Stunting, Wasting and Underweight in Sub-Saharan Africa: A Systematic Review
Abstract
:1. Introduction
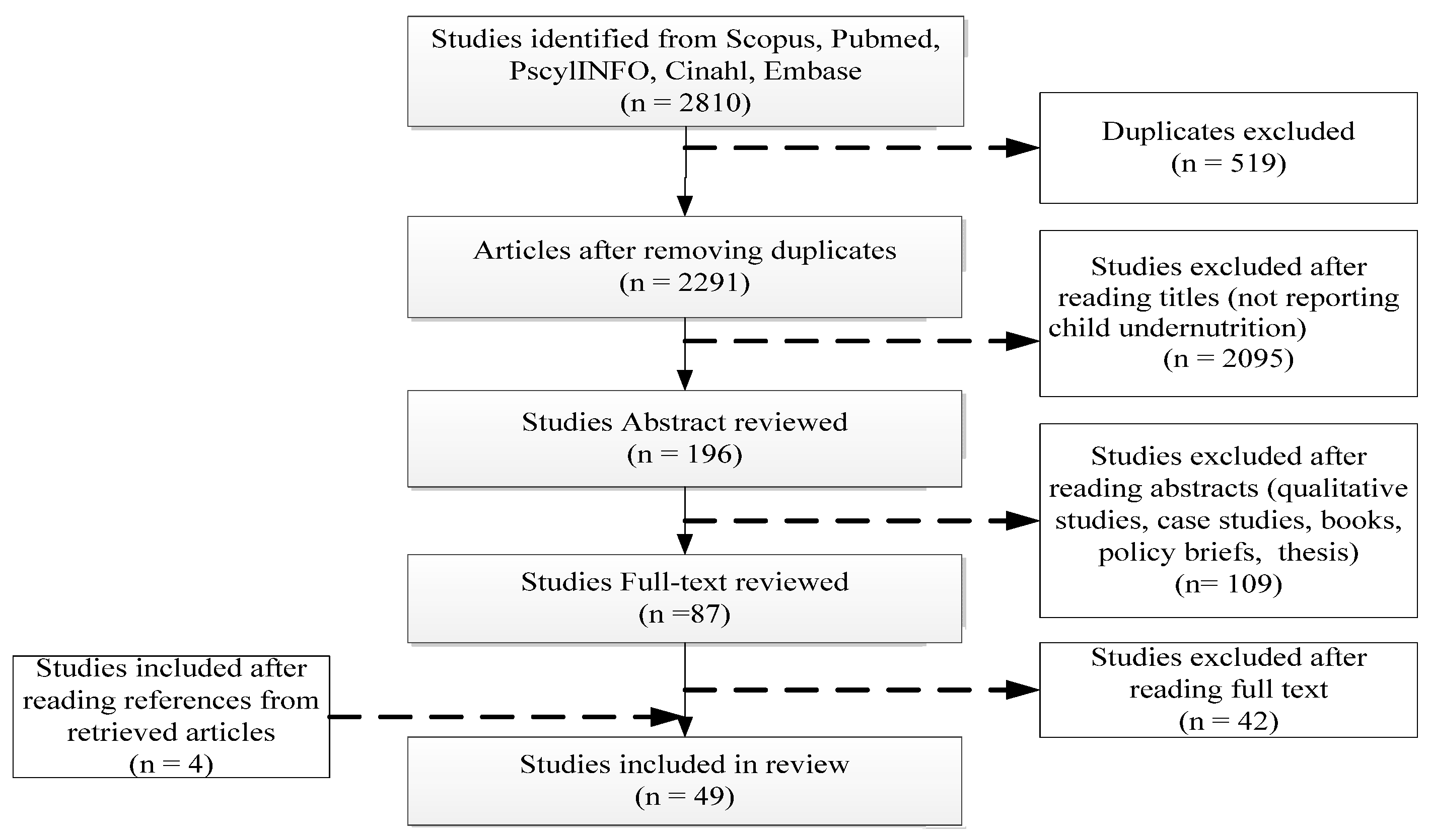
2. Methods
2.1. Anthropometric Indicators
2.2. Search Strategy
- (Malnutr* OR malnourish* OR undernourish* OR undernutr* OR stunt* OR wast* OR underweight*)
- (Child* or under-five* or preschool* or paediatr* or infan* or bab*)
- (Factor* OR determinant* OR correlate* OR cause*)
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction
2.5. Quality Assessment
3. Results
3.1. Characteristics of Included Studies
3.2. Evidence from Reviewed Studies
4. Discussion
4.1. Strengths and Limitations
4.2. Policy Implications
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- United Nations International Children’s Fund; World Health Organization; The World Bank. 2011 Joint Child Malnutrition Estimates-Levels and Trends; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- United Nations International Children’s Fund. State of the World’s Children Statistical Report; United Nations International Children’s Fund: New York, NY, USA, 2015. [Google Scholar]
- Onis, M.; Dewey, K.G.; Borghi, E.; Onyango, A.W.; Blössner, M.; Daelmans, B.; Piwoz, E.; Branca, F. The World Health Organization’s global target for reducing childhood stunting by 2025: Rationale and proposed actions. Matern. Child Nutr. 2013, 9, 6–26. [Google Scholar] [CrossRef] [PubMed]
- Franke, R.H.; Barrett, G.V. The economic implications of malnutrition: Comment. Econ. Dev. Cult. Chang. 1975, 23, 341–350. [Google Scholar] [CrossRef]
- Stewart, C.P.; Lannotti, L.; Dewey, K.G.; Michaelsen, K.F.; Onyango, A.W. Contextualising complementary feeding in a broader framework for stunting prevention. Matern. Child Nutr. 2013, 9, 27–45. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Statistics Report; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- United Nations. The Millennium Development Goals Report; United Nations: New York, NY, USA, 2015. [Google Scholar]
- United Nations International Children’s Fund. Multi-Sectoral Approaches to Nutrition: Nutrition-Specific and Nutrition-Sensitive Interventions to Accelerate Progress; United Nations International Children’s Fund: New York, NY, USA, 2014. [Google Scholar]
- De Onis, M. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeffrey, D.S.; The UN Millennium Project. Investing in Development: A Practical Plan to Achieve the Millennium Development Goals; Routledge: Abingdon, UK, 2005. [Google Scholar]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tette, E.M.; Sifah, E.K.; Nartey, E.T.; Nuro-Ameyaw, P.; Tete-Donkor, P.; Biritwum, R.B. Maternal profiles and social determinants of malnutrition and the MDGs: What have we learnt? BMC Public Health 2016, 16, 214. [Google Scholar] [CrossRef] [PubMed]
- Tette, E.M.; Sifah, E.K.; Nartey, E.T. Factors affecting malnutrition in children and the uptake of interventions to prevent the condition. BMC Pediatr. 2015, 15, 189. [Google Scholar] [CrossRef] [PubMed]
- Cousens, S.; Nacro, B.; Curtis, V.; Kanki, B.; Tall, F.; Traore, E.; Mertens, T. Prolonged breast-feeding: No association with increased risk of clinical malnutrition in young children in Burkina Faso. Bull. World Health Organ. 1993, 71, 713–722. [Google Scholar] [PubMed]
- Shikur, B.; Deressa, W.; Lindtjørn, B. Association between malaria and malnutrition among children aged under-five years in Adami Tulu District, south-central Ethiopia: A case-control study. BMC Public Health 2016, 16, 174. [Google Scholar] [CrossRef] [PubMed]
- Egata, G.; Berhane, Y.; Worku, A. Predictors of acute undernutrition among children aged 6 to 36 months in east rural Ethiopia: A community based nested case-control study. BMC Pediatr. 2014, 14, 91. [Google Scholar] [CrossRef] [PubMed]
- Fikadu, T.; Assegid, S.; Dube, L. Factors associated with stunting among children of age 24 to 59 months in Meskan district, Gurage Zone, South Ethiopia: A case-control study. BMC Public Health 2014, 14, 800. [Google Scholar] [CrossRef] [PubMed]
- Radebe, B.Z.; Brady, P.; Siziya, S.; Todd, H. Maternal risk factors for childhood malnutrition in the Mazowe District of Zimbabwe. Cent. Afr. J. Med. 1996, 42, 240–244. [Google Scholar] [PubMed]
- Bouvier, P.; Papart, J.P.; Wanner, P.; Picquet, M.; Rougemont, A. Malnutrition of children in Sikasso (Mali): Prevalence and socio-economic determinants. Soc. Prev. Med. 1995, 40, 27–34. [Google Scholar] [CrossRef]
- Akombi, B.J.; Agho, K.E.; Merom, D.; Hall, J.J.; Renzaho, A.M. Multilevel analysis of factors associated with wasting and underweight among children under-five years in Nigeria. Nutrients 2017, 9, 44. [Google Scholar] [CrossRef] [PubMed]
