The Neonatal Intensive Care Unit: Environmental Stressors and Supports
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Recruitment
2.2. Procedure
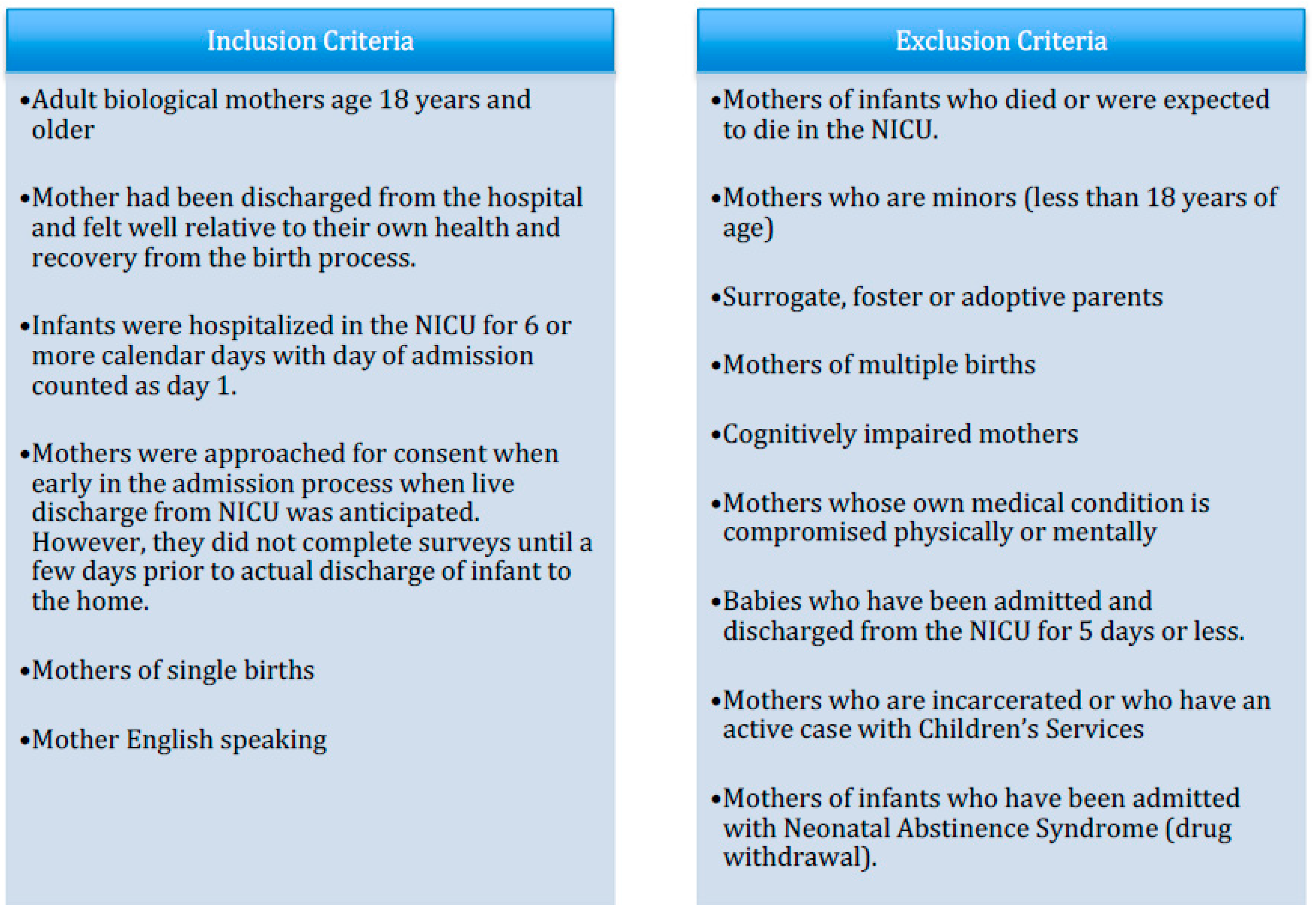
2.3. Participants
2.4. Data Analysis
3. Results
3.1. Amount and Quality of Communication with Medical Staff
Participant: I found it extremely stressful that I never really knew what was going on. Aside from a few nurses, most of the time when I asked a question about why my baby was doing something (For example the “squeaky breathing”) the nurses just said it was normal. However, most of them did not take the time to explain why he was doing such things or what was happening.
Participant: During 2 procedures no one was able to give us an update—one was told to last and hour and 3.5 h later they were finished—we asked other nurses to check for us but they were only told their (the procedure) aren’t (wasn’t) done. When he has (was) admitted no one told us why other than his blood work was really bad, and 4 h later we were finally able to come down to (the) NICU. Someone could have explained more why he was rushed down from well-baby. We were very fearful and anxious which I believe could have been avoided with a little more communication.
