Program Development and Effectiveness of Workplace Health Promotion Program for Preventing Metabolic Syndrome among Office Workers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
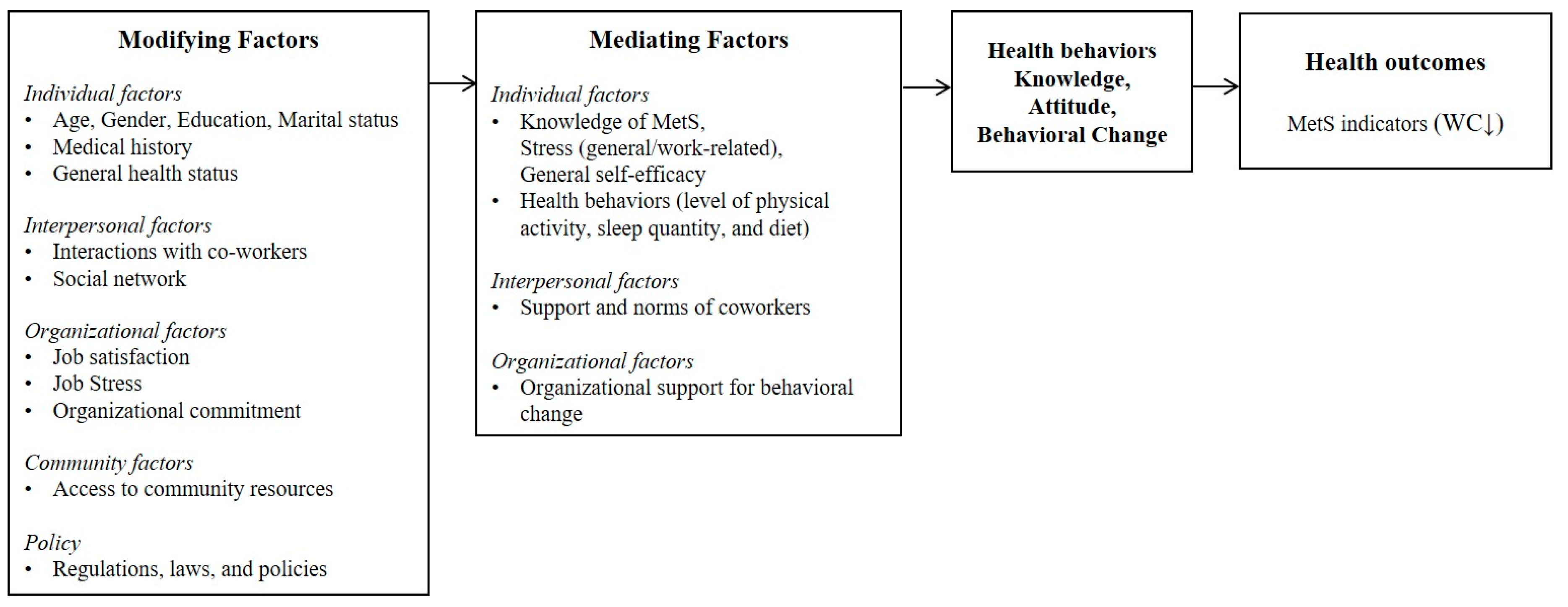
2.2. Program Development
2.3. Implementation Process
2.4. Measurement
2.5. Statistical Analysis
3. Results
3.1. Program Effectiveness for Group 1 and Group 2
3.2. Program Effectiveness for the Target Population (Group 3)
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The metabolic syndrome and cardiovascular risk: A systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 56, 1113–1132. [Google Scholar] [CrossRef] [PubMed]
- Galassi, A.; Reynolds, K.; He, J. Metabolic syndrome and risk of cardiovascular disease: A meta-analysis. Am. J. Med. 2006, 119, 812–819. [Google Scholar] [CrossRef] [PubMed]
- Malik, S.; Wong, N.D.; Franklin, S.S.; Kamath, T.V.; Gilbert, J.; Pio, J.R.; Williams, G.R. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation 2004, 110, 1245–1250. [Google Scholar] [CrossRef] [PubMed]
- Gami, A.S.; Witt, B.J.; Howard, D.E.; Erwin, P.J.; Gami, L.A.; Somers, V.K.; Montori, V.M. Metabolic syndrome and risk of incident cardiovascular events and death: A systematic review and meta-analysis of longitudinal studies. J. Am. Coll. Cardiol. 2007, 49, 403–414. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Shin, H.; Song, J.H.; Kwak, S.H.; Kang, S.M.; Yoon, J.W.; Choi, S.H.; Cho, S.I.; Park, K.S.; Lee, H.K. Increasing prevalence of metabolic syndrome in Korea. Diabetes Care 2011, 34, 1323–1328. [Google Scholar] [CrossRef] [PubMed]
- Mozumdar, A.; Liguori, G. Persistent increase of prevalence of metabolic syndrome among US adults: NHANES III to NHANES 1999–2006. Diabetes Care 2011, 34, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Nestel, P.; Lyu, R.; Low, L.P.; Sheu, W.H.-H.; Nitiyanant, W.; Saito, I.; Tan, C.E. Metabolic syndrome: Recent prevalence in East and Southeast Asian populations. Asia Pac. J. Clin. Nutr. 2007, 16, 362–367. [Google Scholar] [PubMed]
- Ministry of Health and Welfare Current State and Issues of Chronic Diseases: Chronic Disease Factbook 2015. Available online: http://www.cdc.go.kr/CDC/notice/CdcKrIntro0504.jsp?menuIds=HOME001-MNU1154-MNU0005-MNU2572-MNU0110&cid=65024 (accessed on 3 June 2017).