- Akombi, B.J.; Agho, K.E.; Hall, J.J.; Merom, D.; Astell-Burt, T.; Renzaho, A.M. Stunting and severe stunting among children under-5 years in Nigeria: A multilevel analysis. BMC Pediatr. 2017, 17, 15. [Google Scholar] [CrossRef] [PubMed]
- Aheto, J.M.K.; Keegan, T.J.; Taylor, B.M.; Diggle, P.J. Childhood malnutrition and its determinants among under-five children in Ghana. Matern. Child Nutr. 2015, 29, 552–561. [Google Scholar] [CrossRef] [PubMed]
- Ogunlesi, T.A.; Ayeni, V.A.; Fetuga, B.M.; Adekanmbi, A.F. Severe acute malnutrition in a population of hospitalized under-five Nigerian children. Niger. Postgrad. Med. J. 2015, 22, 15–20. [Google Scholar] [PubMed]
- Novignon, J.; Aboagye, E.; Agyemang, O.S.; Aryeetey, G. Socioeconomic-related inequalities in child malnutrition: Evidence from the Ghana multiple indicator cluster survey. Health Econ. Rev. 2015, 5, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Balogun, T.B.; Yakubu, A.M. Recent illness, feeding practices and father’s education as determinants of nutritional status among preschool children in a rural Nigerian community. J. Trop. Pediatr. 2015, 61, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Darteh, E.K.M.; Acquah, E.; Kumi-Kyereme, A. Correlates of stunting among children in Ghana. BMC Public Health 2014, 14, 504. [Google Scholar] [CrossRef] [PubMed]
- Beiersmann, C.; Lorenzo, J.B.; Bountogo, M.; Tiendrébeogo, J.; Gabrysch, S.; Yé, M.; Müller, O. Malnutrition determinants in young children from Burkina Faso. J. Trop. Pediatr. 2013, 59, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Adekanmbi, V.T.; Kayode, G.A.; Uthman, O.A. Individual and contextual factors associated with childhood stunting in Nigeria: A multilevel analysis. Matern. Child Nutr. 2013, 9, 244–259. [Google Scholar] [CrossRef] [PubMed]
- Idris, S.H.; Popoola-Zakariyya, B.; Sambo, M.N.; Sufyan, M.B.; Abubakar, A. Nutritional status and pattern of infant feeding practices among children under five in a rural community of Northwestern Nigeria. Int. Q. Community Health Educ. 2013, 33, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Nikoi, E.; Anthamatten, P. An examination of environmental correlates with childhood height-for-age in Ghana. Public Health Nutr. 2013, 16, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Olusanya, B.O.; Wirz, S.L.; Renner, J.K. Prevalence, pattern and risk factors for undernutrition in early infancy using the WHO Multicentre Growth Reference: A community-based study. Paediatr. Périnat. Epidemiol. 2010, 24, 572–583. [Google Scholar] [CrossRef] [PubMed]
- Van de Poel, E.; Hosseinpoor, A.R.; Jehu-Appiah, C.; Vega, J.; Speybroeck, N. Malnutrition and the disproportional burden on the poor: The case of Ghana. Int. J. Equity Health 2007, 6, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Odunayo, S.I.; Oyewole, A.O. Risk factors for malnutrition among rural Nigerian children. Asia Pac. J. Clin. Nutr. 2006, 15, 491–495. [Google Scholar] [PubMed]
- Ukwuani, F.A.; Suchindran, C.M. Implications of women’s work for child nutritional status in sub-Saharan Africa: A case study of Nigeria. Soc. Sci. Med. 2003, 56, 2109–2121. [Google Scholar] [CrossRef]
- Ojofeitimi, E.O.; Owolabi, O.O.; Aderonmu, A.; Esimai, A.O.; Olasanmi, S.O.H. A study on under-five nutritional status and its determinants in a semi-rural community of Ile-Ife, Osun State, Nigeria. Nutr. Health 2003, 17, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Abidoye, R.O.; Ihebuzor, N.N. Assessment of nutritional status using anthropometric methods on 1–4 year old children in an urban ghetto in Lagos, Nigeria. Nutr. Health 2001, 15, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Ighogboja, S.I. Some factors contributing to protein-energy malnutrition in the middle belt of Nigeria. East Afr. Med. J. 1992, 69, 566–571. [Google Scholar] [PubMed]
- Demilew, Y.M.; Abie, D.D. Undernutrition and associated factors among 24–36-month-old children in slum areas of Bahir Dar city, Ethiopia. Int. J. Gen. Med. 2017, 10, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Kinyoki, D.K.; Berkley, J.A.; Moloney, G.M.; Kandala, N.B.; Noor, A.M. Predictors of the risk of malnutrition among children under the age of 5 years in Somalia. Public Health Nutr. 2015, 18, 3125–3133. [Google Scholar] [CrossRef] [PubMed]
- Yisak, H.; Gobena, T.; Mesfin, F. Prevalence and risk factors for under nutrition among children under five at Haramaya district, Eastern Ethiopia. BMC Pediatr. 2015, 15, 212. [Google Scholar] [CrossRef] [PubMed]
