Is Preoperative Patient-Reported Health Status Associated with Mortality after Total Hip Replacement?
Abstract
:1. Introduction
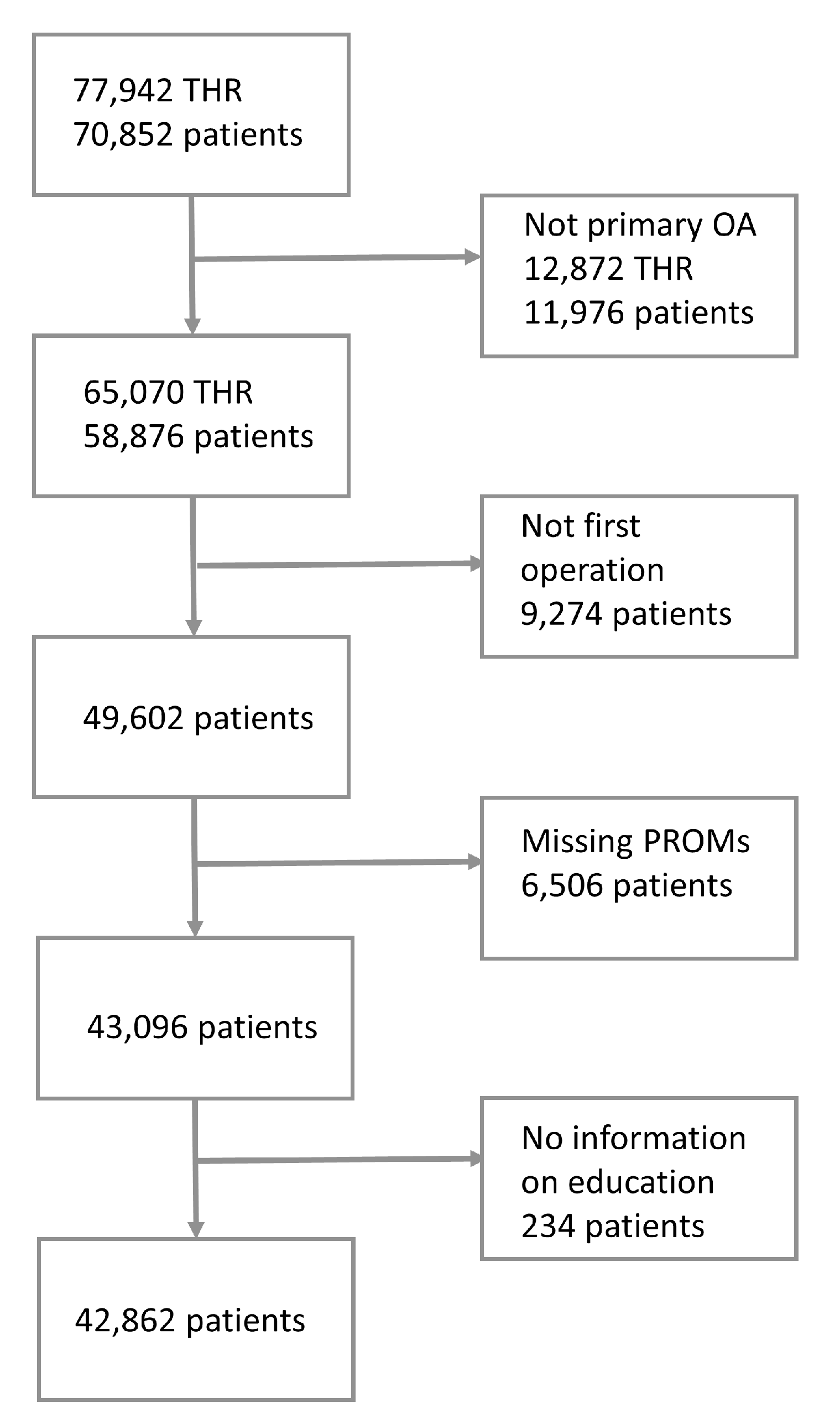
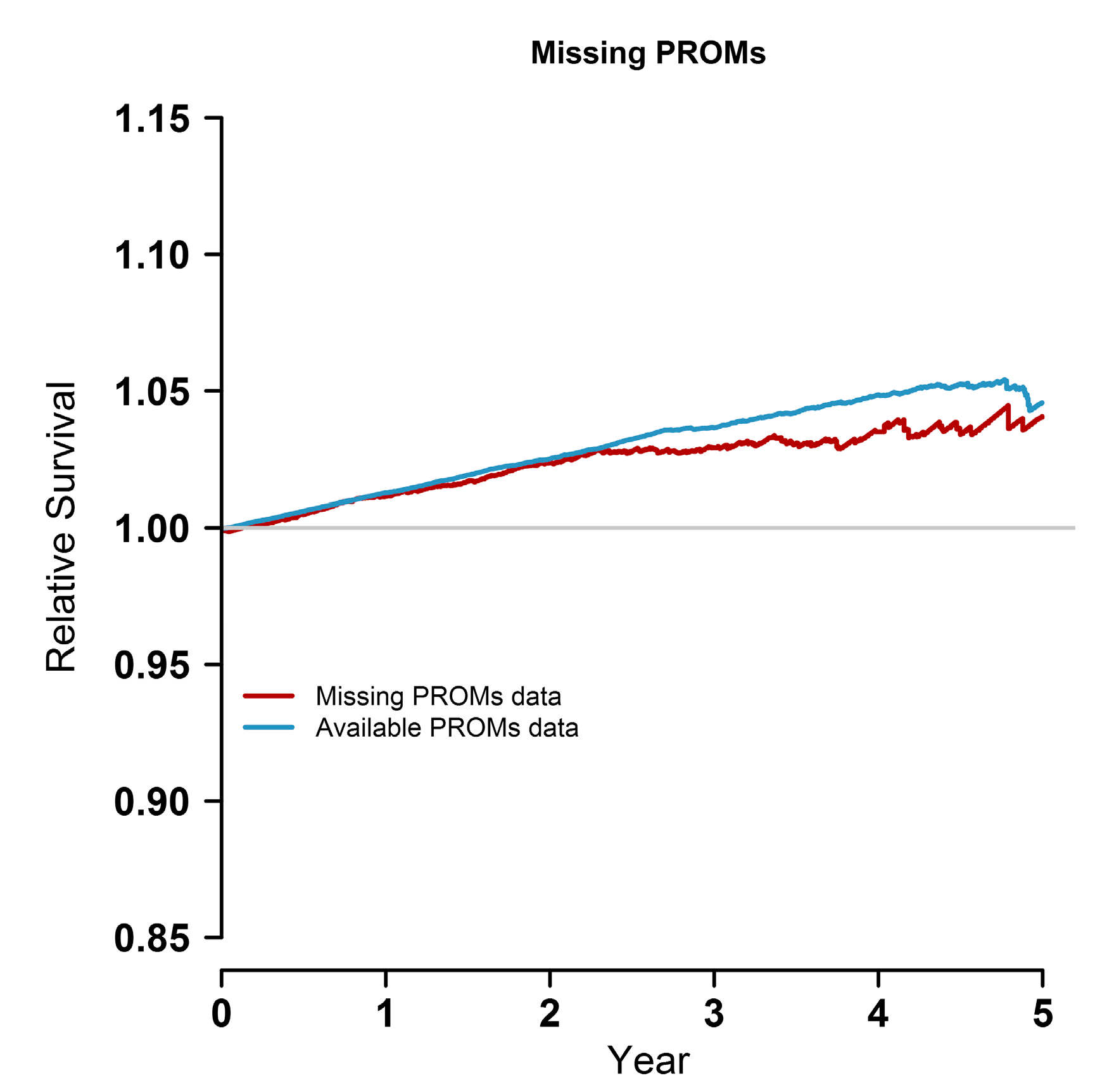
2. Materials and Methods
2.1. Data Sources, Patient Selection, and Measures
2.2. Statistical Analyses and Software
2.3. Research Ethics
2.4. Availability of Data and Materials
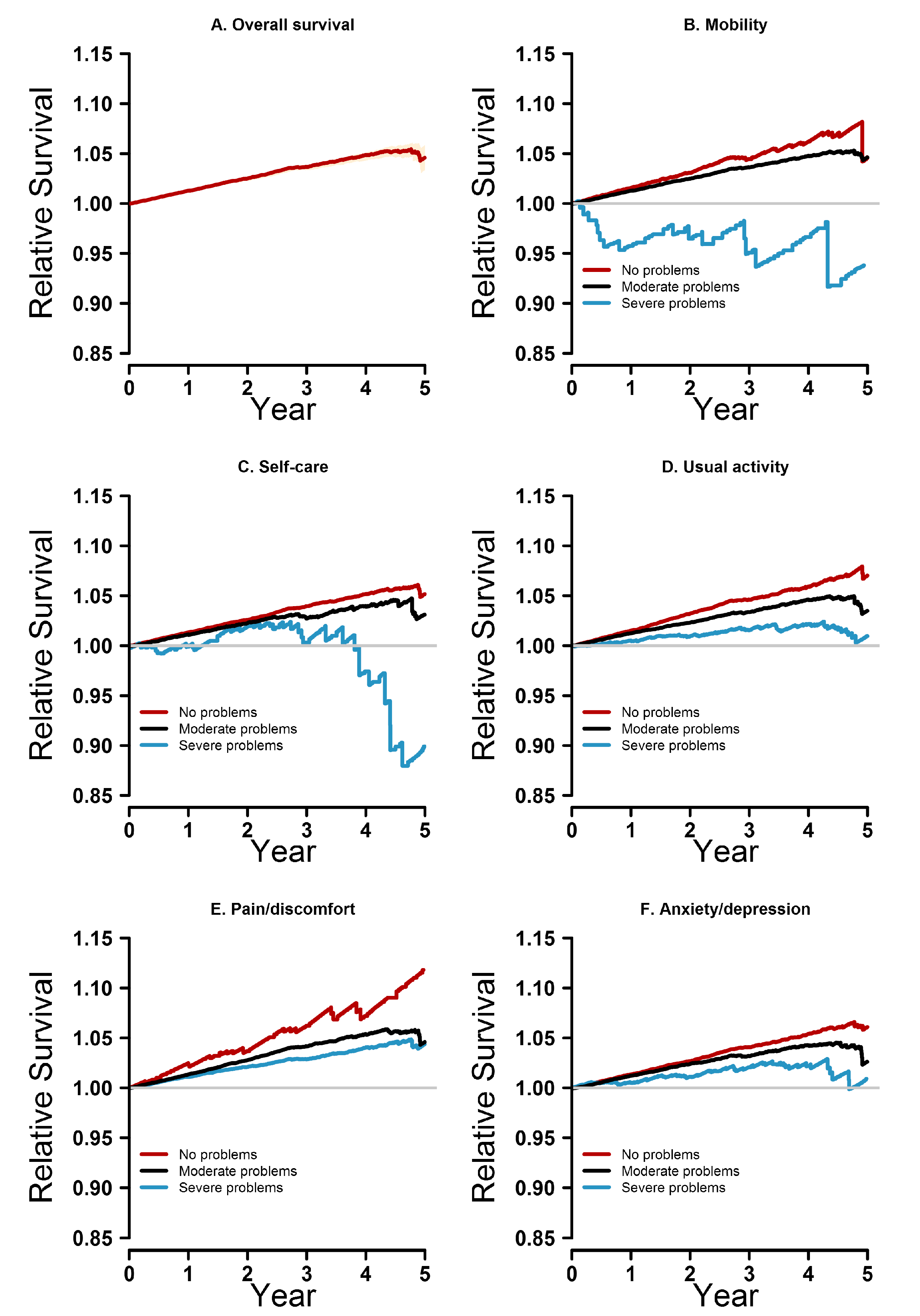
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Cross, M.; Smith, E.; Hoy, D.; Nolte, S.; Ackerman, I.; Fransen, M.; Bridgett, L.; Williams, S.; Guillemin, F.; Hill, C.L.; et al. The global burden of hip and knee osteoarthritis: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014, 73, 1323–1330. [Google Scholar] [CrossRef] [PubMed]
- Mont, M.A.; Issa, K. Updated projections of total joint arthroplasty demands in America: Commentary on an article by Steven M. Kurtz, PhD, et al.: “Impact of the economic downturn on total joint replacement demand in the united states. Updated projections to 2021”. J. Bone Jt. Surg. 2014, 96, e68.61–e68.62. [Google Scholar] [CrossRef] [PubMed]
- Nemes, S.; Gordon, M.; Rogmark, C.; Rolfson, O. Projections of total hip replacement in Sweden from 2013 to 2030. Acta Orthop. 2014, 85, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Hunt, L.P.; Ben-Shlomo, Y.; Clark, E.M.; Dieppe, P.; Judge, A.; MacGregor, A.J.; Tobias, J.H.; Vernon, K.; Blom, A.W. 90-day mortality after 409,096 total hip replacements for osteoarthritis, from the national joint registry for England and Wales: A retrospective analysis. Lancet 2013, 382, 1097–1104. [Google Scholar] [CrossRef]
