How Does Counselling in a Stationary Health Care Setting Affect the Attendance in a Standardised Sports Club Programme? Process Evaluation of a Quasi-Experimental Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Overview
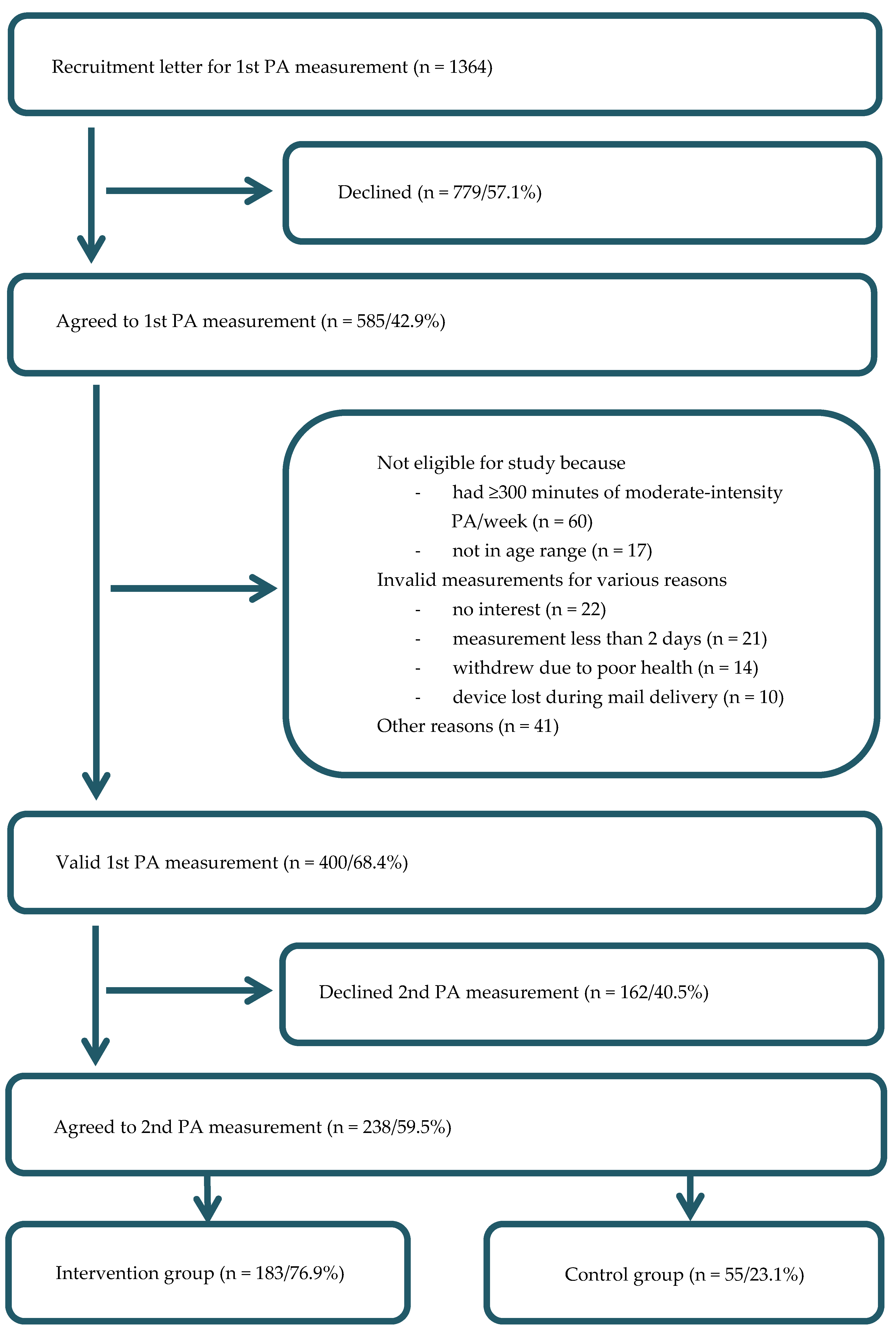
2.2. Recruitment of the Health Resorts and Participants
2.3. Intervention in the Health Resorts
2.4. Intervention in the Sports Clubs
2.5. Measurements
2.6. Statistical Analysis
3. Results
3.1. Health Resorts
3.2. Study Participants
3.3. Attendance Levels
3.4. Intervention Implementation
3.4.1. Health Resorts
3.4.2. Sports Clubs
3.5. Practicability of the Project
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Bamia, C.; Orfanos, P.; Juerges, H.; Schöttker, B.; Brenner, H.; Lorbeer, R.; Aadahl, M.; Matthews, C.E.; Klinaki, E.; Katsoulis, M.; et al. Self-rated health and all-cause and cause-specific mortality of older adults: Individual data meta-analysis of prospective cohort studies in the CHANCES Consortium. Maturitas 2017, 103, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.-M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Shortreed, S.M.; Peeters, A.; Forbes, A.B. Estimating the effect of long-term physical activity on cardiovascular disease and mortality: Evidence from the Framingham Heart Study. Heart 2013, 99, 649–654. [Google Scholar] [CrossRef] [PubMed]
- WHO (World Health Organization). Global Recommendations on Physical Activity for Health. Available online: http://www.who.int/dietphysicalactivity/factsheet_recommendations/en/ (accessed on 7 November 2017).