- Chirande, L.; Charwe, D.; Mbwana, H.; Victor, R.; Kimboka, S.; Issaka, A.I.; Agho, K.E. Determinants of stunting and severe stunting among under-fives in Tanzania: Evidence from the 2010 cross-sectional household survey. BMC Pediatr. 2015, 15, 165. [Google Scholar] [CrossRef] [PubMed]
- Asfaw, M.; Wondaferash, M.; Taha, M.; Dube, L. Prevalence of undernutrition and associated factors among children aged between six to fifty nine months in Bule Hora district, South Ethiopia. BMC Public Health 2015, 15, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fekadu, Y.; Mesfin, A.; Haile, D.; Stoecker, B.J. Factors associated with nutritional status of infants and young children in Somali Region, Ethiopia: A cross-sectional study. BMC Public Health 2015, 15, 846. [Google Scholar] [CrossRef] [PubMed]
- Semali, I.A.; Tengia-Kessy, A.; Mmbaga, E.J.; Leyna, G. Prevalence and determinants of stunting in under-five children in central Tanzania: Remaining threats to achieving Millennium Development Goal 4. BMC Public Health 2015, 15, 1153. [Google Scholar] [CrossRef] [PubMed]
- Alemayehu, M.; Tinsae, F.; Haileslassie, K.; Seid, O.; Gebregziabher, G.; Yebyo, H. Undernutrition status and associated factors in under-5 children, in Tigray, Northern Ethiopia. Nutrition 2015, 31, 964–970. [Google Scholar] [CrossRef] [PubMed]
- Nordang, S.; Shoo, T.; Holmboe-Ottesen, G.; Kinabo, J.; Wandel, M. Women’s work in farming, child feeding practices and nutritional status among under-five children in rural Rukwa, Tanzania. Br. J. Nutr. 2015, 114, 1594–1603. [Google Scholar] [CrossRef] [PubMed]
- Habaasa, G. An investigation on factors associated with malnutrition among under-five children in Nakaseke and Nakasongola districts, Uganda. BMC Pediatr. 2015, 15, 1. [Google Scholar] [CrossRef] [PubMed]
- Dabale, G.A.; Sharma, M.K. Determinants of wasting among under-five children in Ethiopia: A multilevel logistic regression model approach. Int. J. Stat. Med. Res. 2014, 3, 368. [Google Scholar] [CrossRef]
- Abubakar, A.; Uriyo, J.; Msuya, S.E.; Swai, M.; Stray-Pedersen, B. Prevalence and risk factors for poor nutritional status among children in the Kilimanjaro Region of Tanzania. Int. J. Environ. Res. Public Health 2012, 9, 3506–3518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abuya, B.A.; Ciera, J.; Kimani-Murage, E. Effect of mother’s education on child’s nutritional status in the slums of Nairobi. BMC Pediatr. 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Gewa, C.A.; Yandell, N. Undernutrition among Kenyan children: Contribution of child, maternal and household factors. Public Health Nutr. 2012, 15, 1029–1038. [Google Scholar] [CrossRef] [PubMed]
- Mulugeta, A.; Hagos, F.; Kruseman, G.; Linderhof, V.; Stoecker, B.; Abraha, Z.; Samuel, G.G. Child malnutrition in Tigray, northern Ethiopia. East Afr. Med. J. 2010, 87, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Engebretsen, I.; Tylleskär, T.; Wamani, H.; Karamagi, C.; Tumwine, J.K. Determinants of infant growth in Eastern Uganda: A community-based cross-sectional study. BMC Public Health 2008, 8, 418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nyaruhucha, C.N.; Msuya, J.M.; Mamiro, P.S.; Kerengi, A.J. Nutritional status and feeding practices of under-five children in Simanjiro District, Tanzania. Tanzan. J. Health Res. 2006, 8. [Google Scholar] [CrossRef]
- Bloss, E.; Wainaina, F.; Bailey, R.C. Prevalence and predictors of underweight, stunting, and wasting among children aged 5 and under in western Kenya. J. Trop. Pediatr. 2004, 50, 260–270. [Google Scholar] [CrossRef] [PubMed]
- Wamani, H.; Tylleskär, T.; Åstrøm, A.N.; Tumwine, J.K.; Peterson, S. Mothers’ education but not fathers’ education, household assets or land ownership is the best predictor of child health inequalities in rural Uganda. Int. J. Equity Health 2004, 3, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kikafunda, J.K.; Walker, A.F.; Collett, D.; Tumwine, J.K. Risk factors for early childhood malnutrition in Uganda. Pediatrics 1998, 102, e45. [Google Scholar] [CrossRef]
- Getaneh, T.; Assefa, A.; Tadesse, Z. Protein-energy malnutrition in urban children: Prevalence and determinants. Ethiop. Med. J. 1998, 36, 153–166. [Google Scholar] [PubMed]
- Vella, V.; Tomkins, A.; Nviku, J.; Marshall, T. Determinants of nutritional status in south-west Uganda. J. Trop. Pediatr. 1995, 41, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Mbago, M.C.; Namfua, P.P. Some determinants of nutritional status of one-to four-year-old children in low income urban areas in Tanzania. J. Trop. Pediatr. 1992, 38, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Lesiapeto, M.S.; Smuts, C.M.; Hanekom, S.M.; Du Plessis, J.; Faber, M. Risk factors of poor anthropometric status in children under five years of age living in rural districts of the Eastern Cape and KwaZulu-Natal provinces, South Africa. S. Afr. J. Clin. Nutr. 2010, 23, 202–207. [Google Scholar] [CrossRef]
