Care Model Design for E-Health: Integration of Point-of-Care Testing at Dutch General Practices
Abstract
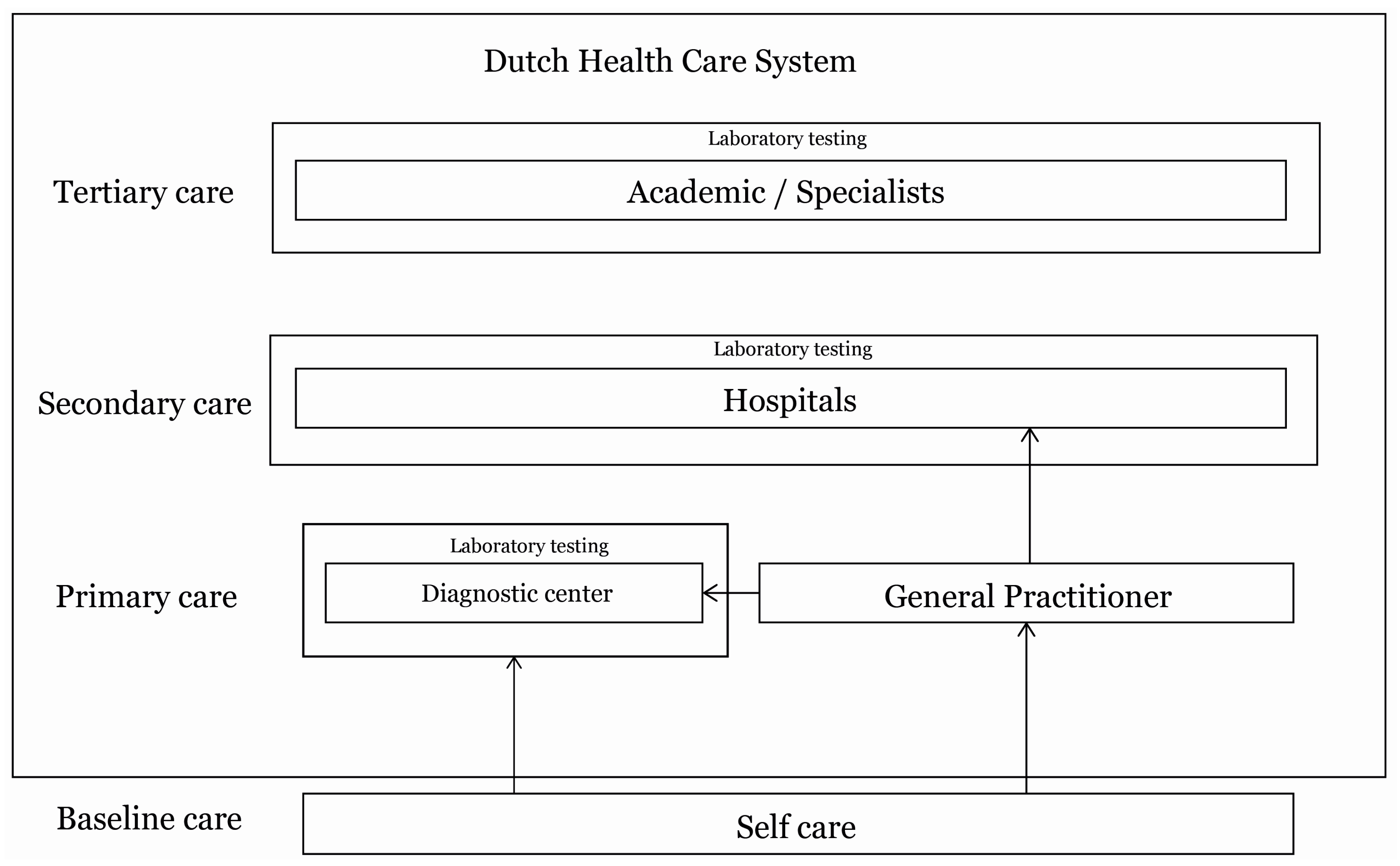
:1. Introduction
1.1. Impact Effects
1.2. Advantages and Barriers of Transformations
1.3. Integrated Care Challenge with Connectivity and eHealth
2. Materials and Methods
2.1. Business Model Parameters
2.2. Preliminary Research—Crafting the Design Model Toolkit
2.3. Design Research
2.4. Data Analysis
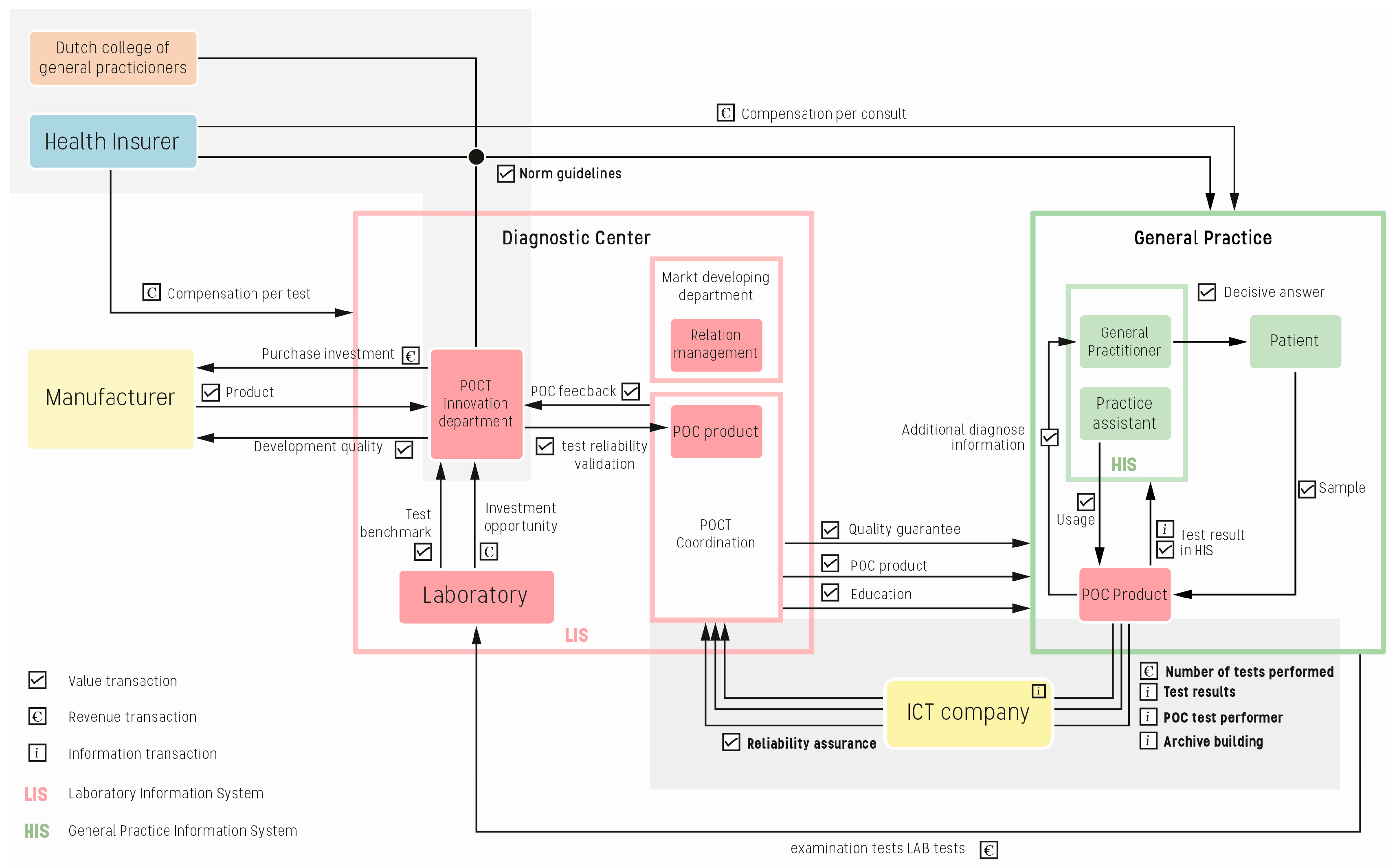
2.5. Designing the Care Model
3. Results
3.1. Findings from GPs That Influence Integration of POCT
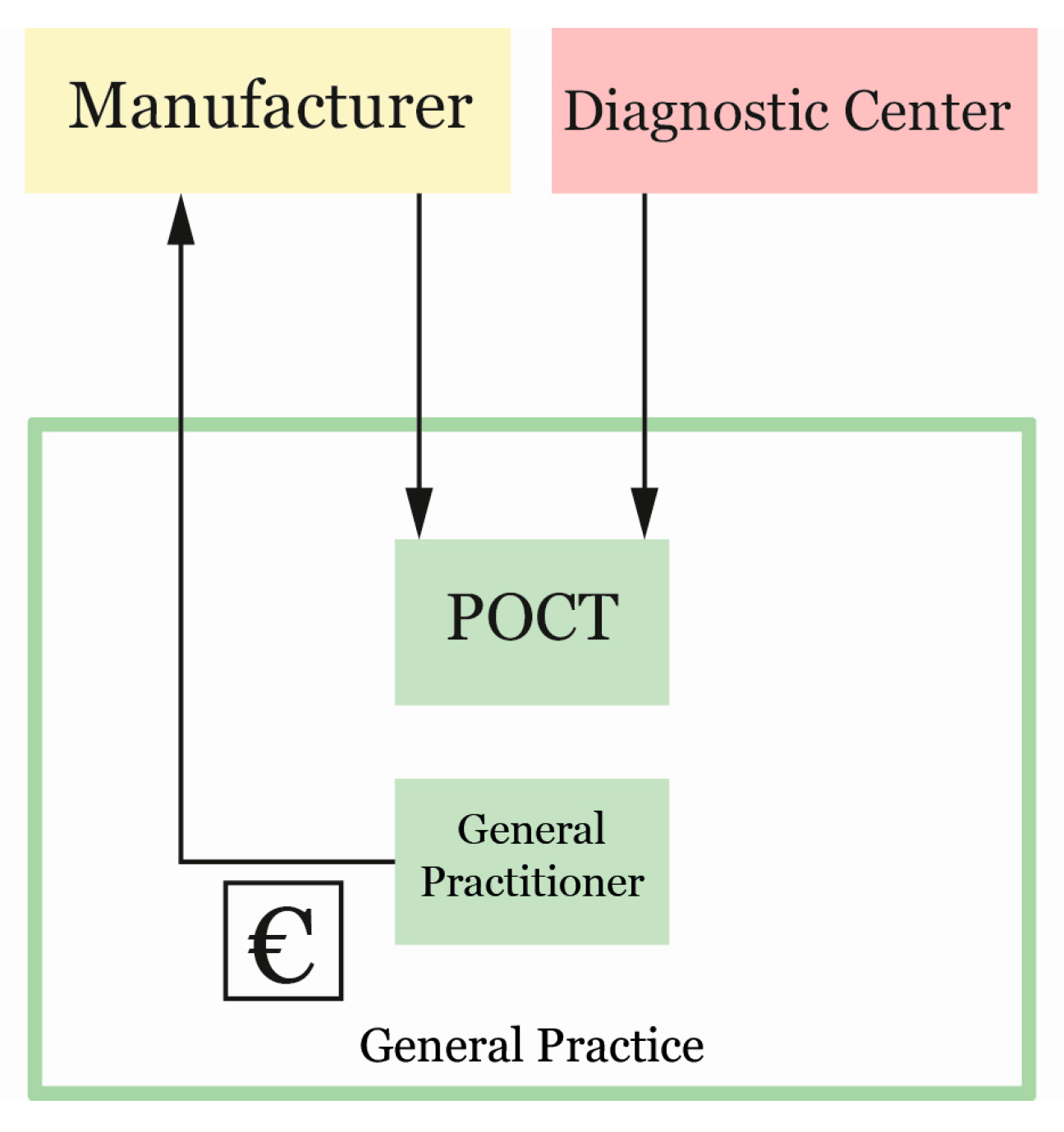
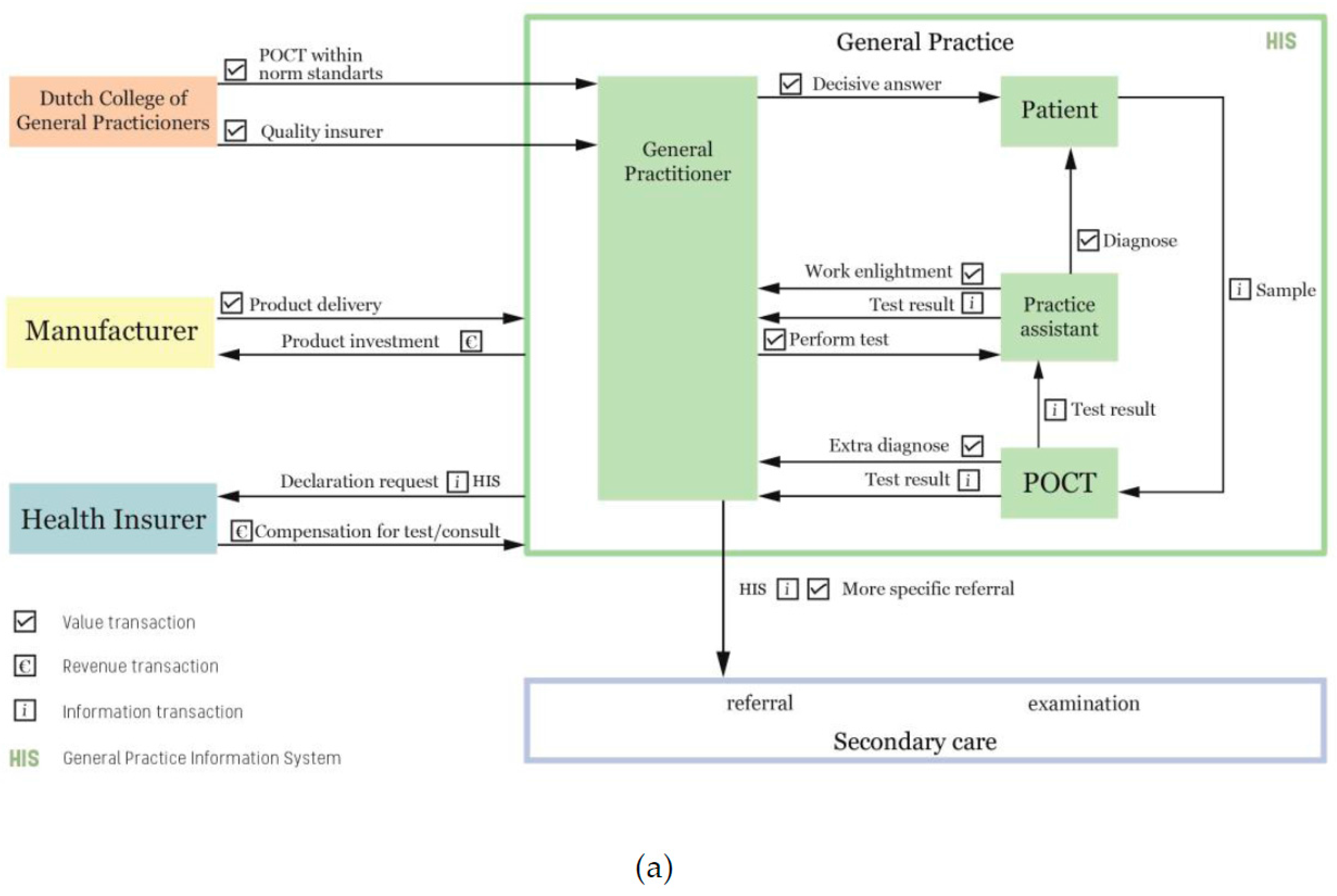
3.2. Point-of-Care Business Models of a General Practice (1)
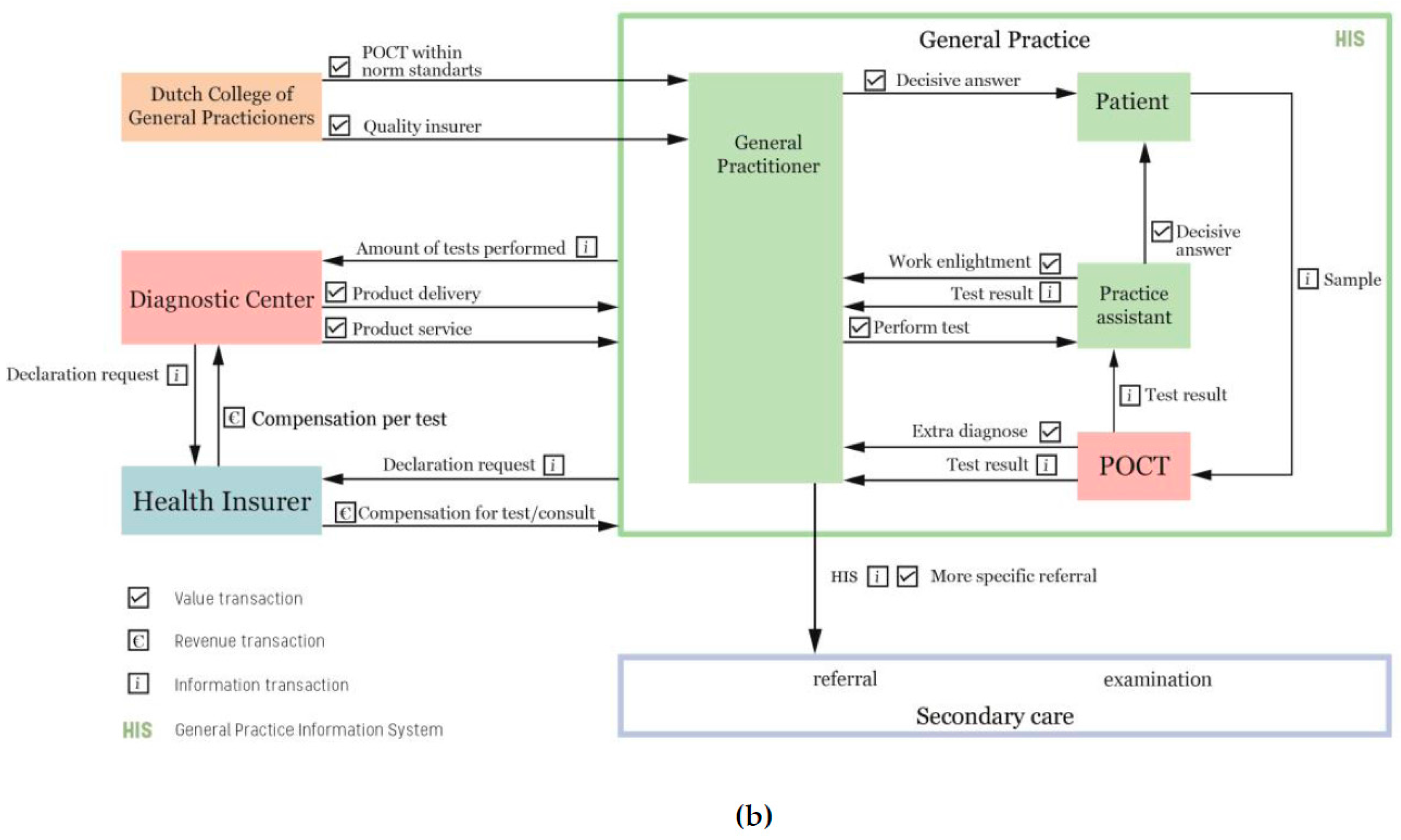
3.3. An Optimized Business Model to Integrate Point-of-Care Testing within the General Practice (2)
4. Discussion
4.1. Limitations and Further Research
4.2. Professional Implications
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Wagar, E.A.; Yasin, B.; Yuan, S. Point-of-care testing: Twenty years’ experience. Lab. Med. 2008, 39, 560–563. [Google Scholar] [CrossRef]