- Statistik Austria. Gesundheitsdeterminanten: Körperliche Aktivität in der Freizeit. Available online: http://www.statistik.at/web_de/statistiken/menschen_und_gesellschaft/gesundheit/gesundheitsdeterminanten/koerperliche_aktivitaet/index.html (accessed on 27 October 2017).
- Bull, F.C.; Gauvin, L.; Bauman, A.; Shilton, T.; Kohl, H.W.; Salmon, A. The Toronto charter for physical activity: A global call for action. J. Phys. Act. Health 2010, 7, 421–422. [Google Scholar] [CrossRef] [PubMed]
- Grossman, D.C.; Bibbins-Domingo, K.; Curry, S.J.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; Krist, A.H.; Kurth, A.E.; et al. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults without cardiovascular risk factors: U.S. Preventive Services Task Force recommendation statement. JAMA 2017, 318, 167–174. [Google Scholar] [PubMed]
- Bundesministerium für Frauen und Gesundheit. Öffentliches Gesundheitsportal Österreichs: Kuraufenthalt. Available online: https://www.gesundheit.gv.at/gesundheitssystem/leistungen/antraege/kurantrag (accessed on 3 November 2017).
- Statistik Styria. Email-Communication: Styrian Population in 2015. Available online: http://www.statistik.steiermark.at/cms/ziel/103034729/DE (accessed on 12 January 2018).
- Pensionsversicherungsanstalt. Pensionsversicherungsanstalt: Jahresbericht 2015. Available online: http://www.pensionsversicherung.at/cdscontent/load?contentid=10008.631742&version=1467614813 (accessed on 7 November 2017).
- Hawley-Hague, H.; Horne, M.; Skelton, D.A.; Todd, C. Review of how we should define (and measure) adherence in studies examining older adults’ participation in exercise classes. BMJ Open 2016, 6, e011560. [Google Scholar] [CrossRef] [PubMed]
- Visek, A.J.; Olson, E.A.; DiPietro, L. Factors predicting adherence to 9 months of supervised exercise in healthy older women. J. Phys. Act. Health 2011, 8, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Withall, J.; Jago, R.; Fox, K.R. The effect a of community-based social marketing campaign on recruitment and retention of low-income groups into physical activity programmes—A controlled before-and-after study. BMC Public Health 2012, 12, 836. [Google Scholar] [CrossRef] [PubMed]
- Zwarenstein, M.; Treweek, S.; Gagnier, J.J.; Altman, D.G.; Tunis, S.; Haynes, B.; Oxman, A.D.; Moher, D. Improving the reporting of pragmatic trials: An extension of the CONSORT statement. BMJ 2008, 337, a2390. [Google Scholar] [CrossRef] [PubMed]
- Loudon, K.; Zwarenstein, M.; Sullivan, F.M.; Donnan, P.T.; Gágyor, I.; Hobbelen, H.J.S.M.; Althabe, F.; Krishnan, J.A.; Treweek, S. The PRECIS-2 tool has good interrater reliability and modest discriminant validity. J Clin. Epidemiol. 2017, 88, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Zwarenstein, M.; Treweek, S.; Loudon, K. PRECIS-2 helps researchers design more applicable RCTs while CONSORT extension for pragmatic trials helps knowledge users decide whether to apply them. J. Clin. Epidemiol. 2017, 84, 27–29. [Google Scholar] [CrossRef] [PubMed]
- Loudon, K.; Treweek, S.; Sullivan, F.; Donnan, P.; Thorpe, K.E.; Zwarenstein, M. The PRECIS-2 tool: Designing trials that are fit for purpose. BMJ 2015, 350, h2147. [Google Scholar] [CrossRef] [PubMed]
- Lackinger, C.; Wilfinger, J.; Mayerhofer, J.; Strehn, A.; Dick, D.; Dorner, T.E. Adherence to and effects on physical function parameters of a community-based standardised exercise programme for overweight or obese patients carried out by local sports clubs. Public Health 2017, 147, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lackinger, C.; Strehn, A.; Dorner, T.E.; Niebauer, J.; Titze, S. Health resorts as gateways for regional, standardised, sports club based exercise programmes to increase the weekly time of moderate- to vigorous-intensity physical activity: Study protocol. BMC Public Health 2015, 15, 1265. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel—A Guide to Designing Interventions, 2nd ed.; Silverback Publishing: Great Britain, UK, 2014. [Google Scholar]
- Fonds Gesundes Österreich. Bewegung. Gesundheit für Alle; Fonds Gesundes Österreich: Wien, Austria, 2016; Available online: http://www.fgoe.org/presse-publikationen/downloads/broschueren-folder/bewegungsbroschure/2017-01-25.9068665598 (accessed on 27 October 2017).