- Willey, B.A.; Cameron, N.; Norris, S.A.; Pettifor, J.M.; Griffiths, P.L. Socio-economic predictors of stunting in preschool children: A population-based study from Johannesburg and Soweto. SAMJ S. Afr. Med. J. 2009, 99, 450–456. [Google Scholar] [PubMed]
- Chopra, M. Risk factors for undernutrition of young children in a rural area of South Africa. Public Health Nutr. 2003, 6, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Tharakan, C.T.; Suchindran, C.M. Determinants of child malnutrition—An intervention model for Botswana. Nutr. Res. 1999, 19, 843–860. [Google Scholar] [CrossRef]
- Nagahori, C.; Tchuani, J.P.; Yamauchi, T. Factors associated with nutritional status in children aged 5–24 months in the Republic of Cameroon. Nurs. Health Sci. 2015, 17, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Nolla, N.P.; Sop, M.M.K.; Mananga, M.J.; Ekoe, T.; Gouado, I. Assessment of nutritional status of preschool children in the Bangang rural community, Cameroon. Int. J. Biotechnol. Food Sci. 2014, 2, 44–52. [Google Scholar]
- Mukatay, A.W.; Kalenga, P.M.; Dramaix, M.; Hennart, P.; Schirvel, C.; Kabamba, L.M.; Donnen, P. Factors associated with malnutrition in children aged under-five years in Lubumbashi (DRC). Sante Publique Fr. 2009, 22, 541–550. [Google Scholar]
- Delpeuch, F.; Traissac, P.; Martin-Prével, Y.; Massamba, J.P.; Maire, B. Economic crisis and malnutrition: Socioeconomic determinants of anthropometric status of preschool children and their mothers in an African urban area. Public Health Nutr. 2000, 3, 39–47. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; United Nations International Children’s Fund. Progress on Drinking Water and Sanitation: 2014 Update; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Sarmiento, O.L.; Parra, D.C.; González, S.A.; González-Casanova, I.; Forero, A.Y.; Garcia, J. The dual burden of malnutrition in Colombia. Am. J. Clin. Nutr. 2014, 100, 1628S–1635S. [Google Scholar] [CrossRef] [PubMed]
- Nutrition, I.C. The Achievable Imperative for Global Progress New York; NY United Nations Children’s Fund: New York, NY, USA, 2013. [Google Scholar]
- Caulfield, L.E.; Huffman, S.L.; Piwoz, E.G. Interventions to improve intake of complementary foods by infants 6 to 12 months of age in developing countries: Impact on growth and on the prevalence of malnutrition and potential contribution to child survival. Food Nutr. Bull. 1999, 20, 183–200. [Google Scholar] [CrossRef]
- Issaka, A.I.; Agho, K.E.; Page, A.N.; Burns, P.L.; Stevens, G.J.; Dibley, M.J. Determinants of suboptimal complementary feeding practices among children aged 6–23 months in four Anglophone West African countries. Matern. Child Nutr. 2015, 11, 14–30. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Indicators for Assessing Infant and Young Child Feeding Practices Part 3: Country Profiles; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Onyango, A.W.; Borghi, E.; de Onis, M.; del Carmen Casanovas, M.; Garza, C. Complementary feeding and attained linear growth among 6–23-month-old children. Public Health Nutr. 2014, 17, 1975–1983. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; De Onis, M.; Uauy, R. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Akhtar, S. Malnutrition in South Asia—A critical reappraisal. Crit. Rev. Food Sci. Nutr. 2016, 56, 2320–2330. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Statistics Report; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Arthur, S.S.; Nyide, B.; Soura, A.B.; Kahn, K.; Weston, M.; Sankoh, O. Tackling malnutrition: A systematic review of 15-year research evidence from INDEPTH health and demographic surveillance systems. Glob. Health Action 2015, 8, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Black, R.; Alderman, H.; Bhutta, Z.; Gillespie, S.; Haddad, L.; Horton, S. Executive summary of the Lancet Maternal and Child Nutrition Series. Matern. Child Nutr. 2013, 1, 1–12. [Google Scholar]
- Smith, L.C.; Haddad, L. Reducing child undernutrition: Past drivers and priorities for the post-MDG era. World Dev. 2015, 68, 180–204. [Google Scholar] [CrossRef]
- Akombi, B.J.; Agho, K.E.; Merom, D.; Renzaho, A.M.; Hall, J.J. Child malnutrition in sub-Saharan Africa: A meta-analysis of Demographic and Health Surveys (2006–2016). PLoS ONE 2017, 12, e0177338. [Google Scholar] [CrossRef] [PubMed]