Participant: What was helpful to me during our time here was the helpful nursing staff and great doctors. They were great at explaining things and it was reassuring to know that my baby was getting the best care possible. Rounding is a great thing.
Participant: Having the nurses sit down and explain what was truly going on with our baby helped (to) comfort us and lessen the stress we had.
3.2. Bedside Manner of Medical Stafff
Participant: … I was reprimanded rudely when I came back from lunch to find my baby had spit up on herself and pooped her diaper and I changed her and cleaned her up in between her feeding time… NOT OK. Some RN’s are quite rude if you’re not getting enough breast milk/don’t have enough.
Participant: The most frustrating thing is when nurses don’t try. For example just hook the baby to the feeding tube so they can sit and talk on the phone (yes, personal phone calls).
Participant: I love most of the nurses but there are a few that I have seen to be careless and too rough with the babies. This made me highly upset because they were so careless and rough. That is unacceptable—these babies are tough but they go through too much and are too precious to be treated that way.
Participant: The nursing staff however was very helpful in assisting and informing me about breastfeeding. (Names specific nurse) was my favorite! She was so helpful and kind. I would describe her as compassionate and yet professional.
Participant: I really appreciated the nurses giving me my space but still checking in on me from time to time. They were also very helpful with supplies for breastfeeding. They never seem to get irritated or frustrated which makes me as a parent feel more comfortable and at home.
3.3. Feeling Alienated from Infant’s Care
Participant: It also seemed like the nurses would rather do things themselves than have me do it (i.e., feedings, baths). It seems like we are in the way and that’s frustrating.
Participant: I was a little disappointed I did not get to witness my baby’s first bath. I didn’t know when they were planning to bathe her.
Participant: … Her nurse came by and told me that it wasn’t her care hour and it would be best if I was there then instead. It made me feel completely unwelcome and as if I wasn’t allowed to see my own child. I had a meltdown. I went back to my room and sobbed.
3.4. Support from Other NICU Moms and Families
Participant: Staying at hospital-based housing (and) talking to other families that have had their babies early is nice.
Participant: Just hearing stories from other women that went through the same thing and their child is/was grown or older and going great, gives me hope and praying makes everything better.
Participant: What was helpful to me during our time here was … talking with other moms going through similar situations and being able to empathize and talk with them.
3.5. NICU Physical Environment and Regulations
Participant: Having to choose between family members to only allow for 3 at a time, lack of waiting area for visitors waiting their turn. Having to coordinate feeding times with the cafeteria hours, not eating due to cafeteria being closed after feedings. Put vending options by unit. Bathrooms available in unit!!! Very hard after surgery to walk far to use bathroom when the one bathroom for the unit is being used.
Participant: Being able to call/visit 24/7 helped. Not being allowed to sleep here was stressful. Poor support trying to pump/breastfeed was stressful. Having rotating doctors was comforting because they all have different views about the situations and medical conditions.
Participant: I feel it is not fair that every baby (is) not in a room with their parents. And (parents) not (being) able to stay, (but) wanting to be with their premie child—something needs to change with that. Because (for) parents who (have) never been through things like this, which is the NICU, (it) is not fair to them. It’s already (missing word here) that we parents (are) not able to take them home. To know you can’t stay the night—I don’t like. How is that you can visit 24 h but not sleep? It’s very stressful on parents.