- Aynardi, M.; Pulido, L.; Parvizi, J.; Sharkey, P.F.; Rothman, R.H. Early mortality after modern total hip arthroplasty. Clin. Orthop. Relat. Res. 2009, 467, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Aynardi, M.; Jacovides, C.L.; Huang, R.; Mortazavi, S.M.; Parvizi, J. Risk factors for early mortality following modern total hip arthroplasty. J. Arthroplast. 2013, 28, 517–520. [Google Scholar] [CrossRef] [PubMed]
- Lalmohamed, A.; Vestergaard, P.; De Boer, A.; Leufkens, H.G.M.; Van Staa, T.P.; De Vries, F. Changes in mortality patterns following total hip or knee arthroplasty over the past two decades: A nationwide cohort study. Arthr. Rheumatol. 2014, 66, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Berstock, J.R.; Beswick, A.D.; Lenguerrand, E.; Whitehouse, M.R.; Blom, A.W. Mortality after total hip replacement surgery: A systematic review. Bone Jt. Res. 2014, 3, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Garellick, G.; Karrbolm, J.; Lindabl, H.; Malcbau, H.; Rogmark, C.; Rolfson, O. Swedish Hip Arthroplasty Register Annual Report 2014; Registercentrum Västra Götaland: Gothenburg, Sweden, 2015. [Google Scholar]
- Singh, J.A.; Kundukulam, J.; Riddle, D.L.; Strand, V.; Tugwell, P. Early postoperative mortality following joint arthroplasty: A systematic review. J. Rheumatol. 