- Lopriore, C.; Muehlhoff, E. Food security and nutrition trends in West Africa—Challenges and the way forward. In Proceedings of the 2nd International Workshop on Food-based Approaches for a Healthy Nutrition, Ouagadougou, Burkina, 23–28 November 2003. [Google Scholar]
- Salami, A.; Kamara, A.B.; Brixiova, Z. Smallholder Agriculture in East Africa: Trends, Constraints and Opportunities; African Development Bank: Tunis, Tunisia, 2010. [Google Scholar]
- Grant, M.J.; Booth, A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
| Author [Ref.] Year, Country | No of Children (N), Age | Factors Associated with Stunting | Factors Associated with Wasting | Factors Associated with Underweight | Quality Assessment (0–8 Points) |
| Akombi et al. [21] 2017 Nigeria | N = 24,529 0–59 months | Place of residence (rural), geopolitical zone (North West), low parent education, home delivery, birth size (small), low mother’s BMI (<18.5), sex (male), No delivery assistance, fever, child’s age (older) | Geographical zone (North West), sex (male), birth size (small), low parent education, home delivery, prolonged duration of BF (>12 months), fever, diarrhoeal episode, low mother’s BMI (<18.5), short birth interval (<24 months) | 8 High quality | |
| Akombi et al. [22] 2017 Nigeria | N = 24,529 0–59 months | Geopolitical zone (North West), diarrhoeal episode, sex (male), birth size (small), wealth index (poor household), prolonged duration of BF (>12 months) | 8 High quality | ||
| Aheto et al. [23] 2015 Ghana | N = 2083 0–59 months | Child’s age (older), prolonged duration of BF (>12 months), multiple births, birth size (small), wealth index (poor household), low mother’s BMI (<18.5) and lack of health insurance | Child’s age (older), diarrhoeal episodes, birth size (small), absence of toilet facility, low mother’s BMI (<18.5) | Child’s age (older), prolonged duration of BF (>12 months), multiple births, diarrhoeal episodes, birth size (small), low mother’s education and BMI (<18.5) | 6 Medium quality |
| Ogunlesi et al. [24] 2015 Nigeria | N = 208 0–59 months | Low mother’s education, Infections, non-exclusive BF | 4 Medium quality | ||
| Novignon et al. [25] 2015 Ghana | N = 3675 0–59 months | Place of residence (rural), low mother’s education, wealth index (poor household), sex (male), Geographical region (Northern) | Place of residence (rural), low mother’s education, wealth index (poor household), sex (male), Geographical region (Northern) | Place of residence (rural), low mother’s education, wealth index (poor household), sex (male), Geographical region (Northern) | 6 Medium quality |
| Balogun et al. [26] 2014 Nigeria | N = 366 2 weeks–59 months | Low father’s education | Diarrhoeal episode | Low father’s education | 3 Low quality |
| Darteh et al. [27] 2014 Ghana | N = 2379 0–59 months | Sex (male), child’s age (36–47 months), geographical region (Eastern), mother’s age (35–44 years), large family size (5–8 children) | 6 Medium quality | ||
| Beiersmann et al. [28] 2013 Burkina Faso | N = 460 6–31 months | Place of residence (rural), child’s age (24–35 months), religion (Muslim), presence of younger siblings | 7 High quality | ||
| Adekanmbi et al. [29] 2013 Nigeria | N = 28,647 0–59 months | Sex (male), child’s age (>11 months), multiple birth, low birthweight, low mother’s education, low mother’s BMI (<18.5), wealth index (poor household), short birth interval, geopolitical zone (North West and North East) | 8 High quality | ||
| Idris et al. [30] 2013 Nigeria | N = 332 0–59 months | Low mother’s education, large family size (>6 children) | Low mother’s education | Low mother’s education | 2 Low quality |
| Nikoi et al. [31] 2012 Ghana | N = 2225 0–59 months | Child’s age (older), birth size (small), not vaccinated, prolonged duration of BF (>12 months), low mother’s BMI (<18.5), wealth index (poor household) | 6 Medium quality | ||
| Olusanya et al. [32] 2010 Nigeria | N = 5888 0–3 months | Multiple births, child’s age (1–2 months), low mother’s education, mother’s age (<20 years), sex (male) | Multiple births, home delivery, sex (male), child’s age (>30 days), mother’s age (<20 years), shared sanitation facilities | Low mother’s education, mother’s age (>35 or < 20 years), child’s age (>30 days), sex (male), multiple births, home delivery | 6 Medium quality |
| Ellen Van de Poel et al. [33] 2007 Ghana | N = 3061 0–59 months | Wealth index (poor household), child’s age (older), birth size (small), sex (male), prolonged duration of BF (>12 months), short birth interval, Low mother’s education, no health care use, geographical region (Northern) | 6 Medium quality | ||
| Odunayo et al. [34] 2006 Nigeria | N = 420 0–59 months | Overcrowding, low maternal income, type of complementary feeds (infant formula feeds) | Child’s age (24 months) | 4 Medium quality | |