4. Discussion
4.1. Amount and Quality of Communication with Medical Staff
4.2. Bedside Manner of Medical Staff
4.3. Feeling Alienated from Infant’s Care
4.4. Support from Other NICU Moms and Families
4.5. NICU Physical Environment and Regulations
4.6. Strengths and Limitations
5. Conclusions
Clinical Implications
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Barkin, J.L.; Wisner, K.L.; Bromberger, J.T.; Beach, S.R.; Terry, M.A.; Wisniewski, S.R. Development of the Barkin index of maternal functioning. J. Women’s Health 2010, 19, 2239–2246. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; Wisner, K.L.; Bromberger, J.T.; Beach, S.R.; Wisniewski, S.R. Assessment of functioning in new mothers. J. Women’s Health 2010, 19, 1493–1499. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.C.; Martin-Anderson, S.; Dudley, R.A. Clinician perspectives on barriers to and opportunities for skin-to-skin contact for premature infants in neonatal intensive care units. Breastfeed. Med. 2012, 7, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Del Fabbro, A.; Cain, K. Infant Mental Health and Family Mental Health Issues. Newborn Infant Nurs. Rev. 2016, 16, 281–284. [Google Scholar] [CrossRef]
- Pleck, J.H.; Masciadrelli, B.P. Paternal involvement by U.S. residential fathers: Levels, sources, and consequences. In The Role of the Father in Child Development, 4th ed.; Lamb, M.E., Ed.; Wiley: Hoboken, NJ, USA, 2004; pp. 222–271. [Google Scholar]
- Harrison, W.; Goodman, D. Epidemiologic trends in neonatal intensive care, 2007–2012. JAMA Pediatr. 2015, 169, 855–862. [Google Scholar] [CrossRef] [PubMed]
- Holditch-Davis, D.; Bartlett, T.R.; Blickman, A.L.; Miles, M.S. Posttraumatic stress symptoms in mothers of premature infants. J. Obstet. Gynecol. Neonatal Nurs. 2003, 32, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Miles, M.S.; Holditch, D.; Schwartz, T.A.; Sher, M. Depressive symptoms in mothers of prematurely born infants. J. Dev. Behav. Pediatr. 2007, 28, 36–44. [Google Scholar] [CrossRef] [PubMed]
- O’Hara, M.W.; McCabe, J.E. Postpartum depression: Current status and future directions. Annu. Rev. Clin. Psychol. 2013, 370–407. [Google Scholar] [CrossRef] [PubMed]
- Feldman, R.; Granat, A.; Pariente, C.; Kanety, H.; Kuint, J.; Gilboa-Schechtman, E. Maternal depression and anxiety across the postpartum year and infant social engagement, fear regulation, and stress reactivity. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 919–927. [Google Scholar] [CrossRef] [PubMed]
- Gonya, J.; Nelin, L.D. Factors associated with maternal visitation and participation in skin-to-skin care in an all referral level IIIc NICU. Acta Paediatr. 2013, 102, e53–e56. [Google Scholar] [CrossRef] [PubMed]
- Feldman, R.; Rosenthal, Z.; Eidelman, A.I. Maternal-preterm skin-to-skin contact enhances child physiologic organization and cognitive control across the first 10 years of life. Biol. Psychiatry 2014, 75, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Holditch-Davis, D.; Miles, M.S. Mothers’ stories about their experiences in the neonatal intensive care unit. Neonatal Netw. 2000, 19, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Singer, L.T.; Fulton, S.; Kirchner, H.L.; Eisengart, S.; Lewis, B.; Short, E.; Min, M.O.; Kercsmar, C.; Baley, J.E. Parenting very low birth weight children at school age: Maternal stress and coping. J. Pediatr. 2007, 151, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Hall, S.; Hynan, N.; Phillips, R.; Press, J.; Kenner, C.; Ryan, D.J. Development of program standards for psychosocial support of parents of infants admitted to a neonatal intensive care unit: A national interdisciplinary consensus model. Newborn Infant Nurs. Rev. 2015, 15, 24–27. [Google Scholar] [CrossRef]
- Heydarpour, S.; Keshavarz, Z.; Bakhtiari, M. Factors affecting adaptation to the role of motherhood in mothers of preterm infants admitted to the neonatal intensive care unit: A qualitative study. J. Adv. Nurs. 2017, 73, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Aagaard, H.; Hall, E.O. Mothers’ experiences of having a preterm infant in the neonatal care unit: A meta-synthesis. J. Pediatr. Nurs. 2008, 23, e26–e36. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; Wisner, K.L.; Wisniewski, S.R. The psychometric properties of the Barkin Index of Maternal Functioning. J. Obstet. Gynecol. Neonatal Nurs. 2014, 43, 792–802. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of Postnatal Depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Wisner, K.L.; Sit, D.K.; McShea, M.C.; Rizzo, D.M.; Zoretich, R.A.; Hughes, C.L.; Eng, H.F.; Luther, J.F.; Wisniewski, S.R.; Costantino, M.L.; et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry 2013, 70, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; McKeever, A.; Lian, B.; Wisniewski, S.R. Correlates of Postpartum Maternal Functioning in a Low-Income Obstetric Population. J. Am. Psychiatr. Nurses Assoc. 2017, 23, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; Willis, G.B.; Hawkins, K.C.; Stanfill-Thomas, T.; Beals, L.; Bloch, J.R. Semantic Assessment of the Barkin Index of Maternal Functioning in a Medically Underserved Obstetric Population. Perspect. Psychiatr. Care 2017, 53, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; Wisner, K.L.; Bromberger, J.T.; Beach, S.R.; Wisniewski, S.R. Factors associated with postpartum maternal functioning in women with positive screens for depression. J. Women’s Health 2016, 25, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Weiss, S.; Goldlust, E.; Vaucher, Y.E. Improving parent satisfaction: An intervention to increase neonatal parent-provider communication. J. Perinatol. 2010, 30, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Merriam-Webster Online. Available online: https://www.merriam-webster.com/dictionary/bedside%20manner?utm_campaign=sd&utm_medium=serp&utm_source=jsonld (accessed on 2 January 2018).