- Organization for Economic Cooperation and Development Employment Rate 2016. Available online: https://data.oecd.org/emp/employment-rate.htm#indicator-chart (accessed on 3 June 2017).
- Organization for Economic Cooperation and Development Average Annual Hours Actually Worked per Worker 2016. Available online: https://data.oecd.org/emp/hours-worked.htm#indicator-chart (accessed on 3 June 2017).
- Chae, D.H.; Kim, S.H.; Lee, C.Y. A study on gender differences in influencing factors of office workers’ physical activity. J. Korean Acad. Community Health Nurs. 2013, 24, 273–281. [Google Scholar] [CrossRef]
- Lee, J.-M.; Kwon, Y.-S.; Paek, K.-S. The relationship between lifestyle and health status among white collar workers in a community. J. Digit. Converg. 2014, 12, 411–421. [Google Scholar] [CrossRef]
- Kim, E.; Oh, S.W. Gender differences in the association of occupation with metabolic syndrome in Korean adults. Korean J. Obes. 2012, 21, 108–114. [Google Scholar] [CrossRef]
- Lee, W.; Yeom, H.; Yoon, J.H.; Won, J.U.; Jung, P.K.; Lee, J.H.; Seok, H.; Roh, J. Metabolic outcomes of workers according to the international standard classification of occupations in Korea. Am. J. Ind. Med. 2016, 59, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Dalle Grave, R.; Calugi, S.; Centis, E.; Marzocchi, R.; El Ghoch, M.; Marchesini, G. Lifestyle modification in the management of the metabolic syndrome: Achievements and challenges. Diabetes Metab. Syndr. Obes. 2010, 3, 373–385. [Google Scholar] [PubMed]
- Lin, K.M.; Chiou, J.Y.; Ko, S.H.; Tan, J.Y.; Huang, C.N.; Liao, W.C. Modifiable lifestyle behaviors are associated with metabolic syndrome in a Taiwanese population. J. Nurs. Scholarsh. 2015, 47, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Carnethon, M.; Whitsel, L.P.; Franklin, B.A.; Kris-Etherton, P.; Milani, R.; Pratt, C.A.; Wagner, G.R. Worksite wellness programs for cardiovascular disease prevention. Circulation 2009, 120, 1725–1741. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention Workplace Health Promotion. Available online: http://www.cdc.gov/workplacehealthpromotion/health-strategies/index.html (accessed on 3 June 2017).
