Type and Context of Alcohol-Related Injury among Patients Presenting to Emergency Departments in a Caribbean Country
Abstract
:1. Introduction
- To document the proportion of victims of non-fatal injuries with alcohol intoxication in a probability sample of emergency room patients at four hospitals geographically distributed throughout Trinidad and Tobago.
- To examine the context in which drinking had occurred prior to the injury, and other drinking variables.
- To collect information on the association of patterns of drinking with injuries.
2. Materials and Methods
- Port-of-Spain General Hospital (POSGH) in the North West Regional Health Authority,
- Eric Williams Medical Sciences Complex (EWMSC) in the North Central Regional Health Authority,
- San Fernando General Hospital (SFGH) in the South West Regional Health Authority, and
- Scarborough General Hospital (SGH) in the Tobago Regional Health Authority.
- were at least 18 years old at the time of the study;
- had given informed consent (unconscious and ventilated patients were not included);
- presented to the ED within 6 h of their injury;
- presented to the ED for the first time for that accident/injury.
3. Results
3.1. Proportion of Patients Drinking Alcohol before Their Injuries
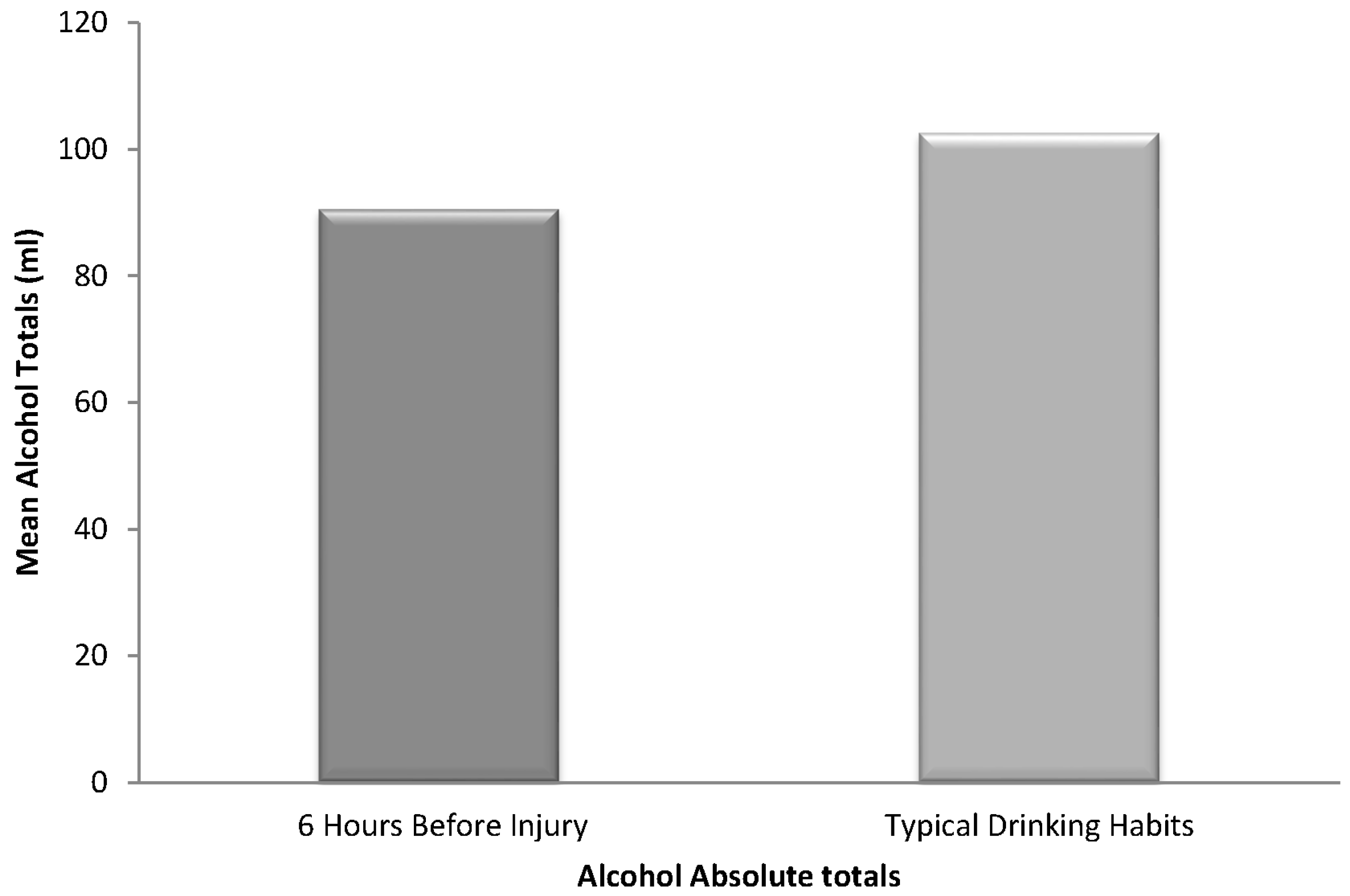
3.2. Description of Patients Who Consumed Alcohol Just before Their Injury
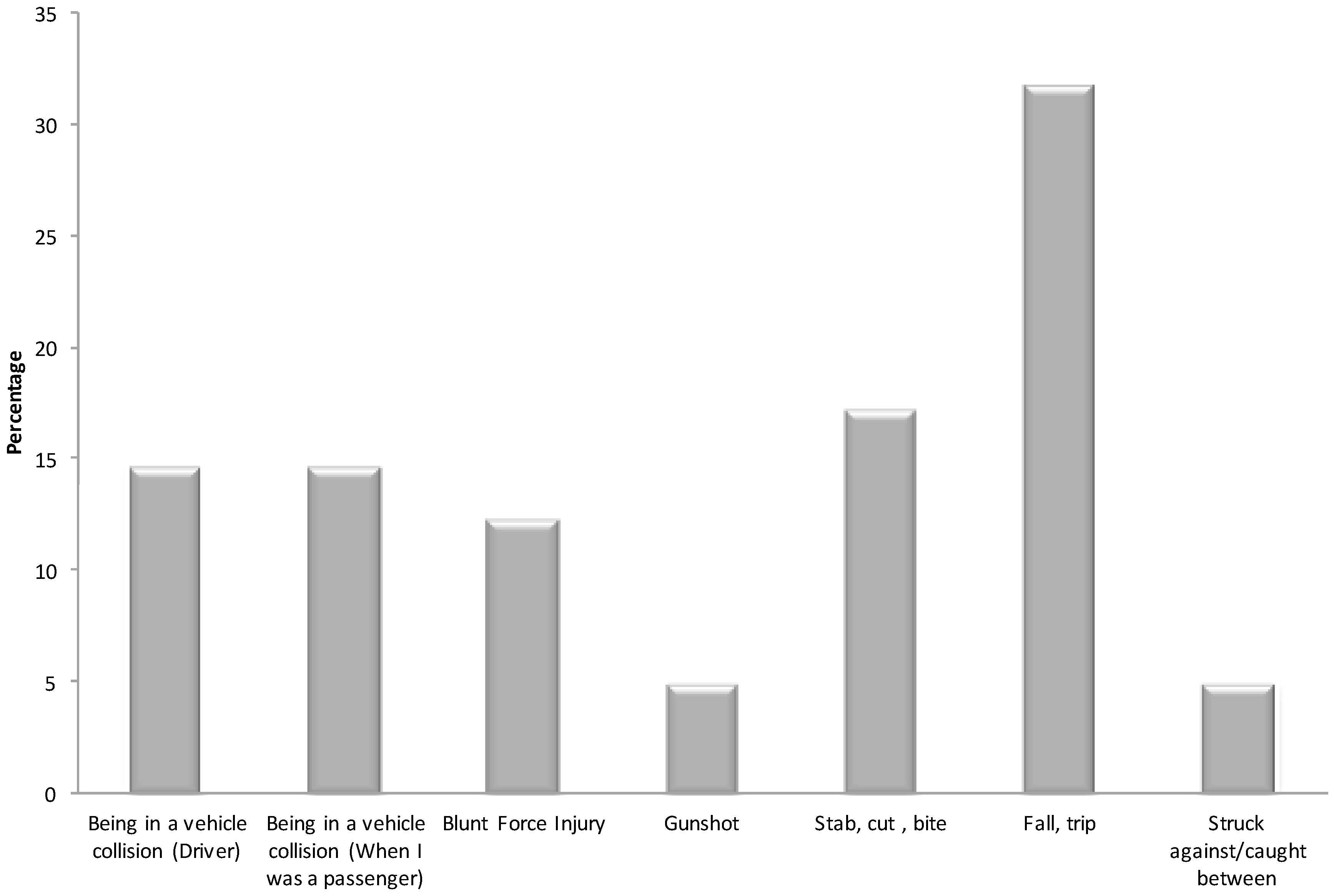
3.3. Nature of the Injuries among Patients Who Had Prior Consumption of Alcohol
3.4. Location of Injury
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Cherpitel, C.J. Focus on: The burden of alcohol use—Trauma and emergency outcomes. Alcohol Res. 2013, 35, 150–154. [Google Scholar] [PubMed]
- Taylor, B.; Irving, H.M.; Kanteres, F.; Room, R.; Borges, G.; Cherpitel, C.; Greenfield, T.; Rehm, J. The more you drink, the harder you fall: A systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug Alcohol Depend. 2010, 110, 108–116. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Status Report on Alcohol and Health 2014; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Andreuccetti, G.; Carvalho, H.B.; Korcha, R.; Ye, Y.; Bond, J.; Cherpitel, C.J. A review of emergency room studies on alcohol and injuries conducted in Latin America and the Caribbean region. Drug Alcohol Rev. 2012, 31, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization/World Health Organization. Regional Status Report on Alcohol and Health in the Americas; PAHO: Washington, DC, USA, 2015. [Google Scholar]
- Shield, K.D.; Monteiro, M.; Roerecke, M.; Smith, B.; Rehm, J. Alcohol consumption and burden of disease in the Americas in 2012: Implications for alcohol policy. Rev. Panam. Salud Publica 2015, 38, 442–449. [Google Scholar] [PubMed]
- Borges, G.; Orozco, R.; Monteiro, M.; Cherpitel, C.; Then, E.P.; López, V.A.; Bassiet-Paltoo, M.; Weil, D.A.; De Bradshaw, A.M. Risk of injury after alcohol consumption from case-crossover studies in five countries from the Americas. Addiction 2013, 108, 97–103. [Google Scholar] [CrossRef] [PubMed]
- The World Bank, World Development Indicators. GNI per Capita, Atlas Method. 2012. Available online: http://data.worldbank.org/indicator/NY.GNP.PCAP.CD (accessed on 27 April 2017).
- Pan American Health Organization. Trinidad and Tobago. In Health in the Americas; Pan American Health Organization: Washington, DC, USA, 2012. [Google Scholar]
- Borges, G.; Cherpitel, C.J. Emergency room studies in the Americas: Methods and context. In Prevention of Alcohol-Related Injuries in the Americas: From Evidence to Policy Action; Cherpitel, C.J., Birges, G., Giesbrecht, N., Monteiro, M., Stockwell, T., Eds.; PAHO: Washington, DC, USA, 2013; pp. 49–52. [Google Scholar]
- Korcha, R.A.; Cherpitel, C.J.; Ye, Y.; Bond, J.; Andreuccetti, G.; Borges, G.; Bazargan-Hejazi, S. Alcohol use and injury severity among emergency department patients in six countries. J. Addict. Nurs. 2013, 24, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Forson, P.K.; Gardner, A.; Oduro, G.; Bonney, J.; Biney, E.A.; Oppong, C.; Momade, E.; Maio, R.F. Frequency of alcohol use among injured adult patients presenting to a Ghanaian Emergency Department. Ann. Emerg. Med. 2016, 68, 492–500. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Cherpitel, C.J.; Macdonald, S. Alcohol-related injuries in the Americas: Variation by cause and country. In Prevention of Alcohol-Related Injuries in the Americas: From Evidence to Policy Action; Cherpitel, C.J., Birges, G., Giesbrecht, N., Monteiro, M., Stockwell, T., Eds.; PAHO: Washington, DC, USA, 2013; pp. 61–68. [Google Scholar]