- Person, A.; Finch, L. Bedside Manner: Concept Analysis and Impact on Advanced Nursing Practice. Int. J. Adv. Nurs. Pract. 2008, 10, 1–6. [Google Scholar]
- Roter, D. The enduring and evolving nature of the patient-physician relationship. Patient Educ. Couns. 2000, 39, 5–15. [Google Scholar] [CrossRef]
- Barkin, J.L.; Bloch, J.R.; Hawkins, K.C.; Thomas, T.S. Barriers to optimal social support in the postpartum period. J. Obstet. Gynecol. Neonatal Nurs. 2014, 43, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Preyde, M.; Ardal, F. Effectiveness of a parent “buddy” program for mothers of very preterm infants in a neonatal intensive care unit. CMAJ 2003, 168, 969–973. [Google Scholar] [PubMed]
- Roman, L.A.; Lindsay, J.K.; Boger, R.P.; DeWys, M.; Beaumont, E.J.; Jones, A.S.; Haas, B. Parent-to-parent support initiated in the neonatal intensive care unit. Res. Nurs. Health 1995, 18, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Stacey, S.; Osborn, M.; Salkovskis, P. Life is a rollercoaster … What helps parents cope with the Neonatal Intensive Care Unit (NICU)? J. Neonatal Nurs. 2015, 21, 136–141. [Google Scholar] [CrossRef] [Green Version]
- Baird, J.; Davies, B.; Hinds, P.S.; Baggott, C.; Rehm, R.S. What Impact Do Hospital and Unit-Based Rules Have Upon Patient and Family-Centered Care in the Pediatric Intensive Care Unit? J. Pediatr. Nurs. 2015, 30, 133–142. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, K.; Bracht, M.; Macdonell, K.; McBride, T.; Robson, K.; O’Leary, L.; Christie, K.; Galarza, M.; Dicky, T.; Levin, A.; et al. A pilot cohort analytic study of Family Integrated Care in a Canadian neonatal intensive care unit. BMC Pregnancy Childbirth 2013, 13, S12. [Google Scholar] [CrossRef] [PubMed]
- Barkin, J.L.; Wisner, K.L. The role of maternal self-care in new motherhood. Midwifery 2013, 29, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
| Categorical Variables-Mother | n | % |
|---|---|---|
| Race | ||
| White | 27 | 60.0 |
| Black | 13 | 28.9 |
| Other | 5 | 11.1 |
| Hispanic | ||
| Yes | 2 | 4.4 |
| No | 43 | 95.6 |
| Marital Status | ||
| Married | 23 | 51.1 |
| Not Married | 22 | 48.9 |
| Education | ||
| <High School | 1 | 2.2 |
| High School diploma or GED | 21 | 46.7 |
| Associate degree/Technical degree | 8 | 17.8 |
| College degree/Postgrad | 15 | 33.3 |
| Insurance | ||
| Medicaid | 20 | 44.4 |
| Other/Private | 25 | 55.6 |
| Employment Status | ||
| Full-time | 21 | 46.7 |
| Part-time | 11 | 24.4 |
| Unemployed | 13 | 28.9 |
| Delivery Type | ||
| Vaginal | 15 | 33.3 |
| C-section | 30 | 66.7 |
| Other children admitted to NICU | ||
| Yes | 4 | 9.1 |
| No | 40 | 90.9 |
| Continuous Variables-Mother | N | Mean (SD) |
| Mother’s age (years) | 45 | 28.9 (5.6) |
| Length of Stay (days) | 45 | 4.1 (1.4) |
| Total number of adults in home | 45 | 2.0 (0.7) |
| Total number of children | 45 | 1.7 (1.0) |
| BIMF-NICU | 45 | 96.1 (14) |
| EPDS | 45 | 7.7 (4.3) |
| PSS:NICU | 45 | 2.9 (0.9) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Williams, K.G.; Patel, K.T.; Stausmire, J.M.; Bridges, C.; Mathis, M.W.; Barkin, J.L. The Neonatal Intensive Care Unit: Environmental Stressors and Supports. Int. J. Environ. Res. Public Health 2018, 15, 60. https://doi.org/10.3390/ijerph15010060
Williams KG, Patel KT, Stausmire JM, Bridges C, Mathis MW, Barkin JL. The Neonatal Intensive Care Unit: Environmental Stressors and Supports. International Journal of Environmental Research and Public Health. 2018; 15(1):60. https://doi.org/10.3390/ijerph15010060
Chicago/Turabian StyleWilliams, Kristen G., Kayla T. Patel, Julie M. Stausmire, Christy Bridges, Mary W. Mathis, and Jennifer L. Barkin. 2018. "The Neonatal Intensive Care Unit: Environmental Stressors and Supports" International Journal of Environmental Research and Public Health 15, no. 1: 60. https://doi.org/10.3390/ijerph15010060