- Rossi, A.F.; Khan, D. Point of care testing: Improving pediatric outcomes. Clin. Biochem. 2004, 37, 456–461. [Google Scholar] [CrossRef] [PubMed]
- Price, C.P. Point of care testing. Br. Med. J. 2001, 322, 1285. [Google Scholar] [CrossRef]
- Bissell, M.; Sanfilippo, F. Empowering patients with point-of-care testing. Trends Biotechnol. 2002, 20, 269–270. [Google Scholar] [CrossRef]
- Luppa, P.B.; Müller, C.; Schlichtiger, A.; Schlebusch, H. Point-of-care testing (POCT): Current techniques and future perspectives. Trends Anal. Chem. 2011, 30, 887–898. [Google Scholar] [CrossRef]
- Kuehn, B.M. More than one-third of U.S. individuals use the internet to self-diagnose. JAMA 2013, 309, 756–757. [Google Scholar] [CrossRef] [PubMed]
- McMullan, M. Patients using the internet to obtain health information: How this affects the patient–health professional relationship. Patient Educ. Couns. 2006, 63, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Swan, M. Emerging patient-driven health care models: An examination of health social networks, consumer personalized medicine and quantified self-tracking. Int. J. Environ. Res. Public Health 2009, 6, 492–525. [Google Scholar] [CrossRef] [PubMed]
- Tatnall, A. Actor-network theory in information systems research. In Encyclopedia of Information Science and Technology, 1st ed.; IGI Global: Hershey, PA, USA, 2005; pp. 42–46. [Google Scholar]
- Gubala, V.; Harris, L.F.; Ricco, A.J.; Tan, M.X.; Williams, D.E. Point of care diagnostics: Status and future. Anal. Chem. 2011, 84, 487–515. [Google Scholar] [CrossRef] [PubMed]
- O’kane, M.J. Point of care testing—Current and emerging quality perspectives. Point Care 2014, 13, 1–5. [Google Scholar] [CrossRef]
- Drenck, N.-E. Point of care testing in Critical Care Medicine: The clinicia’s view. Clin. Chim. Acta 2001, 307, 3–7. [Google Scholar] [CrossRef]
- Gialamas, A.; Yelland, L.N.; Ryan, P.; Willson, K.; Laurence, C.O.; Bubner, T.K.; Tideman, P.; Beilby, J.J. Does point-of-care testing lead to the same or better adherence to medication? A randomised controlled trial: The PoCT in General Practice Trial. Med. J. Aust. 2009, 191, 487. [Google Scholar] [PubMed]