- Paltoo, M. Collaborative study of alcohol and injury in Guyana. In Prevention of Alcohol-Related Injuries in the Americas: From Evidence to Policy Action; Cherpitel, C.J., Birges, G., Giesbrecht, N., Monteiro, M., Stockwell, T., Eds.; PAHO: Washington, DC, USA, 2013; pp. 53–59. [Google Scholar]
- Smart, R.G. Behavioral and social consequences related to the consumption of different beverage types. J. Stud. Alcohol 1996, 57, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Orozco, R.; Andreuccetti, G. Comparison of context of drinking-in-the-event and injury among emergency department patients across 10 countries. In Prevention of Alcohol-Related Injuries in the Americas: From Evidence to Policy Action; Cherpitel, C.J., Birges, G., Giesbrecht, N., Monteiro, M., Stockwell, T., Eds.; PAHO: Washington, DC, USA, 2013; pp. 91–98. [Google Scholar]
- Beaubrun, M.H.; Thomas, C.; McFarlane, H.; Cumberbatch, K.; Bernard, W.; Maharaj, P. Blood alcohol concentrations of motor vehicle accident victims at the Port-of-Spain general hospital casualty department. WIMJ 1986, 35, 55. [Google Scholar]
- Daisley, H.; Landeau, P.; Gordon, A.; Simmons, V.; Barton, E.N. Alcohol, cannabinoids and cocaine in road traffic fatalities in Trinidad and Tobago. WIMJ 1989, 38, 67. [Google Scholar]
- Beaubrun, M. Conversation with Michael Beaubrun. Br. J. Addict. 1982, 77, 229–234. [Google Scholar] [PubMed]
- Honkanen, R. Alcohol in home and leisure injuries. Addiction 1993, 88, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Kool, B.; Ameratunga, S.; Jackson, R. The role of alcohol in unintentional falls among young and middle-aged adults: A systematic review of epidemiological studies. Inj. Prev. 2009, 15, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Rehm, J.; Baliunas, D.; Borges, G.L.; Graham, K.; Irving, H.; Kehoe, T.; Parry, C.D.; Patra, J.; Popova, S.; Poznyak, V.; et al. The relation between different dimensions of alcohol consumption and burden of disease: An overview. Addiction 2010, 105, 817–843. [Google Scholar] [CrossRef] [PubMed]
