Alcohol Rev. 2014, 33, 548–554. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. National Health Survey: First Results, 2014–2015. Available online: http://www.abs.gov.au/ausstats/[email protected]/Lookup/by%20Subject/4364.0.55.001~2014-15~Main%20Features~About%20the%20National%20Health%20Survey~3 (accessed on 13 June 2017).
- World Health Organization. Assessment of the Economic Costs of Smoking; WHO Press: Geneva, Switzerland, 2011. [Google Scholar]
- France, E.K.; Glasgow, R.E.; Marcus, A.C. Smoking cessation interventions among hospitalized patients: What have we learned? Prev. Med. 2001, 32, 376–388. [Google Scholar] [CrossRef]
- Baratiny, G.; Campbell, E.; Sanson-Fisher, R.; Cockburn, J. Hospital patients receptive to quit smoking advice. Health Promot. J. Aust. 2003, 14, 69. [Google Scholar]
- Rigotti, N.A.; Clair, C.; Munafò, M.R.; Stead, L.F. Interventions for smoking cessation in hospitalised patients (review). Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef]
- Rigotti, N.; Munafo, M.; Stead, L. Interventions for smoking cessation in hospitalised patients. Cochrane Database Syst. Rev. 2007, 3. [Google Scholar] [CrossRef]
- Shi, L.; Iguchi, M.Y. “Risk homeostasis” or “teachable moment”? The interaction between smoking behavior and lung cancer screening in the mayo lung project. Tob. Induc. Dis. 2011, 9, 2. [Google Scholar] [CrossRef] [PubMed]
- Lawson, P.J.; Flocke, S.A. Teachable moments for health behavior change: A concept analysis. Patient Educ. Couns. 2009, 76, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Fiore, M. Treating Tobacco Use and Dependence: 2008 Update: Clinical Practice Guideline; DIANE Publishing: Rockville, MD, USA, 2008. [Google Scholar]
- New South Wales Health Department. Guide for the Management of Nicotine Dependent Inpatients; State Government of New South Wales: Sydney, Australia, 2002.
- Freund, M.; Campbell, E.; Paul, C.; McElduff, P.; Walsh, R.A.; Sakrouge, R.; Wiggers, J.; Knight, J. Smoking care provision in hospitals: A review of prevalence. Nicotine Tob. Res. 2008, 10, 757–774. [Google Scholar] [CrossRef] [PubMed]
- Balanda, K.P.; Lowe, J.B.; Stanton, W.; Gillespie, A.; Conway, V. Cancer control activities in Australian public hospitals. Int. Q. Community Health Educ. 1994, 15, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Slattery, C.; Freund, M.; Gillham, K.; Knight, J.; Wolfenden, L.; Bisquera, A.; Wiggers, J. Increasing smoking cessation care across a network of hospitals: An implementation study. Implement. Sci. 2015, 11, 28. [Google Scholar] [CrossRef] [PubMed]
- Wolfenden, L.; Wiggers, J.; Campbell, E.; Knight, J.; Kerridge, R.; Spigelman, A. Providing comprehensive smoking cessation care to surgical patients: The case for computers. Drug Alcohol Rev. 2009, 28, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control. Use of cessation methods among smokers aged 16–24 years—United States, 2003. Morb. Mortal. Wkly. Rep. 2006, 55, 1351. [Google Scholar]
- Michie, S.; Wood, C.E.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W. Behaviour change techniques: The development and evaluation of a taxonomic method for reporting and describing behaviour change interventions (a suite of five studies involving consensus methods, randomised controlled trials and analysis of qualitative data). Health Technol. Assess. 2015, 19, 1–188. [Google Scholar] [PubMed]
- Monnier, J.; Laken, M.; Carter, C.L. Patient and caregiver interest in internet-based cancer services. Cancer Pract. 2002, 10, 305–310. [Google Scholar] [PubMed]
- Burkow, T.M.; Vognild, L.K.; Østengen, G.; Johnsen, E.; Risberg, M.J.; Bratvold, A.; Hagen, T.; Brattvoll, M.; Krogstad, T.; Hjalmarsen, A. Internet-enabled pulmonary rehabilitation and diabetes education in group settings at home: A preliminary study of patient acceptability. BMC Med. Inform. Decis. Mak. 2013, 13, 33. [Google Scholar]
- Myung, S.-K.; McDonnell, D.D.; Kazinets, G.; Seo, H.G.; Moskowitz, J.M. Effects of web-and computer-based smoking cessation programs: Meta-analysis of randomized controlled trials. Arch. Intern. Med. 2009, 169, 929–937. [Google Scholar] [PubMed]
- Shahab, L.; McEwen, A. Online support for smoking cessation: A systematic review of the literature. Addiction 2009, 104, 1792–1804. [Google Scholar] [CrossRef] [PubMed]