2011, 38, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, A.B.; Baron, J.A.; Overgaard, S.; Johnsen, S.P. Short- and long-term mortality following primary total hip replacement for osteoarthritis: A Danish nationwide epidemiological study. J. Bone Jt. Surg. Ser. B 2011, 93, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Maradit Kremers, H.; Larson, D.R.; Noureldin, M.; Schleck, C.D.; Jiranek, W.A.; Berry, D.J. Long-term mortality trends after total hip and knee arthroplasties: A population-based study. J. Arthrop. 2016, 31, 1163–1169. [Google Scholar] [CrossRef] [PubMed]
- Lie, S.A.; Engesaeter, L.B.; Havelin, L.I.; Gjessing, H.K.; Vollset, S.E. Mortality after total hip replacement: 0–10-year follow-up of 39,543 patients in the Norwegian arthroplasty register. Acta Orthop. Scand. 2000, 71, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Robertsson, O.; Stefansdottir, A.; Lidgren, L.; Ranstam, J. Increased long-term mortality in patients less than 55 years old who have undergone knee replacement for osteoarthritis: Results from the Swedish knee arthroplasty register. J. Bone Jt. Surg. Br. 2007, 89, 599–603. [Google Scholar] [CrossRef] [PubMed]
- Jamsen, E.; Puolakka, T.; Eskelinen, A.; Jantti, P.; Kalliovalkama, J.; Nieminen, J.; Valvanne, J. Predictors of mortality following primary hip and knee replacement in the aged. A single-center analysis of 1998 primary hip and knee replacements for primary osteoarthritis. Acta Orthop. 2013, 84, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Burstrom, B.; Fredlund, P. Self-rated health: Is it as good a predictor of subsequent mortality among adults in lower as well as in higher social classes? J. Epidemiol. Commun. Health 2001, 55, 836–840. [Google Scholar] [CrossRef]