- Sozialversicherungsanstalt der Gewerblichen Wirtschaft. JACKPOT: Manual Fuer Die JACKPOT-Bewegungseinheiten. Available online: http://jackpot.fit/data/jackpot_stundenbilder.pdf (accessed on 18 October 2017).
- Pavey, T.; Taylor, A.; Hillsdon, M.; Fox, K.; Campbell, J.; Foster, C.; Moxham, T.; Mutrie, N.; Searle, J.; Taylor, R. Levels and predictors of exercise referral scheme uptake and adherence: A systematic review. JECH 2012, 66, 737–744. [Google Scholar] [CrossRef] [PubMed]
- Waterman, M.R.; Wiecha, J.M.; Manne, J.; Tringale, S.M.; Costa, E.; Wiecha, J.L. Utilization of a free fitness center-based exercise referral program among women with chronic disease risk factors. J. Community Health 2014, 39, 1179–1185. [Google Scholar] [CrossRef] [PubMed]
- Toobert, D.J.; Strycker, L.A.; Glasgow, R.E.; Bagdade, J.D. If you build it, will they come? Patient Educ. Couns. 2002, 48, 99–105. [Google Scholar] [CrossRef]
- Hunt, K.; Wyke, S.; Gray, C.M.; Anderson, A.S.; Brady, A.; Bunn, C.; Donnan, P.T.; Fenwick, E.; Grieve, E.; Leishman, J.; et al. A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): A pragmatic randomised controlled trial. Lancet 2014, 383, 1211–1221. [Google Scholar] [CrossRef]
- Williams, N.H.; Hendry, M.; France, B.; Lewis, R.; Wilkinson, C. Effectiveness of exercise-referral schemes to promote physical activity in adults: Systematic review. Br. J. Gen. Pract. 2007, 57, 979–986. [Google Scholar] [CrossRef] [PubMed]
- Kelly, S.; Martin, S.; Kuhn, I.; Cowan, A.; Brayne, C.; Lafortune, L. Barriers and facilitators to the uptake and maintenance of healthy behaviours by people at mid-life: A rapid systematic review. PLoS ONE 2016, 11, e0145074. [Google Scholar] [CrossRef] [PubMed]
- Canuto, K.J.; Spagnoletti, B.; McDermott, R.A.; Cargo, M. Factors influencing attendance in a structured physical activity program for aboriginal and Torres Strait Islander women in an urban setting: A mixed methods process evaluation. Int. J. Equity Health 2013, 12, 11. [Google Scholar] [CrossRef] [PubMed]
- Arsenijevic, J.; Groot, W. Physical activity on prescription schemes (PARS): Do programme characteristics influence effectiveness? Results of a systematic review and meta-analyses. BMJ Open 2017, 7, e012156. [Google Scholar] [CrossRef] [PubMed]
| Participants’ Characteristics | Total (238) | IG (n = 183) | CG (n = 55) |
|---|---|---|---|
| Sex (%) | |||
| Women | 118 (49.6) | 88 (48.1) | 30 (54.5) |
| Men | 120 (50.4) | 95 (51.9) | 25 (45.5) |
| Age in years (median and Q25; Q75) | 53.0 (49.0; 57.0) | 53.0 (48.0; 56.0) | 54.0 (50.0; 59.0) |
| Missing | 1 | ||
| Education (%) | |||
| ≤Completed apprenticeship | 128 (54.5) | 96 (53.3) | 32 (58.2) |
| ≥Intermed. voc. degree | 107 (45.5) | 84 (46.7) | 23 (41.8) |
| Missing | 3 | ||
| BMI (median and Q25; Q75) | 26.2 (24.0; 29.7) | 26.1 (24.0; 29.7) | 26.2 (24.3; 29.7) |
| Missing | 6 | ||
| Self-reported fitness level 1 (%) | |||
| ≥Fitter | 86 (37.6) | 67 (38.5) | 19 (34.5) |
| Equally fit | 93 (40.6) | 69 (39.7) | 24 (43.6) |
| ≤Less fit | 50 (21.8) | 38 (21.8) | 12 (21.8) |
| Missing | 9 |
| Attended Sessions | n | n (Grouped) | % |
|---|---|---|---|
| 1 session | 9 | 23 | 25.6 |
| 2 sessions | 5 | ||
| 3 sessions | 2 | ||
| 4 sessions | 7 | ||
| 5 sessions | 6 | 18 | 20.0 |
| 6 sessions | 2 | ||
| 7 sessions | 3 | ||
| 8 sessions | 7 | ||
| 9 sessions | 6 | 49 | 54.4 |
| 10 sessions | 3 | ||
| 11 sessions | 3 | ||
| 12 sessions | 37 |
| Stated Reasons | n | % |
|---|---|---|
| Lack of time | 6 | 37.5 |
| Poor health status of the participant | 5 | 31.3 |
| Prefers to continue on his/her own | 2 | 12.5 |
| Location too far away | 1 | 6.3 |
| Training too exhausting | 1 | 6.3 |
| Training not intensive enough | 1 | 6.3 |
| Domain | Score | Rationale |
|---|---|---|
| Eligibility criteria | 5 | All health resort patients from 11 regions in the state of Styria between 30 to 65 years were eligible. However, those meeting ≥300 min of moderate-intensity PA were excluded from the study. |