- An, L.C.; Betzner, A.; Schillo, B.; Luxenberg, M.G.; Christenson, M.; Wendling, A.; Saul, J.E.; Kavanaugh, A. The comparative effectiveness of clinic, work-site, phone, and web-based tobacco treatment programs. Nicotine Tob. Res. 2010, 12, 989–996. [Google Scholar] [PubMed]
- Li, I.C.; Lee, S.Y.D.; Chen, C.Y.; Jeng, Y.Q.; Chen, Y.C. Facilitators and barriers to effective smoking cessation: Counselling services for inpatients from nurse-counsellors’ perspectives—A qualitative study. Int. J. Environ. Res. Public Health 2014, 11, 4782–4798. [Google Scholar] [CrossRef] [PubMed]
- Helgason, A.R.; Lund, K.E. General practitioners’ perceived barriers to smoking cessation-results from four Nordic countries. Scand. J. Public Health 2002, 30, 141–147. [Google Scholar] [PubMed]
- Twardella, D.; Brenner, H. Lack of training as a central barrier to the promotion of smoking cessation: A survey among general practitioners in Germany. Eur. J. Public Health 2005, 15, 140–145. [Google Scholar] [PubMed]
- Raupach, T.; Merker, J.; Hasenfuß, G.; Andreas, S.; Pipe, A. Knowledge gaps about smoking cessation in hospitalized patients and their doctors. Eur. J. Cardiovasc. Prev. Rehabil. 2011, 18, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Sarna, L.; Bialous, S.A.; Rice, V.H.; Wewers, M.E. Promoting tobacco dependence treatment in nursing education. Drug Alcohol Rev. 2009, 28, 507–516. [Google Scholar] [PubMed]
- Saito, A.; Nishina, M.; Murai, K.; Mizuno, A.; Ueshima, F.; Makiishi, T.; Ichinohe, T. Health professional’s perceptions of and potential barriers to smoking cessation care: A survey study at a dental school hospital in Japan. BMC Res. Notes 2010, 3, 329. [Google Scholar] [CrossRef] [PubMed]
- Freund, M.; Campbell, E.; Paul, C.; Sakrouge, R.; Wiggers, J. Smoking care provision in smoke-free hospitals in Australia. Prev. Med. 2005, 41, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Martínez, C.; Garcia, M.; Méndez, E.; Peris, M.; Fernández, E. Barriers and challenges for tobacco control in a smoke-free hospital. Cancer Nurs. 2008, 31, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Duffy, S.A.; Reeves, P.; Hermann, C.; Karvonen, C.; Smith, P. In-hospital smoking cessation programs: What do VA patients and staff want and need? Appl. Nurs. Res. 2008, 21, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Krempec, J.; Hall, J.; Biermann, J.S. Internet use by patients in orthopaedic surgery. Iowa Orthop. J. 2003, 23, 80. [Google Scholar] [PubMed]
- Fraval, A.; Ming Chong, Y.; Holcdorf, D.; Plunkett, V.; Tran, P. Internet use by orthopaedic outpatients-current trends and practices. Australas. Med. J. 2012, 5, 633–638. [Google Scholar] [CrossRef] [PubMed]
- McCrabb, S.; Balogh, Z.; Baker, A.L.; Harris, I.A.; Attia, J.; Lott, N.; Naylor, J.; Doran, C.; George, J.; Wolfenden, L.; et al. Development of an online smoking cessation program for use in hospital and following discharge: Smoke-free recovery. BMJ Innov. 2017. [Google Scholar] [CrossRef]
- Harrington, K.F.; Kim, Y.I.; Chen, M.; Ramachandran, R.; Pisu, M.; Sadasivam, R.S.; Houston, T.K.; Bailey, W.C. Web-based intervention for transitioning smokers from inpatient to outpatient care: An RCT. Am. J. Prev. Med. 2016, 51, 620–629. [Google Scholar] [CrossRef] [PubMed]
- Strecher, V.J.; Shiffman, S.; West, R. Randomized controlled trial of a web-based computer-tailored smoking cessation program as a supplement to nicotine patch therapy. Addiction 2005, 100, 682–688. [Google Scholar] [CrossRef] [PubMed]
- Smit, E.S.; Linn, A.J.; Weert, J. Taking online computer-tailoring forward: The potential of tailoring the message frame and delivery mode of online health behaviour change interventions. Eur. Health Psychol. 2015, 17, 25–31. [Google Scholar]
- Soetens, K.C.; Vandelanotte, C.; de Vries, H.; Mummery, K.W. Using online computer tailoring to promote physical activity: A randomized trial of text, video, and combined intervention delivery modes. J. Health Commun. 2014, 19, 1377–1392. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.O.; DiClemente, C.C. Toward a comprehensive model of change. In Treating Addictive Behaviors; Miller, W.R., Ed.; Plenum Press: New York, NY, USA, 1986. [Google Scholar]