- Mossey, J.M.; Shapiro, E. Self-rated health: A predictor of mortality among the elderly. Am. J. Public Health 1982, 72, 800–808. [Google Scholar] [CrossRef] [PubMed]
- Jerant, A.; Tancredi, D.J.; Franks, P. Mortality prediction by quality-adjusted life year compatible health measures: Findings in a nationally representative us sample. Med. Care 2011, 49, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Pocock, S.; Bueno, H.; Licour, M.; Medina, J.; Zhang, L.; Annemans, L.; Danchin, N.; Huo, Y.; Van de Werf, F. Predictors of one-year mortality at hospital discharge after acute coronary syndromes: A new risk score from the epicor (long-term follow up of antithrombotic management patterns in acute coronary syndrome patients) study. Eur. Heart J. Acute Cardiovasc. Care 2015, 4, 509–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haddad, F.S.; Manktelow, A.R.; Skinner, J.A. Publication of surgeon level data from registers: Who benefits? Bone Jt. J. 2016, 98, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Whitehouse, S.L.; Bolland, B.J.; Howell, J.R.; Crawford, R.W.; Timperley, A.J. Mortality following hip arthroplasty—Inappropriate use of national joint registry (NJR) data. J. Arthrop. 2014, 29, 1827–1834. [Google Scholar] [CrossRef] [PubMed]
- Nelson, E.C.; Dixon-Woods, M.; Batalden, P.B.; Homa, K.; Van Citters, A.D.; Morgan, T.S.; Eftimovska, E.; Fisher, E.S.; Ovretveit, J.; Harrison, W.; et al. Patient focused registries can improve health, care, and science. BMJ 2016, 