- Cherpitel, C.J.; Ye, Y.; Bond, J.; Borges, G.; Chou, P.; Nilsen, P.; Ruan, J.; Xiang, X. Multi-level analysis of alcohol-related injury and drinking pattern: Emergency department data from 19 countries. Addiction 2012, 107, 1263–1272. [Google Scholar] [CrossRef] [PubMed]
- Rossow, I.; Bogstrand, S.T.; Ekeberg, Ø.; Normann, P.T. Associations between heavy episodic drinking and alcohol related injuries: A case control study. BMC Public Health 2013, 13, 1076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borges, G.; Cherpitel, C.; Orozco, R.; Bond, J.; Ye, Y.; Macdonald, S.; Rehm, J.; Poznyak, V. Multicentre study of acute alcohol use and non-fatal injuries: Data from the WHO collaborative study on alcohol and injuries. Bull. World Health Organ. 2006, 84, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Watt, K.; Purdie, D.M.; Roche, A.M.; McClure, R.J. Risk of injury from acute alcohol consumption and the influence of confounders. Addiction 2004, 99, 1262–1273. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Cherpitel, C.J. Risk of injury associated with alcohol and alcohol-related injury. In Alcohol and Injuries: Emergency Department Studies in an International Perspective; Cherpitel, C., Borges, G., Giesbrecht, N., Hungerford, D., Peden, M., Poznyak, V., Rom, R., Stockwell, T., Eds.; World Health Organization: Geneva, Switzerland, 2009; pp. 3–13. [Google Scholar]
- Gmel, G.; Bissery, A.; Gammeter, R.; Givel, J.C.; Calmes, J.M.; Yersin, B.; Daeppen, J.B. Alcohol-attributable injuries in admissions to a Swiss emergency room—An analysis of the link between volume of drinking, drinking patterns, and preattendance drinking. Alcohol Clin. Exp. Res. 2006, 30, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Barker, R.; Swaminathan, M.; Arora, A.; Scott, D. Emergency Department Presentations Due to Alcohol-Related Injury in Queensland. Queensland Injury Surveillance Unit Injury Bulletin No. 111. QISU, 2011. Available online: http://www.qisu.org.au/ModCoreFilesUploaded/Bulletin_111282.pdf (accessed on 12 April 2017).