- Braun, V.; Clarke, V.; Terry, G. Thematic analysis. In APA Handbook of Research Methods in Psychology, Vol. 2. Research Designs: Quantitative, Qualitative, Neuropsychological, and Biological; Cooper, H., Camic, P.M., Long, D.L., Panter, A.T., Rindskopf, D., Sher, K.J., Eds.; American Psychological Association: Washington, DC, USA, 2012; Volume 1, pp. 57–71. ISBN 978-1-4338-1003-9. [Google Scholar]
- Fereday, J.; Muir-Cochrane, E. Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. Int. J. Qual Methods 2006, 5, 80–92. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Zurek, A.A.; Orser, B.A. Understanding anesthesia-induced memory loss. In Essentials of Pharmacology for Anesthesia, Pain Medicine, and Critical Care; Springer: New York, NY, USA, 2015; pp. 847–858. [Google Scholar]
- Kelders, S.M.; Kok, R.N.; Ossebaard, H.C.; Van Gemert-Pijnen, J.E.W.C. Persuasive system design does matter: A systematic review of adherence to web-based interventions. J. Med. Internet Res. 2012, 14, e152. [Google Scholar] [CrossRef] [PubMed]
- Pike, K.J.; Rabius, V.; McAlister, A.; Geiger, A. American cancer society’s quitlink: Randomized trial of internet assistance. Nicotine Tob. Res. 2007, 9, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Wangberg, S.C.; Bergmo, T.S.; Johnsen, J. Adherence in internet-based interventions. Patient Prefer. Adherence 2008, 2, 57–65. [Google Scholar] [PubMed]
- Ludden, G.D.; van Rompay, T.J.; Kelders, S.M.; van Gemert-Pijnen, J.E. How to increase reach and adherence of web-based interventions: A design research viewpoint. J. Med. Internet Res. 2015, 17, e172. [Google Scholar] [CrossRef] [PubMed]
- Comello, M.L.G.; Qian, X.; Deal, A.M.; Ribisl, K.M.; Linnan, L.A.; Tate, D.F. Impact of game-inspired infographics on user engagement and information processing in an ehealth program. J. Med. Internet Res. 2016, 18, e237. [Google Scholar] [CrossRef] [PubMed]
- Schubart, J.R.; Stuckey, H.L.; Ganeshamoorthy, A.; Sciamanna, C.N. Chronic health conditions and internet behavioral interventions: A review of factors to enhance user engagement. Comput. Inform. Nurs. 2011, 29, 81–92. [Google Scholar] [CrossRef] [PubMed]
| Demographic Characteristics | n = 20 (%) |
|---|---|
| Gender | |
| Male | 14 (70%) |
| Female | 6 (30%) |
| Age mean (SD) | 47.9 (14.3) |
| Fractured type | |
| ankle/leg | 6 (30%) |
| Hand/wrist/elbow/arm | 4 (20%) |
| NOF */femur/pelvis | 6 (30%) |
| Multiple fractures | 4 (20%) |
| Insurance type | |
| No insurance | 15 (75%) |
| Private insurance | 5 (25%) |
| Indigenous status | |
| Non-indigenous | 19 (95%) |
| Indigenous | 1 (5%) |
| Country of Birth | |
| Australia | 17 (85%) |
| Other | 3 (15%) |
| Marital status | |
| Single | 10 (50%) |
| Married/defacto/Partner | 7 (35%) |
| Widowed/divorced/Seperated | 3 (15%) |
| Module | Number (%) | Total Minutes | Time per Participant Mean (SD) |
|---|---|---|---|
| Welcome | 28 (90%) | - * | - * |
| Recovery from surgery | 22 (71%) | 81 | 4 (5.6) |
| Thinking about quitting | 11 (36%) | 102 | 9.5 (8.1) |
| Quitting | 6 (19%) | 164 | 27.4 (24.7) |
| Staying quit | 6 (19%) | 21 | 3.4 (2.0) |
| Heading home | 5 (16%) | 49 | 9.8 (11.2) |
| Having trouble staying quit | 3 (10%) | 48 | 15.9 (9.5) |
| Games and quizzes | 6 (19%) | 44 | 7.5 (6.7) |
| Smoke-Free Diary | 3 (10%) | 80 | 26.9 (40.6) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
McCrabb, S.; Baker, A.L.; Attia, J.; Balogh, Z.J.; Lott, N.; Naylor, J.; Harris, I.A.; Doran, C.M.; George, J.; Wolfenden, L.; et al. Smoke-Free Recovery from Trauma Surgery: A Pilot Trial of an Online Smoking Cessation Program for Orthopaedic Trauma Patients. Int. J. Environ. Res. Public Health 2017, 14, 847. https://doi.org/10.3390/ijerph14080847
McCrabb S, Baker AL, Attia J, Balogh ZJ, Lott N, Naylor J, Harris IA, Doran CM, George J, Wolfenden L, et al. Smoke-Free Recovery from Trauma Surgery: A Pilot Trial of an Online Smoking Cessation Program for Orthopaedic Trauma Patients. International Journal of Environmental Research and Public Health. 2017; 14(8):847. https://doi.org/10.3390/ijerph14080847
Chicago/Turabian StyleMcCrabb, Sam, Amanda L. Baker, John Attia, Zsolt J. Balogh, Natalie Lott, Justine Naylor, Ian A. Harris, Christopher M. Doran, Johnson George, Luke Wolfenden, and et al. 2017. "Smoke-Free Recovery from Trauma Surgery: A Pilot Trial of an Online Smoking Cessation Program for Orthopaedic Trauma Patients" International Journal of Environmental Research and Public Health 14, no. 8: 847. https://doi.org/10.3390/ijerph14080847