- Beresford, S.A.; Locke, E.; Bishop, S.; West, B.; McGregor, B.A.; Bruemmer, B.; Duncan, G.E.; Thompson, B. Worksite study promoting activity and changes in eating (PACE): Design and baseline results. Obesity 2007, 15, 4S–15S. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.R.; Hannon, P.A.; Beresford, S.A.; Linnan, L.A.; McLellan, D.L. Health promotion in smaller workplaces in the United States. Annu. Rev. Public Health 2014, 35, 327–342. [Google Scholar] [CrossRef] [PubMed]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Behav. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. Toward an experimental ecology of human development. Am. Psychol. 1977, 32, 513. [Google Scholar] [CrossRef]
- Ryu, H.; Kim, Y.; Lee, J.; Yoon, S.-J.; Cho, J.-H.; Wong, E.; Jung, J. Office workers’ risk of metabolic syndrome-related indicators: A 10-year cohort study. West. J. Nurs. Res. 2016, 38, 1433–1447. [Google Scholar] [CrossRef] [PubMed]
- Ryu, H.; Chin, D.L. Factors associated with metabolic syndrome among Korean office workers. Archiv. Environ. Occup. Health 2016, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Wandersman, A.; Valois, R.; Ochs, L.; de la Cruz, D.S.; Adkins, E.; Goodman, R.M. Toward a social ecology of community coalitions. Am. J. Health Promot. 1996, 10, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C. Diagnosis and management of the metabolic syndrome. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Park, H.S.; Kim, D.J.; Han, J.H.; Kim, S.M.; Cho, G.J.; Kim, D.Y.; Kwon, H.S.; Kim, S.R.; Lee, C.B. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res. Clin. Pract. 2007, 75, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R.; Jerusalem, M. Generalized Self-Efficacy scale. In Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs; Weinman, J., Wright, K., Johnston, M., Eds.; NFER-NELSON: Windsor, UK, 1995; pp. 35–37. [Google Scholar]
- Lambert, S.J.; Hopkins, K. Occupational conditions and workers’ sense of community: Variations by gender and race. Am. J. Commun. Psychol. 1995, 23, 151–179. [Google Scholar] [CrossRef]
- Chang, S.J.; Koh, S.B.; Kang, D.; Kim, S.A.; Kang, M.G.; Lee, C.G.; Chung, J.J.; Cho, J.J.; Son, M.; Chae, C.H. Developing an occupational stress scale for Korean employees. Korean J. Occup. Environ. Med. 2005, 17, 297–317. [Google Scholar]
- Johnson, J.L.; Slentz, C.A.; Houmard, J.A.; Samsa, G.P.; Duscha, B.D.; Aiken, L.B.; McCartney, J.S.; Tanner, C.J.; Kraus, W.E. Exercise training amount and intensity effects on metabolic syndrome (from studies of a targeted risk reduction intervention through defined exercise). Am. J. Cardiol. 2007, 100, 1759–1766. [Google Scholar] [CrossRef] [PubMed]