- Foster, J.H.; Ferguson, C.S. Home drinking in the UK: Trends and causes. Alcohol Alcohol. 2012, 47, 355–358. [Google Scholar] [CrossRef] [PubMed]
- Bunker, N.; Woods, C.; Conway, J.; Barker, R.; Usher, K. Patterns of ‘at-home’ alcohol-related injury presentations to emergency departments. J. Clin. Nurs. 2017, 26, 157–169. [Google Scholar] [CrossRef] [PubMed]
- Ostrom, M.; Eriksson, A. Pedestrian fatalities and alcohol. Accid. Anal. Prev. 2001, 33, 173–180. [Google Scholar] [CrossRef]
- Prijon, T.; Ermenc, B. Influence of alcohol intoxication of pedestrians on injuries in fatal road accidents. Forensic Sci. Int. Suppl. Ser. 2009, 1, 33–34. [Google Scholar] [CrossRef]
- Dultz, L.A.; Frangos, S.; Foltin, G.; Marr, M.; Simon, R.; Bholat, O.; Levine, D.A.; Slaughter-Larkem, D.; Jacko, S.; Ayoung-Chee, P.; et al. Alcohol use by pedestrians who are struck by motor vehicles: How drinking influences behaviors, medical management, and outcomes. J. Trauma Acute Care Surg. 2011, 71, 1252–1257. [Google Scholar] [CrossRef] [PubMed]
- Plackett, T.P.; Ton-That, H.H.; Mueller, J.; Grimley, K.M.; Kovacs, E.J.; Esposito, T.J. Screening for at-risk drinking behavior in trauma patients. J. Am. Osteopath. Assoc. 2015, 115, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Gentilello, L.M.; Ebel, B.E.; Wickizer, T.M.; Salkever, D.S.; Rivara, F.P. Alcohol interventions for trauma patients treated in emergency departments and hospitals: A cost benefit analysis. Ann. Surg. 2005, 241, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Mello, M.J.; Nirenberg, T.D.; Longabaugh, R.; Woolard, R.; Minugh, A.; Becker, B.; Baird, J.; Stein, L. Emergency department brief motivational interventions for alcohol with motor vehicle crash patients. Ann. Emerg. Med. 2005, 45, 620–625. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, G.; Pantalon, M.V.; Degutis, L.C.; Fiellin, D.A.; Busch, S.H.; Chawarski, M.C.; Owens, P.H.; O’Connor, P.G. Brief intervention for hazardous and harmful drinkers in the emergency department. Ann. Emerg. Med. 2008, 51, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Woolard, R.; Cherpitel, C.; Kathleen, T. Brief intervention for emergency department patients with alcohol misuse: Implications for current practice. Alcohol Treat. Q. 2011, 29, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Crawford, M.J.; Patton, R.; Touquet, R.; Drummond, C.; Byford, S.; Barrett, B.; Reece, B.; Brown, A.; Henry, J.A. Screening and referral for brief intervention of alcohol-misusing patients in an emergency department: A pragmatic randomised controlled trial. Lancet 2004, 364, 1334–1339. [Google Scholar] [CrossRef]
- Dauer, A.R.; Rubio, E.S.; Coris, M.E.; Valls, J.M. Brief intervention in alcohol-positive traffic casualties: Is it worth the effort? Alcohol Alcohol. 2006, 41, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Sommers, M.S.; Dyehous, J.M.; Howe, S.R.; Fleming, M.; Fargo, J.D.; Schafer, J.C. Effectiveness of brief interventions after alcohol-related vehicular injury: A randomized controlled trial. J. Trauma Acute Care Surg. 2006, 61, 523–533. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, P.; Baird, J.; Mello, M.J.; Nirenberg, T.; Woolard, R.; Bendtsen, P.; Longabaugh, R. A systematic review of emergency care brief alcohol interventions for injury patients. J. Subst. Abuse Treat. 2008, 35, 184–201. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, E.; Bernstein, J.A.; Stein, J.B.; Saitz, R. SBIRT in emergency care settings: Are we ready to take it to scale? Acad. Emerg. Med. 2009, 16, 1072–1077. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, E.; Bernstein, J.; Feldman, J.; Fernandez, W.; Hagan, M.; Mitchell, P.; Owens, P. The impact of screening, brief intervention and referral for treatment in emergency department patients’ alcohol use: A 3-, 6-, and 12-month follow-up. Alcohol Alcohol. 2010, 45, 514–519. [Google Scholar] [CrossRef]