| Recruitment path | 4 | Health insurance companies sent an invitation letter as part of their routine communication and offered the PA measurement. |
| Setting | 5 | Health resorts which agreed to join the project did not differ from the health resorts which did not respond to the invitation or agreed to participate later. Therefore, the setting in our study is identical to the usual health resort setting. The JACKPOT programme takes place in already existing sports clubs. No additional equipment is needed. |
| Organisation of intervention | 3 | Health resort: The PA counselling as well as the delivery of the starter package were additional and new tasks for the health resort staff. Otherwise, no more staff and no additional training were required. |
| 3 | Sports club: Exercise instructors who already worked in the sports clubs were recruited. The additional 2-day training for JACKPOT instructors and the first 12 sessions were funded. | |
| Flexibility of experimental intervention: delivery | 5 | Health resorts: A framework for the content existed, but when, where, and by whom the intervention was delivered was flexible. Sports club session: The framework for each JACKPOT session was standardised and a manual with 12 lectures was delivered. However, instructors could adapt the content as long as they stuck to the framework. |
| Flexibility of experimental intervention: attendance | 5 | JACKPOT instructors actively encouraged participants to regularly attend JACKPOT sessions. Participants were not excluded based on their attendance level. However, the 12 sessions were only free for the first five months. |
| Follow-up | PO = 1 | Primary Outcome: Delivery of the accelerometer devices was expensive and time consuming. |
| SO = 3 | Secondary Outcome: Participants’ attendance was recorded by attendance lists which are part of the instructors’ routine. In addition, we asked instructors to make notes about reasons for their drop-out and from which health resorts the participants came. To obtain the attendance lists from instructors required additional effort. | |
| Relevance of primary and secondary outcome | PO = 5 | Primary Outcome: Regular PA is an important outcome for the participants because regular PA reduces the risks of many non-communicable diseases. |
| SO = 5 | Secondary Outcome: Only if people continue with the newly adopted PA behaviour they will derive health benefits. Therefore, it is important to assess the success of the implementation, the recruitment of participants and the attendance level of the programme. | |
| Analysis | PO = 1 | Primary Outcome: Because of the three measurements, careful screening of the data and complex analyses to ensure the validity of the results will be required. |
| SO = 4 | Secondary Outcome: No special programmes or statistical skills, but regular records are required. |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Titze, S.; Lackinger, C.; Grossschaedl, L.; Strehn, A.; Dorner, T.E.; Niebauer, J.; Schebesch-Ruf, W. How Does Counselling in a Stationary Health Care Setting Affect the Attendance in a Standardised Sports Club Programme? Process Evaluation of a Quasi-Experimental Study. Int. J. Environ. Res. Public Health 2018, 15, 134. https://doi.org/10.3390/ijerph15010134
Titze S, Lackinger C, Grossschaedl L, Strehn A, Dorner TE, Niebauer J, Schebesch-Ruf W. How Does Counselling in a Stationary Health Care Setting Affect the Attendance in a Standardised Sports Club Programme? Process Evaluation of a Quasi-Experimental Study. International Journal of Environmental Research and Public Health. 2018; 15(1):134. https://doi.org/10.3390/ijerph15010134
Chicago/Turabian StyleTitze, Sylvia, Christian Lackinger, Lena Grossschaedl, Albert Strehn, Thomas E. Dorner, Josef Niebauer, and Wolfgang Schebesch-Ruf. 2018. "How Does Counselling in a Stationary Health Care Setting Affect the Attendance in a Standardised Sports Club Programme? Process Evaluation of a Quasi-Experimental Study" International Journal of Environmental Research and Public Health 15, no. 1: 134. https://doi.org/10.3390/ijerph15010134