- Takimoto, M.; Kibushi, M.; Okoshi, Y.; Nakagawa, T.; Irokawa, M.; Yakura, H.; Tanaka, M.; Matsuda, S. Body weight reduction program for metabolic syndrome. Asian Pac. J. Dis. Manag. 2008, 2, 93–96. [Google Scholar] [CrossRef]
- Maruyama, C.; Kimura, M.; Okumura, H.; Hayashi, K.; Arao, T. Effect of a worksite-based intervention program on metabolic parameters in middle-aged male white-collar workers: A randomized controlled trial. Prev. Med. 2010, 51, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, T.; So, R.; Shimojo, N.; Tanaka, K. Effect of aerobic exercise training followed by a low-calorie diet on metabolic syndrome risk factors in men. Nutr. Metabol. Cardiovasc. Dis. 2015, 25, 832–838. [Google Scholar] [CrossRef] [PubMed]
- Mache, S.; Jensen, S.; Linnig, S.; Jahn, R.; Steudtner, M.; Ochsmann, E.; Preuß, G. Do overweight workers profit by workplace health promotion, more than their normal-weight peers? Evaluation of a worksite intervention. J. Occup. Med. Toxicol. 2015, 10, 28. [Google Scholar] [CrossRef] [PubMed]
- Engbers, L.H.; van Poppel, M.N.; Paw, M.J.C.A.; van Mechelen, W. Worksite health promotion programs with environmental changes: A systematic review. Am. J. Prev. Med. 2005, 29, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Lemon, S.C.; Zapka, J.; Li, W.; Estabrook, B.; Rosal, M.; Magner, R.; Andersen, V.; Borg, A.; Hale, J. Step ahead: A worksite obesity prevention trial among hospital employees. Am. J. Prev. Med. 2010, 38, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Muse, L.; Harris, S.G.; Giles, W.F.; Feild, H.S. Work-life benefits and positive organizational behavior: Is there a connection? J. Organ. Behav. 2008, 29, 171–192. [Google Scholar] [CrossRef]
| Subjects’ Characteristics | Intervention Methods and Contents |
|---|---|
| Group 1 (n = 891; Health Education Group) Whole office workers in the firm |
|
| Group 2 (n = 180; U-health System Group) Voluntary participant using U-health system |
|
| Group 3 (n = 62; Target Population Group) Workers with over 3 MetS indicators (or/and) BMI ≥ 25 |
|
| Characteristics | Group 1 (n = 449) a | Group 2 (n = 75) a | Group 3 (n = 41) a |
|---|---|---|---|
| Mean ± SD or n (%) | |||
| Age (Years) | 35.31 ± 7.74 | 32.92 ± 7.07 | 36.49 ± 8.25 |
| Gender | |||
| Male | 331 (73.7) | 55 (73.3) | 31 (75.6) |
| Female | 118 (26.3) | 20 (26.7) | 10 (24.4) |
| Education | |||
| High school or lower | 25 (5.6) | 2 (2.7) | 5 (12.2) |
| College or University | 359 (80.0) | 70 (93.4) | 34 (82.9) |
| Graduate school | 65 (14.5) | 3 (4.0) | 2 (4.9) |
| Marriage status | |||
| Unmarried | 207 (46.2) | 45 (60.0) | 19 (46.3) |
| Married | 241 (53.8) | 30 (40.0) | 22 (53.7) |
| Working type | |||
| Management | 106 (23.6) | 27 (36.0) | 11 (26.8) |