354, i3319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berry, D.J. Joint registries: What can we learn in 2016? Bone Jt. J. 2017, 99, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Rolfson, O.; Kärrholm, J.; Dahlberg, L.E.; Garellick, G. Patient-reported outcomes in the Swedish hip arthroplasty register: Results of a nationwide prospective observational study. J. Bone Jt. Surg. Br. 2011, 93, 867–875. [Google Scholar] [CrossRef] [PubMed]
- EuroQol, G. EuroQol—A new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar]
- Cnudde, P.; Rolfson, O.; Nemes, S.; Karrholm, J.; Rehnberg, C.; Rogmark, C.; Timperley, J.; Garellick, G. Linking Swedish health data registers to establish a research database and a shared decision-making tool in hip replacement. BMC Musculoskelet. Disord. 2016, 17, 414. [Google Scholar] [CrossRef] [PubMed]
- Mohaddes, M.; Garellick, G.; Karrholm, J. Method of fixation does not influence the overall risk of rerevision in first-time cup revisions. Clin. Orthop. Relat. Res. 2013, 471, 3922–3931. [Google Scholar] [CrossRef] [PubMed]
- Bülow, E.; Rolfson, O.; Cnudde, P.; Rogmark, C.; Garellick, G.; Nemes, S. Comorbidity does not predict long-term mortality after total hip arthroplasty. Acta Orthop. 2017, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Pohar Perme, M.; Stare, J.; Estève, J. On estimation in relative survival. Biometrics 2012, 68, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Statistics Sweden. The Future Population of Sweden 2012–2060; Institute, F., Ed.; SCB: Stockholm, Sweden, 2012; 220p.