- Laurence, C.O.; Gialamas, A.; Bubner, T.; Yelland, L.; Willson, K.; Ryan, P.; Beilby, J.; Point of Care Testing in General Practice Trial Management Group. Patient satisfaction with point-of-care testing in general practice. Br. J. Gen. Pract. 2010, 60, e98–e104. [Google Scholar] [CrossRef] [PubMed]
- Jani, I.V.; Peter, T.F. How point-of-care testing could drive innovation in global health. N. Engl. J. Med. 2013, 368, 2319–2324. [Google Scholar] [CrossRef] [PubMed]
- Ha, J.F.; Longnecker, N. Doctor-patient communication: A review. Ochsn. J. 2010, 10, 38–43. [Google Scholar]
- Pai, N.P.; Vadnais, C.; Denkinger, C.; Engel, N.; Pai, M. Point-of-care testing for infectious diseases: Diversity, complexity, and barriers in low-and middle-income countries. PLoS Med. 2012, 9, e1001306. [Google Scholar] [CrossRef] [PubMed]
- Custers, T.; Arah, O.A.; Klazinga, N.S. Is there a business case for quality in The Netherlands? A critical analysis of the recent reforms of the health care system. Health Policy 2007, 82, 226–239. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Hines, M.B.; Power, E.; Shaw, T.; Togher, L. Enabler for Interdisciplinary eHealthcare: A Qualitative Study; IOS Press: Amsterdam, The Netherlands, 2017; Volume 239, p. 160. [Google Scholar]
- Bailey, T.M.; Topham, T.M.; Wantz, S.; Grant, M.; Cox, C.; Jones, D.; Zerbe, T.; Spears, T. Laboratory process improvement through point-of-care testing. Joint Comm. J. Qual. Improv. 1997, 23, 362–380. [Google Scholar] [CrossRef]
- Hwang, J.; Christensen, C.M. Disruptive innovation in health care delivery: A framework for business-model innovation. Health Aff. 2008, 27, 1329–1335. [Google Scholar] [CrossRef] [PubMed]
- Amit, R.; Zott, C. Value creation in e-business. Strateg. Manag. J. 2001, 22, 493–520. [Google Scholar] [CrossRef]
- Holloway, I.; Galvin, K. Qualitative Research in Nursing and Healthcare; John Wiley and Sons: Hoboken, NJ, USA, 2016. [Google Scholar]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Simonse, L. Modelling Business Models; Design Issues; MIT Press: Cambridge, MA, USA, 2014; pp. 67–82. [Google Scholar]
- Van Meeuwen, D.P.; van Walt Meijer, Q.J.; Simonse, L.W. Care Models of eHealth Services: A Case Study on the Design of a Business Model for an Online Precare Service. J. Med. Int. Res. Protoc. 2015, 4, e32. [Google Scholar] [CrossRef] [PubMed]
- Simon, H.A. Prediction and prescription in systems modeling. Oper. Res. 1990, 38, 7–14. [Google Scholar] [CrossRef]
- Bogaart, H. Personal Interview: Influencers on Transactions within a General Practice; Verhees, B., Kuijk, K.V., Eds.; Delft University of Technology, Faculty of Industrial Design Engineering: Delft, The Netherlands, 2017. [Google Scholar]
- Walsham, G. Actor-network theory and IS research: Current status and future prospects. In Information Systems and Qualitative Research; Springer: Berlin, Germany, 1997; pp. 466–480. [Google Scholar]
- De kwaliteit van Elektronische Verslaglegging Door Huisartsen Gemeten: EPD-Scan Regio Twente, eindrapport. Available online: https://www.narcis.nl/publication/RecordID/publicat%3A1002257 (accessed on 20 December 2017).