| Sales | 343 (76.4) | 48 (64.0) | 30 (73.2) |
| Years worked on the job | 7.85 ± 7.63 | 6.07 ± 7.27 | 9.73 ± 9.51 |
| Characteristics | Group 1 (n = 449) a | Group 2 (n = 75) a | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | t | p c | Pre | Post | t | p c | |
| Mean ± SD or n (%) b | Mean ± SD or n (%) b | |||||||
| Waist circumference (cm) | 81.07 ± 10.72 | 81.41 ± 10.76 | −1.479 | 0.140 | 82.09 ± 10.60 | 82.53 ± 10.02 | −0.733 | 0.466 |
| Blood pressure (mmHg) | ||||||||
| Systolic blood pressure | 115.75 ± 12.80 | 116.40 ± 13.77 | −1.229 | 0.220 | 116.10 ± 10.99 | 116.07 ± 12.84 | 0.022 | 0.982 |
| Diastolic blood pressure | 72.21 ± 9.62 | 75.13 ± 10.42 | −6.433 | <0.001 | 71.55 ± 7.89 | 73.73 ± 10.57 | −2.080 | 0.041 |
| Fasting glucose (g/dL) | 93.28 ± 13.51 | 94.63 ± 18.00 | −2.628 | 0.009 | 92.00 ± 9.39 | 94.85 ± 18.41 | −1.344 | 0.183 |
| Triglycerides (g/dL) | 114.15 ± 92.63 | 119.63 ± 109.51 | −1.546 | 0.123 | 100.00 ± 65.58 | 99.27 ± 68.98 | 0.127 | 0.900 |
| HDL-cholesterol (g/dL) | 55.60 ± 12.79 | 55.54 ± 13.47 | 0.160 | 0.873 | 55.88 ± 11.94 | 56.20 ± 12.51 | −0.340 | 0.735 |
| MetS indicators prevalence | ||||||||
| Elevated waist circumference | 86 (20.5) | 84 (20.0) | 0.878 | 18 (25.7) | 17 (24.3) | 1.000 | ||
| Elevated fasting glucose | 85 (19.4) | 97 (22.1) | 0.195 | 9 (12.2) | 14 (18.9) | 0.302 | ||
| Elevated triglycerides | 91 (20.9) | 107 (24.6) | 0.068 | 9 (12.2) | 11 (14.9) | 0.727 | ||
| Reduced HDL-cholesterol | 62 (14.3) | 58 (13.3) | 0.672 | 9 (12.2) | 8 (10.8) | 1.000 | ||
| Elevated blood pressures | 94 (21.3) | 124 (28.1) | 0.002 | 15 (20.8) | 17 (23.6) | 0.804 | ||
| MetS prevalence | 0.551 | 0.508 | ||||||
| Less than 3 components | 360 (85.7) | 355 (84.5) | 62 (91.2) | 59 (86.8) | ||||
| 3 or more components * | 60 (14.3) | 65 (15.5) | 6 (8.8) | 9 (13.2) | ||||
| Individual factors | ||||||||
| General health status d | 0.207 | 0.791 | ||||||
| Bad | 207 (68.3) | 219 (72.3) | 38 (61.3) | 40 (64.5) | ||||
| Good | 96 (31.7) | 84 (27.7) | 24 (38.7) | 22 (35.5) | ||||
| General self-efficacy | 29.09 ± 3.72 | 29.65 ± 3.46 | −2.796 | 0.006 | 30.00 ± 4.01 | 29.56 ± 3.39 | 0.945 | 0.348 |
| Stress level (1–14) | 9.02 ± 2.32 | 8.91 ± 2.17 | 0.952 | 0.342 | 8.44 ± 2.15 | 8.45 ± 1.86 | −0.075 | 0.940 |
| General (1–7) | 3.96 ± 1.37 | 3.86 ± 1.36 | 1.259 | 0.209 | 3.53 ± 1.28 | 3.45 ± 1.17 | 0.567 | 0.573 |
| Work-related (1–7) | 5.06 ± 1.26 | 5.04 ± 1.26 | 0.183 | 0.855 | 4.90 ± 1.33 | 5.00 ± 1.17 | −0.704 | 0.484 |
| Knowledge of MetS (0–6) | 1.73 ± 1.77 | 1.51 ± 1.54 | 2.365 | 0.018 | 1.81 ± 1.59 | 1.52 ± 1.52 | 1.302 | 0.197 |
| Physical activity (per week) | 0.315 | 0.542 | ||||||
| No | 186 (41.4) | 187 (41.6) | 29 (38.7) | 26 (34.7) | ||||