| Ukwuani et al. [35] 2003 Nigeria | N = 5331 0–59 months | Prolonged duration of BF (>12 months), high child parity, toilet facility (pit toilet), wealth index (poor household), sex (male), low mother’s education, low birthweight, no immunization, geopolitical zone (Northern) | Diarrhoeal episode, short duration of BF, fever, low birthweight, religion (Non-Christian), no immunization | 6 Medium quality | |
| Ojofeitimi et al. [36] 2003 Nigeria | N = 230 0–59 months | Low mother’s education, child’s age (12–36 months), high child parity, no immunization, family type (polygamous) | Low mother’s education, child’s age (12–36 months), high child parity, no immunization, family type (polygamous) | 3 Low quality | |
| Abidoye et al. [37] 2001 Nigeria | N = 370 0–59 months | Low mother’s education, marital status (single), non-working mothers, wealth index (poor household), prolonged duration of BF (>12 months), poor water supply and regularity, type of housing and toilet facilities | 4 Medium quality | ||
| Ighogboja et al. [38] 1992 Nigeria | N = 400 0–59 months | Wealth index (poor household), family instability, poor environmental sanitation, faulty weaning practices, illiteracy, large family size, infections | 5 Medium quality | ||
| East Africa | |||||
| Author [Ref.] Year, Country | No of Children (N), Age | Factors Associated with Stunting | Factors Associated with Wasting | Factors Associated with Underweight | Quality Assessment (0–8 Points) |
| Demilew et al. [39] 2017 Ethiopia | N = 480 24–36 months | Fever, having two children under three years, taking pre-lacteal feeding, early or late initiation of complementary feeding | Fever, lack of latrine utilization, and lack of hand washing practice | 8 High quality | |
| Kinyoki et al. [40] 2015 Somalia | N = 73,778 6–59 months | Fever, diarrhoeal episode, sex (male), child’s age (>12 months), low intensity of vegetation cover | Fever, diarrhoeal episode, sex (male), child’s age (<12 months), low intensity of vegetation cover | 6 Medium quality | |
| Yisak et al. [41] 2015 Ethiopia | N = 791 0–59 months | Geographical region (lowland), high birth order (>6th child), large family size (>2 children), low mother’s BMI (<18.5), source of drinking water (unimproved), place of residence (rural), low mother’s education, sex (male), lacking of farmland, wealth index (poor household) | Sex (male), fever, diarrhoeal episode, no antenatal visit, method of garbage disposal (open field), large family size (>12 children), pre-lacteal feeding | Geographical region (lowland), poor initiation of complementary feeding, diarrhoeal episode, low mother’s BMI (<18.5), high birth order (4–5), home delivery, multiple births, fever, no antenatal visit, mother’s age (<20 years), source of drinking water (unimproved) | 7 High quality |
| Chirande et al. [42] 2015 Tanzania | N = 7324 0–59 months | Home delivery, no antenatal visit, Low parent education, sex (male), birth size (small), no access to potable drinking water, child’s age (0–23 months), mother’s age (<20 years), low mother’s BMI (<18.5), non-breastfed, wealth index (poor household), place of residence (rural) | 8 High quality | ||
| Asfaw et al. [43] 2015 Ethiopia | N = 796 6–59 months | Diarrhoeal episode, sex (male), receiving pre-lacteal feeding at time of birth | Diarrhoeal episode, age at start of complementary feeding (<6 years), lack of family planning | Diarrhoeal episode, sex (male), low father’s education | 8 High quality |
| Fekadu et al. [44] 2015 Ethiopia | N = 214 6–23 months | Bottle feeding, poor dietary diversity, inappropriate age of complementary feeding initiation | Diarrhoeal episode, bottle feeding | Diarrhoeal episode | 7 High quality |
| Semali et al. [45] 2015 Tanzania | N = 678 0–59 months | Low mother’s education, father’s age (<35 years), mother’s age (<25 years), no ownership of a mobile phone. | 5 Medium quality | ||
| Alemayehu et al. [46] 2015 Ethiopia | N = 605 0–59 months | Low mother’s education, low father’s education, sex (male), source of drinking water (unimproved), Child’s age (12–36 months), large family size (>10 members), late initiation of BF | Late initiation of BF, short duration of BF (6–11 months), mother’s inability to make financial decisions | Late initiation of BF, sex (female), child’s age (12–23 months), lack of toilet facility, type of complementary food (milk), mother’s inability to make financial decisions | 7 High quality |
| Nordang et al. [47] 2015 Tanzania | N = 152 0–59 months | Increased mother’s work | Diarrhoeal episode, fever, food shortage, dry-season cultivation | 8 High quality | |