- Stare, J.; Henderson, R.; Pohar, M. An individual measure of relative survival. J. R. Stat. Soc. Ser. C 2005, 54, 115–126. [Google Scholar] [CrossRef]
- Stare, J.; Pohar, M.; Henderson, R. Goodness of fit of relative survival models. Stat. Med. 2005, 24, 3911–3925. [Google Scholar] [CrossRef] [PubMed]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann. Int. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Nuesch, E.; Dieppe, P.; Reichenbach, S.; Williams, S.; Iff, S.; Juni, P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: Population based cohort study. BMJ 2011, 342, d1165. [Google Scholar] [CrossRef] [PubMed]
- Kessing, D.; Denollet, J.; Widdershoven, J.; Kupper, N. Self-care and all-cause mortality in patients with chronic heart failure. JACC Heart Fail. 2016, 4, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Buller, L.T.; Best, M.J.; Klika, A.K.; Barsoum, W.K. The influence of psychiatric comorbidity on perioperative outcomes following primary total hip and knee arthroplasty; a 17-year analysis of the national hospital discharge survey database. J. Arthrop. 2015, 30, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Stundner, O.; Kirksey, M.; Chiu, Y.L.; Mazumdar, M.; Poultsides, L.; Gerner, P.; Memtsoudis, S.G. Demographics and perioperative outcome in patients with depression and anxiety undergoing total joint arthroplasty: A population-based study. Psychosomatics 2013, 54, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Asberg, A.N.; Stovner, L.J.; Zwart, J.A.; Winsvold, B.S.; Heuch, I.; Hagen, K. Chronic musculoskeletal complaints as a predictor of mortality-the hunt study. Pain 2016, 157, 1443–1447. [Google Scholar] [CrossRef] [PubMed]
- Asberg, A.N.; Heuch, I.; Hagen, K. The mortality associated with chronic widespread musculoskeletal complaints: A systematic review of the literature. Musculoskelet. Care 2017, 15, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Bliemel, C.; Sielski, R.; Doering, B.; Dodel, R.; Balzer-Geldsetzer, M.; Ruchholtz, S.; Buecking, B. Pre-fracture quality of life predicts 1-year survival in elderly patients with hip fracture-development of a new scoring system. Osteoporos. Int. 2016, 27, 1979–1987. [Google Scholar] [CrossRef] [PubMed]
- Black, N. Patient reported outcome measures could help transform healthcare. BMJ 2013, 346. [Google Scholar] [CrossRef] [PubMed]
- Lacny, S.; Bohm, E.; Hawker, G.; Powell, J.; Marshall, D.A. Assessing the comparability of hip arthroplasty registries in order to improve the recording and monitoring of outcome. Bone Jt. J. 2016, 98, 442–451. [Google Scholar] [CrossRef] [PubMed]
- Pivec, R.; Johnson, A.J.; Mears, S.C.; Mont, M.A. Hip arthroplasty. Lancet 2012, 380, 1768–1777. [Google Scholar] [CrossRef]
- Graves, S.E. The value of arthroplasty registry data. Acta Orthop. 2010, 81, 8–9. [Google Scholar] [CrossRef] [PubMed]
- Cobb, J. Arthroplasty registries, patient safety and outlier surgeons: The case for change. Acta Orthop. Belg. 2015, 81, 594–599. [Google Scholar] [PubMed]