| 1–2 times | 171 (38.1) | 186 (41.4) | 29 (38.7) | 31 (41.3) | ||||
| ≥3 times | 92 (20.5) | 76 (16.9) | 17 (22.7) | 18 (24.0) | ||||
| Sleep quantity (h) (3–10) | 0.141 | - | ||||||
| Others | 213 (70.5) | 225 (74.5) | 39 (62.9) | 40 (64.5) | ||||
| Good sleep (7 or 8 h) | 89 (29.5) | 77 (25.5) | 23 (37.1) | 22 (35.5) | ||||
| Diet (scores) (0–10) | 4.89 ± 2.30 | 5.12 ± 3.02 | −1.481 | 0.140 | 4.69 ± 2.54 | 5.81 ± 3.97 | −2.358 | 0.022 |
| Organizational factors | ||||||||
| Organizational commitment | 6.08 ± 1.06 | 6.07 ± 0.95 | 0.235 | 0.815 | 6.15 ± 0.97 | 5.82 ± 0.80 | 2.224 | 0.030 |
| Job satisfaction e | 0.470 | 0.503 | ||||||
| Not satisfied | 145 (48.5) | 154 (51.5) | 31 (50.0) | 35 (56.5) | ||||
| Satisfied | 153 (51.2) | 146 (48.8) | 31 (50.0) | 27 (43.5) | ||||
| Job stress | ||||||||
| Job demand | 54.27 ± 12.38 | 54.18 ± 11.41 | 0.107 | 0.915 | 55.26 ± 11.64 | 56.87 ± 11.90 | −0.894 | 0.375 |
| Insufficient job control | 56.65 ± 14.90 | 57.95 ± 14.57 | −1.514 | 0.131 | 57.31 ± 15.36 | 57.16 ± 15.06 | 0.079 | 0.938 |
| Inadequate social support | 64.39 ± 15.60 | 64.35 ± 14.23 | 0.038 | 0.970 | 60.43 ± 18.43 | 58.48 ± 16.34 | 0.980 | 0.331 |
| Job insecurity | 42.52 ± 22.55 | 47.94 ± 23.04 | −3.367 | 0.001 | 41.52 ± 20.20 | 51.46 ± 24.25 | −2.572 | 0.013 |
| Organizational system | 54.36 ± 15.98 | 54.77 ± 14.20 | −0.464 | 0.643 | 52.49 ± 16.66 | 54.53 ± 16.82 | −0.952 | 0.345 |
| Lack of rewards | 57.40 ± 16.25 | 56.69 ± 14.50 | 0.773 | 0.440 | 55.36 ± 18.24 | 57.50 ± 16.68 | −0.900 | 0.372 |
| Occupational climate | 36.13 ± 17.13 | 37.84 ± 17.73 | −1.564 | 0.119 | 39.91 ± 19.21 | 42.54 ± 20.64 | −0.828 | 0.411 |
| Characteristics | Pre-Intervention | Post-Intervention | t | p c |
|---|---|---|---|---|
| Mean ± SD or n (%) b | ||||
| Waist circumference (cm) | 89.96 ± 9.87 | 86.93 ± 9.79 | −4.363 | <0.001 |
| Blood pressure (mmHg) | ||||
| Systolic blood pressure | 126.13 ± 12.68 | 125.05 ± 13.49 | −0.596 | 0.555 |
| Diastolic blood pressure | 84.68 ± 10.91 | 85.13 ± 10.75 | 0.329 | 0.744 |
| Fasting glucose (g/dL) | 93.44 ± 11.78 | 84.56 ± 9.55 | −4.16 | <0.001 |
| Triglycerides (g/dL) | 155.44 ± 90.31 | 146.61 ± 71.59 | −0.871 | 0.39 |
| HDL-cholesterol (g/dL) | 52.39 ± 13.52 | 55.97 ± 10.99 | 1.533 | 0.134 |
| MetS indicators prevalence | ||||
| Elevated waist circumference | 26 (68.4) | 16 (42.1) | 0.002 | |
| Elevated fasting glucose | 10 (27.0) | 6 (16.2) | 0.219 | |
| Elevated triglycerides | 16 (44.4) | 16 (44.4) | 1 | |
| Reduced HDL-cholesterol | 9 (25.0) | 7 (19.4) | 0.688 | |
| Elevated blood pressures | 22 (57.9) | 20 (52.6) | 0.688 | |
| MetS prevalence | 0.344 | |||
| Less than 3 components | 19 (52.8) | 23 (63.9) | ||