| Gilbert Habaasa [48] 2015 Uganda | N = 104 0–59 months | Mother’s occupation (peasant farmers were more likely than pastoralist) | Child’s age (<12 months) | 6 Medium quality | |
| Debale et al. [49] 2014 Ethiopia | N = 9611 0–59 months | Sex (male), birth size (small), child’s age (<11 months), place of residence (rural), no mother’s education, low mother’s BMI (<18.5), wealth index (poor household), diarrhoeal episode, fever | 4 Medium quality | ||
| Abubakar et al. [50] 2012 Tanzania | N = 423 1–35 months | Low mother’s education, child’s age (older) concerns over child growth and development | Concerns over child’s growth and development, proximity to water source | 5 Medium quality | |
| Abuya et al. [51] 2012 Kenya | N = 5156 0–42 months | Low mother’s education, low birth weight, sex (male), marital status (single), high mother’s parity (1 < birth), home delivery, low SES | 6 Medium quality | ||
| Gewa et al. [52] 2011 Kenya | N = 3793 0–59 months | Sex (female), birth size (small), prolonged duration of BF(>12 months), short maternal stature (<150 cm), maternal underweight, low mother’s education, wealth index (poor household) | Sex (female), diarrhoeal episode, maternal underweight, low mother’s education, wealth index (poor household), place of residence (urban) | Sex (female), birth size (small), diarrhoeal episode, prolonged duration of BF (>12 months), maternal underweight, low mother’s education, wealth index (poor household), place of residence (urban) | 7 High quality |
| Mulugeta et al. [53] 2010 Ethiopia | N = 318 0–59 months | Child’s age (>6 months), low mother’s height, inadequate complementary foods, geographical region (Eastern and central) | Child’s age (>6 months) | Child’s age (>6 months), low mother’s weight, inadequate complementary foods | 4 Medium quality |
| Engebretsen et al. [54] 2008 Uganda | N = 723 0–11 months | Child’s age (older), sex (male), wealth index (poor household), sub-optimal infant feeding practices after birth | Diarrhoeal episode | 6 Medium quality | |
| Nyaruhucha et al. [55] 2006 Tanzania | N = 250 0–59 months | Low mother’s education, mother’s age (<20 years), child’s age (>12 months), large family size (>7 members), prolonged duration of food shortage, marital status (married polygamous) | 3 Low quality | ||
| Bloss et al. [56] 2004 Kenya | N = 175 0–59 months | Child’s age (>12 months), immunization not up-to-date | Diarrhoeal episode, early initiation of complementary feeding (<6 months), source of drinking water (unimproved), immunization not up-to-date, no kitchen garden | Child’s age (>12 months), early initiation of complementary feeding (<6 months), upper respiratory infection or other illness | 4 Medium quality |
| Wamani et al. [57] 2004 Uganda | N = 720 0–23 months | Low mother’s education, sex (male), child’s age (older), wealth index (poor household) | 7 High quality | ||
| Kikafunda et al. [58] 1998 Uganda | N = 261 0–59 months | Child’s age (older), poor health status, prolonged duration of BF (>18 months), low SES, low mother’s education, lack of paraffin as fuel, consumption of low energy density food, presence of eye pathology, consumption of small meals | Place of residence (rural), poor health status, source of drinking water (unimproved), lack of charcoal as fuel, lack of milk consumption, lack of personal hygiene | Place of residence (rural), poor health status, source of drinking water (unimproved), lack of charcoal as fuel, lack of milk consumption, lack of personal hygiene | 4 Medium quality |
| Getaneh et al. [59] 1998 Ethiopia | N = 669 0–59 months | Child’s age (>2 years), low SES, poor housing condition, non-availability of latrine, source of drinking water (unimproved), an attack of pertussis, not completing immunization, prolonged duration of BF (>12 months), nutritionally inadequate diet | Child’s age (>2 years), low SES, non-availability of latrine, source of drinking water (unimproved), an attack of pertussis, not completing immunization, nutritionally inadequate diet, poor housing condition, prolonged duration of BF (>12 months) | Child’s age (>2 years), low SES, poor housing condition, non-availability of latrine, source of drinking water (unimproved), an attack of pertussis, not completing immunization, prolonged duration of BF (>12 months), nutritionally inadequate diet | 6 Medium quality |