- Anderson, P.; Chisholm, D.; Fuhr, D.C. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet 2009, 373, 2234–2246. [Google Scholar] [CrossRef]
- Kelly-Weeder, S.; Phillips, K.; Rounseville, S. Effectiveness of public health programs for decreasing alcohol consumption. Patient Intell. 2011, 2011, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Babor, T.F.; Caetano, R.; Casswell, S.; Edwards, G.; Giesbrecht, N.; Graham, K.; Rossow, I. Alcohol: No Ordinary Commodity: Research and Public Policy; Oxford University Press: Oxford, UK, 2010. [Google Scholar]
- Livingston, M.; Chikritzhs, T.; Room, R. Changing the density of alcohol outlets to reduce alcohol-related problems. Drug Alcohol Rev. 2007, 26, 557–566. [Google Scholar] [CrossRef] [PubMed]
- Campbell, C.A.; Hahn, R.A.; Elder, R.; Brewer, R.; Chattopadhyay, S.; Fielding, J.; Naimi, T.S.; Toomey, T.; Lawrence, B.; Middleton, J.C.; et al. The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms. Am. J. Prev. Med. 2009, 37, 556–569. [Google Scholar] [CrossRef] [PubMed]
- Connor, J.L.; Kypri, K.; Bell, M.L.; Cousins, K. Alcohol outlet density, levels of drinking and alcohol-related harm in New Zealand: A national study. J. Epidemiol. Community Health 2011, 65, 841–846. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Status Report: Alcohol Policy. 2004. Available online: http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=15965&Itemid=270 (accessed on 24 July 2017).
- Maharaj, R.; Babwah, T.; Motilal, S.; Nunes, P.; Brathwaite, R.; Legall, G.; Reid, S.D. The National Alcohol Survey of Households in Trinidad and Tobago (NASHTT): Willingness to support changes in policy, laws and regulations. In Proceedings of the Global Alcohol Policy Conference, Edinburgh, UK, 7–9 October 2015. [Google Scholar]
- Miller, P.; Droste, N.; Baker, T.; Gervis, C. Last drinks: A study of rural emergency department data collection to identify and target community alcohol-related violence. Emerg. Med. Australas. 2015, 27, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Reid, S.D. Time for a regional alcohol policy—A literature review of the burden of normative alcohol use in the Caribbean. J. Public Health Policy 2015, 36, 469–483. [Google Scholar] [CrossRef] [PubMed]
- Cutter, H.S.; Maloof, B.; Kurtz, N.R.; Jones, W.C. “Feeling no pain” differential responses to pain by alcoholics and nonalcoholics before and after drinking. J. Stud. Alcohol 1976, 37, 273–277. [Google Scholar] [CrossRef] [PubMed]
| Hospital | No. of Patients Eligible for Interview | No. of Patients Consenting to Be Interviewed | Completion Rate |
|---|---|---|---|
| EWMSC | 93 | 75 | 80.6% |
| SGH | 24 | 12 | 50.0% |
| SFGH | 123 | 98 | 79.7% |
| POSGH | 89 | 52 | 58.4% |
| Total | 329 | 237 | 72.0% |
| Main Reason for Being Here | Frequency | Percent |
|---|---|---|
| Fracture | 6 | 12.8 |
| Strain, sprain, dislocation | 7 | 14.9 |
| Cut, bite, penetrating injury, open wound | 19 | 40.4 |
| Bruise, scrape, superficial wound | 9 | 19.1 |
| Concussion, closed head injury | 2 | 4.3 |
| Organ system injury/multiple organ injury | 2 | 4.3 |
| Other | 1 | 2.1 |
| Unknown | 1 | 2.1 |
| Total | 47 | 100.0 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reid, S.D.; Gentius, J. Type and Context of Alcohol-Related Injury among Patients Presenting to Emergency Departments in a Caribbean Country. Int. J. Environ. Res. Public Health 2017, 14, 877. https://doi.org/10.3390/ijerph14080877
Reid SD, Gentius J. Type and Context of Alcohol-Related Injury among Patients Presenting to Emergency Departments in a Caribbean Country. International Journal of Environmental Research and Public Health. 2017; 14(8):877. https://doi.org/10.3390/ijerph14080877
Chicago/Turabian StyleReid, Sandra D., and Jannel Gentius. 2017. "Type and Context of Alcohol-Related Injury among Patients Presenting to Emergency Departments in a Caribbean Country" International Journal of Environmental Research and Public Health 14, no. 8: 877. https://doi.org/10.3390/ijerph14080877