- Loghum, B.S.V. Steeds meer virtueel contact tussen eerste en tweede lijn: Teleconsultatie niet meer weg te denken in de praktijk. In Mednet; Springer: Berlin, Germany, 2012; Volume 5, pp. 23–25. [Google Scholar]
- Wolff, J.S.; Wogalter, M.S. Comprehension of pictorial symbels: Effects of context and test method. Hum. Factors 1998, 40, 173–186. [Google Scholar] [CrossRef]
- Patton, M.Q. Qualitative interviewing. In Qualitative Research and Evaluation Methods; Sage: Newcastle upon Tyne, UK, 2002. [Google Scholar]
- Casadesus-Masanell, R.; Ricart, J.E. Strategy vs. Business Models vs. Tactics; IESE Business School: Madrid, Spain, 2009. [Google Scholar]

| Practice No. | Geographic Information | No. Patients in Practice | Supporting Hours | Demographic Information Patients | Specialty’s Practice | No. of GP’s in Practice |
|---|---|---|---|---|---|---|
| 1 | Rural | 2900 | 65 h pharmacy assistant 66 h practice assistant 18 h practice support (chronicle diseases) | Aged population | Heart and vascular disease Intern pharmacy | 2 |
| 2 | Urban | 8400 | 80 h practice support GGZ support 15 employees | Normal | Palliative | 4 |
| 3 | Urban | 9 employees | Aged population | Heart and vascular disease | 4 | |
| 4 | Urban | 3000 | 20 h practice support (chronicle diseases) 1 GP in training 38 h practice support | Low multicultural rate | none | 2 |
| 5 | Urban | 4670 | 24 h practice support 13 h GGZ support 80 h practice assistant | Palliative | 3 | |
| 6 | Urban | Diagnostic Center | ||||
| 7 | Urban | Diagnostic Center |
| Actor View From | Actor to | Transaction | ||
|---|---|---|---|---|
| Value | Revenue | Connectivity | ||
| GP | - | - | - | |
| ... | Dutch College of General Practitioners (NHG) | ∎∎∎∎ Quality guarantee of the treatment, reinsurance for the general practitioner (GP) | ∎∎∎∎∎ NHG provides GP with Norm standards through (Website) | |
| Health Insurer | ∎∎ Negotiating compensation rates | ∎∎∎∎∎∎∎ Compensation consult on bank account ∎∎∎ Compensation test on bank account | ∎∎∎ Consult compensation request in the General Practitioners Information System (HIS) ∎∎∎ Double consult compensation request (HIS) ∎∎∎ Test compensation request (HIS) | |
| Secondary care | ∎∎∎∎ Specific referral ∎ Diagnosis from specialist ∎ Less referrals | ∎ Sample photo ∎ to specialist ( Zorgdomein) Diagnose from specialist (Zorgdomein) | ||
| Diagnostic center | ∎∎∎∎ Delivers product and service to GP ∎∎ Acquisition of new POC products ∎∎∎∎ Quality insurer and calibration of POCT equipment | ∎∎∎∎ Validation test result (
Zorgmail, Zorgdomein) ∎∎∎∎ Number of tests performed (Zorgmail, Zorgdomein) | ||
| GP assistant | ∎ Referral to GP when complex test result ∎ Create extra appointment to perform test | ∎∎∎ Test result to GP from assistant (paper, verbal, HIS) ∎∎∎∎∎ Test to assistant (paper, verbal) | ||
| POCT | ∎∎∎∎∎∎ Extra diagnosis information, additional argument ∎ Creates sample for testing | ∎ Product investment | ||
| Patient | ∎∎∎∎∎∎∎∎ Complementary information and evidence for diagnosis to the patient ∎ Same day diagnosis from the specialist | ∎∎∎∎ Test result to GP (paper) ∎ Test result to patient (telephone) | ||
| GP assistant | ||||
| Health Insurer | ∎ Consult compensation request (HIS) | |||