| 3 or more components * | 17 (47.2) | 13 (36.1) | ||
| MetS score(z-score) | ||||
| Male (n = 31) | −0.61 ± 3.35 | −2.32 ± 2.55 | −3.586 | 0.001 |
| Female (n = 10) | −3.99 ± 2.05 | −5.50 ± 2.19 | −2.620 | 0.028 |
| Individual factors | ||||
| General health status d | 0.109 | |||
| Bad | 30 (78.9) | 26 (68.4) | ||
| Good | 8 (21.1) | 12 (31.6) | ||
| General self-efficacy | 29.08 ± 2.76 | 30.05 ± 2.94 | −1.81 | 0.079 |
| Stress level (1–14) | 9.08 ± 1.62 | 8.86 ± 1.67 | 0.796 | 0.431 |
| General (1–7) | 4.11 ± 0.99 | 3.86 ± 1.03 | 1.222 | 0.23 |
| Work-related (1–7) | 4.97 ± 0.90 | 5.00 ± 1.03 | −0.19 | 0.85 |
| Knowledge of MetS (0–6) | 2.56 ± 1.73 | 2.71 ± 1.27 | −0.482 | 0.632 |
| Physical activity (per week) | 0.376 | |||
| No | 14 (34.1) | 9 (22.0) | ||
| 1–2 times | 20 (48.8) | 22 (53.7) | ||
| ≥3 times | 7 (17.1) | 10 (24.4) | ||
| Sleep quantity (h) (3–10) | 0.508 | |||
| Others | 29 (78.4) | 26 (70.3) | ||
| Good sleep (7 or 8 h) | 8 (21.6) | 11 (29.7) | ||
| Diet (scores) (0–10) | 4.47 ± 1.86 | 4.42 ± 2.38 | 0.151 | 0.881 |
| Organizational factors | ||||
| Organizational commitment | 6.22 ± 0.71 | 6.14 ± 1.03 | 0.572 | 0.571 |
| Job satisfaction e | 0.581 | |||
| Not satisfied | 14 (37.8) | 17 (45.9) | ||
| Satisfied | 23 (62.2) | 20 (54.1) | ||
| Job stress | ||||
| Job demand | 57.43 ± 9.58 | 53.83 ± 10.50 | 2.053 | 0.047 |
| Insufficient job control | 56.98 ± 11.87 | 63.29 ± 13.68 | −2.6 | 0.013 |
| Inadequate social support | 62.46 ± 11.82 | 67.57 ± 16.43 | −1.667 | 0.104 |
| Job insecurity | 39.64 ± 21.28 | 42.34 ± 17.83 | −0.758 | 0.454 |
| Organizational system | 55.86 ± 12.69 | 54.95 ± 12.02 | 0.384 | 0.703 |
| Lack of rewards | 55.86 ± 12.69 | 61.56 ± 14.49 | −2.522 | 0.016 |
| Occupational climate | 34.91 ± 17.77 | 31.08 ± 12.98 | 1.432 | 0.161 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ryu, H.; Jung, J.; Cho, J.; Chin, D.L. Program Development and Effectiveness of Workplace Health Promotion Program for Preventing Metabolic Syndrome among Office Workers. Int. J. Environ. Res. Public Health 2017, 14, 878. https://doi.org/10.3390/ijerph14080878
Ryu H, Jung J, Cho J, Chin DL. Program Development and Effectiveness of Workplace Health Promotion Program for Preventing Metabolic Syndrome among Office Workers. International Journal of Environmental Research and Public Health. 2017; 14(8):878. https://doi.org/10.3390/ijerph14080878
Chicago/Turabian StyleRyu, Hosihn, Jiyeon Jung, Jeonghyun Cho, and Dal Lae Chin. 2017. "Program Development and Effectiveness of Workplace Health Promotion Program for Preventing Metabolic Syndrome among Office Workers" International Journal of Environmental Research and Public Health 14, no. 8: 878. https://doi.org/10.3390/ijerph14080878