| Vella et al. [60] 1995 Uganda | N = 4320 0–59 months | Diarrhoeal episode, non-availability of latrine, low father’s education, crowded household, pregnant mother, not being breastfed, religion (Muslim) | Diarrhoeal episode, marital status (divorced), religion (Muslim or Catholic), distance from health centre (>4 miles) | Diarrhoeal episode, marital status (divorced), pregnant mother, non-availability of latrine, large family size (>3 members), distance from health centre (>4 miles), father’s occupation (subsistence farmer), low father’s education, birth order (first or second child), religion (Catholic) | 4 Medium quality |
| Mbago et al. [61] 1992 Tanzania | N = 949 12–48 months | Sex (female), place of residence (small towns), malaria | Sex (female), low mother’s education, mother’s age (<25 years), diarrhoeal episode, low frequency of feeding | 3 Low quality | |
| Southern Africa | |||||
| Author [Ref.] Year, Country | No of Children (N), Age | Factors Associated with Stunting | Factors Associated with Wasting | Factors Associated with Underweight | Quality Assessment (0–8 Points) |
| Lesiapeto et al. [62] 2010 South Africa | N = 2485 0–59 months | Sex (male), mother’s perception that child is not growing well | Sex (male), low mother’s education, mother’s perception that child is not growing well, currently not BF (for children <24 months), diarrhoeal episode, irregular source of income | 6 Medium quality | |
| Willey et al. [63] 2009 South Africa | N = 1186 0–30 months | Sex (male), low birth weight, mother’s age (<20 years), unemployed mothers, ethnicity (black) | 4 Medium quality | ||
| Chopra et al. [64] 2003 South Africa | N = 868 0–35 months | Low mother’s education, absence of toilet facility, low birth weight, house made of traditional materials, long distance from health clinic (>1 h) | Absence of father, low mother’s education, absence of toilet facility, short duration of BF (<1 month), low birth weight, house made of traditional materials | 4 Medium quality | |
| Tharakan et al. [65] 1999 Botswana | N = 734 0–59 months | Child’s age (>12 months), low birth weight, prolonged duration of BF (>12 months), place of residence (rural), toilet facility (pit latrine), low mother’s education, low father’s education | Low birth weight, gender of family head (female), toilet facility (pit latrine), diarrhoeal episode | Place of residence (rural), gender of family head (female), low birth weight, prolonged duration of BF (>12 months), child’s age (>12 months), toilet facility (pit latrine), low mother’s education, low father’s education | 4 Medium quality |
| Central Africa | |||||
| Author [Ref.] Year, Country | No of Children (N), Age | Factors Associated with Stunting | Factors Associated with Wasting | Factors Associated with Underweight | Quality Assessment (0–8 points) |
| Nagahori et al. [66] 2015 Cameroun | N = 100 5–24 months | Mother’s age (<20 years), child’s age (older), low mother’s education, mothers with no family planning information, source of drinking water (unimproved) | Mother’s age (low), low mother’s education, mothers with no family planning information, source of drinking water (unimproved) | Mother’s age (low), low mother’s education, mothers with no family planning information, source of drinking water (unimproved) | 6 Medium quality |
| Nolla et al. [67] 2014 Cameroun | N = 475 2 weeks–59 months | Low mother’s education, low fruits and vegetables intake | Low mother’s education, , low fruits and vegetables intake | Low mother’s education, , low fruits and vegetables intake | 6 Medium quality |
| Mukatay et al. [68] 2010 DRC | N = 1963 0–59 months | Low mother’s education, source of drinking water (unimproved), sex (male), child’s age (>11 months) | Decreased appetite, diarrhoeal episode, child’s age (<12 months) | 4 Medium quality | |
| Delpeuch et al. [69] 1999 DRC | N = 2373 0–59 months | Low SES, low mother’s education, place of residence (peripheral area) | Child’s age (12–23 months) | 4 Medium quality | |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akombi, B.J.; Agho, K.E.; Hall, J.J.; Wali, N.; Renzaho, A.M.N.; Merom, D. Stunting, Wasting and Underweight in Sub-Saharan Africa: A Systematic Review. Int. J. Environ. Res. Public Health 2017, 14, 863. https://doi.org/10.3390/ijerph14080863
Akombi BJ, Agho KE, Hall JJ, Wali N, Renzaho AMN, Merom D. Stunting, Wasting and Underweight in Sub-Saharan Africa: A Systematic Review. International Journal of Environmental Research and Public Health. 2017; 14(8):863. https://doi.org/10.3390/ijerph14080863
Chicago/Turabian StyleAkombi, Blessing J., Kingsley E. Agho, John J. Hall, Nidhi Wali, Andre M. N. Renzaho, and Dafna Merom. 2017. "Stunting, Wasting and Underweight in Sub-Saharan Africa: A Systematic Review" International Journal of Environmental Research and Public Health 14, no. 8: 863. https://doi.org/10.3390/ijerph14080863