| POCT | ∎∎∎∎∎∎∎ Perform tests for additional diagnosis information | Test result information (paper, visual) | ||
| Patient | ∎∎∎∎∎∎∎ Perform tests for direct diagnosis ∎ Patient brings sample for testing | ∎∎∎∎∎∎ Test result to patient (paper, verbal) | ||
| Health Insurer | ||||
| Secondary care | ∎ Compensation for teledermatology diagnosis on bank account | ∎ Test compensation request | ||
| Diagnostic Center | ∎∎∎∎ Compensation per test on bank account | ∎∎∎∎ Test compensation request | ||
| Number of GP’s | Findings from GP’s That Influence Integration of POC Products |
|---|---|
| ∎∎∎∎∎ | A GP has his own preferential areas to work in |
| ∎∎∎∎ | A GP has his specific work skills, subjective knowledge |
| ∎∎∎∎∎ | When a GP purchases any new equipment and when it is available in the practice, a GP needs to explain why you do or do not use the equipment during a consultation |
| ∎∎∎∎∎ | The interpretation of the test result by a GP is the diagnosis, and not the test result itself |
| ∎∎∎∎∎ | The usages and results of a test need to be within reasonable time to have value for the GP, otherwise the patient will be referred |
| ∎∎∎∎ | Current external actors do not stimulate new use of POC products |
| ∎∎∎∎∎ | The GP purchases only a new product when this product is widely validated between actors within the health system |
| ∎∎∎∎∎ | When product use is too complex or time consuming for examination and result, the GPs refer the patient to other parties (hospital, diagnostic center) |
| ∎∎∎ | Practice owners have a small commercial mind-set for their practice, care first, revenue second |
| ∎∎∎∎∎ | POCT results need to be interpreted by the GP to create a diagnosis, and this diagnosis is submitted to the HIS, and therefore, this submission happens manually |
| ∎∎∎∎∎ | POC products need to be of a size that can easily fit inside the general practice |
| ∎∎∎ | The GP is more cost effective than the secondary care → only 5% of the Dutch care costs are on behalf of the primary care |
| ∎∎∎ | The rural areas are more dependent on treatments within the general practice, because of the lack of hospital density within the area |
| Actor | Actor | Negative Value Transactions | |
|---|---|---|---|
| GP | |||
| GP assistant | ∎∎∎∎∎ | Complex usages of product, many actions needed to operate | |
| ∎∎∎∎∎ | Product usage is time consuming | ||
| POCT | ∎∎∎ | Many false negatives | |
| ∎∎∎∎∎ | Large “grey” diagnosis area of interpretation | ||
| Patient | ∎∎∎∎ | No decisive answer | |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Verhees, B.; Van Kuijk, K.; Simonse, L. Care Model Design for E-Health: Integration of Point-of-Care Testing at Dutch General Practices. Int. J. Environ. Res. Public Health 2018, 15, 4. https://doi.org/10.3390/ijerph15010004
Verhees B, Van Kuijk K, Simonse L. Care Model Design for E-Health: Integration of Point-of-Care Testing at Dutch General Practices. International Journal of Environmental Research and Public Health. 2018; 15(1):4. https://doi.org/10.3390/ijerph15010004
Chicago/Turabian StyleVerhees, Bart, Kees Van Kuijk, and Lianne Simonse. 2018. "Care Model Design for E-Health: Integration of Point-of-Care Testing at Dutch General Practices" International Journal of Environmental Research and Public Health 15, no. 1: 4. https://doi.org/10.3390/ijerph15010004