- Varagunam, M.; Hutchings, A.; Black, N. Do patient-reported outcomes offer a more sensitive method for comparing the outcomes of consultants than mortality? A multilevel analysis of routine data. BMJ Qual. Saf. 2015, 24, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Greene, M.E.; Rolfson, O.; Garellick, G.; Gordon, M.; Nemes, S. Improved statistical analysis of pre- and post-treatment patient-reported outcome measures (PROMs): The applicability of piecewise linear regression splines. Qual. Life Res. 2015, 24, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Nemes, S.; Rolfson, O.; Garellick, G. Development and validation of a shared decision—Making instrument for health—Related quality of life one year after total hip replacement based on quality registries data. J. Eval. Clin. Pract. 2016. [Google Scholar] [CrossRef] [PubMed]
- Jansson, K.A.; Granath, F. Health-related quality of life (EQ-5D) before and after orthopedic surgery. Acta Orthop. 2011, 82, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Fryar, C. Clarifying the Montgomery judgment. BMJ 2015, 350, h2217. [Google Scholar] [CrossRef] [PubMed]
- Greene, M.E.; Rader, K.A.; Garellick, G.; Malchau, H.; Freiberg, A.A.; Rolfson, O. The EQ-5D-5L improves on the EQ-5D-3L for health-related quality-of-life assessment in patients undergoing total hip arthroplasty. Clin. Orthop. Relat. Res. 2015, 473, 3383–3390. [Google Scholar] [CrossRef] [PubMed]
| Alive | Dead | p-Value | ||
|---|---|---|---|---|
| n = 41,516 | n = 1346 | |||
| Mobility (%) | No problems | 3210 (7.7) | 52 (3.9) | <0.001 |
| Moderate problems | 38,190 (92.0) | 1279 (95.0) | ||
| Severe problems | 116 (0.3) | 15 (1.1) | ||
| Self-care (%) | No problems | 32,066 (77.2) | 910 (67.6) | <0.001 |
| Moderate problems | 9102 (21.9) | 403 (29.9) | ||
| Severe problems | 348 (0.8) | 33 (2.5) | ||
| Usual activities (%) | No problems | 16,086 (38.7) | 460 (34.2) | <0.001 |
| Moderate problems | 21,125 (50.9) | 684 (50.8) | ||
| Severe problems | 4305 (10.4) | 202 (15.0) | ||
| Pain/discomfort (%) | No problems | 631 (1.5) | 16 (1.2) | <0.001 |
| Moderate problems | 23,822 (57.4) | 706 (52.5) | ||
| Severe problems | 17,063 (41.1) | 624 (46.4) | ||
| Anxiety/depression (%) | No problems | 23,963 (57.7) | 711 (52.8) | <0.001 |
| Moderate problems | 16,079 (38.7) | 568 (42.2) | ||
| Severe problems | 1474 (3.6) | 67 (5.0) | ||
| EQ VAS score (SD) | 54.77 (22.17) | 50.61 (21.76) | <0.001 | |
| Pain VAS score (SD) | 62.39 (15.91) | 62.67 (17.34) | 0.53 | |
| Females (%) | 23,358 (56.3) | 633 (47.0) | <0.001 | |
| Age (SD) | 67.70 (10.09) | 75.76 (8.83) | <0.001 | |
| Educational level (%) | low | 14,018 (33.8) | 658 (48.9) | <0.001 |
| middle | 17,038 (41.0) | 466 (34.6) | ||
| high | 10,460 (25.2) | 222 (16.5) | ||
| Hospital (%) | University | 3018 (7.3) | 117 (8.7) | <0.001 |
| County | 13,026 (31.4) | 464 (34.5) | ||
| Rural | 17,490 (42.1) | 603 (44.8) | ||
| Private | 7982 (19.2) | 162 (12.0) | ||
| Fixation (%) | Cemented | 28,237 (68.4) | 1168 (87.0) | <0.001 |
| Uncemented | 6363 (15.4) | 58 (4.3) | ||
| Hybrid | 536 (1.3) | 12 (0.9) | ||
| Reverse hybrid | 5503 (13.3) | 102 (7.6) | ||
| Resurfacing | 639 (1.5) | 2 (0.1) | ||
| HR | 95% CI | ||
|---|---|---|---|
| Mobility | No problems | ref | |
| Moderate problems | 1.46 | 1.09–1.96 | |
| Severe problems | 2.65 | 1.43–4.92 | |
| Self-care | No problems | ref | |
| Moderate problems | 1.15 | 1.01–1.31 | |
| Severe problems | 1.57 | 1.08–2.29 | |
| Usual activity | No problems | ref | |
| Moderate problems | 1.05 | 0.93–1.20 | |
| Severe problems | 1.28 | 1.06–1.56 | |
| Pain/discomfort | No problems | ref | |
| Moderate problems | 1.07 | 0.64–1.77 | |
| Severe problems | 1.20 | 0.71–2.00 | |
| Anxiety/depression | No problems | ref | |
| Moderate problems | 1.09 | 0.96–1.22 | |
| Severe problems | 1.24 | 0.95–1.62 | |
| EQ VAS (in units of 10) | 0.95 | 0.92–0.98 | |
| Pain VAS (in units of 10) | 0.96 | 0.92–1.01 | |
| Sex | Male | ref | |
| Female | 0.86 | 0.76–0.96 | |
| Age | 0.96 | 0.95–0.97 | |
| Operation Year | 0.91 | 0.86–0.96 | |
| Education | Low | ref | |
| Middle | 0.93 | 0.83–1.06 | |
| High | 0.85 | 0.73–1.01 | |
| Hospital | University | ref | |
| County | 0.79 | 0.65–0.97 | |
| Rural | 0.82 | 0.67–1.00 | |
| Private | 0.72 | 0.56–0.91 | |
| Fixation | Cemented | ref | |
| Uncemented | 0.60 | 0.45–0.81 | |
| Hybrid | 0.80 | 0.45–1.43 | |
| Reverse hybrid | 0.94 | 0.76–1.16 | |
| Resurfacing | 0.20 | 0.05–0.84 | |
| Missing PROMs | Available PROMs | p-Value | ||
|---|---|---|---|---|
| n = 6506 | n = 43,096 | |||
| Females (%) | 3676 (56.5) | 24,139 (56.0) | 0.466 | |
| Age (SD) | 68.59 (11.16) | 67.97 (10.16) | <0.001 | |
| Educational level (%) | Low | 2407 (37.0) | 14,676 (34.1) | <0.001 |
| Middle | 2557 (39.3) | 17,504 (40.6) | ||
| High | 1453 (22.3) | 10,682 (24.8) | ||
| Missing | 89 (1.4) | 234 (0.5) | ||
| Hospital (%) | University | 687 (10.6) | 3154 (7.3) | <0.001 |
| County | 2288 (35.2) | 13,571 (31.5) | ||
| Rural | 2239 (34.4) | 18,194 (42.2) | ||
| Private | 1292 (19.9) | 8177 (19.0) | ||
| Fixation (%) | Cemented | 4226 (65.0) | 29,594 (68.7) | <0.001 |
| Uncemented | 1099 (16.9) | 6451 (15.0) | ||
| Hybrid | 107 (1.6) | 551 (1.3) | ||
| Reverse hybrid | 883 (13.6) | 5627 (13.1) | ||
| Resurfacing | 83 (1.3) | 643 (1.5) | ||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cnudde, P.; Nemes, S.; Mohaddes, M.; Timperley, J.; Garellick, G.; Burström, K.; Rolfson, O. Is Preoperative Patient-Reported Health Status Associated with Mortality after Total Hip Replacement? Int. J. Environ. Res. Public Health 2017, 14, 899. https://doi.org/10.3390/ijerph14080899
Cnudde P, Nemes S, Mohaddes M, Timperley J, Garellick G, Burström K, Rolfson O. Is Preoperative Patient-Reported Health Status Associated with Mortality after Total Hip Replacement? International Journal of Environmental Research and Public Health. 2017; 14(8):899. https://doi.org/10.3390/ijerph14080899
Chicago/Turabian StyleCnudde, Peter, Szilard Nemes, Maziar Mohaddes, John Timperley, Göran Garellick, Kristina Burström, and Ola Rolfson. 2017. "Is Preoperative Patient-Reported Health Status Associated with Mortality after Total Hip Replacement?" International Journal of Environmental Research and Public Health 14, no. 8: 899. https://doi.org/10.3390/ijerph14080899






